Abstract
BACKGROUND
Recent pooled analyses show an increased risk of death with increasing levels of the body-mass index (BMI, the weight in kilograms divided by the square of the height in meters) of 25.0 or higher in populations of European ancestry, a weaker association among East Asians, and no association of an increased BMI with an increased risk of death among South Asians. The limited data available on blacks indicate that the risk of death is increased only at very high levels of BMI (≥35.0).
METHODS
We prospectively assessed the relation of both BMI and waist circumference to the risk of death among 51,695 black women with no history of cancer or cardiovascular disease who were 21 to 69 years of age at study enrollment. Our analysis was based on follow-up data from 1995 through 2008 in the Black Women’s Health Study. Multivariable proportional-hazards models were used to estimate hazard ratios and 95% confidence intervals.
RESULTS
Of 1773 deaths identified during follow-up, 770 occurred among 33,916 women who had never smoked. Among nonsmokers, the risk of death was lowest for a BMI of 20.0 to 24.9. For a BMI above this range, the risk of death increased as the BMI increased. With a BMI of 22.5 to 24.9 as the reference category, multivariable-adjusted hazard ratios were 1.12 (95% confidence interval [CI], 0.87 to 1.44) for a BMI of 25.0 to 27.4, 1.31 (95% CI, 1.01 to 1.72) for a BMI of 27.5 to 29.9, 1.27 (95% CI, 0.99 to 1.64) for a BMI of 30.0 to 34.9, 1.51 (95% CI, 1.13 to 2.02) for a BMI of 35.0 to 39.9, and 2.19 (95% CI, 1.62 to 2.95) for a BMI of 40.0 to 49.9 (P<0.001 for trend). A large waist circumference was associated with an increased risk of death from any cause among women with a BMI of less than 30.0.
CONCLUSIONS
The risk of death from any cause among black women increased with an increasing BMI of 25.0 or higher, which is similar to the pattern observed among whites. Waist circumference appeared to be associated with an increased risk of death only among nonobese women. (Funded by the National Cancer Institute.)
The prevalence of overall and abdominal obesity has increased rapidly in the United States, with the greatest increases reported among black women.1 By 2020, overall obesity (body-mass index [BMI, the weight in kilograms divided by the square of the height in meters] ≥30.0) and abdominal obesity (waist circumference >35 in. [>88.0 cm]) are projected to affect up to 70% and 90% of black women, respectively, in the United States.1
Although overall obesity has been clearly associated with an increased risk of death,2-4 the association of overweight (BMI, 25.0 to 29.9) with risk of death has been inconsistent.5,6 A recent analysis of pooled data from 19 cohort studies involving 1.46 million white adults showed an increased risk of death from any cause with increasing levels of BMI of 25.0 or higher (the World Health Organization cutoff point for normal BMI) and with levels of BMI below 20.0 among participants who had never smoked.7 In a similar pooled analysis involving 1.1 million Asians, the risk of death was lowest for a BMI of 22.6 to 27.5 among East Asians who had never smoked, with an increasing risk of death below and above this range, whereas only a low BMI was associated with an increased risk of death among Indians and Bangladeshis.8 Studies based on limited numbers of blacks2,3,9-15 suggest a weaker association than among whites.2,3,9-13
Waist circumference, a measure of body-fat distribution and abdominal obesity, has been associated with an increased risk of death independently of overall obesity in several large cohort studies,4,16-18 but only a few have reported separately on blacks, with inconsistent results.11,13,18
The present study was designed to assess the relation of general and abdominal obesity to the risk of death with the use of prospective data from a large follow-up study involving black women. Because the association of body size with the risk of death may be confounded by the effects of cigarette smoking, our primary analyses are focused on women who had never smoked.
METHODS
STUDY POPULATION
The Black Women’s Health Study is an ongoing follow-up study involving 59,001 black women from all regions of the United States. In 1995, women 21 to 69 years of age enrolled by responding to health questionnaires mailed to subscribers of Essence magazine (a general-readership magazine targeted to black women), members of several black professional associations, and friends of early respondents.19 Follow-up questionnaires were sent every 2 years, with follow-up data available on more than 80% of the original cohort through 2009. Information on race or ethnic group, other demographic characteristics, lifestyle factors, and medical history was obtained.
