Abstract
Allergic conjunctivitis (AC) represents a spectrum of disorders, comprising seasonal allergic conjunctivitis (SAC), perennial allergic conjunctivitis (PAC), atopic keratoconjunctivitis (AKC), vernal keratoconjunctivitis (VKC) and giant papillary conjunctivitis. Of these ocular allergy types, SAC and PAC are the most common.The most striking difference within this group of ocular diseases is that SAC and PAC remain self-limited without ocular surface damage, while AKC and VKC can compromise the cornea, causing ulcers and scarring and can ultimately lead to vision loss. Data on AC in the Asia Pacific is scarce however some understanding of prevalence of the condition has been obtained from the International Study of Asthma and Allergies in Childhood (ISAAC) studies and more recently from the Allergies in Asia Pacific study as well as some information from individual country surveys. Unfortunately none of this data has been collected using validated survey instruments specifically designed for AC. Surveys such as ISAAC have been predominantly concerned with respiratory allergic symptoms with questions added that incorporate some ocular symptoms. These questionnaires do not detect individuals who may have AC in the absence of allergic rhinitis. Using hospital ophthalmology outpatient populations for prevalence studies of ocular allergy immediately introduces a bias towards the more severe, complex forms of the condition as patients with the milder forms of SAR and PAR will rarely present to a hospital outpatient clinic. There is a real need for the development of validated questionnaires specifically addressing ocular allergy. There are no widely accessible studies examining prevalence of the complex forms of ocular allergy (AKC, VKC) in Asia Pacific region. This review will provide an overview of ocular allergy, its classification, clinical presentation and differential diagnosis, and will also discuss what is known about the epidemiology of ocular allergy in the Asian Pacific region.
Keywords: Allergic conjunctivitis, Ocular allergy, Epidemiology, Asia Pacific, AKC, VKC, ISAAC studies
INTRODUCTION
Until recently, little attention has been given to allergic conjunctivitis (AC) in its own right as a comorbid condition with other atopic disorders such as asthma, allergic rhinitis (AR), and atopic dermatitis.
In the USA ocular allergies are estimated to affect 15-20% of the general population [1]. In Sweden, one study reports a cumulative prevalence of AC of 19% in 12-13 year old schoolchildren with 92% having AR as well [2]. Unfortunately, in most studies and surveys terms such as hay fever and allergic rhinoconjunctivitis (ARC) have been used and AC prevalence has been extrapolated from this; very few studies have explored AC specifically so our knowledge and understanding about AC is less well developed than it is for AR [3].
This review will provide an overview of ocular allergy, its classification, clinical presentation and differential diagnosis, and will also discuss what is known about the epidemiology of ocular allergy in the Asian Pacific region.
What is ocular allergy
AC is the commonest cause of red eye seen in allergy practice. Symptoms consist of watery eyes (88%), itching (88%), redness (78%), soreness (75%), swelling (72%) or stinging (65%).
It is difficult to diagnose ocular allergy in the absence of any itching.
Approximately 10% of all ophthalmology consults are for ocular allergy. In general practice, about 6% of consultations are for inflamed or red eyes, half of these being caused by ocular allergy [4]. For the allergist, red eye as a primary referral is uncommon but red eye is a common accompaniment to other allergic disorders; in fact, allergists treat the majority of patients with AC who present for medical attention.
Ocular allergy is distressing for sufferers. Over 50% of nasal allergy sufferers stated that watering and red/itching eyes were moderately to extremely bothersome in the recent Allergies in America survey, and for 15% of sufferers the ocular component of the allergic hypersensitive reactions was the most troublesome symptom [5]. Similarly, seasonal allergic conjunctivitis (SAC) sufferers have been shown to have a significantly reduced quality of life score as determined by the Rhinoconjunctivitis Quality of Life Questionnaire compared with age-matched non-SAC patient controls.
Classification of AC
AC represents a spectrum of disorders, comprising SAC, perennial allergic conjunctivitis (PAC), atopic keratoconjunctivitis (AKC), vernal keratoconjunctivitis (VKC) and giant papillary conjunctivitis (GPC). GPC is not always included in this grouping as it is caused by physical trauma and is typically associated with use of 'extended wear' soft contact lenses, although patients with a history of allergy may be at greater risk. Of these ocular allergy types, SAC and PAC are the most common.
