Abstract
Objective
The purpose of this case report is to describe and discuss the clinical diagnosis of a medial meniscus tear in an older patient using a multimodal management approach provided by a chiropractor.
Clinical Features
A 60-year-old woman reported to a chiropractic clinic with left knee pain and swelling. The history and physical examination findings suggested a medial meniscus tear, which was confirmed with magnetic resonance imaging.
Intervention and Outcome
Treatment consisted of therapeutic ultrasound; rest, ice, compression, and elevation protocol; soft tissue therapy using effleurage and lymphatic drainage; chiropractic mechanically assisted adjusting techniques to the left knee using a handheld mechanical thrusting instrument; sports taping applied to assist facilitation of the vastus medialis obliquus; and a specific rehabilitation program aimed at strengthening this musculature. The patient's pain was assessed using a quadruple numeric pain scale. Function of the left knee was examined using McMurray, Apley, and a variation of Helfet orthopedic tests, as well as joint line tenderness. Monitoring was done at the initial consultation and at the sixth and 12th treatments. The patient reported being able to walk, swim, and ride a bicycle asymptomatically. Her pain score at the concluding visit was 16.7%, indicating low-intensity pain.
Conclusion
This case indicated that conservative management of a meniscus tear through a chiropractic multimodal treatment approach provided an alternative or adjunctive therapy to routine orthopedic surgery for this patient.
Key indexing terms: Chiropractic; Meniscus, tibial; Knee; Diagnosis; Therapeutics
Introduction
The menisci of the tibiofemoral joint are crescent-shaped fibrocartilage structures firmly attached at their anterior and posterior horns to the intercondylar eminence, with their external margins attached by the coronary ligaments to the tibial condyles. The menisci deepen the joint surface; act like shock absorbers for load transmission; increase the congruency, stability, and lubrication of the joint; and are involved in the joint's nutrition cycle and proprioceptive feeback.1,2 The medial meniscus is “C shaped”; it is stably attached to the joint capsule around its entire outer border, with the middle third firmly adhered to the deep surface of the medial collateral ligament. It is therefore less mobile than the lateral meniscus that is “O shaped,” loosely attached to the joint capsule and popliteus, but is not attached to the lateral collateral ligament.1-3
Meniscal tears usually occur in the medial meniscus (posterior third) because of its relative lack of mobility.2,3 Meniscus injury is common in sports especially in young individuals with normal meniscal tissue.3,4 However, meniscus injury in active older individuals appears to be associated with a change in the meniscal tissue such that tears may occur more easily. Many times, these meniscal tears are associated with degenerative change of the knee joint.4-7 There are several common noncontact mechanisms for meniscal injury: a sudden change in direction while walking or running; forceful full flexion, such as squatting or arising from a squat position; or (for the older individual) a minor stress applied to the joint. Contact mechanisms in which varus, valgus, rotational, or hyperextension forces are applied to the knee and exceed the strength of the meniscus may produce longitudinal or transverse tears. An important aspect in relation to healing of a tear depends on its location, that is, whether the tear is in a more vascular or avascular region of the meniscus. Vessels penetrate from the outer margins into only 10% to 30% of the medial meniscus and 10% to 25% of the lateral meniscus. Therefore, more than two thirds of the menisci are avascular. It has been shown that injury to the avascular region of the meniscus does not produce an inflammatory or repair response. Injuries to the vascular region initiate the sequence of inflammation, repair, and remodeling for restoration of structure and function. It should be noted that, during the early repair process, repeated loading and motion may preclude healing.2,4 From a neuroanatomical perspective, the outer margins and the anterior and posterior horns of the menisci have sensory and mechanoreceptor fibers. This suggests that the menisci have a role in proprioceptive feedback mechanisms as well as in pain production. In a study by Dye et al,8 the menisci (and other intraarticular structures) of one of the authors were arthroscopically palpated without intraarticular anesthesia. They found that the periphery of the menisci produced slight to moderate discomfort with poorly localized sensation, whereas the inner margin of the menisci produced “nonpainful awareness” only.