The study was approved by the institutional review board of the Boston University Medical Campus. The return of a completed questionnaire was accepted by the institutional review board as implied informed consent.
The present analyses are based on follow-up data from 1995 through 2008, with follow-up beginning at 30 years of age. We excluded from the analysis 1459 women who reported a history of cancer (except nonmelanoma skin cancer), 3519 who reported a history of cardiovascular disease, 989 who reported a current pregnancy, 677 who did not report height or weight, 450 with a calculated BMI of less than 15.0 or 50.0 or higher, 91 for whom data on smoking status were missing, 91 for whom data on years of education were missing, and 30 who died before 30 years of age. After all exclusions, 51,695 women remained.
ASSESSMENT OF BODY SIZE AND COVARIATES
In 1995, we collected information on self-reported height (in feet and inches), current weight (in pounds), and waist circumference (in inches) at the level of the umbilicus. In a validation study involving 115 participants, Spearman correlations for self-reported versus technician-measured height, weight, and waist circumference were 0.93, 0.97, and 0.75, respectively.20,21 Information on years of education, marital status, vigorous physical activity, alcohol intake, and smoking status was obtained at baseline.
END POINTS
We searched the National Death Index22 for all study participants who had not completed the 2009 questionnaire and were not previously known to be deceased. A total of 1773 deaths were identified through 2008. The underlying cause of death was obtained for each participant from either a state-issued death certificate or the National Death Index. We used the International Classification of Diseases, Ninth Revision (ICD-9) to classify the underlying cause of death as cardiovascular disease (ICD-9 code 390–459, in 420 women), cancer (ICD-9 code 140–239, in 696 women), or other (in 657 women). The most common other causes of death were respiratory disease, diabetes, and renal disease.
STATISTICAL ANALYSIS
Person-years were measured from the beginning of follow-up in 1995 or from 30 years of age (if the participant was younger than 30 years of age at baseline) until the date of death or the end of follow-up (December 31, 2008), whichever occurred first. We used Cox proportional-hazards models, stratified according to age and 2-year questionnaire cycle, to estimate hazard ratios and 95% confidence intervals for the risk of death in relation to baseline measures of BMI and waist circumference. All multivariable models included terms for education (<12, 12, 13 to 15, or ≥16 years), marital status (single, married or living as married, divorced or separated, or widowed), vigorous physical activity (0, <1, 1 to 2, 3 to 4, 5 to 6, or ≥7 hours per week), and alcohol intake (<1, 1 to 6, or ≥7 drinks per week). In analyses among current or former smokers, multivariable models were further adjusted for pack-years of smoking (<5, 5 to 9, 10 to 14, 15 to 19, or ≥20 pack-years). For analyses of waist circumference, we excluded participants with missing or implausible waist circumference values (values below the 1st or above the 99th percentiles). Multivariable models for waist circumference were adjusted for the factors described above and for baseline BMI (15.0 to 18.4, 18.5 to 19.9, 20.0 to 22.4, 22.5 to 24.9, 25.0 to 27.4, 27.5 to 29.9, 30.0 to 34.9, 35.0 to 39.9, or 40.0 to 49.9). Tests for trend were conducted with the use of the median value for each category of BMI or waist circumference modeled as a continuous variable.
We conducted prespecified subgroup analyses within strata of smoking status (never smoked, former smoker, or current smoker), age (<45 or ≥45 years), level of education (≤12 or >12 years), vigorous physical activity (<1 or ≥1 hour per week), and duration of follow-up (≤6 or >6 years). We also assessed waist circumference within categories of BMI as a prespecified subgroup analysis. Tests for interaction were performed with the use of the likelihood-ratio test, comparing models with and without cross-product terms between the covariate and measure of body size. All statistical analyses were performed with the use of SAS statistical software, version 9.1 (SAS Institute).
RESULTS
BMI AND WAIST CIRCUMFERENCE
Among 51,695 women with no history of cancer or cardiovascular disease at baseline, the mean (±SD) BMI and waist circumference were 27.6±6.1 and 31.8±4.9 in. (80.8±12.4 cm), respectively. The Pearson correlation coefficient between BMI and waist circumference was 0.74. Two thirds (66%) of participants reported that they had never smoked, 18% were former smokers, and 16% were current smokers.
