Abstract
The authors report a case of epidural and extraforaminal calcification caused by repetitive triamcinolone acetonide injections. A 66-year-old woman was admitted presenting with lower extremity weakness and radiating pain in her left leg. Ten months before admission, the patient was diagnosed as having an L4-5 spinal stenosis and underwent anterior lumbar interbody fusion followed by posterior fixation. Her symptoms had been sustained and she did not respond to transforaminal steroid injections. Repetitive injections (10 times) had been performed on the L4-5 level for six months. She had been taking bisphosphonate as an antiresorptive agent for ten months after surgery. Calcification in the ventral epidural and extraforaminal space was detected. The gritty particles were removed during decompressive surgery and these were proven to be a dystrophic calcification. The patient recovered from weakness and radiating leg pain. Repetitive triamcinolone acetonide injections after discectomy may be the cause of dystrophic calcification not only in the degenerated residual disc, but also in the posterior longitudinal ligament. Possible mechanisms may include the toxicity of preservatives and the insolubility of triamcinolone acetonide. We should consider that repetitive triamcinolone injections in the postdisectomy state may cause intraspinal ossification and calcification.
Keywords: Triamcinolone acetonide, Steroid injection, Epidural calcification, Dystrophic calcification
INTRODUCTION
Epidural calcification is rarely described as a cause of cauda equina syndrome in the lumbar spine. Calcification secondary to prior traumatic hematomas, meningioma or following intradiscal injection of triamcinolone hexacetonide has been previously reported6,7,12,18). However, we would like to report the first case of lumbar spinal canal ossification and calcification after decompressive surgery followed by repetitive triamcinolone acetonide (TA) injections and propose the pathogenesis.
CASE REPORT
A 66-year-old woman was admitted to our hospital with a one-month history of aggravated lower extremity weakness and radiating pain to the left buttock and posterior thigh. Ten months before admission, the patient was diagnosed as having an L4-5 spinal stenosis and underwent anterior lumbar interbody fusion via a retroperitoneal approach using a harvested iliac autograft followed by bilateral decompressive partial hemilaminectomies and posterior fixation in another clinic. Because of incomplete foraminal disectomy and decompression, her symptoms had been sustained and did not respond to non-steroidal anti-inflammatory drugs (NSAIDs) or multiple steroid injections via a transforaminal approach. TA injectable suspension was used each time. During the 3 months after the initial surgery, repetitive transforaminal steroid injections (10 times) had been performed on the L4-5 level within six months. She had been taking anti-osteoporotic medications (calcium and bisphosphonate) for ten months after surgery.
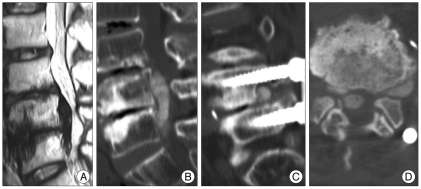
Neurologic examination revealed pain in the lateral calf of both legs and progressive weakness in the leg (knee extension Grade VI+/IV, ankle and big toe dorsiflexion Grade III/II, ankle plantar flexion IV+/IV+). Deep tendon reflexes were physiologic and the straight leg raising test was negative. No additional neurologic deficits were detected. The erythrocyte sedimentation rate and C-reactive protein were within normal limits. There was no evidence of hypercalcemia, hypophosphatemia, hyperparathyroidism, idiopathic tumoral calcinosis, end-stage renal disease, hypervitaminosis D, sarcoidosis, collagen vascular disease or parasitic disease. Preoperative magnetic resonance (MR) images demonstrated severe central stenosis and left extraforaminal disc herniation on the L4-5 level disc space (Fig. 1). T2-weighted images of the lumbar spine 10 months after the previous surgery showed a mass with dark signal intensity in the ventral epidural space on the L4 and L5 levels of the vertebral body and in the L4-5 extraforaminal space. The mass was mainly located in the ventral epidural space along the posterior longitudinal ligament. A computed tomography (CT) scan showed calcification in the same sites. The calcification in the ventral epidural space was not fused with, but abutting onto, the posterior vertebral cortical bone (Fig. 2B, C, D). The authors inferred from the radiologic findings that the preoperative L4-5 extraforaminal disc was converted into degenerated materials with calcification. Also, we could not detect the iliac tricortical graft that had been inserted into the L4-5 disc space in previous surgery on the CT scan.