Common ocular clinical features of SAC, PAC, AKC and VKC include redness, itching and tearing. The most striking difference within this group of ocular diseases is that SAC and PAC remain self-limited without ocular surface damage, while AKC and VKC can compromise the cornea, causing ulcers and scarring and can ultimately lead to vision loss [6].
VKC most commonly occurs in boys living in warm, dry subtropical climates in the Middle East, and Mediterranean, Africa and South America. In Asia it is more commonly seen in Japan, Thailand and India but it is difficult to find comprehensive data on prevalence in Asia. The limbal form is most commonly seen in dark skinned individuals from Africa and India. Age of onset is generally less than 10 years and patients usually improve or "outgrow" the condition after puberty. Exacerbations are common in Spring but perennial attacks increase after a few years. VKC is associated with aeroallergen sensitisation and other atopic disorders such as asthma and AR [7, 8].
AKC is a chronic allergic ocular disease occurring in patients with a history of atopic dermatitis. Prevalence data varies but in one study, 20-40% of those with AD had AKC. Unlike VKC, It primarily affects adults in the second and third decades. AKC may involve eyelids, conjunctiva and cornea and is characterised by intense itching, tearing mucus discharge and redness. Chronic ocular surface inflammation may lead to vision loss. It has a complex pathogenesis with mixed type 1 and type IV hypersensitivity mechanisms described [9].
Differential diagnosis of ocular allergy
It is important for the allergist to be able to differentiate the various conditions that may present with a "red eye". A red eye indicates ocular inflammation and this may involve one or more of the ocular structures-eyelids, conjunctiva, orbit, cornea, sclera and uvea. Injection of the conjunctiva is the most common cause and is usually caused by a benign condition but a red eye may herald a more serious vision threatening condition for which urgent ophthalmology referral is necessary.
The commonest causes of conjunctivitis are infective and allergic. Viral and bacterial conjunctivitis are the commonest in childhood and are second to AC in adults. Viral conjunctivitis, characterised by tearing, watery discharge and burning, is most likely caused by adenovirus and picornavirus. Finding pre-auricular adenopathy is a helpful sign. Pain is suggestive of corneal involvement and requires urgent referral. Viral conjunctivitis is a highly contagious but self-limiting condition.
Herpes simplex virus is the most serious viral infection characterised by unilateral injection, irritation, mucoid discharge, pain and photophobia. Herpes vesicles may be seen on the face and lids. In most cases the cornea is affected and this requires treatment. Antivirals are indicated [4].
Bacterial conjunctivitis presents with unilateral, or more commonly, bilateral ocular irritation and conjunctival redness with a mucopurulent (yellowish-green) discharge that is worse in the morning.
Usual organisms are Staphylococcus aureus (more frequent in adults), Streptococcus pneumoniae and Haemophilus influenzae (more common in children).
Dry eye is a common condition often confused with AC as the symptoms of dry eye and ocular allergy frequently overlap.
Dry eye is a common complaint in the general population particularly in the older age group, post menopausal women, computer users, and contact lens wearers. It can be the end result of multiple conditions including autoimmune systemic diseases, ocular disease and as a side effect of various drugs. Symptoms include red eye, excess mucous production, grittiness, itching, burning and stinging. Symptoms usually worsen over the course of a day and are affected by air conditioning, fan forced hot air and computer work.
Drugs with anti cholinergic properties including antihistamines can contribute to the problem.
Dry eye results from abnormality in the tear film that is composed of three layers, the lipid, aqueous and mucin layers. Functional dry eye may result from diseases affecting any of the 3 layers. The diagnosis is made by a combination of typical symptoms, examination findings of a very thin precorneal tear film, abnormal Schirmer's test, an abnormal tear break up time and abnormal staining with special dyes.
Other conditions that may be considered in the differential diagnosis include blepharitis, a common but often unrecognized inflammatory condition related to bacterial colonisation of the eyelid margins. Toxic conjunctivitis may result from the regular use of any ocular preparation and in particular, abuse of over-the-counter vasoconstrictor drops. Contact dermatoconjunctivitis, involving conjunctiva and eyelids, is a delayed type hypersensitivity reaction associated with cosmetic preparations, contact lens solutions, topical drops and ointments.
Appropriate management of the patient presenting with red eye begins with correct diagnosis; it is only then that treatment may be appropriately tailored to relieve symptoms and underlying inflammation.
