Abstract
Most of Tarlov or perineurial cysts remain asymptomatic throughout the patient's life. The pathogenesis is still unclear. Hemorrhage has been suggested as one of the possible causes and trauma with resultant hemorrhage into subarachnoid space has been suggested as an origin of these cysts. However, Tarlov cysts related to spontaneous subarachnoid hemorrhage has not been reported. The authors report a case of Tarlov cyst which was symptomatic following spontaneous subarachnoid hemorrhage.
Keywords: Tarlov cyst, Spontaneous subarachnoid hemorrhage, Aneurysm rupture
INTRODUCTION
Tarlov or perineurial cysts were first described by Tarlov in 1938 as an incidental finding during autopsy studies of the filum terminale. The cysts arise at the junction of the dorsal root ganglion and the posterior nerve root and develop between the endoneurium and perineurium and are most often found in the sacral region2,12). The prevalence of perineurial cysts has been reported in 9% of autopsy specimens before the magnetic resonance (MR) era and estimated to be approximately 1.5-4.6% in large series using MR images4,9,10). Although cases of Tarlov cysts causing coccydynia, sacral pain, sacral radiculopathies, and sacral insufficiency fractures have been reported, most Tarlov cysts remain asymptomatic throughout the patient's life1,4). Most of the cysts are found incidentally during computed tomography (CT) or MR imaging for other reasons and 13-22% of the patients with the cysts had symptoms4,9).
Why some of the Tarlov cysts progress to cause symptoms is unclear. These cysts may become symptomatic by local compression of adjacent bone or displacing nerve roots, if they become large1,4). Hemorrhage has been suggested as one of the possible causes of these cysts and trauma with resultant hemorrhage into the subarachnoid space has been suggested as an origin of these cysts6,7,12). However, symptomatic Tarlov cysts related to spontaneous SAH have not been reported. We report a case of symptomatic Tarlov cyst following spontaneously ruptured aneurysmal SAH.
CASE REPORT
A 75-year-old woman was transferred to the emergency room, complaining of severe headache of sudden onset, low back pain, nausea, and dizziness. She was alert and oriented. She had signs of meningeal irritation, but the neurological examination was otherwise normal. Brain CT revealed SAH in the right Sylvian fissure and basal cistern. Three-dimensional brain CT angiography showed a right middle cerebral artery aneurysm. Emergent craniotomy via right-sided pterional approach without installation of lumbar cerebrospinal fluid (CSF) drain and neck clipping of the aneurysm was performed uneventfully under general anesthesia.
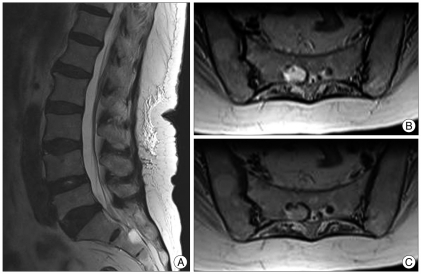
Following operation, she complained of worsening pain in the lumbosacral, buttock, and the posterior aspect of the right thigh. The pain was intermittent at onset and exacerbated by sitting, walking, and coughing. Bed rest relieved the pain. She had no history of previous back problems, or recent trauma. On neurological examination, no abnormal findings were found. Lumbar spine MR images 2 weeks postoperatively showed a 15×15×16 mm Tarlov cyst at the S2 level affecting the right S2 root with high signal intensity in T2 and T1 images, suggestive of bleeding within the cyst and a so-called "dark disc" at multilevel lumbar spines (Fig. 1). She suffered from pain despite analgesics and physical therapy for 2 weeks after MR imaging.
Fig. 1.
Magnetic resonance images of the lumbar spine. A : T2-weighted sagittal image shows Tarlov cyst at the S2 level and multilevel disk degeneration. B : T2-weighted axial image at the S2 level shows 15×15×16 mm-sized Tarlov cyst affecting the right S2 root with high signal intensity and bony erosion. C : T1-weighted axial image at the S2 level shows Tarlov cyst with high signal intensity.
