Abstract
Spinal epidural lipomatosis (SEL) is an overgrowth of the normally encapsulated adipose tissue in the epidural space around the spinal cord in the thoracic and lumbar spine causing compression of the neural components. Idiopathic SEL in non-obese patients is exceptional. Idiopathic SEL can result in thoracic myelopathy and lumbar radiculopathy. A thoracic radiculopathy due to idiopathic SEL has not been reported yet. We report a case of idiopathic SEL with intractable chest pain and paresthesia. We suggest that idiopathic SEL should be considered as a cause of chest pain.
Keywords: Spinal, Idiopathic, Epidural, Lipomatosis, Thoracic, Chest pain
INTRODUCTION
Spinal epidural lipomatosis (SEL) is an overgrowth of the normally encapsulated adipose tissue in the epidural space around the spinal cord in the thoracic and lumbar spine causing compression of the neural components5,12,13,25,26,32,34). In cases without definite predisposing factors, the term 'idiopathic SEL' has been used. Idiopathic SEL in non-obese patients is exceptional3,12,13,26).
According to previous reports, idiopathic SEL can result in thoracic myelopathy and lumbar radiculopathy2,4,8,9,13,19). To our knowledge, a thoracic radiculopathy due to idiopathic SEL has not been reported yet.
We report a case of chest pain caused by idiopathic thoracic SEL in a female patient who did not have any other recognized predisposing factors for this condition.
CASE REPORT
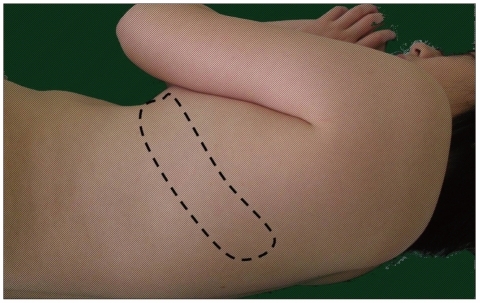
A 16-year-old girl presented with a 2-month history of pain on her left chest. She reported that the pain spontaneously started around 2 months prior to admission and got worse over the two weeks. She could not do her usual daily living activities due to the intractable pain. She had no medical history for diabetes or steroid intake. On physical examination, her body weight was 55 kg and height was 155 cm, her body mass index was 22.8 kg/m2 which was within the normal range. Neurologic examination revealed paresthesia on the left side, at the level of the T5 and T6 dermatomes, without myelopathy, motor weakness or claudication (Fig. 1). Hyperesthesia and allodynia were not evident. Laboratory evaluation, including full blood count, electrolytes, creatinine, liver function test, vitamin B12 and folate, urine analysis and culture, thyroid function tests, adrenocorticotropic hormone, and cortisol, were all unremarkable.
Fig. 1.
Photograph of patient in a lateral decubitus position showing left T5 and T6 dermatomes (dotted line) where she had the intractable pain with paresthesia.
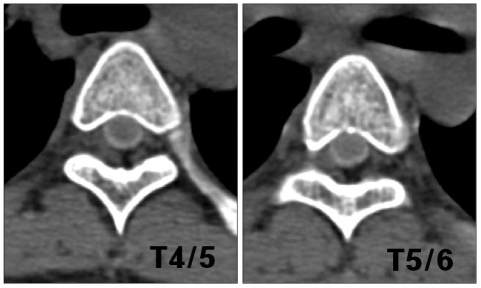
Plain radiographs of the thoracic spine showed no abnormalities. Myelography computed tomography (CT) demonstrated a hypodense soft tissue mass within the posterior spinal canal and mainly in left vertebral foramen on T4/5 and 5/6 level (Fig. 2).
Fig. 2.
Myelography computerized tomography (CT) demonstrating a hypodense soft tissue mass in the posterior spinal canal and mainly in the left vertebral foramen on T4/5 and T5/6 level.