ASSOCIATION OF BMI AND WAIST CIRCUMFERENCE WITH THE RISK OF DEATH FROM ANY CAUSE
Among 33,916 women who had never smoked and who were followed from 1995 through 2008, there were 770 deaths from all causes. We observed a curvilinear association between BMI and the risk of death from any cause, with the lowest risk of death for a BMI of 20.0 to 24.9 (Fig. 1A, and Table 1 in the Supplementary Appendix, available with the full text of this article at NEJM.org). Relative to a BMI of 22.5 to 24.9 (the reference category used in the pooled analysis of cohort data from white populations7), multivariable-adjusted hazard ratios for the higher categories increased from 1.12 (95% confidence interval [CI], 0.87 to 1.44) for a BMI of 25.0 to 27.4 to 2.19 (95% CI, 1.62 to 2.95) for a BMI of 40.0 to 49.9 (P<0.001 for trend). Among women with a BMI of 20.0 or higher, a 5-unit increase in the BMI was associated with an 18% increase in the risk of death (95% CI, 1.11 to 1.25). The hazard ratios for a BMI of less than 18.5 and for a BMI of 18.5 to 19.9 were 1.89 (95% CI, 1.03 to 3.44) and 1.36 (95% CI, 0.87 to 2.14), respectively.
Figure 1. Estimated Hazard Ratios for Death from Any Cause According to Body-Mass Index (BMI) and Waist Circumference among Women Who Never Smoked.
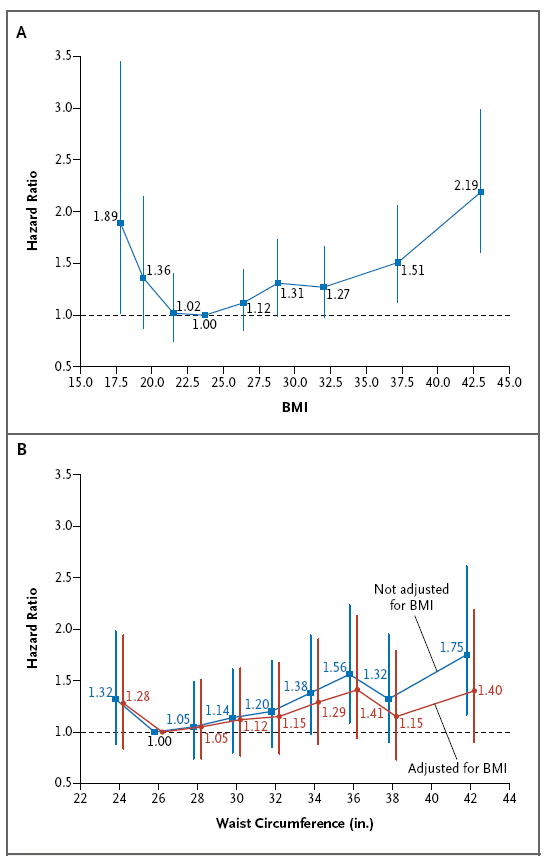
Hazard ratios for death from any cause, with 95% confidence intervals, are shown for BMI (the weight in kilograms divided by the square of the height in meters) (Panel A) and waist circumference (Panel B). Vertical lines indicate 95% confidence intervals. To convert inches to centimeters, multiply by 2.54. The analyses were adjusted for age, questionnaire cycle, educational level, marital status, vigorous physical activity, and alcohol intake.
Larger waist circumference was associated with an increased risk of death from any cause among women who had never smoked, after adjustment for all covariates except BMI (Fig. 1B, and Table 1 in the Supplementary Appendix). With a waist circumference of 26 to 27 in. as the reference category, hazard ratios increased from 1.05 (95% CI, 0.74 to 1.49) for a waist circumference of 28 to 29 in. to 1.75 (95% CI, 1.17 to 2.61) for a waist circumference of 40 to 47 in. (P<0.001 for trend). Adjustment for BMI attenuated the hazard ratios; the adjusted hazard ratio for the highest waist-circumference category was 1.40 (95% CI, 0.90 to 2.19) (P = 0.13 for trend). A waist circumference of less than 26 in. was associated with a nonsignificant increase in the risk of death (hazard ratio, 1.28; 95% CI, 0.84 to 1.94) relative to a waist circumference of 26 to 27 in. In an analysis that excluded women with a waist circumference of less than 26 in., a 5-unit increase in waist circumference, with adjustment for BMI, was associated with a 12% increase in the risk of death (95% CI, 0.99 to 1.26).