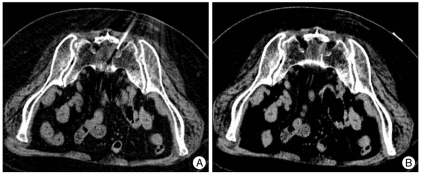
CT-guided aspiration of the cyst was performed and approximately 1 cc of old blood was aspirated (Fig. 2). Her pain was relieved immediately after aspiration and she had only mild discomfort for 8 months.
Fig. 2.
Computed tomography-guided aspiration of the Tarlov cyst. A : Needle tip is positioned within the cyst during the aspiration. B : Post-aspiration computed tomography shows decreased cyst size and air within the cyst.
DISCUSSION
The pathogenesis of Tarlov cysts remains unclear, although several hypotheses have been suggested including inflammation within the nerve root cysts followed by inoculation of fluid, developmental or congenital origin, arachnoidal proliferation along and around the existing sacral nerve root, and ischemic degeneration2,8,9,12). Hemorrhage into the subarachnoid space has also been suggested. It is theorized that such hemorrhage would cause accumulation of red blood cells which impairs drainage of the veins in the perineurium and epineurium. This impaired drainage of venous blood from the perineurium and epineurium results in rupture of these veins and subsequent cyst formation5,9,12). Posttraumatic causes of cyst formation have been reported and some authors report that approximately 40% to 60% of the patients have history of antecedent trauma7,11,12). Voyadzis et al.12) reported evidence of old hemorrhage in the form of hemosiderin deposits was present in four of eight cases studied and two cases had foci of dystrophic calcification within the cyst wall, suggestive of previous trauma and/or chronicity. But, we have not found any reports on Tarlov cysts originating from non-traumatic SAH in the extant literature.
Most Tarlov cysts remain asymptomatic throughout the patient's life1,4). The reasons why some of the Tarlov cysts cause symptoms are uncertain. A ball-valve mechanism has been postulated as expansion of the cyst causing symptoms and it has been hypothesized that the cyst neck serves as a valve. Regardless of the underlying cause, the ultimate mechanism of cyst formation is stenosis of the ostium of the nerve root sheath. CSF is able to flow into the cysts with arterial pulsation, but outflow is restricted because of a ball-valve mechanism4,9). The cysts can enlarge with time by the hydrostatic and pulsatile forces of CSF and local nerve root or periosteal compression. This could cause pain or radicular symptom. Intermittent and worsening pain when standing or walking might also be derived from a ball-valve mechanism. According to the systolic pulsation and a patient's postural changes, CSF enters the cyst but cannot exit. When the cyst fills, pain occurs; when the cyst deflates, pain is relieved5).
In the present patient, SAH was not the origin of the Tarlov cyst because the pain began shortly after the occurrence of SAH. However, the increased hydrostatic pressure of CSF during or after aneurysmal rupture could introduce the CSF and SAH into the pre-existing Tarlov cyst, and was considered to cause rapid expansion of the cyst resulting in lumbosacral pain. The old blood aspirated in our patient could be evidence of the ball-valve mechanism in the cyst expansion. Voyadzis et al.12) reported a patient who had marked worsening of symptoms after percutaneous aspiration of the Tarlov cyst and suggested this deterioration may have been the result of hemorrhage of the cyst wall. Another possible mechanism that causes lumbosacral pain is that hemorrhage or hematoma can also irritate S2 nerve roots, causing pain. Lam reported transient radicular irritation by SAH after spinal anesthesia and he stated the haematoma displaced and irritated the lumbosacral nerve roots, causing the symptoms3). In our patient, hemorrhage infiltrated from the subarachnoid space during or after aneurysmal rupture is presumed to be the cause of not only the expansion of the pre-existing cyst but the irritation or stretching of the nerve root leading to pain. Although another finding including degeneration of disks in the MR images or hemorrhage in the spinal subarachnoid space could be the source of pain, immediate relief of the pain after aspiration of the cyst suggested a causal relationship between the Tarlov cyst and pain.