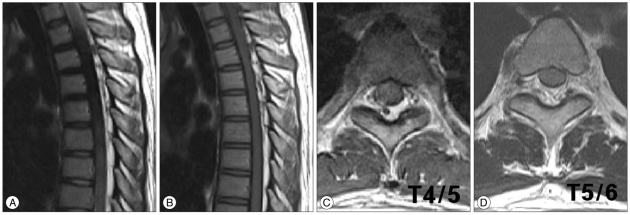
Magnetic resonance image (MRI) of the thoracic region presented a posterior compressing mass lesion of increased signal intensity on T1-weighted image (WI) and T2 WI in the epidural space, suggesting an epidural lipomatosis in the thoracic area. An extensive epidural fat deposition was about 6 mm in thickness, extended from T3 to T9 causing anterior displacement of the spinal cord and root compression in the left vertebral foramen on T4/5 and T5/6 levels (Fig. 3).
Fig. 3.
Thoracic spinal magnetic resonance imaging; Sagittal T2-WI (A), sagittal T1-WI (B), T4/5 axial T2-WI (C) and T5/6 axial T2-WI (D), showing a posterior epidural mass with mild compression of the dura extending from T3 to T9 segments with high signal intensity at T2-WI (A) and T1-WI (B) similar to that of subcutaneous adipose tissues. This epidural mass is extending into the left vertebral foramen on thoracic 4/5 (C), and T5/6 (D) levels. WI : weighted image.
The patient's pain was refractory to medication. We did a diagnostic root block at the left vertebral foramina of T4/5 and T5/6 level. Her pain improved for about three hours but recurred. The presumptive diagnosis was a radiculopathy of left T5 and 6 nerve root due to SEL.
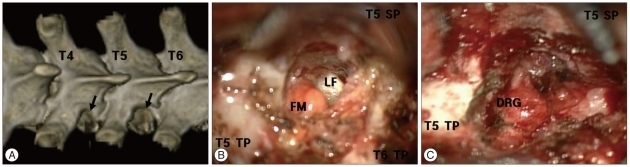
An operation for the chest pain with paresthesia was decided. We performed a lateral partial facetectomy and fat debulking on the left side of T4/5 and T5/6 levels (Fig. 4A). During the operation, a fatty mass crowded out of the vertebral foramen after removal of the ligament flavum (Fig. 4B). It appeared as fat tissue severely compressing the dorsal root ganglion (DRG). The compression was more remarkable at the T5/6 than T4/5 level. The fat tissue compressing the nerve root and DRG was removed (Fig. 4C).
Fig. 4.
Postoperative 3D computerized tomography (A) and intra-operative photos (B and C). A : Lateral facetectomy was done at the left side of T4/5 and T5/6 levels. B : A fatty mass bulging out of the vertebral foramen after removal of LF. C : DRG has been decompressed after removal of surrounding fatty tissue. T5 TP : T5 transverse process, T6 TP : T6 transverse process, T6 SP : T6 spinous process, LF : ligament flavum, DRG : dorsal root ganglion, T4 : T4 vertebra, T5 : T5 vertebra, T6 : T6 vertebra.
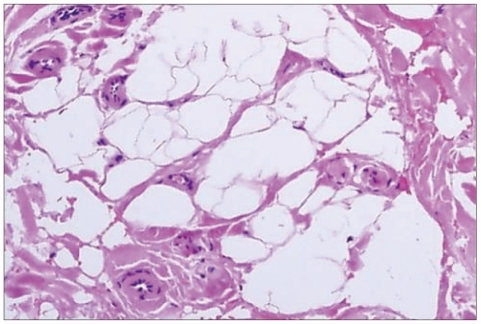
Histopathological examination postoperatively demonstrated nodular proliferation of mature fat cells, consistent with lipomatosis (Fig. 5). The patient's intractable chest pain resolved completely and the paresthesia disappeared immediately. The patient was discharged by the 8th postoperative day. The patient had no recurrence of symptoms at 2 years after the operation.
Fig. 5.