The associations of high BMI or large waist circumference with an increased risk of death were similar during the first 6 years of follow-up and in subsequent follow-up (data not shown). However, a low BMI and small waist circumference were associated with an increased risk of death only in the first 6 years of follow-up: with a BMI of 20.0 to 24.9 as the reference category, the hazard ratios for a BMI of less than 20.0 were 2.23 (95% CI, 1.22 to 4.10) during the first 6 years of follow-up (14 deaths) and 1.28 (95% CI, 0.79 to 2.06) during subsequent follow-up (21 deaths). With a waist circumference of 26 to 29 in. as the reference category, the hazard ratios for a waist circumference of less than 26 in. were 1.62 (95% CI, 0.85 to 3.07) during the first 6 years of follow-up (16 deaths) and 1.02 (95% CI, 0.64 to 1.63) in later follow-up (25 deaths). Because a low BMI and small waist circumference may have resulted from preexisting illness among women who died early in the follow-up period, we restricted subsequent analyses to women with a BMI of 20.0 or higher and a waist circumference of 26 in. or greater.
We assessed the association between waist circumference and the risk of death from any cause within categories of BMI. With a waist circumference of 35 in. or less as the reference category, the risk of death from any cause was increased for a waist circumference greater than 35 in. (a clinical cutoff point for abdominal obesity) among women with a BMI of less than 30.0 (hazard ratio, 1.55; 95% CI, 1.17 to 2.06) but not among women with a BMI of 30.0 or higher (hazard ratio, 1.07; 95% CI, 0.82 to 1.40). There was significant heterogeneity between obese and nonobese women for the association of abdominal obesity with the risk of death (P = 0.04 for interaction).
SUBGROUP ANALYSES
Table 1 shows results for the associations of BMI and waist circumference with the risk of death from any cause according to years of education. The hazard ratios for both BMI and waist circumference were higher among women with more than 12 years of education than among less-educated women, but there was no significant heterogeneity (for tests of interaction, P = 0.12 for BMI, P = 0.70 for waist circumference without adjustment for BMI, and P = 0.74 for waist circumference with adjustment for BMI).
Table 1.
Body-Mass Index (BMI) and Waist Circumference in Relation to Death from Any Cause among Women Who Never Smoked, According to Level of Education.*
| Variable | Education ≤12 Yr | Education >12 Yr | ||||||
|---|---|---|---|---|---|---|---|---|
| No. of Deaths | Person-Yr | Hazard Ratio (95% CI)† | No. of Deaths | Person-Yr | Hazard Ratio (95% CI)† | |||
| Adjusted | Additionally Adjusted for BMI | Adjusted | Additionally Adjusted for BMI | |||||
| BMI | ||||||||
|
| ||||||||
| 20.0–24.9 | 39 | 14,883 | 1.00 (reference) | 117 | 115,888 | 1.00 (reference) | ||
|
| ||||||||
| 25.0–29.9 | 61 | 21,465 | 0.88 (0.59–1.33) | 187 | 105,599 | 1.38 (1.09–1.75) | ||
|
| ||||||||
| 30.0–34.9 | 42 | 13,181 | 0.90 (0.57–1.41) | 105 | 52,480 | 1.48 (1.13–1.94) | ||
|
| ||||||||
| 35.0–49.9 | 48 | 10,675 | 1.43 (0.93–2.21) | 107 | 40,445 | 1.94 (1.48–2.55) | ||
|
| ||||||||
| P value for trend | 0.06 | <0.001 | ||||||
|
| ||||||||
| Waist circumference | ||||||||
|
| ||||||||
| 26–29 in. | 23 | 10,607 | 1.00 (reference) | 1.00 (reference) | 95 | 88,999 | 1.00 (reference) | 1.00 (reference) |
|
| ||||||||
| 30–33 in. | 39 | 15,116 | 0.99 (0.58–1.67) | 0.96 (0.55–1.67) | 128 | 84,604 | 1.20 (0.91–1.56) | 1.12 (0.84–1.48) |
|
| ||||||||
| 34–37 in. | 46 | 14,137 | 1.18 (0.71–1.96) | 1.10 (0.61–1.99) | 119 | 55,332 | 1.53 (1.16–2.02) | 1.34 (0.97–1.85) |
|
| ||||||||
| 38–47 in. | 37 | 10,187 | 1.29 (0.75–2.21) | 1.03 (0.53–2.01) | 94 | 39,398 | 1.67 (1.24–2.24) | 1.33 (0.91–1.94) |
|
| ||||||||
| P value for trend | 0.24 | 0.84 | <0.001 | 0.11 | ||||
The BMI is the weight in kilograms divided by the square of the height in meters. To convert inches to centimeters, multiply by 2.54.