A proper clinical history is the first step of clinical diagnosis, as careful questioning can point to the diagnosis.3,6,9 Historical evaluation that may raise suspicion for an underlying meniscus injury include the following: traumatic onset, with the knee hit from the side; nontraumatic onset, with weight-bearing on the knee and then twisting it; a pop at the time of injury; delayed swelling; a give-way sensation; and/or the knee painfully locks in one position. As the meniscus blends with the synovial lining of the joint capsule, a meniscal tear injury will apply a mechanical traction on the peripheral aspect, potentially producing inflammation of the synovial lining or a mechanical locking.10 The patient may report wasting of the quadriceps if the injury occurred at least a week earlier.3,9,11,12 Information in the older individual as to status of degeneration of the knee and prior trauma is important.6,13
Current evidence suggests that multiple assessment procedures during the physical examination increase the specificity and sensitivity and therefore diagnostic accuracy of identifying whether a patient has (or does not have) a medial meniscus lesion.3,7,12,14 Joint line tenderness has been reported as an accurate assessment; in reality, by itself, it has only moderate diagnostic accuracy.12,15-17 However, combined with 2 widely used classic orthopedic tests, McMurray and Apley (which are used for meniscal injury diagnosis) and Helfet (a test for the “screw-home” function of the tibiofemoral and patellofemoral joints), the diagnostic accuracy is improved.3,7,9,11,12,14,18,19
In the examination, the joint line is palpated for pain during the normal motion of the meniscus, moving posteriorly on flexion and anteriorly on extension. If the pain is found posteriorly on flexion and then disappears on extension, that would suggest involvement of the damaged meniscus.12,16,17 McMurray test is evaluated with the hip at 90° and knee flexed to more than 90°. A positive test result is signaled by palpating the joint line for clicking or popping with accompanying pain as the tibia is taken from a position of abduction and external rotation to one of adduction and internal rotation.9,11,18 Apley test is evaluated with the patient prone. A positive test result is the production of deep pain or joint line pain when the tibia is internally and externally rotated under compression in different position of knee extension.9,18 The authors use a variation of the Helfet test that not only includes observation of the screw-home mechanism, that is, the tibia moving in external rotation with quadriceps stabilization of the patella during extension of the knee in a seated position, but adds palpation of the quality, quantity, and timing of the screw-home mechanism and of the vastus medialis obliquus (VMO) contraction and stabilization of the patella (Fig 1A-F).
Fig 1.

The authors' variation of Helfet test. A and B, The original Helfet test in which the practitioner observes markings on the tibial tuberosity move relative to the markings on the patella during knee extension. Lateral movement of the lower mark represents the external rotation of the tibia during the “screw-home” mechanism during knee extension. C and D, First aspect of the variation in which the practitioner palpates for the screw-home mechanism, that is, quality, quantity, and timing of both the external rotation of the tibia and the stabilization of the patella with contacts on the patella and tibial tuberosity. E and F, Second variation in which the practitioner palpates for quality, quantity, and timing of the vastus medialis contraction as it stabilizes the patella medially, comparing the uninvolved to the involved side.
Magnetic resonance imaging (MRI) is considered by some as the criterion standard for accurate, noninvasive evaluation of meniscal tears.11,20 However, it has been demonstrated that clinical diagnosis of meniscal tears is as reliable as the results for MRI.11,21 If there is any doubt with the physical examination, an MRI should be performed to negate the need for further invasive procedures.5,20,22,23 It must be noted that many regard arthroscopy as the criterion standard, as it allows definitive classification and assessment of the entire meniscus.7
It is well recognized that large numbers of patients attend orthopedic clinics with knee injuries.11 Chiropractors often serve a role as primary contact and conservative management alternatives to a secondary contact orthopedic consultation.9 It is reasonable to assume that a well-trained chiropractic practitioner can safely rely on clinical examination for diagnosing meniscal injuries and provide conservative management as an alternative or in conjunction with orthopedic therapy.21,24-28 For a chiropractor to serve as the conservative management alternative, it is the authors' opinion that a multimodal approach to management should be used. Hoskins et al29 stated that multimodal chiropractic management integrates components of passive and active care to address both the acute (pain) phase and the chronic (rehabilitation) phase. A multimodal management approach incorporates a combination of therapies and techniques including adjusting (manipulation) and mobilization, soft tissue and stretching techniques, rehabilitation and corrective exercises, taping, physiologic therapeutics, nutrition, and training advice/programs.30
The purpose of this case report is to describe and discuss the clinical diagnosis of a medial meniscus tear in an older patient that responded to a multimodal management approach provided by a chiropractic practitioner.