History and examination are very important in formulating a correct diagnosis. Careful examination includes assessment of visual acuity, ocular motility and location of redness. Clues may be gained from the presence and nature of facial and eyelid rashes. A complete examination of the conjunctiva includes lid eversion so the tarsal surface can be visualised. Serious conditions presenting with red eye are often unilateral, characterised by intense inflammation, pain and reduced visual acuity. Chronic, progressive symptoms may suggest conditions such as glaucoma, uveitis and keratitis. Urgent ophthalmology referral is necessary if any of these signs and symptoms are present.
What is known about AC in the Asia Pacific region?
Data on AC in the Asia Pacific is scarce however some understanding of prevalence of the condition has been obtained from the International Study of Asthma and Allergies in Childhood (ISAAC) studies [10, 11] and more recently from the Allergies in Asia Pacific (AIAP) study [12] as well as some information from individual country surveys. Unfortunately none of this data has been collected using validated survey instruments specifically designed for AC.
Validated questionnaires on ocular allergy have asked questions not only about the presence of "itching, watery and red eyes" but also about occurrence of symptoms in relation to pollen or animal exposure and In addition, about a "doctor diagnosis" of the condition. These latter two questions added higher specificity than asking about the symptoms of AC alone [13].
The ISAAC surveys
By far the largest body of epidemiological data on prevalence of allergic symptoms has been collected from the ISAAC studies. ISAAC is a multi-country cross sectional survey of two age groups of children, 6-7 year olds and 13-14 year olds, performed through schools. The major instrument used is a standardised questionnaire related to symptoms of ARC, eczema and asthma. Ocular symptoms, specifically "watery-itchy eyes", are asked about in the context of symptoms of rhinitis in the absence of a respiratory infection. The ISAAC questionnaire does not contain validated questions on ocular allergy. The specific questions in the ISAAC survey are:
Have you (or your child) ever had a problem with sneezing or runny or blocked nose when you (he or she) did not have a cold or flu?
In the past 12 months have (has your child) had a problem with sneezing or a runny or blocked nose when you (he or she) did not have a cold or flu?
In the past 12 months has this nose problem been accompanied by itchy-watery eyes?
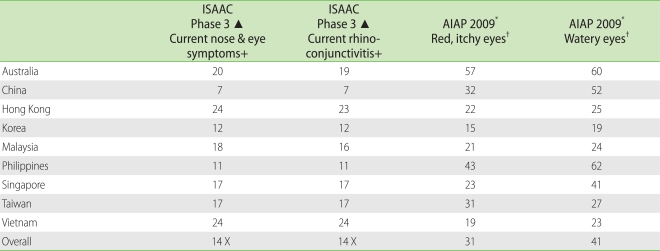
This 3rd question was used to estimate prevalence of current nose and eye symptoms. The 13-14 year age group involved 670,242 children across 232 centres in 97 countries. The average prevalence of current ARC symptoms across all centres was 14.6% [10].
Examination of the data collected for the 13-14 year old age group reveal prevalence rates of between 4.8% for Indonesia up to 17.6% in Japan, 22.6% in Hong Kong and 23.9% in Bangkok (Table 1). ARC was found to be more prevalent in areas of greater affluence while the lowest levels were seen in more rural regions. There was a demonstration of increasing prevalence of ARC symptoms between the ISAAC studies spanning a period of 5-10 years [10].
Table 1.
Ocular symptoms from ISAAC and AIAP data
ISAAC: International Study of Asthma and Allergies in Childhood, AIAP: Allergies in Asia Pacific. All figures are percentages. X: total includes countries not included in AIAP survey - India, Sri Lanka, New Zealand. ▴ Adapted from Aït-Khaled et al. [10]. See text for questions. +: in 13-14 year olds. *See Ref 12: response to question: "during the worst month period last year did you have red, itchy eyes or watery eyes". Answers include those who had symptoms from a few days to every day per week. †Adult populations >18 years.
Within Asian Pacific countries, significant variation in prevalence was noted for different centres, for example, 1% in Davangere, India to 24.4% in Ho Chi Minh City Vietnam. Furthermore, large variations in prevalence were seen between centres in the same country. In Thailand, rates varied between 9.1% and 23.9% and in India between 1% and 23.6% [10].
AIAP study
More recently a very different survey has been conducted in a number of Asia Pacific countries. Known as the "Allergies in Asia Pacific", this survey was initiated and funded by a pharmaceutical company, Nycomed, and parallels similar, published surveys conducted in North America and Latin America. A regional advisory board of experts met to supervise the study, devise and adapt the questionnaire and after completion, to examine and interpret findings. Details of the methodology used have been published [12].