All hazard ratios were adjusted for age, questionnaire cycle, level of education, marital status, vigorous physical activity, and alcohol intake. Hazard ratios for waist circumference were additionally adjusted for BMI. CI denotes confidence interval.
The association between BMI and the risk of death did not differ according to age (P = 0.73 for interaction) or physical activity (P = 0.68 for interaction). Similarly, the association of waist circumference with the risk of death did not differ according to age (P = 0.72 for interaction) or physical activity (P = 0.22 for interaction).
ASSOCIATION OF BMI AND WAIST CIRCUMFERENCE WITH THE RISK OF DEATH FROM SPECIFIC CAUSES
The associations of BMI and waist circumference with the risk of death from a specific cause are shown in Table 2. A higher BMI was strongly associated with an increased risk of death from cardiovascular conditions, with the risk increasing across categories of BMI (P<0.001 for trend). There was no significant association with the risk of death from cancer. Only a BMI of 35.0 or higher was associated with an increased risk of death from other causes. The risk of death from cardiovascular conditions increased with an increasing waist circumference after adjustment for BMI (P = 0.03 for trend), whereas waist circumference was not significantly associated with the risk of death from cancer or other causes.
Table 2.
Body-Mass Index (BMI) and Waist Circumference in Relation to Death from Specific Causes among Women Who Never Smoked.*
| Variable | Death from Cardiovascular Disease | Death from Cancer | Death from Other Causes | ||||||
|---|---|---|---|---|---|---|---|---|---|
| No. of Deaths | Hazard Ratio (95% CI)† | No. of Deaths | Hazard Ratio (95% CI)† | No. of Deaths | Hazard Ratio (95% CI)† | ||||
| Adjusted | Additionally Adjusted for BMI | Adjusted | Additionally Adjusted for BMI | Adjusted | Additionally Adjusted for BMI | ||||
| BMI | |||||||||
|
| |||||||||
| 20.0–24.9 | 21 | 1.00 (reference) | 71 | 1.00 (reference) | 64 | 1.00 (reference) | |||
|
| |||||||||
| 25.0–29.9 | 62 | 2.25 (1.36–3.72) | 106 | 1.14 (0.84–1.54) | 80 | 1.00 (0.72–1.40) | |||
|
| |||||||||
| 30.0–34.9 | 42 | 2.77 (1.62–4.73) | 52 | 1.03 (0.71–1.48) | 53 | 1.16 (0.80–1.68) | |||
|
| |||||||||
| 35.0–49.9 | 45 | 3.90 (2.29–6.64) | 45 | 1.23 (0.84–1.81) | 65 | 1.76 (1.23–2.52) | |||
|
| |||||||||
| P value for trend | <0.001 | 0.42 | <0.001 | ||||||
|
| |||||||||
| Waist circumference | |||||||||
|
| |||||||||
| 26–29 in. | 14 | 1.00 (reference) | 1.00 (reference) | 56 | 1.00 (reference) | 1.00 (reference) | 48 | 1.00 (reference) | 1.00 (reference) |
|
| |||||||||
| 30–33 in. | 34 | 1.97 (1.05–3.69) | 1.51 (0.78–2.92) | 76 | 1.08 (0.76–1.53) | 1.05 (0.72–1.52) | 57 | 0.97 (0.66–1.44) | 0.98 (0.65–1.48) |
|
| |||||||||
| 34–37 in. | 44 | 3.37 (1.83–6.22) | 2.18 (1.10–4.34) | 69 | 1.28 (0.89–1.85) | 1.21 (0.80–1.85) | 52 | 1.08 (0.72–1.62) | 1.07 (0.66–1.72) |
|
| |||||||||
| 38–47 in. | 41 | 4.29 (2.30–8.01) | 2.29 (1.08–4.85) | 36 | 0.94 (0.61–1.45) | 0.82 (0.48–1.39) | 54 | 1.48 (0.99–2.21) | 1.34 (0.79–2.29) |
|
| |||||||||
| P value for trend | <0.001 | 0.03 | 0.93 | 0.61 | 0.04 | 0.24 | |||
The BMI is the weight in kilograms divided by the square of the height in meters. To convert inches to centimeters, multiply by 2.54.
