Abstract
The objectives of this study are 1) To review the published data and document the current knowledge on allergic manifestations to the fruit mango 2) To highlight the two distinct clinical presentations of hypersensitivity reactions caused by mango 3) To discuss the role of cross-reactivity 4) To increase awareness of potentially life threatening complications that can be caused by allergy to mango. An extensive search of the literature was performed in Medline/PubMed with the key terms "mango", "anaphylaxis", "contact dermatitis", "cross-reactivity", "food hypersensitivity", "oral allergy syndrome" and "urticaria". The bibliographies of all papers thus located were searched for further relevant articles. A total of 17 reports describing 22 patients were documented, including ten patients with immediate hypersensitivity reaction and twelve patients with delayed hypersensitivity reaction to mango. Ten of these patients (four with immediate reaction; six with delayed reaction) were from geographical areas cultivating mango, whereas twelve patients (six with immediate reaction; six with delayed reaction) were from the countries where large scale mango cultivation does not occur. The clinical features, pathogenesis and diagnostic modalities of both these presentations are highlighted. The fruit mango can cause immediate and delayed hypersensitivity reactions, as also "oral allergy syndrome". Although rare, it can even result in a life threatening event. Reactions may even occur in individuals without prior exposure to mango, owing to cross reactivity. It is imperative to recognize such a phenomenon early so as to avoid potentially severe clinical reactions in susceptible patients.
Keywords: Allergy, Anaphylaxis, Contact dermatitis, Cross-reactivity, Mango, Oral allergy syndrome, Urticaria
INTRODUCTION
The fruit mango (Mangifera indica) belongs to the family Anacardiacae and is often, regarded as the 'king of fruits'. It is partaken in many forms, both during as well as off season. During season, it is eaten as fresh fruit, shakes and ice creams while off season, it is available as pickles, juices and jams. Native to southern Asia, especially India and Burma, mango has been cultivated in the Indian subcontinent for thousands of years. Nearly half of the world's mangoes are cultivated in India alone and is the country's national fruit. By the 10th century AD, cultivation of mango had begun in East Africa and later in Brazil, the West Indies and Mexico and is now cultivated in most frost-free tropical and warmer subtropical climates including Spain and Australia. Despite the large consumption of mangoes, especially in India, hypersensitivity reactions to mango are distinctly rare. Allergy to mango can manifest in two forms viz. the immediate hypersensitivity reaction presenting as anaphylaxis, angioedema, erythema, urticaria, wheezing dyspnoea and the late reaction presenting as contact dermatitis and periorbital edema. Allergic reaction to mango was first described in 1939, by Zakon [1] in a 29-year-old female who developed acute vesicular dermatitis involving lips and circumoral area, 24 h after eating a mango. Kahn in 1942 [2] was the first to document immediate hypersensitivity to mango in a female patient, who also suffered from hay fever. To our knowledge, this is the first systematic review on hypersensitivity manifestations to the fruit mango; it aims to document an updated summary of the evidence in the field.
Data sources
An extensive search of the literature was performed in Medline/PubMed and other available database sources with the key terms "mango" and "anaphylaxis", "contact dermatitis", "cross-reactivity", "food hypersensitivity", "oral allergy syndrome" and "urticaria". The bibliographies of all papers thus located were searched for further relevant articles. As this is a narrative review of published studies, institutional review board clearance was not required.
RESULTS
A total of 17 reports documenting 22 patients were found on searching the databases. A total of only ten patients with immediate hypersensitivity reaction [2-10] and twelve patients with delayed hypersensitivity reaction [1, 11-17] to mango were documented in these reports.