Case report
A 60-year-old female university lecturer had left knee pain and swelling of 8 weeks' duration. The onset occurred while on a holiday hiking trip, when she stepped onto a bench and felt a twisting sensation in her left knee. She recalled feeling immediate pain and, within 24 hours, noticed a moderate effusion along the medial joint line of the knee, extending from the patella anteriorly to the medial hamstring tendons posteriorly. With no access to first aid equipment, she could only use her “hiking poles” to reduce the amount of weight-bearing through her left knee. It was 1 week before she returned to a metropolitan area where she was able to seek treatment. She initially sought consultation with a physiotherapist, where the left knee was diagnosed as a sprain of the medial collateral ligament. Her left knee was strapped with a compression bandage, and she was advised to use crutches and be non–weight-bearing for 6 weeks. Two weeks, later she returned home and consulted her medical doctor who felt the problem was self-limiting and prescribed 25 mg daily dosage of indomethacin anti-inflammatory medication and continued non–weight-bearing. There was no improvement in her pain and swelling symptoms 8 weeks after the initial onset, so she sought chiropractic opinion.
She reported the pain being located “within” the medial joint line of the left knee. She said that the pain was there all the time and has an “achy” quality. However, she said that, on weight-bearing, the pain had a “sharp” quality and “that something felt like it was catching!” She also reported that the left knee was always swollen along the anteromedial joint line. She said that attempting to walk stairs aggravated the problem, especially downstairs. She reported no priory injury to the left knee. However, she related a history of degeneration and pain in the right knee with a notable varus deformity for which she had sought prior chiropractic treatment. She stated that both parents had knee replacement surgery related to degeneration.
Before examination, a quadruple numeric pain scale (QNPS) assessment tool was administered to measure the pain intensity, monitor the patient's progress, and indicate the effectiveness of management.31,32 Her initial score on the QNPS was 56.7%, indicating high-intensity pain (Fig 2).
Fig 2.
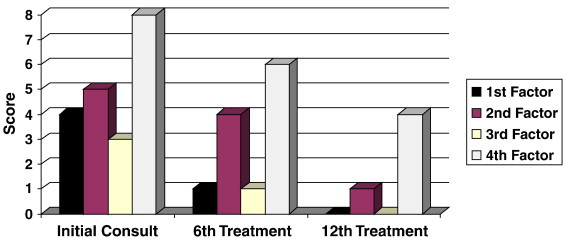
Quadruple numeric pain scale scores at initial consultation, sixth treatment, and 12th treatment. The QNPS is a questionnaire based on 4 specific factors—first factor: pain level at the time of the current consultation, second factor: typical or average pain since the onset of the condition, third factor: pain level at its best since the onset of the condition, and fourth factor: pain level at its worst since the onset of the condition. The scores from the first, second and fourth factors are averaged and then multiplied by 10 to yield a score from 0 to 100. The final score is then categorized as “low-intensity” pain (<50) or “high-intensity” pain (>50). (Color version of figure is available online.)
Upon standing postural examination, the patient held her left knee in slight flexion. Inspection and palpation of the left knee revealed edema in the inferomedial patella region anteriorly with an increase in temperature and atrophy of the VMO with the patella sitting laterally. Pain was elicited during palpation of the medial joint line. Upon range of motion (ROM) examination, there was a decrease in left knee flexion (limited to 60°) and extension (limited by 10°), with the patient reporting that pain and tightness were felt “within the knee joint.” Orthopedic provocation examinations including the McMurray and Apley tests reproduced the left knee pain. Result of the authors' variation of Helfet test was also positive on the left for a lack of patella medial motion and tibial external rotation with minimal VMO contraction. The patient provided radiographs taken 6 months earlier for a previous right knee complaint. The radiological examination revealed minor loss of the medial joint space with some early degenerative changes of the tibia, affecting both the medial and lateral plateaus of the left knee (Fig 3A, B).