Hazard ratios were adjusted for age, questionnaire cycle, education, marital status, vigorous physical activity, and alcohol intake. Hazard ratios for waist circumference were additionally adjusted for BMI.
ASSOCIATION OF BMI AND WAIST CIRCUMFERENCE WITH THE RISK OF DEATH AMONG SMOKERS
Among both former and current smokers, an increase in the risk of death from any cause was observed only in very low and very high categories of BMI, with no increases in the risk of death for the categories of BMI in the overweight range (Table 1 in the Supplementary Appendix). A positive association between waist circumference and risk of death, after adjustment for BMI, was observed among former smokers, whereas there was no such association among current smokers.
DISCUSSION
In this large prospective study involving black women, the risk of death from any cause among women who had never smoked was lowest among women with a BMI of 20.0 to 24.9, with an increased risk of death for all categories of BMI in the overweight and obesity range. A larger waist circumference was associated with an increase in the risk of death from any cause only among nonobese nonsmokers. For both BMI and waist circumference, the positive association with the risk of death was stronger for deaths from cardiovascular disease than for deaths from cancer or other causes. Weaker associations were observed among current and former smokers than among women who had never smoked, even after adjustment for pack-years of smoking.
The results of the present study are similar to those of a pooled analysis involving white men and women, in which the risk of death from any cause was lowest for a BMI of 20.0 to 24.9 among subjects who had never smoked and all categories of overweight and obesity were associated with an increased risk of death from any cause.7 The hazard ratios are also similar in magnitude. Previous studies involving black women have shown weaker associations of BMI with the risk of death and a higher nadir of risk, but some of these studies were small, had limited follow-up, or did not present results separately for women who had never smoked and had no history of cancer or cardiovascular disease.2,3,9-15
In a pooled analysis involving Asians, the risk of death was lowest for a BMI of 22.6 to 27.5 among East Asians who had never smoked, with an increased risk of death below and above this range, whereas among South Asians, the risk of death did not increase with increasing BMI.8 For a given BMI, Asians are reported to have a higher percentage of body fat and blacks a lower percentage of body fat than whites.23 Despite these differences, our findings in blacks for the optimal BMI range with respect to the risk of death are generally consistent with those in both whites and East Asians.7,8
Waist circumference has been positively associated with the risk of death independently of BMI in several large cohort studies that mostly included white participants.4,16-18 In two of these studies, the association was stronger among women with a lower BMI than among heavier women,4,16 but in two other studies, the association was similar across categories of BMI.17,18 In the present study, a larger waist circumference was associated with an increased risk of death only among nonobese women. In the three previous studies that have reported on waist circumference and the risk of death among blacks, associations were weaker than those in other racial or ethnic groups18 or were absent.11,13
We observed increases in the risk of death among women with a low BMI or a small waist circumference. The stronger associations during the first few years of follow-up suggest that the increases may reflect, at least in part, illness-related weight loss.
A higher BMI and a larger waist circumference were each strongly associated with an increased risk of death from cardiovascular conditions. Only a very high BMI was significantly associated with an increased risk of death from other causes, and we observed no significant associations for the risk of death from cancer. Previous studies that comprised mostly white participants showed increases in the risk of death from both cardiovascular conditions and cancer in association with a high BMI2,7 or a large waist circumference,4,16,17 with stronger associations for death from cardiovascular causes. Our study may have had insufficient power to detect associations with the risk of death from cancer.