Geographical distribution
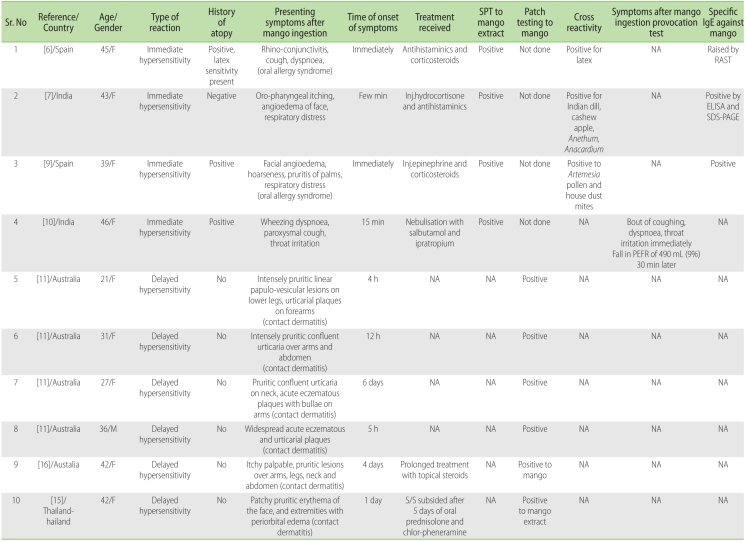
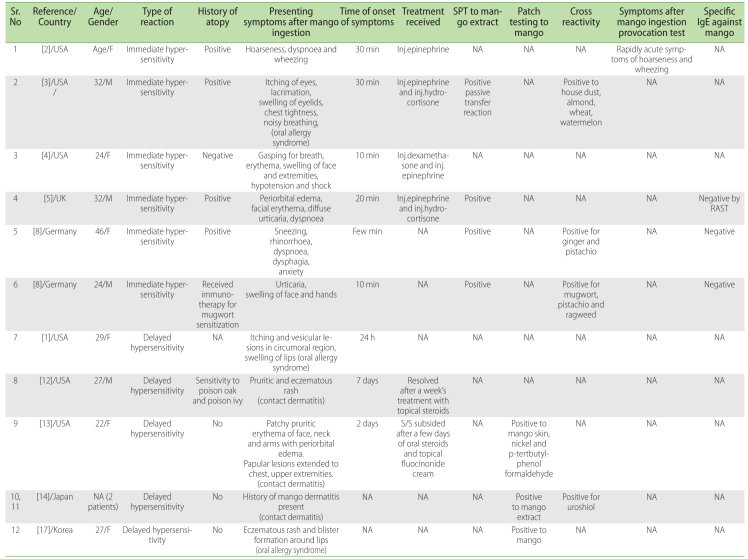
Ten of these patients (four with immediate reaction [6, 7, 9, 10]; six with delayed reaction [11, 15, 16]) were reported from geographical areas cultivating mango. Five of these patients were documented from Australia [11, 16], two each from Spain [6, 9] and India [10] and one patient from Thailand [15] (Table 1). Twelve patients (six with immediate reaction [2-5, 8]; six with delayed reaction [1, 12-14, 17]) were reported from the countries where large scale mango cultivation does not occur. Six of these patients were documented from USA [1-4, 12, 13], two each from Germany [8] and Japan [14] and one patient each from UK [5] and Korea [17] (Table 2).
Table 1.
Documented reports of hypersensitivity manifestations to mango from geographical regions cultivating the fruit
ELISA: enzyme linked immuno sorbet assay; IgE: immunoglobulin E; NA: not available; PEFR: peak expiratory flow rate; RAST: radio allergo sorbet assay; SDS PAGE: sodium dodecyl sulphate polyacrylamide gel electrophoresis; SPT: skin prick test.
Table 2.
Documented reports of hypersensitivity manifestations to mango from geographical regions not cultivating the fruit
ELISA: enzyme linked immuno sorbet assay; IgE: immunoglobulin E; NA: not available; PEFR: peak expiratory flow rate; RAST: radio allergo sorbet assay; SDS PAGE: sodium dodecyl sulphate polyacrylamide gel electrophoresis; SPT: skin prick test.
Immediate hypersensitivity to mango
The first patient, documented with immediate hypersensitivity to mango, by Kahn [2], had "some symptoms" initially on ingestion of mangoes. She was "persuaded" to undergo a mango ingestion provocation test with which she experienced "rapidly acute symptoms such as hoarseness, dyspnoea and bronchitic rales (asthma)". Her symptoms were relieved with injection epinephrine. Since then, this phenomenon has been described in only nine other patients. We have recently documented a 46-year-old lady [10], who presented to us with exacerbation of asthma within 15 min of ingestion of fresh mango.