Fig 3.

A, Lateral radiograph views of the right and left knee. B, Bilateral knee anteroposterior view. Note the early degeneration in the left knee and the extensive degeneration in the right knee.
Clinical diagnosis of a medial meniscal tear was made through synthesis of the patient history and physical examination.3,7,11,12,14,19,21 Differential diagnosis of coronary ligament sprain, an intraarticular loose body, and a meniscal cyst was also considered. Confirmation of the clinical diagnosis was obtained through MRI, ordered through the patient's medical doctor after the initial chiropractic consultation. The MRI results indicated an undisplaced transverse oblique tear of the body and posterior horn of the medial meniscus with slight meniscal extrusion (Fig 4A, B). Evaluation by an orthopedic surgeon was advised to provide the patient with all possible management options. The earliest appointment available was in 7 weeks' time. The patient decided to commence chiropractic treatment while awaiting her consultation with the orthopedic surgeon.
Fig 4.
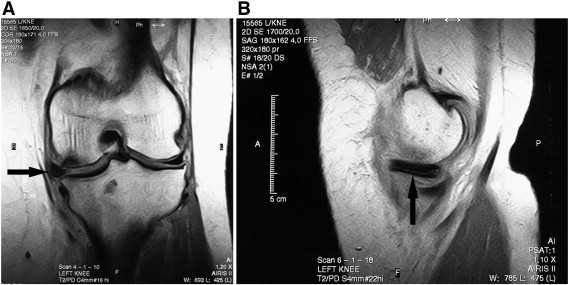
A, Left knee coronal MRI. Arrow indicates changes to the medial meniscus. Note the bone edema within the medial femoral condyle. B, Left knee sagittal MRI. Arrow indicates changes to the medial meniscus.
A chiropractic multimodal approach to treatment and management of this patient was initiated.24 The early management strategy was aimed at mobilizing and reducing the inflammation, as well as decreasing pain. Soft tissue therapy,3,12 using an Arnica ointment, consisted of effleurage and lymphatic drainage massage to the left gastrocnemius/soleus complex, popliteus, hamstrings, and quadriceps musculature. Therapeutic ultrasound26 was then applied at 1.0 W/cm2 pulsed 50% for 5 minutes over the anteromedial left knee. This sequence of treatment was intended to further enhance the absorption of the topically applied Arnica through the therapeutic application of ultrasound (phonophoresis). In addition, the patient was prescribed the rest, ice, compression, and elevation protocol25,26 in the following method: rest as much as possible, initially using crutches for non–weight-bearing ambulation with progression to weight-bearing as pain allowed; ice (crushed or cubes wrapped in a cool moist towel) applied to the medial joint line of the left knee for 10 minutes, removed for 10 minutes, and reapplied for 10 minutes 3 to 5 times per day; a compression bandage applied throughout the day (removed while sleeping); and the left knee kept elevated whenever possible. As the swelling subsided, chiropractic mechanically assisted adjusting techniques to the left knee using a handheld mechanical thrusting instrument was applied to restore normal joint motion.3,24,27 With the patient supine and the left knee supported in 5° to 10° of flexion, 3 repetitions of mechanically assisted adjusting techniques were applied to each of the tibiofemoral and patellofemoral articulations in a lateral to medial direction (as determined by dynamic palpation). Normal zinc oxide sports tape was applied to the patient's left anteromedial quadriceps, in line with the fibers of the VMO, to assist facilitation33-36 of the atrophied and weakened musculature (Fig 5). The patient was advised to perform isometric VMO exercises for periods up to 30 seconds, in conjunction with the facilitaping (Fig 6A, B).3,9,27,28,37-39 Exacerbation of the knee pain was to be avoided during the rehabilitation exercises; that is, if the patient felt that the exercises were reproducing or aggravating the knee pain, she was to stop performing them. The patient received a total of 12 treatments over a 9-week period (2 treatments per week for 3 weeks, and 1 treatment per week for 6 weeks). The patient filled out a QNPS outcome assessment on the sixth and 12th treatments.
Fig 5.

The authors' use of facilitaping. Tape is applied in line with the fibers of the VMO to assist facilitation of the musculature.
Fig 6.