Although many treatment options have been reported and discussed in the literature, such as anti-inflammatory medications, permanent CSF drainage as provided by lumboperitoneal shunt, cyst-arachnoidal shunt, CT-guided method for percutaneous drainage, CT-guided infusion of fibrin glue, simple decompressive laminectomy, excision of the cysts, and microsurgical cyst fenestration and imbrications, there has been a great deal of controversy regarding the efficacy or complications2,4,9,12). The effectiveness of percutaneous drainage is also a debatable issue. Voyadzis et al.12) did not recommend percutaneous aspiration of the Tarlov cyst because of the high rate of recurrence of symptoms and low rate of improvement. Others have recommended it should be used prior to considering open surgical decompression because surgical decompression is both technically demanding and implicates high risk4,9). In our patient, although a longer conservative treatment might have relieved the pain, failure of the conservative treatment led us to CT-guided aspiration of the cyst without the need for general anesthesia and longer time of the procedure. We achieved successful results, at least in relatively short period of time. Close observation for the recurrence of symptoms should be taken into major concern.
CONCLUSION
Hemorrhage from the subarachnoid space, including spontaneous aneurysmal SAH, could be the source of development of pain from asymptomatic Tarlov cysts. CT-guided aspiration could be one of the treatment options for symptomatic Tarlov cysts.
References
- 1.Acosta FL, Jr, Quinones-Hinojosa A, Schmidt MH, Weinstein PR. Diagnosis and management of sacral Tarlov cysts. Case report and review of the literature. Neurosurg Focus. 2003;15:E15. doi: 10.3171/foc.2003.15.2.15. [DOI] [PubMed] [Google Scholar]
- 2.Guo D, Shu K, Chen R, Ke C, Zhu Y, Lei T. Microsurgical treatment of symptomatic sacral perineurial cysts. Neurosurgery. 2007;60:1059–1065. doi: 10.1227/01.NEU.0000255457.12978.78. discussion 1065-1066. [DOI] [PubMed] [Google Scholar]
- 3.Lam DH. Subarachnoid haematoma after spinal anaesthesia mimicking transient radicular irritation : a case report and review. Anaesthesia. 2008;63:423–427. doi: 10.1111/j.1365-2044.2007.05368.x. [DOI] [PubMed] [Google Scholar]
- 4.Langdown AJ, Grundy JR, Birch NC. The clinical relevance of Tarlov cysts. J Spinal Disord Tech. 2005;18:29–33. doi: 10.1097/01.bsd.0000133495.78245.71. [DOI] [PubMed] [Google Scholar]
- 5.Mummaneni PV, Pitts LH, McCormack BM, Corroo JM, Weinstein PR. Microsurgical treatment of symptomatic Tarlov cysts. Neurosurgery. 2000;47:74–78. doi: 10.1097/00006123-200007000-00016. discussion 78-79. [DOI] [PubMed] [Google Scholar]
- 6.Nadler SF, Bartoli LM, Stitik TP, Chen B. Tarlov cyst as a rare cause of S1 radiculopathy : a case report. Arch Phys Med Rehabil. 2001;82:689–690. doi: 10.1053/apmr.2001.22353. [DOI] [PubMed] [Google Scholar]
- 7.Nishiura I, Koyama T, Handa J. Intrasacral perineurial cyst. Surg Neurol. 1985;23:265–269. doi: 10.1016/0090-3019(85)90093-x. [DOI] [PubMed] [Google Scholar]
- 8.Park HJ, Kim IS, Lee SW, Son BC. Two cases of symptomatic perineural cysts (Tarlov cysts) in one family : a case report. J Korean Neurosurg Soc. 2008;44:174–177. doi: 10.3340/jkns.2008.44.3.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paulsen RD, Call GA, Murtagh FR. Prevalence and percutaneous drainage of cysts of the sacral nerve root sheath (Tarlov cysts) AJNR Am J Neuroradiol. 1994;15:293–297. discussion 298-299. [PMC free article] [PubMed] [Google Scholar]
- 10.Smith DT. Cystic formations associated with human spinal nerve roots. J Neurosurg. 1961;18:654–660. [Google Scholar]
- 11.Tarlov IM. Spinal perineurial and meningeal cysts. J Neurol Neurosurg Psychiatry. 1970;33:833–843. doi: 10.1136/jnnp.33.6.833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Voyadzis JM, Bhargava P, Henderson FC. Tarlov cysts : a study of 10 cases with review of the literature. J Neurosurg. 2001;95:25–32. doi: 10.3171/spi.2001.95.1.0025. [DOI] [PubMed] [Google Scholar]