Clinical features
Immediate hypersensitivity reaction to mango may manifest either as a systemic anaphylaxis or a local reaction. It presents as wheezing dyspnoea, erythema, urticaria, angioedema and anaphylaxis. Of the ten patients documented with immediate hypersensitivity reaction to mango, the symptoms overlapped with respiratory distress/dyspnoea developed in nine, angioedema in five [3, 5, 7-9] and erythema developed in three [4, 5, 8]. Mango allergy may rarely present as anaphylactic shock and was documented in two patients [3, 4]. Rubin et al. [3] described a 32-year-old African American male, who presented with itching of eyes and mouth, swelling of eyelids, profuse sweating and chest tightness along with features of shock within 30 min of consuming two slices of mango. The patient required intervention with parentral epinephrine and hydrocortisone for control of symptoms. A similar event was described in a 24-year-old Caucasian lady [4] within five minutes of ingestion of mango. Both these reports [3, 4] highlighted the fact that ingestion of mango can be life threatening in some susceptible individuals.
Type I hypersensitivity reaction occurs within a few minutes of mango ingestion. It was observed that symptoms in most of these patients occurred almost immediately [4-9], while in two patients, symptoms commenced in about 30 min [2, 3]. Our patient too developed wheezing dyspnoea, cough and throat irritation within 15 min after ingestion [10].
Pathogenesis
The immediate hypersensitivity reaction to mango is mediated through the classical IgE pathophysiological mechanisms and is thought to occur in individuals who were previously sensitized to the antigens present in the mango [6]. Sensitization usually occurs by prior ingestion, but it may also follow intake of other fruits belonging to family Anacardiaceae viz. cashew nut, pistachio nut, poison ivy, poison oak, sumac (Rhus glabia), and mastic. Sensitization by ingestion of mango in unrecognisable forms, such as fruit punch and fruit salad has also been reported [3]. Consumption of canned or packaged mango too can precipitate an allergic reaction as allergenicity of mango nectar persists even after heating, enzymatic degradation and mechanically caused tissue degradation [18].
This type of hypersensitivity reaction is thought to occur within minutes of combination of the mango antigen with the corresponding IgE antibody [6], which is in turn bound to the mast cell. This promptly causes mast cell degranulation, with the release of primary (histamine, proteases and acid hydrolases) and secondary (leukotrienes, prostaglandins and platelet activating factor) mediators of inflammation. This produces vasodilation, recruitment of eosinophils and leukocyte infilteration mediating an inflammatory response. This is followed by bronchoconstriction. Type I hypersensitivity reaction is also more often seen in atopic individuals [5]. History of atopy was present in eight of the ten reported patients, including ours [2, 3, 5, 6, 8-10].
Diagnosis
Antigen sensitization can be observed in the patients with immediate reaction to mango by prick to prick testing and can be confirmed by intra dermal testing with mango extract [10]. Information regarding the skin allergy test to mango was available in eight of the ten patients and was positive in all [3, 5-9]. Our patient too had a prick to prick test positive to mango extract which was confirmed by the positive intradermal test [10].
Specific IgE antibodies against mango, which mediate this reaction, may also be demonstrated in some but not all patients presenting with immediate hypersensitivity to mango. It is possible that in some patients, specific IgE antibodies against mango antigen may not be demonstrated as the corresponding allergens may be unstable and remain undetected. Specific IgE against mango was evaluated in six patients [5-9], but was positive in only three [6, 7, 9]. The IgE detection system currently available appears to be lacking some of the specific mango allergens and is yet to emerge as a yardstick for diagnosing type-1 sensitization to mango.
Oral food challenge test may also be used to elicit the immediate hypersensitivity reaction. The patient reported by Kahn [2] underwent a mango ingestion provocation test to establish the temporal relation between intake of mango and appearance of symptoms. Our patient too was subjected to an open oral food challenge test. She consented to ingest a slice of a mango under observation in the emergency room. Peak expiratory flow rate was recorded prior to ingestion. The patient had a bout of coughing, wheezing dyspnoea and irritation in the throat within 15 min of the ingestion. She also developed bilateral polyphonic rhonchi and we recorded an acute fall of 490 mL (9%) in peak expiratory flow. This reaction subsided within half an hour of the onset of symptoms after nebulisation with salbutamol and ipratropium [10].
Delayed hypersensitivity to mango
Mango is also known to rarely cause delayed hypersensitivity reaction in the form of contact dermatitis and periorbital edema, and has been documented in twelve patients till date [1, 11-17]. The first patient with allergic reaction to mango documented in the literature had presented with manifestations of delayed hypersensitivity [1].
Clinical features
The delayed type of hypersensitivity reaction to mango was documented in the form of contact dermatitis [1, 11-16], periorbital edema [13-15] and eczematous rash and blister formation around lips [17]. Amongst the twelve such patients described in the literature [1, 11-17], the symptoms overlapped with contact dermatitis present in eleven [1, 11-16], perorbital edema in four [13-15] and vesicular lesions and blister formation in the circumoral region in two [1, 17]. It was observed that the duration of onset of symptoms in these twelve patients was variable and ranged from 4 h [11] to 7 days [12].