A, Isometric VMO exercise—knee in flexion. With the knee at 90° of flexion and the foot in contact with the floor, the patient pushes her heel into the ground. The patient attempts to maintain an isometric contraction of the VMO. B, Isometric VMO exercise—knee in extension. The patient externally rotates the leg, dorsiflexes the ankle, and extends the knee. The patient attempts to maintain an isometric contraction of the VMO.
Nine weeks after the initial treatment (ie, on the 12th treatment), a reexamination revealed negative findings for McMurray, Apley, and Helfet orthopedic examinations. No pain could be elicited during palpation of the medial joint line, and no inflammatory signs of the left knee were apparent. The left knee ROM was full and pain free. The patient reported being able to walk, swim, and ride a bicycle asymptomatically. Her QNPS score at the concluding visit was 16.7%, indicating low-intensity pain (Fig 2).
Discussion
For this patient, functional improvement of the left knee was demonstrated through changes in the QNPS factors and physical examination findings. Fig 2 shows the results of the QNPS scores obtained at the initial treatment, sixth treatment, and 12th treatment. After 6 treatments, each of the QNPS factors had decreased 20% compared with initial treatment values. After 12 treatments, the QNPS factors had further decreased another 20%, indicating a reduction in overall pain intensity score of 40% compared with initial treatment values.
Palpatory and orthopedic test assessments demonstrated a complete negation of signs and symptoms in the sixth and 12th treatments. The patient's perception of her ability to function normally improved during chiropractic care, as she experienced a reduction of her left knee pain and swelling. The decrease of pain and swelling allowed her to perform the rehabilitation exercises optimally, providing continual functional improvement of the knee joint and surrounding musculature.
Astute clinical decision-making requires a knowledge base of multiple assessment procedures that can be varied depending on the type of patient, for example, patient's age. As well as the procedures used in this case, other “orthopedic tests” may be useful. One is an expansion of joint line palpation and is known as Steinmann's Tenderness Displacement Test.12 The Thessaly test is a functional test that may reproduce the mechanism of injury and has good research background with high specificity, sensitivity, and diagnostic accuracy.15,40 In this test, the patient stands with the knee held in 20° flexion and internally and externally rotates the leg. Pain in the joint line and/or catching or locking is considered a positive response. Another suggested functional provocation assessment is the squat test, which compresses the meniscus and produces pain posteriorly in the joint space.3,7
Astute clinical decision-making also uses a multimodal management approach. A review of the literature revealed 2 citations describing the positive effects of chiropractic care on meniscal injury.27,39 Polkinghorn27 reported the utilization of a handheld mechanical thrusting instrument and auxiliary homeopathic therapy resulted in the complete resolution of his patient's symptoms. Brantingham et al39 performed genu-circumduction-extension mobilization; high-velocity, low-amplitude axial elongation; and a knee exercise program that helped 4 of 5 patients in their case series. In addition, Muché26 demonstrated that the management of a meniscal tear using the rest, ice, compression, and elevation protocol and therapeutic ultrasound decreased pain and increased knee ROM, allowing the patient to make significant functional gains and progressions within a rehabilitation program. Furthermore, a study comparing arthroscopic treatment with conservative (exercise) treatment determined that exercise alone should be the first choice of treatment in nontraumatic medial meniscus tears.28
The natural history of a meniscal injury is not well established. It has been suggested that stable tears in the outer vascular portion should be left alone to heal.41 As well, there is a small amount of evidence that patients may experience relief of symptoms if treated conservatively.28,42 Some have the clinical observation that very few patients respond well to a conservative, nonsurgical approach especially if there are “mechanical” aspects to their condition.7 However, the empirical evidence suggests that conservative treatment can be used as an alternative or in conjunction with orthopedic therapy for meniscus tears and that a chiropractic multimodal management approach that integrates components of passive and active care may be useful in the alleviation of a patient's symptoms and promote functional progression from a meniscal injury. 3,19,26-29,39
Limitations
There are limitations to this case study, particularly the paucity of research on the reliability of chiropractic multimodal management for meniscal injuries. This report demonstrates only a single case; and therefore, the management protocol cannot be generalized to all cases of meniscal injury. In addition, it must be noted that the positive outcome demonstrated in this case might suggest that the mechanical properties of the meniscal tear were such that it was not the pain generating tissue. Further research involving randomized controlled and clinical trials, as well as observational and clinical studies with long-term follow up, is both required and warranted. Future directions for chiropractic research should investigate multimodal management of meniscal injuries in patients both with and without joint degeneration, incorporating additional functional outcome assessment tools such as the Lower Extremity Functional Scale and the Knee Injury and Osteoarthritis Outcome Score.