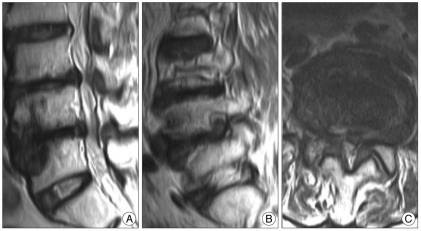
Fig. 1.
Preoperative magnetic resonance T2-weighted images. A : Midsagittal image showing the sclerotic change in both L4 lower and L5 upper endplates. B : Parasagittal image revealing the left L4-5 extraforaminal herniated disc. C : Axial image demonstrating the central stenosis on the level of the L4-5 disc space.
Fig. 2.
A and B : T2-weighted midsagittal image and computed tomography scans 10 months postsurgery showing the calcific mass along the posterior longitudinal ligament on L4-5 vertebral body. C : Parasagittal image indicating the degenerated foraminal disc with calcification. D : Axial image demonstrating the calcifed mass in the ventral epidural and extraforaminal space.
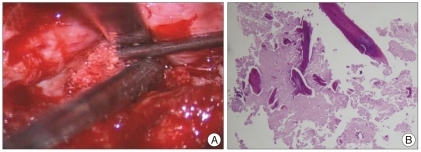
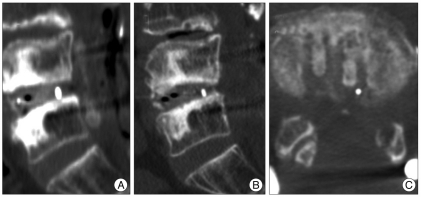
The decompressive laminectomy and interbody fusion in the L4-5 disc space was performed. Small gritty particles with the appearance of salt grains were seen in the encapsulated fibrotic tissue in the operative field (Fig. 3A). After the removal of the particles, ossification of the posterior longitudinal ligament (PLL) was found flattened longitudinally, along the midline of the L4 vertebral body. Because laminectomy was sufficient to decompress the thecal sac, the ossified PLL was kept in situ. There was no connection between the previous operated disc space and the ventral epidural space. The same particles were detected in the left L4-5 extraforaminal disc after anulotomy. The pathologist reported that the gritty particles were degenerated cartilage and bone showing dystrophic calcification without an inflammatory cellular reaction around the calcific deposits (Fig. 3B). Myxoid degeneration with dystrophic calcification was observed in the degenerated PLL. Neither inflammatory changes nor aggregates of rhomboid-shaped crystals which favored a diagnosis of calcium pyrophosphate dihydrate deposition disease (CPPD) were present. The patient recovered from the leg weakness and the radiating pain to the left buttock and posterior thigh. However, paresthesia in the lateral shin area persisted partially due to residual ossification of PLL (Fig. 4A). CT scan taken 14 months after surgery revealed that there was no residual calcific mass (Fig. 4B, C).
Fig. 3.
A : Intraoperative photograph revealing small gritty particles with the appearance of salt grains. B : Photograph demonstrates the dystrophic calcifications in the degenerated tissue (Hematoxylin-Eosin stain, magnification ×100).
Fig. 4.
A : Immedate postoperative CT scan indicating the residual calcification of posterior longitudinal ligament. B and C : CT scan taken 14 months after initial surgery showing there is no residual calcific mass.
DISCUSSION
Many possible causes of the epidural and extraforaminal calcification in this patient may include crystal-induced calcification such as hydroxyapatite deposition disease or CPPD, heterotopic calcification due to graft retropulsion, ossifying epidural hematoma and triamcinolone injection-related calcification. Although aseptic spondylodiscitis due to microcrystalline arthropathy could be the origin of the spontaneous epidural calcification, clinical manifestations of this case were not concordant with those of cases with crystal deposition disease19).
Clinical symptoms of the different crystal diseases are very similar and usually reflect a nonspecific inflammatory reaction around the crystals. Clinical manifestations are as follows : pain with a spontaneous and brutal onset, inflammatory pain, decreased range of motion, inflammatory signs such as fever, laboratory findings such as leukocytosis and an increased C-reactive protein8).