In brief, telephone and in-person interviewing were utilised depending on the most appropriate mode of screening and interviewing in a particular country. Most of the interviews were conducted in urban areas due to the low telephone penetration and lack of interviewing infrastructure in rural Asia-Pacific. Persons appropriate for inclusion were individuals 4 years and older residing in Australia, China, Hong Kong, Korea, Malaysia, Singapore, Taiwan, Vietnam and the Philippines. Individuals must have reported currently experiencing or being treated for nasal allergies (the generic term used for AR, ARC, hay fever, "sinus") and having been diagnosed by a physician as having the condition. Field-work was conducted between December 2009 and January 2010. The survey was developed and conducted by ABT SRBI, an international survey research organisation.
A total of 243 interviews were completed with parents of AR sufferers 4-17 years of age and a total of 1,292 interviews were completed with adults with AR across the nine countries for 33,986 households screened.
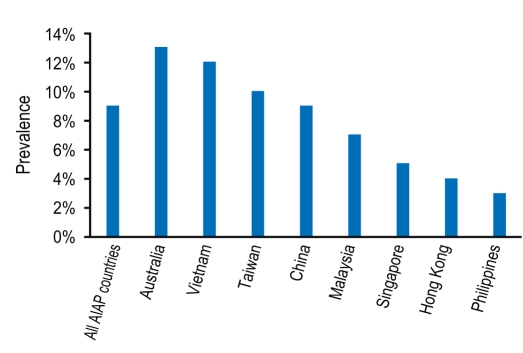
The AIAP survey found that 8.7% of respondents across eight Asia Pacific countries surveyed had a physician diagnosis of AR, nasal allergies, sinus disease or hay fever (Fig. 1). Korea was not included in this prevalence analysis as survey participants were obtained from physician referral and not household screening. The prevalence ranged from 2.5% in the Philippines to 13.2% in Australia (Fig. 1).
Fig. 1.
Allergies in Asia Pacific (AIAP) survey prevalence data for "doctor diagnosis of ARC". Adapted from Ref 12.
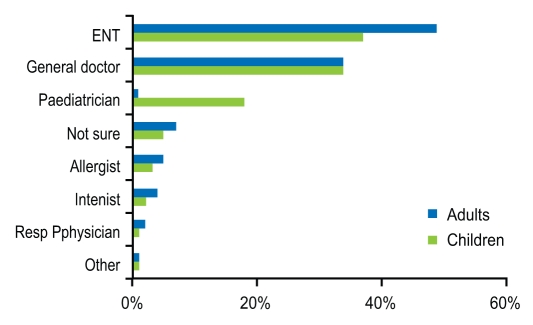
The majority of survey respondents reported having been diagnosed with AR by an otolaryngologist (49%) or general practice physician (34%) and rarely by an allergist (Fig. 2).
Fig. 2.
Doctor most likely to diagnose allergic rhinoconjunctivitis in Asia Pacific region. Adapted from Ref 12.
Asia Pacific surveys - individual countries
There are few published, comprehensive individual country studies that examine the prevalence of AC in the AP region that are accessible in English language journals.
Yadav et al. [14] have published data on symptom profiles of AR patients attending an ENT clinic in Haryana, India over a 12 month period. Of all patients attending the ENT department over a year, 3% (1,075) had a diagnosis of AR; males were more affected 62%. Conjunctival symptoms were present in 42.5%.
A study of the prevalence of ARC has been conducted in a population of 2,693 university students in Northern Thailand. For this survey, Uthaisangsook [15] used the ISAAC Phase 1 questionnaire including a question on the prevalence of nasal symptoms together with eye symptoms. This was a young adult population (17-53 years; mean age 20 ± 3.2 years) in whom a history of rhinitis with conjunctivitis occurred in 25.6% of individuals over the past 12 months.
In Korea, Lee et al. [16] examined the national prevalence of allergic diseases in 42,886 schoolchildren in two age groups, 6-12 years and 12-15 years. They took the ISAAC Phase 1 questionnaire, translated it to Korean and added more questions specifically on AC but also on drug and food allergy. Overall, in the 6-12 year olds, 11.2% had eye symptoms in the last 12 months with 7% having treatment in last 12 months. In the older group, 17.8% had ocular symptoms in the past 12 months with 3.6% having treatment. Approximately 10% in both age groups stated that they had ARC in the last 12 months, suggesting that further questions are necessary to detect those who may have AC alone without nasal symptoms.