Conclusion
With a focus of activity in an aging population, chiropractors will be required to assess, diagnose, and manage a variety of degenerative related problems. The literature proposes that a comprehensive clinical history in combination with multiple physical examination procedures is an important diagnostic methodology and is as reliable as MRI to diagnose meniscal tears. The positive response observed in this case suggests that chiropractic multimodal management of meniscus tears may be of benefit to patients and offers an alternative option to routine orthopedic surgery. Further research involving randomized controlled and clinical trials, as well as observational and clinical studies with long-term follow-up, is both required and warranted to clarify the effectiveness of a chiropractic multimodal approach in the management of meniscal injury.
Funding sources and potential conflicts of interest
No funding sources or conflicts of interest were reported for this study.
Acknowledgment
The authors thank Dr Tom Molyneux, BAppSc(Chiro), GradDipEd(Tertiary), for his assistance with the images used in this paper.
References
- 1.Moore K.L., Dalley A.F., Agur A.M. Clinically orientated anatomy. 6th ed. Lippincott Williams & Wilkins; Baltimore: 2010. pp. 641–642. [Google Scholar]
- 2.Lee J.M., Fu F.H. The meniscus: basic science and clinical implications. Op Tech Orthop. 2000;10(3):162–168. [Google Scholar]
- 3.Souza TA, Hyde TE. The knee. In: Hyde TE, Gengenbach MS. Conservative management of sports injuries. 2nd ed. Sudbury, MA: Jones and Bartlett Publishers, 2007:666, 675, 703.
- 4.Brinker M.R., O'Connor D.P., Almekinders L.C., Best T.M., Buckwalter J.A., Garrett W.E. Physiology of injury to musculoskeletal structures. 4. Meniscus injury. In: DeLee J.C., Drez D., Miller M.D., editors. Orthopaedic sports medicine. 3rd ed. Saunders-Elselvier; Philadelphia: 2010. pp. 56–65. [Google Scholar]
- 5.Lange A.K., Fiatrone Singh M.A., Smith R.M., Foroughi N., Baker M.K., Shnier R. Degenerative meniscus tears and mobility impairment in women with knee osteoarthritis. Osteoarthritis Cartilage. 2007;15:701–708. doi: 10.1016/j.joca.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 6.Wagemakers H.P., Heintjes E.M., Boks S.S., Berger M.Y., Verhaar J.A., Koes B.W. Diagnostic value of history-taking and physical examination for assessing meniscal tears of the knee in general practice. Clin J Sports Med. 2008;18(1):24–31. doi: 10.1097/JSM.0b013e31815887a7. [DOI] [PubMed] [Google Scholar]
- 7.Brockmeir S.F., Rodeo S.A. Knee: section b—meniscal injuries. In: DeLee J.C., Drez D., Miller M.D., editors. Orthopaedic sports medicine. 3rd ed. Saunders-Elselvier; Philadelphia: 2010. pp. 1597–1604. [Google Scholar]
- 8.Dye S.F., Vaupel G.L., Dye C.C. Conscious neurosensory mapping of the internal structures of the human knee without intraarticular anesthesia. Am J Sports Med. 1998;26(6):773–777. doi: 10.1177/03635465980260060601. [DOI] [PubMed] [Google Scholar]
- 9.Souza T.A. Differential diagnosis and management for the chiropractor. 4th ed. Jones and Bartlett Publishers; Sudbury, MA: 2009. pp. 380–382. [Google Scholar]
- 10.Reid D.C. Sports injury assessment and rehabilitation. Churchill Livingstone; New York: 1992. p. 311. [Google Scholar]
- 11.Mohan B.R., Gosal H.S. Reliability of clinical diagnosis in meniscal tears. Int Orthop. 2007;31(1):57–60. doi: 10.1007/s00264-006-0131-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hammer W.I. The knee and leg. In: Hammer W.I. Functional soft-tissue examination and treatment by manual methods. 3rd ed. Sudbury, MA: Jones and Bartlett Publishers, 2007:319, 323-352, 371-373.