We found that the positive association between BMI and the risk of death was stronger among women with more years of education than among those with fewer years of education, but there was not a significant interaction according to educational level. These results are compatible with those of the Cancer Prevention Study I, which showed a significant positive association between BMI and the risk of death among black women with at least a high-school education and no significant association among those with less education.12 Other studies involving blacks have not reported results according to level of education. An association between body size and risk of death may be less evident among less-educated persons because they have higher absolute rates of death24 and because factors associated with low socioeconomic status (e.g., psychosocial stress and limited access to care) may play a greater role.25,26 In the Black Women’s Health Study, 97% of participants had at least a high-school education, as compared with 83% of the general population of black women of the same ages.27 Thus, we were able to informatively assess body size and risk of death among women with educational levels achieved by most black women but not among those with less than a high-school education. Previous studies of BMI and risk of death involving blacks have included a greater proportion of less-educated participants. This difference may account in part for the stronger relationship in the present study than that previously reported among blacks.2,3,9-13
Strengths of our study include its large size, the detailed data on potential confounders, and the long duration of follow-up. Restricting the primary analyses to participants who had never smoked and had no history of cancer or cardiovascular disease at baseline reduced the potential for confounding by smoking and preexisting illness. A limitation of the study was the use of self-reported measures of body size. However, data from a validation study in our cohort indicated a high correlation between self-reported and measured anthropometric variables.20,21
Whether these results are generalizable to men is unknown. In the pooled analyses of BMI and risk of death involving whites7 and Asians,8 the results were similar for men and women. The largest studies that have reported results according to race included insufficient numbers of blacks to establish whether the associations of obesity with the risk of death are similar in black men and women.2,3,18
In conclusion, overweight as well as obesity was associated with an increased risk of death from any cause among black women who had never smoked. In addition, a large waist circumference was associated with an increased risk of death among women who were not obese.
Supplementary Material
Acknowledgments
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Supported by a grant (CA058420) from the National Cancer Institute.
We thank the participants and staff of the Black Women’s Health Study for their dedication.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Beydoun MA, Wang Y. Gender-ethnic disparity in BMI and waist circumference distribution shifts in US adults. Obesity (Silver Spring) 2009;17:169–76. doi: 10.1038/oby.2008.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW., Jr Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341:1097–105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 3.Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355:763–78. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- 4.Pischon T, Boeing H, Hoffmann K, et al. General and abdominal adiposity and risk of death in Europe. N Engl J Med. 2008;359:2105–20. doi: 10.1056/NEJMoa0801891. Erratum, N Engl J Med 2010;362:2433. [DOI] [PubMed] [Google Scholar]
- 5.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–7. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 6.Orpana HM, Berthelot JM, Kaplan MS, Feeny DH, McFarland B, Ross NA. BMI and mortality: results from a national longitudinal study of Canadian adults. Obesity (Silver Spring) 2010;18:214–8. doi: 10.1038/oby.2009.191. [DOI] [PubMed] [Google Scholar]
- 7.Berrington de Gonzalez A, Hartge P, Cerhan JR, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010;363:2211–9. doi: 10.1056/NEJMoa1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zheng W, McLerran DF, Rolland B, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011;364:719–29. doi: 10.1056/NEJMoa1010679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wienpahl J, Ragland DR, Sidney S. Body mass index and 15-year mortality in a cohort of black men and women. J Clin Epidemiol. 1990;43:949–60. doi: 10.1016/0895-4356(90)90078-4. [DOI] [PubMed] [Google Scholar]