Another Korean study of over 70,000 attendees at ENT clinics of 23 tertiary referral centres in 1999/2000 revealed a prevalence of perennial ARC of 3.39% [17]. This study does not specifically address prevalence of AC in its own right.
Baig et al. [18] determined the prevalence of AC among Karachi schoolchildren age 5-19 years in a study conducted in 2008. This cross sectional study involved ophthalmological assessment using a slit lamp. Criteria for diagnosis of AC included papillae in the upper tarsal conjunctiva, redness of eye and presence or history of itching and burning. A total of 818 children were examined; 19.2% had AC. Boys were more affected and increasing age was significantly associated with the diagnosis.
Choi & Lee [19] reported on the characteristics of a highly selected group of patients presenting to a corneal clinic in Singapore. They undertook a retrospective review of 33 patients presenting to National University Hospital corneal subspecialist clinic between 2005 and 2006. 88% of these patients had corneal erosions and twelve had a corneal defect or shield ulcer. There was a male predominance (76%); 51% had concomitant AR; 48% had asthma and 51% had AD. Only a minority (27%) could name precipitating factors for symptoms and 66% stated symptoms were perennial. These features suggest that most of the survey population represented the more severe end of the spectrum of AC such as VKC.
In India Gaur et al. [20] examined prevalence of AR in adults living in Delhi. A total of 5,900 adult subjects were surveyed using a questionnaire. The prevalence of AR in this adult population was calculated as 11.7%.
In a fascinating study from Japan, Mimura and colleagues [21] have demonstrated that patients with SAC are more myopic than healthy individuals. Myopic eyes have a longer axial eye length and wider palpebral fissures and this may allow more conjunctival allergen exposure.
Unmet needs
There have been no rigorously designed surveys in the Asia Pacific region that address the specific condition of ocular allergy in its various forms. Surveys such as ISAAC have been predominantly concerned with respiratory allergic symptoms with questions added that incorporate some ocular symptoms. These questionnaires do not detect individuals who may have AC in the absence of AR. Using hospital ophthalmology outpatient populations for prevalence studies of ocular allergy immediately introduces a bias towards the more severe, complex forms of the condition as patients with the milder forms of SAR and PAR will rarely present to a hospital outpatient clinic. There is a real need for the development of validated questionnaires specifically addressing ocular allergy. Furthermore, as detailed above, red, itchy eyes as a symptom complex may be experienced in other ocular conditions so some objective measure of allergy must be incorporated in order to differentiate the various ocular conditions. Finally, there are no widely accessible studies examining prevalence of the complex forms of ocular allergy (AKC, VKC) in the region.
The AIAP survey indicated that in the Asia Pacific region, diagnosis of ARC is most often made by an ENT specialist or a general practitioner [12]. Educational programmes regarding diagnosis, management and need for ophthalmology referral, of all forms of AC must target these medical practitioners as well as Allergists/Immunologists, to ensure that all patients with ocular allergy receive correct therapy.
References
- 1.Nathan RA, Meltzer EO, Selner JC, Storms W. Prevalence of allergic rhinitis in the United States. J Allergy Clin Immunol. 1997;99:S808–S814. [PubMed] [Google Scholar]
- 2.Hesselmar B, Aberg B, Eriksson B, Aberg N. Allergic rhinoconjunctivitis, eczema, and sensitization in two areas with differing climates. Pediatr Allergy Immunol. 2001;12:208–215. doi: 10.1034/j.1399-3038.2001.012004208.x. [DOI] [PubMed] [Google Scholar]
- 3.Riedi CA, Rosario NA. Prevalence of allergic conjunctivitis: a missed opportunity? Allergy. 2010;65:131–132. doi: 10.1111/j.1398-9995.2009.02100.x. [DOI] [PubMed] [Google Scholar]