- 13.March L.M., Bagga H. Epidemiology of osteoarthritis in Australia. Med J Aust. 2004;180:S6–S10. doi: 10.5694/j.1326-5377.2004.tb05906.x. [DOI] [PubMed] [Google Scholar]
- 14.Cleland J. Orthopaedic clinical examination: an evidence-based approach for physical therapists. Icon Learning Systems; Carlstadt, NJ: 2005. pp. 311–315. [Google Scholar]
- 15.Karachalios T., Hantes M., Aristides H.Z., Zachos V., Karantanas A.H., Konstantinos N.M. Diagnostic accuracy of a new clinical test (the Thessaly test) for early detection of meniscal tears. J Bone Joint Surg. 2005;87(5):955–962. doi: 10.2106/JBJS.D.02338. [DOI] [PubMed] [Google Scholar]
- 16.Eren O.T. The accuracy of joint line tenderness by physical examination in the diagnosis of meniscal tears. Arthroscopy. 2003 Oct;19(8):850–854. doi: 10.1016/s0749-8063(03)00736-9. [DOI] [PubMed] [Google Scholar]
- 17.Rose R.E. The accuracy of joint line tenderness in the diagnosis of meniscal tears. West Indian Med J. 2006 Oct;55(5):323–326. doi: 10.1590/s0043-31442006000500006. [DOI] [PubMed] [Google Scholar]
- 18.Rath E., Richmond J.C. The menisci: basic science and advances in treatment. Br J Sports Med. 2000 Aug;34(4):252–257. doi: 10.1136/bjsm.34.4.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Solomon D.H., Simel D.L., Bates D.W., Katz J.N., Schaffer J.L. The rational clinical examination. Does this patient have a torn meniscus or ligament of the knee? Value of the physical examination. JAMA. 2001 Oct 3;286(13):1610–1620. doi: 10.1001/jama.286.13.1610. [DOI] [PubMed] [Google Scholar]
- 20.Van Dyck P., Gielen J., D'Anvers J., Vanhoenacker F., Dossche L., Van Gestel J. MR diagnosis of meniscal tears of the knee: analysis of error patterns. Arch Orthop Trauma Surg. 2007;127:849–854. doi: 10.1007/s00402-007-0318-7. [DOI] [PubMed] [Google Scholar]
- 21.Kocabey Y., Tetik O., Isbell W.M., Atay O.A., Johnson D.L. The value of clinical examination versus magnetic resonance imaging in the diagnosis of meniscal tears and anterior cruciate ligament rupture. Arthroscopy. 2004;20(7):696–700. doi: 10.1016/j.arthro.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 22.Amendola A. MRI vs clinical examination for diagnosing meniscus tears: a review. Clin J Sport Med. 2008;18(4):377–379. doi: 10.1097/01.jsm.0000299228.59773.9e. [DOI] [PubMed] [Google Scholar]
- 23.Huysse W.C.J., Verstraete K.L. Health technology assessment of magnetic resonance imaging of the knee. European J Rad. 2008;65:190–193. doi: 10.1016/j.ejrad.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 24.Brantingham J.W., Globe G., Pollard H., Hicks M., Korporaal C., Hoskins W. Manipulative therapy for lower extremity conditions: expansion of the literature review. J Manipulative Physiol Ther. 2009;32(1):53–71. doi: 10.1016/j.jmpt.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 25.Alcantara J., McDaniel J.W., Plaugher G., Alcantara J. Management of a patient with calcium pyrophosphate deposition disease and meniscal tear of the knee: a case report. J Manipulative Physiol Ther. 1998;21(3):197–204. [PubMed] [Google Scholar]
- 26.Muché J.A. Efficacy of therapeutic ultrasound treatment of a meniscus tear in a severely disabled patient: a case report. Arch Phys Med Rehabil. 2003 Oct;84(10):1558–1559. doi: 10.1016/s0003-9993(03)00315-0. [DOI] [PubMed] [Google Scholar]
- 27.Polkinghorn B.S. Conservative treatment of torn medial meniscus via mechanical force, manually assisted short lever chiropractic adjusting procedures. J Manipulative Physiol Ther. 1994;17(7):474–484. [PubMed] [Google Scholar]