Delayed hypersensitivity reaction to mango can occur either by direct contact with the mango or even the tree itself. Ingestion too, can cause a cell mediated response. The sensitizing substances include uroshiol, cardol, limonene and B-pinene. These are present in the skin, bark, pericarp as well as in the mango pulp up to five millimetres below the skin [15]. Three of these twelve patients [10, 13, 15] developed the symptoms after mango ingestion, while the remaining nine patients developed the reaction after contact with mango skin or bark of mango tree [11, 12, 14, 16, 17]. This type of reaction occurs frequently in non atopic individuals. Amongst these twelve patients, history of atopy was present in only one [12].
Pathogenesis
Delayed hypersensitivity to mango is cell mediated and CD-4 cells of Th-I type are thought to be the prime mediators of this reaction. The sensitizing substances (uroshiol, cardol, limonene and B-pinene) present in mango [14], get deposited in the epidermal layer of the skin and sensitize the CD-4 cells. On repeated exposure, the sensitized CD-4 cells first accumulate in the dermis and then migrate towards the epidermis where they release cytokines which damage keratinocytes, causing separation of these cells and leading to epidermal spongiosis [13]. Erythema and induration of the site occurs within 8-12 h of exposure, reaches a peak in 24-72 h, and then slowly subsides. This accounts for the later onset of symptoms in these patients.
Diagnosis
Patch testing can be done to elicit the delayed hypersensitivity reaction. It was done in ten of these twelve patients [11, 13-17] and was positive in all. Cross reactivity and positive specific IgE antibody against mango antigen was not reported in any of these twelve patients. This possibly rules out any concomitant immediate hypersensitivity reaction in the patients presenting with delayed manifestations.
Oral allergy syndrome
Oral allergy syndrome, also known as pollen food syndrome [19] is a well recognized, but little known disorder. It is characterized by tingling, burning sensation of lips, palate, tongue or oropharynx with or without swelling, within a few minutes of ingestion of a foodstuff. It is a type I hypersensitivity reaction and is IgE mediated. It occurs due to cross reactivity between certain food items and pollens, house dust mites, latex and other allergens and is only rarely manifested in patients without a previous sensitivity to pollen. Fresh fruit, vegetables and nuts are common causes of oral allergy syndrome. Some patients are allergic to a wide range of these foods. It has been shown that pollens from trees (especially birch), grasses and weeds contain proteins of similar structure to those present in certain fruit, vegetables, nuts and spices. These proteins are recognized by the immune system and on ingestion of a foodstuff which shares the same protein as the pollen, can result in triggering an allergic reaction in a susceptible individual. The basis of oral allergy syndrome is the presence of IgE antibodies that can recognize specific pollens as well as fruit allergens [20].
Oral allergy syndrome is also known to be associated with mango allergy and was documented in two [6, 9] of the 22 patients in the literature. However, three [1, 3, 17] other patients had symptoms suggestive of oral allergy syndrome, but the authors did not classify them as such. Three of these five patients had presented with immediate hypersensitivity to mango [3, 6, 9] and two with delayed hypersensitivity [1, 17]. Cross reactivity was evaluated in three of them, and was found to be positive in all. Although, oral allergy syndrome, by definition is a type I reaction, it is possible that its occurrence in patients with delayed hypersensitivity could be due to cross-reactivity.
Cross reactivity
Mango antigen has been shown to cross react with artemesia pollen, birch pollen, poison ivy, poison oak, mugwort, celery, carrot, pistachio nut, tomato, papaya and banana [9]. This cross reactivity is attributed to the fact that multiple antigens can bind to an IgE antibody at corresponding sites and result in an immune response. It was thought that allergens responsible for cross reactivity between botanically unrelated pollens and fruits, termed as profilins, accounted for this phenomenon [21, 22]. However, this is yet to be proved conclusively.
Allergy to mango has also occasionally been reported in people with latex (Hevea braziliensis) hypersensitivity, a phenomenon common in health care professionals, who frequently wear latex gloves [8, 23]. Rubber elongation factors; hevein and prohevein present in natural latex are the allergens thought to be responsible for this latex allergy which usually manifest as contact dermatitis, oropharyngeal allergy syndrome and rarely as anaphylaxis. The cross reactivity between latex and various fruits like chestnut, peach, avocado, passion fruit, fig, grape and orange has been termed as "latex-fruit syndrome" [23]. The specific proteins responsible for this cross-reactivity are yet to be identified.