Histopathological examination demonstrates nodular proliferation of mature fat cells, consistent with lipomatosis (H&E ×200).
DISCUSSION
SEL is a condition wherein excess adipose tissue deposits around the thecal sac causing compression of neural structures2,3,5,7,8,12,17,18,24,31,32). In 1975, Lee et al.18) reported the first case of symptomatic epidural cord compression secondary to SEL. It is well known that the main etiological factors of SEL are associated with endocrine dysfunction such as Cushing disease, hypothyroidism, obesity, iatrogenic steroid treatment for immune disorders, COPD and transplantation9,11,20,27). In approximately 75% of SEL, this may be secondary to exogenous steroid administration for systemic diseases such as rheumatoid arthritis, systemic lupus erythematous, dermatomyositis, chronic obstructive pulmonary disease, or following organ transplantation27). Obesity is the second most common associated category of SEL5,9,11).
Idiopathic SEL was first reported by Badami and Hinck3) in 1982. Haddad, et al.12) first hypothesized that idiopathic SEL was a byproduct of obesity, with the gradual overgrowth of epidural fat resulting in compression of the spinal cord and nerves. Thereafter, several researchers asserted that the term 'idiopathic' should be used solely to characterize cases of SEL that develop in non-obese patients, who were not receiving corticosteroid therapy, and without any other underlying SEL-related disease such as hypothyroidism or endogenous corticosteroid production4,6,9,19). About 16 cases of idiopathic SEL in non-obese patients were reported previously1,9). The underlying pathological mechanism of SEL is still unknown.
Our patient was neither receiving steroids nor had any kind of endocrinopathy. Moreover, she was not obese. For this reason, we had difficulty diagnosing idiopathic SEL as the cause of chest pain.
The majority of idiopathic SEL involve the mid-thoracic and lower lumbar vertebral levels, representing two peaks9,15). SEL causing neurological deficits occurs more frequently in the thoracic than the lumbar spine17,23). Patients may present with progressive and long standing complaints of pain, weakness, numbness, incontinence, ataxia, abnormal reflexes and rarely paralysis. According to Al-Khawaja et al.2), patients with idiopathic SEL involving the thoracic segments had myelopathy in 70% and paraplegia in 5% of patients. All of these symptoms were induced by compression of the spinal cord. In cases of lumbar SEL, symptoms associated with lumbar radiculopathy were reported but thoracic radiculopathy has not been reported1,4,8,9,30,34).
The mechanism of SEL induced neurologic symptom is mainly by direct compression of the adjacent nervous structures and epidural blood vessels resulting in venous engorgement which then compromise contribute to the evolution of myelopathic and radicular complaints1,30). We identified the direct compression by the lipomatous tissue and with venous engorgement around the DRG during the operation and believed that these findings induced the radiculopathy with intractable chest pain and paresthesia. The DRG is exquisitely sensitive to direct pressure and can generate prolonged neural discharges even after brief compression. The nerve root itself responds to this same stimulus only after it has become inflamed and sensitized14,33). These features of the DRG are thought to be the cause of intractable pain in our case.
Symptoms and signs associated with SEL can be caused by a variety of diseases. Disc disease, thoracic intradural extramedullary tumor like meningioma and intradural lesions, like ependymoma, astrocytoma, or a syrix were considered likely differentials prior to MRI30). Diagnosis is best based on MRI6,10,15). T1-WI differentiate epidural fat from dural content with a high degree of specificity and allow for measurement of adipose tissue thickness. Definite MRI finding of SEL is the pathognomonic appearance of fat on MRI; high signal intensity on T1-WI, intermediate signal intensity on T2-WI2,6,9,10,15). On CT scans, SEL presents as a homogenous hypodense epidural mass with a density between -80 and -160 HU24). Several grading system by MRI were reported but could not show correlation with clinical symptoms6,10,15,16,21). The mean sagittal thickness of the epidural fat in these studies was 4.6 mm with a normal range of 3 to 6 mm. In contrast, imaging in 6 patients with SEL revealed a mean thickness of 8 mm25).