- 28.Herrlin S., Hallander M., Wange P., Weidenhielm L., Werner S. Arthroscopic or conservative treatment of degenerative medial meniscal tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 2007;15(4):393–401. doi: 10.1007/s00167-006-0243-2. [DOI] [PubMed] [Google Scholar]
- 29.Hoskins W., McHardy A., Pollard H., Windsham R., Onley R. Chiropractic treatment of lower extremity conditions: a literature review. J Manipulative Physiol Ther. 2006;29(8):658–671. doi: 10.1016/j.jmpt.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 30.Hoskins W., Pollard H., Garbutt P. How to select a chiropractor for the management of athletic conditions. Chiropr Osteopat. 2009;17:3. doi: 10.1186/1746-1340-17-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khorsan R., Coulter I.D., Hawk C., Goertz Choate C. Measures in chiropractic research: choosing patient-based outcome assessments. J Manipulative Physiol Ther. 2008;31(5):355–375. doi: 10.1016/j.jmpt.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 32.Von Korff M., Deyo R.A., Cherkin D., Barlow W. Back pain in primary care. Spine. 1993;18(7):858–862. doi: 10.1097/00007632-199306000-00008. [DOI] [PubMed] [Google Scholar]
- 33.Smith M., Sparkes V., Busse M., Enright S. Upper and lower trapezius muscle activity in subjects with subacromial impingement symptoms: is there imbalance and can taping change it? Phys Ther Sport. 2009;10(2):45–50. doi: 10.1016/j.ptsp.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 34.Hsu Y.H., Chen W.Y., Lin H.C., Wang W.T.J., Shih Y.F. The effects of taping on scapular kinematics and muscle performance in baseball players with shoulder impingement syndrome. J Electromyogr Kinesiol. 2009;19(6):1092–1099. doi: 10.1016/j.jelekin.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 35.Morrissey D. Proprioceptive shoulder taping. J Bodyw Mov Ther. 2000;4(3):189–194. [Google Scholar]
- 36.Tobin S., Robinson G. The effect of McConnell's vastus lateralis inhibition taping technique on vastus lateralis and vastus medialis obliquus activity. Physiotherapy. 2000;86(4):173–183. [Google Scholar]
- 37.Heckmann T.P., Barber-Westin S.D., Noyes F.R. Meniscal repair and transplantation: indications, techniques, rehabilitation, and clinical outcome. J Orthop Sports Phys Ther. 2006;36(10):795–814. doi: 10.2519/jospt.2006.2177. [DOI] [PubMed] [Google Scholar]
- 38.Roos E.M. Meniscus tear, meniscectomy and osteoarthritis—cause or consequence? Osteoarthritis Cartilage. 2007;15:C9. [Google Scholar]
- 39.Brantingham J.W., Globe G., Tong V., Bates C.C., Jukes G., Van-Houten C., Doorly K. Diversified chiropractic adjusting and management in the treatment of five clinically diagnosed meniscus injury patients with MRI imaging in four cases. J Am Chiropr Assoc. 2008;45(5):11–24. [Google Scholar]
- 40.Mirzatolooei F., Yekta Z., Bayazidchi M., Ershadi S., Afshar A. Validation of the Thessaly test for detecting meniscal tears in anterior cruciate deficient knees. The Knee. 2010;17(3):221–223. doi: 10.1016/j.knee.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 41.Weiss C.B., Lundberg M., Hamberg P., DeHaven K.E., Gillquist J. Non-operative treatment of meniscal tears. J Bone Joint Surg Am. 1989;71(6):811–822. [PubMed] [Google Scholar]
- 42.Hede A., Hempel-Poulsen S., Jensen J.S. Symptoms and level of sports activity in patients awaiting arthroscopy for meniscal lesions of the knee. J Bone Joint Surg Am. 1990;72(4):550–552. [PubMed] [Google Scholar]