Occurrence of contact dermatitis on first exposure to mango has also been observed in 17 (11 males; 6 females) youths from America during their visit to Israel [24]. These subjects developed skin rash, of varying intensity, one week after picking mangoes at a summer camp in Israel. None of these youths recalled previous contact with mangoes but all hailed from Oakland Bay area, northern California, USA where poison oak and/or poison ivy exposure was very common. The distribution of the rash was linear in 14 of these subjects and was photosensitive in four. In contrast, their fellow Israeli youths, who had never been exposed to poison ivy/oak, did not develop dermatitis while performing the same task. However, these subjects were not investigated further. The authors postulated that the exposure to poison ivy/oak, had sensitized these individuals to mango due to presence of common substances like uroshiol. An earlier report [12] had documented the occurrence of a pruritic and eczematous rash in a 27-year-old man, previously sensitized to poison oak and poison ivy. He developed the rash one week subsequent to resting his hand on his leg after peeling mango. A recent report [25] described a 25-year-old Caucasian male, a volunteer in Malawi, with a past history of contact dermatitis to poison oak, who developed swelling and erythematous rash over his lips, nose and left side of the face along with angioedema within 24 h of peeling a mango with his teeth. The patient was not investigated further and his symptoms were thought to be due to cross reactivity between mango and poison oak. These reports highlight the fact that cross reactivity can result in allergic manifestations to mango, even without prior exposure.
CONCLUSION
Allergic reactions to mango have also been observed in individuals residing in geographical areas where cultivation of the fruit does not occur [1-5, 8, 12-14, 17]. It may be due to sensitization to mango in packaged / canned forms as jams, juices, and pickles; or because of cross reactivity with other fruits belonging to the family Anacardiacae. Hence, a vigilant approach is required to identify these hypersensitivity manifestations especially in individuals residing in countries where large scale cultivation of mango does not occur.
Although rare, the fruit mango can cause immediate and delayed hypersensitivity reactions which can even result in a life threatening event. Allergic reactions to mango may also occur without prior exposure, owing to cross reactivity and it may also manifest as "oral allergy syndrome". It is imperative to recognize such manifestations early so as to avoid morbidity and potential mortality in susceptible individuals.
References
- 1.Zakon SJ. Contact dermatitis due to mango. J Am Med Assoc. 1939;113:1808. [Google Scholar]
- 2.Kahn IS. Fruit sensitivity. South Med J. 1942;35:858–859. [Google Scholar]
- 3.Rubin JM, Shapiro J, Muehlbauer P, Grolnick M. Shock reaction following ingestion of mango. JAMA. 1965;193:397–398. doi: 10.1001/jama.1965.03090050073027. [DOI] [PubMed] [Google Scholar]
- 4.Dang RW, Bell DB., 2nd Anaphylactic reaction to the ingestion of mango. Case report. Hawaii Med J. 1967;27:149–150. [PubMed] [Google Scholar]
- 5.Miell J, Papouchado M, Marshall AJ. Anaphylactic reaction after eating a mango. BMJ. 1988;297:1639–1640. doi: 10.1136/bmj.297.6664.1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duque S, Fernández-Pellón L, Rodríguez F. Mango allergy in a latex-sensitized patient. Allergy. 1999;54:1004–1005. doi: 10.1034/j.1398-9995.1999.00136.x. [DOI] [PubMed] [Google Scholar]
- 7.Hegde VL, Venkatesh YP. Anaphylaxis following ingestion of mango fruit. J Investig Allergol Clin Immunol. 2007;17:341–344. [PubMed] [Google Scholar]