In our patient, laboratory results showed normal findings. The patient did not respond to NSAIDs or steroid injections via a transforaminal approach. She deteriorated to the extent of cauda equina syndrome, contrary to the usual clinical course of crystal-induced inflammation. Macroscopically, hydroxyapatite and the related phosphate crystal deposits appeared as calcified amorphous material with a milky or cheesy consistency in the para-articular fibrous connective tissue9). However, gritty particles showed a hard consistency in this case. The pathological report indicated that the lesions were composed of dystrophic calcification in the degenerated fibrocartilagenous tissue without showing any aggregates of rhomboid-shaped crystals favoring a diagnosis of CPPD14).
Although the iliac tricortical graft was not visible in the disc space, the authors thought the possibility of graft retropulsion followed by heterotopic calcification was very low due to the narrow posterior disc space of L4-5. Even if graft material had been backed out, the bone in the epidural space must have been be resorbed like the findings on the CT scan 14 months after initial surgery. There was also no connection between the previous operated disc space and the ventral epidural space during surgery.
Spinal epidural hematoma is an uncommon entity. Willner et al.18) reported an ossifying organized epidural blood patch in the dorsal spinal canal, resulting in radicular symptoms. In consideration of the shape and location of the calcific mass, there were several findings favoring the correlation with repetitive transforaminal triamcinolone injections. The location of calcification was consistent with the location of the site where repetitive injections were administered. A CT scan showed that the L4-5 residual extraforaminal disc degenerated into dystrophic calcification due to incomplete discectomy in the previous anterior approach. This finding has already been gaining wide support. De novo ossification and calcification in the outer layer of the posterior annulus fibrosus or posterior longitudinal ligament has been reported in patients with intradiscal triamcinolone hexacetonide injection therapy6,12). Menei et al.12) insisted that necrosis with a granulomatous inflammatory reaction and bone metaplasia seemed to be the primary cause of calcifications. Duquesnoy et al.7) declared that intradiscal triamcinolone injections should no longer be continued. Therefore, we are suggesting that the most probable cause of extraforaminal and epidural calcification was related to repeated injections in this patient, with the exception of the use of TA instead of triamcinolone hexacetonide.
TA has only been used instead of triamcinolone hexacetonide in South Korea. Because triamcinolone acetonide injectable suspension provides longer-lasting anti-inflammatory, antiproliferative and antipermeable effects compared with other steroid preparations, it has recently become more widely used for treating pain in the back and leg. The plausible pathogenesis of calcification in the epidural and extraforaminal space was related to the toxicity of the vehicles and the insolubility of TA.
Toxicity of vehicles
Vehicles are frequently used in the manufacture of ordinary drugs, and are evaluated for their safety when taken orally. However, little is known about the toxicity of these agents when administered directly into tissue cells in the intervertebral disc or epidural space. Ito et al.10) doubted that sodium carboxymethyl-cellulose, which was used in the triamcinolone suspension, was a cause of tissue necrosis and dystrophic calcification. Methylprednisolone acetate and its vehicle polyethylene glycol cause degeneration and formation of crystal-like matrix vesicles, which would become calcified in the discs, as shown by an experimental study using rabbits by Aoki et al.1).
Benzyl alcohol was used in our patient. The report of Chang et al.4) indicated that benzyl alcohol used in South Korea as a vehicle in TA suspensions, not the crystalline corticosteroid drug itself, resulted in cytotoxicity to cultured human retinal epithelial cells in a time and dose-dependent manner. Chang et al.3) also showed that a benzyl alcohol concentration of 9 mg/mL caused extensive lysis of rabbit corneal endothelial cells within the first minute of exposure. Recently, Shaikh et al.17) showed that both the preserved TA formulation and its vehicle caused significant reductions in the viability of cultured retinal epithelial cells. Similarly, Narayanan et al.15) concluded that the vehicle was not totally responsible for toxicity but may initiate TA-dependent toxicity. In the last analysis, it is certain that TA injectable suspension has a connection with dystrophic calcification.