- 4.Granet D. Allergic rhinoconjunctivitis and differential diagnosis of the red eye. Allergy Asthma Proc. 2008;29:565–574. doi: 10.2500/aap.2008.29.3170. [DOI] [PubMed] [Google Scholar]
- 5.Blaiss MS. Allergic rhinoconjunctivitis: burden of disease. Allergy Asthma Proc. 2007;28:393–397. doi: 10.2500/aap.2007.28.3013. [DOI] [PubMed] [Google Scholar]
- 6.Katelaris CH. Ocular allergy: implications for the clinical immunologist. Ann Allergy Asthma Immunol. 2003;90:23–27. doi: 10.1016/s1081-1206(10)61656-0. [DOI] [PubMed] [Google Scholar]
- 7.Jun J, Bielory L, Raizman MB. Vernal conjunctivitis. Immunol Allergy Clin North Am. 2008;28:59–82. doi: 10.1016/j.iac.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 8.Kumar S. Vernal keratoconjunctivitis: a major review. Acta Ophthalmol. 2009;87:133–147. doi: 10.1111/j.1755-3768.2008.01347.x. [DOI] [PubMed] [Google Scholar]
- 9.Bielory B, Bielory L. Atopic dermatitis and keratoconjunctivitis. Immunol Allergy Clin North Am. 2010;30:323–336. doi: 10.1016/j.iac.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 10.Aït-Khaled N, Pearce N, Anderson HR, Ellwood P, Montefort S, Shah J. Global map of the prevalence of symptoms of rhinoconjunctivitis in children: The International Study of Asthma and Allergies in Childhood (ISAAC) Phase Three. Allergy. 2009;64:123–148. doi: 10.1111/j.1398-9995.2008.01884.x. [DOI] [PubMed] [Google Scholar]
- 11.Fok AO, Wong GW. What have we learnt from ISAAC phase III in the Asia-Pacific rim? Curr Opin Allergy Clin Immunol. 2009;9:116–122. doi: 10.1097/aci.0b013e3283292256. [DOI] [PubMed] [Google Scholar]
- 12.Katelaris CH, Lai CK, Rhee CS, Lee SH, Yun WD, Lim-Varona L, Quang VT, Hwang J, Singh H, Kim J, Boyle JM, Dhong HJ, Narayanan P, Vicente G, Blaiss M, Sacks R. Nasal allergies in the Asian-Pacific population: Results from the Allergies in Asia-Pacific Survey. Am J Rhinol Allergy. 2011;25:S3–S15. doi: 10.2500/ajra.2011.25.3674. [DOI] [PubMed] [Google Scholar]
- 13.Kilpeläinen M, Terho EO, Helenius H, Koskenvuo M. Validation of a new questionnaire on asthma, allergic rhinitis, and conjunctivitis in young adults. Allergy. 2001;56:377–384. doi: 10.1034/j.1398-9995.2001.056005377.x. [DOI] [PubMed] [Google Scholar]
- 14.Yadav SP, Goel HC, Chanda R, Ranga R, Gupta KB. A clinical profile of allergic rhinitis in Haryana. Indian J Allergy Asthma Immunol. 2001;15:13–15. [Google Scholar]
- 15.Uthaisangsook S. Prevalence of asthma, rhinitis, and eczema in the university population of Phitsanulok, Thailand. Asian Pac J Allergy Immunol. 2007;25:127–132. [PubMed] [Google Scholar]
- 16.Lee SI, Shin MH, Lee HB, Lee JS, Son BK, Koh YY, Kim KE, Ahn YO. Prevalences of symptoms of asthma and other allergic diseases in Korean children: a nationwide questionnaire survey. J Korean Med Sci. 2001;16:155–164. doi: 10.3346/jkms.2001.16.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Min YG. The pathophysiology, diagnosis and treatment of allergic rhinitis. Allergy Asthma Immunol Res. 2010;2:65–76. doi: 10.4168/aair.2010.2.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baig R, Ali AW, Ali T, Ali A, Shah MN, Sarfaraz A, Ahmad K. Prevalence of allergic conjunctivitis in school children of Karachi. J Pak Med Assoc. 2010;60:371–373. [PubMed] [Google Scholar]
- 19.Choi H, Lee SB. Nonseasonal allergic conjunctivitis in the tropics: experience in a tertiary care institution. Ocul Immunol Inflamm. 2008;16:141–145. doi: 10.1080/09273940802184182. [DOI] [PubMed] [Google Scholar]
- 20.Gaur SN, Gupta K, Rajpal S, Singh AB, Rohatgi A. Prevalence of bronchial asthma and allergic rhinitis among urban and rural adult population of Delhi. Indian J Allergy Asthma Immunol. 2006;20:90–97. [Google Scholar]
- 21.Mimura T, Mimura Y, Arimoto A, Amano S, Yamagami S, Funatsu H, Usui T, Noma H, Honda N, Okamoto S. Relationship between refraction and allergic conjunctivitis. Eye (Lond) 2009;23:63–66. doi: 10.1038/sj.eye.6702999. [DOI] [PubMed] [Google Scholar]