- 8.Renner R, Hipler C, Treudler R, Harth W, Süß A, Simon JC. Identification of a 27 kDa protein in patients with anaphylactic reactions to mango. J Investig Allergol Clin Immunol. 2008;18:476–481. [PubMed] [Google Scholar]
- 9.Silva R, Lopes C, Castro E, Ferraz de Oliveira J, Bartolomé B, Castel-Branco MG. Anaphylaxis to mango fruit and cross-reactivity with Artemisia vulgaris pollen. J Investig Allergol Clin Immunol. 2009;19:420–422. [PubMed] [Google Scholar]
- 10.Sareen R, Gupta A, Shah A. Immediate hypersensitivity to mango manifesting as asthma exacerbation. J Bras Pneumol. 2011;37:135–138. doi: 10.1590/s1806-37132011000100020. [DOI] [PubMed] [Google Scholar]
- 11.Calvert ML, Robertson I, Samaratunga H. Mango dermatitis: allergic contact dermatitis to Mangifera indica. Australas J Dermatol. 1996;37:59–60. doi: 10.1111/j.1440-0960.1996.tb01000.x. [DOI] [PubMed] [Google Scholar]
- 12.Tucker MO, Swan CR. The mango-poison ivy connection. N Engl J Med. 1998;339:235. doi: 10.1056/NEJM199807233390405. [DOI] [PubMed] [Google Scholar]
- 13.Weinstein S, Bassiri-Tehrani S, Cohen DE. Allergic contact dermatitis to mango flesh. Int J Dermatol. 2004;43:195–196. doi: 10.1111/j.1365-4632.2004.01703.x. [DOI] [PubMed] [Google Scholar]
- 14.Oka K, Saito F, Yasuhara T, Sugimoto A. A study of cross-reactions between mango contact allergens and urushiol. Contact Dermatitis. 2004;51:292–296. doi: 10.1111/j.0105-1873.2004.00451.x. [DOI] [PubMed] [Google Scholar]
- 15.Wiwanitkit V. Mango dermatitis. Indian J Dermatol. 2008;53:158. doi: 10.4103/0019-5154.43215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thoo CH, Freeman S. Hypersensitivity reaction to the ingestion of mango flesh. Australas J Dermatol. 2008;49:116–119. doi: 10.1111/j.1440-0960.2008.00433.x. [DOI] [PubMed] [Google Scholar]
- 17.Lee D, Seo JK, Lee HJ, Kang JH, Sung HS, Hwang SW. A case of allergic contact dermatitis caused by a duoderm extrathin® dressing. Korean J Dermatol. 2009;47:612–614. [Google Scholar]
- 18.Dube M, Zunker K, Neidhart S, Carle R, Steinhart H, Paschke A. Effect of technological processing on the allergenicity of mangoes (Mangifera indica L.) J Agric Food Chem. 2004;52:3938–3945. doi: 10.1021/jf030792r. [DOI] [PubMed] [Google Scholar]
- 19.Katelaris CH. Food allergy and oral allergy or pollen-food syndrome. Curr Opin Allergy Clin Immunol. 2010;10:246–251. doi: 10.1097/ACI.0b013e32833973fb. [DOI] [PubMed] [Google Scholar]
- 20.Ausucua M, Dublin I, Echebarria MA, Aguirre JM. Oral Allergy Syndrome (OAS). General and stomatological aspects. Med Oral Patol Oral Cir Bucal. 2009;14:e568–e572. doi: 10.4317/medoral.14.e568. [DOI] [PubMed] [Google Scholar]
- 21.Saraswat A, Kumar B. Anaphylactic reaction to apple, banana and lychee: what is common between botanically disparate plant families? Int J Dermatol. 2005;44:996–998. doi: 10.1111/j.1365-4632.2005.02286.x. [DOI] [PubMed] [Google Scholar]
- 22.Paschke A, Kinder H, Zunker K, Wigotzki M, Steinhart H, Weβbecher R, Vieluf I. Characterization of cross-reacting allergens in mango fruit. Allergy. 2001;56:237–242. doi: 10.1034/j.1398-9995.2001.056003237.x. [DOI] [PubMed] [Google Scholar]
- 23.Brehler R, Theissen U, Mohr C, Luger T. "Latex-fruit syndrome": frequency of cross-reacting IgE antibodies. Allergy. 1997;52:404–410. doi: 10.1111/j.1398-9995.1997.tb01019.x. [DOI] [PubMed] [Google Scholar]
- 24.Hershko K, Weinberg I, Ingber A. Exploring the mango-poison ivy connection: the riddle of discriminative plant dermatitis. Contact Dermatitis. 2005;52:3–5. doi: 10.1111/j.0105-1873.2005.00454.x. [DOI] [PubMed] [Google Scholar]
- 25.Trehan I, Meuli GJ. Mango contact allergy. J Travel Med. 2010;17:284. doi: 10.1111/j.1708-8305.2010.00420.x. [DOI] [PMC free article] [PubMed] [Google Scholar]