Insolubility of TA
Triamcinolone hexacetonide has much lower solubility in water (0.0004% w/v at 258℃) than methylprednisolone acetate (0.0014% w/v at 258℃) or hydrocortisone (0.07% w/v at 258℃)16). While this may produce a longer lasting effect, it also renders the compound more likely to induce a foreign body reaction after subcutaneous injection or extravasation from a joint and has therefore been withdrawn from use. Triamcinolone acentonide is 10 times more water soluble (0.004% w/v at 258℃) than the hexacetonide16). Repetitive injections (over 10 times within six months) may lead to the increased concentration of TA injectable suspension in the ventral epidural space due to postoperative scar tissue changes in the dorsal spinal canal.
Although TA is more soluble than triamcinolone hexacetonide, aggregation occurs differently according to the preparation of TA. Moshfeghi et al.13) revealed that TA injectable suspension showed much larger aggregate size than both preservative-free TA and commercially available TA. This phenomenon may increase over time. These findings support that TA injectable suspension tends to conglomerate and gravitates toward the most dependent section of spinal canal. Particulate triamcinolone showed a risk for embolic infarct, which could result in serious neurologic sequelae or death11). Therefore, Lee et al.11) recommended that an interlaminar dexamethasone injection was safer than a transforaminal triamcinolone injection to avoid embolic infarcts in the cervical spine.
In a histological point of view, it was suggested that the accumulation of an insoluble steroid may act as a foreign body particle and induce a chronic granulomatous response with dystrophic calcification similar to the case of Conti and Shinder5). Additionally, Raghavendran et al.16) reported a case of subcutaneous gritty calcification surrounded by a chronic histiocytic response following two injections of triamcinolone hexacetonide for plantar fasciitis. However, we could not confirm the granulomatous lesion but did confirm dystrophic calcification in our patient. Carruthers et al.2) reported localized dystrophic calcification, which was found eight months after intralesional TA injections for infantile periocular hemangiomas, and suggested that undissolved steroid crystals may have formed a nidus for calcification in the subcutaneous tissue. This case is similar to our case demonstrating dystrophic calcification without a granulomatous change.
CONCLUSION
To our knowlege, this is a rare case showing that dystrophic calcificication may have developed after repeated TA injections. It is unclear whether the destruction of tissue cells preceding ossification and dystrophic calcification is attributable to the additives alone or both the additives and steroids in combination.
Repetitive postoperative TA injections at the same site may be the cause of dystrophic calcification not only in the degenerated residual disc but also in the posterior longitudinal ligament. It is important that we should know that there is a probability of TA injectable suspension causing epidural calcification. Therefore, experiments using animal models are needed to help disclose the effects of triamcinolone acetonide and benzyl alcohol on tissue cells in the spinal canal.
References
- 1.Aoki M, Kato F, Mimatsu K, Iwata H. Histologic changes in the intervertebral disc after intradiscal injections of methylprednisolone acetate in rabbits. Spine (Phila Pa 1976) 1997;22:127–131. doi: 10.1097/00007632-199701150-00001. discussion 132. [DOI] [PubMed] [Google Scholar]
- 2.Carruthers J, Jevon G, Prendiville J. Localized dystrophic periocular calcification : a complication of intralesional corticosteroid therapy for infantile periocular hemangiomas. Pediatr Dermatol. 1998;15:23–26. doi: 10.1046/j.1525-1470.1998.1998015023.x. [DOI] [PubMed] [Google Scholar]
- 3.Chang YS, Tseng SY, Tseng SH, Wu CL, Chen MF. Triamcinolone acetonide suspension toxicity to corneal endothelial cells. J Cataract Refract Surg. 2006;32:1549–1555. doi: 10.1016/j.jcrs.2006.04.025. [DOI] [PubMed] [Google Scholar]