MRI findings of our patient showed that the spinal cord was displaced anteriorly by a lipomatous tissue which was 6 mm in thickness and extended into the vertebral foramen around the DRG. We believe that the epidural fat with a 6 mm thickness was not enough to induced myelopathy.
The treatment of SEL ranges from conservative management to surgical excision. The treatment of SEL is a matter of debate, because many patients have been treated by simple weight reduction with good results7,22,24). However, this conservative treatment remains restricted to patients with mild neurological symptoms. Surgery is often necessary in cases wherein weight reduction failed to alleviate the symptoms or in severely symptomatic patients although the clinical suspicion for the presence of this particular neoplasia was not high4,15,19,26,28). A decompressive surgery with fat debulking should be considered when diet therapy proves unsuccessful or when the patient suffers acute neurological deterioration15). The prognosis of patients with idiopathic SEL after surgical management is favorable and no case of recurrence has been reported9).
Although our patient did not present with myelopathy, she was not able to do her usual activities and could not sleep well because of intractable chest pain which was not controlled by medications. We chose the operation for symptomatic relief and decompressed just lateral part of facet joint at symptomatic level minimally. The outcome of the operation was good and there was no recurrence for 2 years.
Whether the epidural fat shows histological alterations compared with normal fat remains unclear. Further studies should focus on the histological entity of epidural fat, given that hypervascularization and bleeding within the epidural fat could be a risk factor for symptomatic manifestation of extradural lipomatous tissue28,29,31). Our patient demonstrated irregular fibroadipose tissue, nodules of mature fat cells with venous engorgement on histopathological examination and no hypervascularization and bleeding. Also, we suggested that the main cause of our patient's symptom was the direct compression of the DRG by the lipomatous tissue.
CONCLUSION
We report a case of idiopathic SEL with intractable chest pain and paresthesia. We suggest that idiopathic SEL should be considered as a cause of chest pain.
References
- 1.Akhaddar A, Ennouali H, Gazzaz M, Naama O, Elmostarchid B, Boucetta M. Idiopathic spinal epidural lipomatosis without obesity : a case with relapsing and remitting course. Spinal Cord. 2008;46:243–244. doi: 10.1038/sj.sc.3102099. [DOI] [PubMed] [Google Scholar]
- 2.Al-Khawaja D, Seex K, Eslick GD. Spinal epidural lipomatosis--a brief review. J Clin Neurosci. 2008;15:1323–1326. doi: 10.1016/j.jocn.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 3.Badami JP, Hinck VC. Symptomatic deposition of epidural fat in a morbidly obese woman. AJNR Am J Neuroradiol. 1982;3:664–665. [PMC free article] [PubMed] [Google Scholar]
- 4.Bednar DA, Esses SI, Kucharczyk W. Symptomatic lumbar epidural lipomatosis in a normal male. A unique case report. Spine (Phila Pa 1976) 1990;15:52–53. doi: 10.1097/00007632-199001000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Bodelier AG, Groeneveld W, van der Linden AN, Haak HR. Symptomatic epidural lipomatosis in ectopic Cushing's syndrome. Eur J Endocrinol. 2004;151:765–769. doi: 10.1530/eje.0.1510765. [DOI] [PubMed] [Google Scholar]