- 10.Cornoni-Huntley JC, Harris TB, Everett DF, et al. An overview of body weight of older persons, including the impact on mortality: the National Health and Nutrition Examination Survey I–Epidemiologic Follow-up Study. J Clin Epidemiol. 1991;44:743–53. doi: 10.1016/0895-4356(91)90126-t. [DOI] [PubMed] [Google Scholar]
- 11.Stevens J, Keil JE, Rust PF, Tyroler HA, Davis CE, Gazes PC. Body mass index and body girths as predictors of mortality in black and white women. Arch Intern Med. 1992;152:1257–62. [PubMed] [Google Scholar]
- 12.Stevens J, Plankey MW, Williamson DF, et al. The body mass index-mortality relationship in white and African American women. Obes Res. 1998;6:268–77. doi: 10.1002/j.1550-8528.1998.tb00349.x. [DOI] [PubMed] [Google Scholar]
- 13.Reis JP, Araneta MR, Wingard DL, Macera CA, Lindsay SP, Marshall SJ. Overall obesity and abdominal adiposity as predictors of mortality in U.S. white and black adults. Ann Epidemiol. 2009;19:134–42. doi: 10.1016/j.annepidem.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 14.Durazo-Arvizu R, Cooper RS, Luke A, Prewitt TE, Liao Y, McGee DL. Relative weight and mortality in U.S. blacks and whites: findings from representative national population samples. Ann Epidemiol. 1997;7:383–95. doi: 10.1016/s1047-2797(97)00044-6. [DOI] [PubMed] [Google Scholar]
- 15.Durazo-Arvizu RA, McGee DL, Cooper RS, Liao Y, Luke A. Mortality and optimal body mass index in a sample of the US population. Am J Epidemiol. 1998;147:739–49. doi: 10.1093/oxfordjournals.aje.a009518. [DOI] [PubMed] [Google Scholar]
- 16.Jacobs EJ, Newton CC, Wang Y, et al. Waist circumference and all-cause mortality in a large US cohort. Arch Intern Med. 2010;170:1293–301. doi: 10.1001/archinternmed.2010.201. [DOI] [PubMed] [Google Scholar]
- 17.Zhang C, Rexrode KM, van Dam RM, Li TY, Hu FB. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation. 2008;117:1658–67. doi: 10.1161/CIRCULATIONAHA.107.739714. [DOI] [PubMed] [Google Scholar]
- 18.Koster A, Leitzmann MF, Schatzkin A, et al. Waist circumference and mortality. Am J Epidemiol. 2008;167:1465–75. doi: 10.1093/aje/kwn079. [DOI] [PubMed] [Google Scholar]
- 19.Rosenberg L, Palmer JR, Rao RS, Adams-Campbell LL. Risk factors for coronary heart disease in African American women. Am J Epidemiol. 1999;150:904–9. doi: 10.1093/oxfordjournals.aje.a010098. [DOI] [PubMed] [Google Scholar]
- 20.Carter-Nolan PL, Adams-Campbell LL, Makambi K, Lewis S, Palmer JR, Rosenberg L. Validation of physical activity instruments: Black Women’s Health Study. Ethn Dis. 2006;16:943–7. [PubMed] [Google Scholar]
- 21.Wise LA, Palmer JR, Spiegelman D, et al. Influence of body size and body fat distribution on risk of uterine leiomyomata in U.S. black women. Epidemiology. 2005;16:346–54. doi: 10.1097/01.ede.0000158742.11877.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National death index user’s manual. Hyattsville, MD: National Center for Health Statistics; Oct, 2000. [Google Scholar]
- 23.Deurenberg P, Yap M, van Staveren WA. Body mass index and percent body fat: a meta analysis among different ethnic groups. Int J Obes Relat Metab Disord. 1998;22:1164–71. doi: 10.1038/sj.ijo.0800741. [DOI] [PubMed] [Google Scholar]
- 24.Jemal A, Thun MJ, Ward EE, Henley SJ, Cokkinides VE, Murray TE. Mortality from leading causes by education and race in the United States, 2001. Am J Prev Med. 2008;34:1–8. doi: 10.1016/j.amepre.2007.09.017. [DOI] [PubMed] [Google Scholar]
- 25.Stringhini S, Dugravot A, Shipley M, et al. Health behaviours, socioeconomic status, and mortality: further analyses of the British Whitehall II and the French GAZEL prospective cohorts. PLoS Med. 2011;8(2):e1000419. doi: 10.1371/journal.pmed.1000419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lantz PM, House JS, Lepkowski JM, Williams DR, Mero RP, Chen J. Socioeconomic factors, health behaviors, and mortality: results from a nationally representative prospective study of US adults. JAMA. 1998;279:1703–8. doi: 10.1001/jama.279.21.1703. [DOI] [PubMed] [Google Scholar]
- 27.Educational attainment in the United States: March 1995. Washington, DC: Department of Commerce, Bureau of the Census; 1996. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