- 4.Chang YS, Wu CL, Tseng SH, Kuo PY, Tseng SY. Cytotoxicity of triamcinolone acetonide on human retinal pigment epithelial cells. Invest Ophthalmol Vis Sci. 2007;48:2792–2798. doi: 10.1167/iovs.06-1146. [DOI] [PubMed] [Google Scholar]
- 5.Conti RJ, Shinder M. Soft tissue calcifications induced by local corticosteroid injection. J Foot Surg. 1991;30:34–37. [PubMed] [Google Scholar]
- 6.Debiais F, Bontoux D, Alcalay M, Vandermarcq P, Azais O, Denis A, et al. [Calcification after intra-disk injection of triamcinolone hexacetonide in lumbar disk hernia. Evaluation of therapeutical results in 3 years] Rev Rhum Mal Osteoartic. 1991;58:565–570. [PubMed] [Google Scholar]
- 7.Duquesnoy B, Debiais F, Heuline A, Houvenagel E, Bourgeois P, Alcalay M, et al. [Unsatisfactory results of intradiscal injection of triamcinolone hexacetonide in the treatment of sciatica caused by intervertebral disk herniation] Presse Med. 1992;21:1801–1804. [PubMed] [Google Scholar]
- 8.Feydy A, Lioté F, Carlier R, Chevrot A, Drapé JL. Cervical spine and crystal-associated diseases : imaging findings. Eur Radiol. 2006;16:459–468. doi: 10.1007/s00330-005-2776-z. [DOI] [PubMed] [Google Scholar]
- 9.Garcia GM, McCord GC, Kumar R. Hydroxyapatite crystal deposition disease. Semin Musculoskelet Radiol. 2003;7:187–193. doi: 10.1055/s-2003-43229. [DOI] [PubMed] [Google Scholar]
- 10.Ito S, Usui H, Maruyama K, Muro T. Roentgenographic evaluation of ossification and calcification of the lumbar spinal canal after intradiscal betamethasone injection. J Spinal Disord. 2001;14:434–438. doi: 10.1097/00002517-200110000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Lee JW, Park KW, Chung SK, Yeom JS, Kim KJ, Kim HJ, et al. Cervical transforaminal epidural steroid injection for the management of cervical radiculopathy : a comparative study of particulate versus non-particulate steroids. Skeletal Radiol. 2009;38:1077–1082. doi: 10.1007/s00256-009-0735-5. [DOI] [PubMed] [Google Scholar]
- 12.Menei P, Fournier D, Alhayek G, Mercier P, François H, Audran M, et al. [Calcificated necrotic inflammatory granuloma after intradiscal injection of triamcinolone hexacetonide] Rev Rhum Mal Osteoartic. 1991;58:605–609. [PubMed] [Google Scholar]
- 13.Moshfeghi AA, Nugent AK, Nomoto H, Sanislo SR, Kitchens JW, Moshfeghi DM. Triamcinolone acetonide preparations : impact of crystal size on in vitro behavior. Retina. 2009;29:689–698. doi: 10.1097/IAE.0b013e31819e390a. [DOI] [PubMed] [Google Scholar]
- 14.Mwaka ES, Yayama T, Uchida K, Kobayashi S, Kokubo Y, Nakajima H, et al. Calcium pyrophosphate dehydrate crystal deposition in the ligamentum flavum of the cervical spine : histopathological and immunohistochemical findings. Clin Exp Rheumatol. 2009;27:430–438. [PubMed] [Google Scholar]
- 15.Narayanan R, Mungcal JK, Kenney MC, Seigel GM, Kuppermann BD. Toxicity of triamcinolone acetonide on retinal neurosensory and pigment epithelial cells. Invest Ophthalmol Vis Sci. 2006;47:722–728. doi: 10.1167/iovs.05-0772. [DOI] [PubMed] [Google Scholar]
- 16.Raghavendran RR, Peart F, Grindulis KA. Subcutaneous calcification following injection of triamcinolone hexacetonide for plantar fasciitis. Rheumatology (Oxford) 2008;47:1838. doi: 10.1093/rheumatology/ken375. [DOI] [PubMed] [Google Scholar]
- 17.Shaikh S, Ho S, Engelmann LA, Klemann SW. Cell viability effects of triamcinolone acetonide and preservative vehicle formulations. Br J Ophthalmol. 2006;90:233–236. doi: 10.1136/bjo.2005.076190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Willner D, Weissman C, Shamir MY. Chronic back pain secondary to a calcified epidural blood patch. Anesthesiology. 2008;108:535–537. doi: 10.1097/ALN.0b013e31816499b7. [DOI] [PubMed] [Google Scholar]
- 19.Ziadé M, Zufferey P, So AK. Recurrent acute low back pain secondary to lumbar epidural calcification. Skeletal Radiol. 2007;36(Suppl 1):S116–S119. doi: 10.1007/s00256-006-0147-8. [DOI] [PubMed] [Google Scholar]