- 6.Borré DG, Borré GE, Aude F, Palmieri GN. Lumbosacral epidural lipomatosis : MRI grading. Eur Radiol. 2003;13:1709–1721. doi: 10.1007/s00330-002-1716-4. [DOI] [PubMed] [Google Scholar]
- 7.Borstlap AC, van Rooij WJ, Sluzewski M, Leyten AC, Beute G. Reversibility of lumbar epidural lipomatosis in obese patients after weight-reduction diet. Neuroradiology. 1995;37:670–673. doi: 10.1007/BF00593392. [DOI] [PubMed] [Google Scholar]
- 8.Fassett DR, Schmidt MH. Spinal epidural lipomatosis : a review of its causes and recommendations for treatment. Neurosurg Focus. 2004;16:E11. [PubMed] [Google Scholar]
- 9.Fogel GR, Cunningham PY, 3rd, Esses SI. Spinal epidural lipomatosis : case reports, literature review and meta-analysis. Spine J. 2005;5:202–211. doi: 10.1016/j.spinee.2004.05.252. [DOI] [PubMed] [Google Scholar]
- 10.Geers C, Lecouvet FE, Behets C, Malghem J, Cosnard G, Lengelé BG. Polygonal deformation of the dural sac in lumbar epidural lipomatosis : anatomic explanation by the presence of meningovertebral ligaments. AJNR Am J Neuroradiol. 2003;24:1276–1282. [PMC free article] [PubMed] [Google Scholar]
- 11.Gupta R, Kumar AN, Gupta V, Madhavan SM, Sharma SK. An unusual cause of paraparesis in a patient on chronic steroid therapy. J Spinal Cord Med. 2007;30:67–69. doi: 10.1080/10790268.2007.11753916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haddad SF, Hitchon PW, Godersky JC. Idiopathic and glucocorticoid-induced spinal epidural lipomatosis. J Neurosurg. 1991;74:38–42. doi: 10.3171/jns.1991.74.1.0038. [DOI] [PubMed] [Google Scholar]
- 13.Han YM, Ahn MS. Idiopathic spinal epidural lipomatosis. J Korean Neurosurg Soc. 2001;30:795–799. [Google Scholar]
- 14.Howe JF, Loeser JD, Calvin WH. Mechanosensitivity of dorsal root ganglia and chronically injured axons : a physiological basis for the radicular pain of nerve root compression. Pain. 1977;3:25–41. doi: 10.1016/0304-3959(77)90033-1. [DOI] [PubMed] [Google Scholar]
- 15.Ishikawa Y, Shimada Y, Miyakoshi N, Suzuki T, Hongo M, Kasukawa Y, et al. Decompression of idiopathic lumbar epidural lipomatosis : diagnostic magnetic resonance imaging evaluation and review of the literature. J Neurosurg Spine. 2006;4:24–30. doi: 10.3171/spi.2006.4.1.24. [DOI] [PubMed] [Google Scholar]
- 16.Kuhn MJ, Youssef HT, Swan TL, Swenson LC. Lumbar epidural lipomatosis : the "Y" sign of thecal sac compression. Comput Med Imaging Graph. 1994;18:367–372. doi: 10.1016/0895-6111(94)90007-8. [DOI] [PubMed] [Google Scholar]
- 17.Kumar K, Nath RK, Nair CP, Tchang SP. Symptomatic epidural lipomatosis secondary to obesity. Case report. J Neurosurg. 1996;85:348–350. doi: 10.3171/jns.1996.85.2.0348. [DOI] [PubMed] [Google Scholar]
- 18.Lee M, Lekias J, Gubbay SS, Hurst PE. Spinal cord compression by extradural fat after renal transplantation. Med J Aust. 1975;1:201–203. doi: 10.5694/j.1326-5377.1975.tb111328.x. [DOI] [PubMed] [Google Scholar]
- 19.Lisai P, Doria C, Crissantu L, Meloni GB, Conti M, Achene A. Cauda equina syndrome secondary to idiopathic spinal epidural lipomatosis. Spine (Phila Pa 1976) 2001;26:307–309. doi: 10.1097/00007632-200102010-00017. [DOI] [PubMed] [Google Scholar]
- 20.Maillot F, Mulleman D, Mammou S, Goupille P, Valat JP. Is epidural lipomatosis associated with abnormality of body fat distribution? A case report. Eur Spine J. 2006;15:105–108. doi: 10.1007/s00586-005-0955-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Naka N, Matsuoka T, Yamamoto K, Mitsuhashi K, Kawano J. Lumbar epidural lipomatosis-morphological evaluation of epidural fat. Cent Jpn J Orthop Trauma. 1998;41:327–328. [Google Scholar]
- 22.Olsen LT, Tigyer LM, Antonacci MD. Management of cervicothoracic spinal lipomatosis and rapidly progressive neurologic symptoms. Orthopedics. 2006;29:727–730. doi: 10.3928/01477447-20060801-06. [DOI] [PubMed] [Google Scholar]
- 23.Payer M, Van Schaeybroeck P, Reverdin A, May D. Idiopathic symptomatic epidural lipomatosis of the lumbar spine. Acta Neurochir (Wien) 2003;145:315–320. doi: 10.1007/s00701-003-0001-x. discussion 321. [DOI] [PubMed] [Google Scholar]
- 24.Pouchot J, Si-Hassen C, Damade R, Bayeux MC, Mathieu A, Vinceneux P. Cauda equina compression by epidural lipomatosis in obesity. Effectiveness of weight reduction. J Rheumatol. 1995;22:1771–1775. [PubMed] [Google Scholar]
- 25.Quint DJ, Boulos RS, Sanders WP, Mehta BA, Patel SC, Tiel RL. Epidural lipomatosis. Radiology. 1988;169:485–490. doi: 10.1148/radiology.169.2.3174998. [DOI] [PubMed] [Google Scholar]
- 26.Robertson SC, Traynelis VC, Follett KA, Menezes AH. Idiopathic spinal epidural lipomatosis. Neurosurgery. 1997;41:68–74. doi: 10.1097/00006123-199707000-00015. discussion 74-75. [DOI] [PubMed] [Google Scholar]
- 27.Sabharwal S, Mahmood F. Thoracic spinal epidural lipomatosis associated with adolescent scoliosis. J Spinal Disord Tech. 2006;19:217–221. doi: 10.1097/01.bsd.0000179672.80229.0d. [DOI] [PubMed] [Google Scholar]
- 28.Sato M, Yamashita K, Aoki Y, Hiroshima K. Idiopathic spinal epidural lipomatosis. Case report and review of literature. Clin Orthop Relat Res. 1995:129–134. [PubMed] [Google Scholar]
- 29.Selmi F, Davies KG, Sharma RR, Redfern RM. Idiopathic spinal extradural lipomatosis in a non-obese otherwise healthy man. Br J Neurosurg. 1994;8:355–358. doi: 10.3109/02688699409029626. [DOI] [PubMed] [Google Scholar]
- 30.Shah JA, Flynn P, Choudhari KA. Idiopathic spinal epidural lipomatosis. Br J Neurosurg. 2005;19:265–267. doi: 10.1080/02688690500210086. [DOI] [PubMed] [Google Scholar]
- 31.Stambough JL, Cheeks ML, Keiper GL. Nonglucocorticoid-induced lumbar epidural lipomatosis : a case report and review of literature. J Spinal Disord. 1989;2:201–207. [PubMed] [Google Scholar]
- 32.Toshniwal PK, Glick RP. Spinal epidural lipomatosis : report of a case secondary to hypothyroidism and review of literature. J Neurol. 1987;234:172–176. doi: 10.1007/BF00314138. [DOI] [PubMed] [Google Scholar]
- 33.Wall PD, Devor M. Sensory afferent impulses originate from dorsal root ganglia as well as from the periphery in normal and nerve injured rats. Pain. 1983;17:321–339. doi: 10.1016/0304-3959(83)90164-1. [DOI] [PubMed] [Google Scholar]
- 34.Zevgaridis D, Nanassis K, Zaramboukas T. Lumbar nerve root compression due to extradural, intraforaminal lipoma. An underdiagnosed entity? J Neurosurg Spine. 2008;9:408–410. doi: 10.3171/SPI.2008.9.11.408. [DOI] [PubMed] [Google Scholar]