Abstract
Recent theories of Generalized Anxiety Disorder (GAD) have emphasized interpersonal and personality functioning as important aspects of the disorder. The current paper examines heterogeneity in interpersonal problems in two studies of individuals with GAD (n = 47 and n = 83). Interpersonal subtypes were assessed using the Inventory of Interpersonal Problems (IIP-C; Alden, Wiggins, & Pincus, 1990). Across both studies, individuals with GAD exhibited heterogeneous interpersonal problems, and cluster analyses of these patients' interpersonal characteristics yielded four replicable clusters identified as intrusive, exploitable, cold, and nonassertive subtypes. Consistent with our pathoplasticity hypotheses, clusters did not differ in GAD severity, anxiety severity, depression severity. Clusters in study two differed on rates of personality disorders, including avoidant personality disorder, further providing support for the validity of interpersonal subtypes. The presence of interpersonal subtypes in GAD may have important implications for treatment planning and efficacy.
Recent conceptualizations of Generalized Anxiety Disorder (GAD) have identified maladaptive interpersonal problems as central to the diagnosis (e.g., Newman & Erickson, 2010). Maladaptive interpersonal functioning overlaps considerably with conceptualizations of personality problems, as both can be viewed as disturbances of the self and interpersonal relationships (Pincus, 2005; Sullivan, 1953). Consistent with this overlap, some have suggested that the diagnosis of GAD may actually reflect a disturbance of personality (Beck, Stanley, & Zebb, 1996; Newman & Erickson, 2010). Like personality disturbances, GAD tends to have a lifelong duration (Rapee, 1985), chronic course (Wittchen & Hoyer, 2001), and typical age of onset during early adulthood (Hoehn-Saric, Hazlett, & McLeod, 1993). Also, nearly 50% of individuals with GAD may be diagnosed with a comorbid Axis II diagnosis (Sanderson, Wetzler, Beck, & Betz, 1994).
Studies of temperament, considered to be an infant manifestation of personality traits (Buss & Plomin, 1975; Rothbart, 1989), suggest that compared with individuals who do not develop anxiety disorders, those who develop anxiety disorders demonstrate more fearful, anxious, and avoidant behaviors in early childhood (Biederman, Rosenbaum, Chaloff, & Kagan, 1995). Attachment styles, often conceptualized as the basis for ingrained lifelong interpersonal styles, have also been associated consistently with GAD (e.g., Cassidy, Lichtenstein-Phelps, Sibrava, Thomas, & Borkovec, 2009; Cassidy & Shaver, 1999). In fact, a form of insecure attachment, anxious attachment, is associated with worry and magnification of threats (for a review see Mikulincer & Shaver, 2007), characteristics fundamental to the experience and presentation of GAD. Thus, personality disturbance and GAD may be inherently linked, and examining dimensions of personality functioning may enhance clinical understanding of GAD.
Interpersonal functioning is also the most common worry topic for GAD patients (Breitholtz, Johansson, & Ost, 1999; Roemer, Molina, & Borkovec, 1997). GAD is more strongly associated with marital conflict and dissatisfaction than any other anxiety or mood disorder (McLeod, 1994; Whisman, Sheldon, & Goering, 2000). Individuals with GAD tend to have few friends (Whisman, et al., 2000), have biased social judgment regarding their negative impact on others (Erickson & Newman, 2007), and view themselves as less effective in interpersonal relationships than others (Eng & Heimberg, 2006; Erickson & Newman, 2007).
The Interpersonal Circumplex Model
The “interpersonal tradition” conceptualizes personality as “the relatively enduring pattern of recurrent interpersonal situations that characterizes a human life” (Sullivan, 1953 pp. 110-111). This approach uses a two-dimensional model to measure interpersonal motivations, as well as normal and abnormal interpersonal dispositions and behaviors (Horowitz, 2004; Wiggins, 2003). Agency/Dominance and Communion/Love are the two orthogonal axes at the center of a circular Euclidean space defining the interpersonal circumplex (IPC; Leary, 1957; Wiggins, 1996). Dominance refers to individuation, autonomy, and directedness, whereas Love refers to associating, involvement with, and sharing with others.
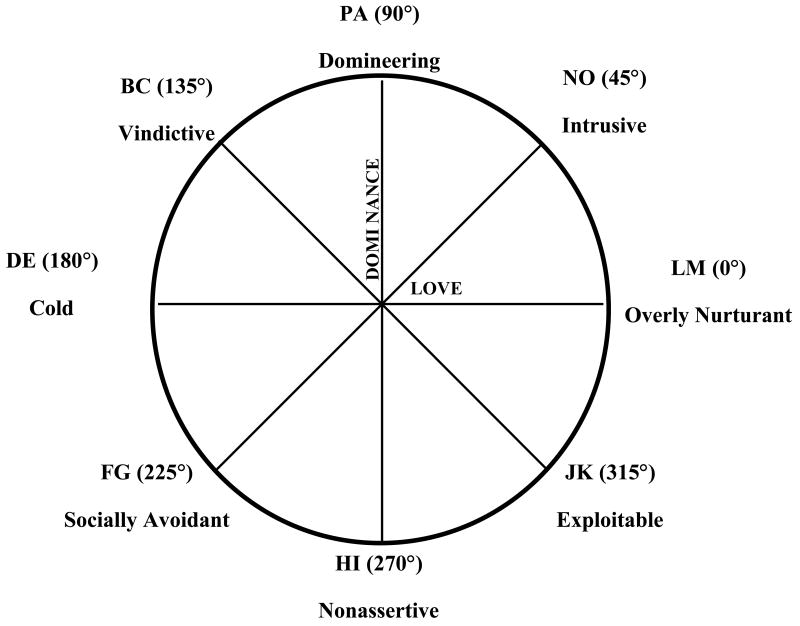
One interpersonal circumplex model is the Inventory of Interpersonal Problems Circumplex (IIP-C; Alden, et al., 1990; see Figure 1). The two dimensions of Dominance and Love anchor the IIP-C model and are associated with more problematic manifestations of interpersonal behavior. The poles of the agentic axis are Domineering vs. Nonassertive, whereas the poles of the communal axis are Cold vs. Overly-nurturant. The IIP-C allows for the location of individual or group data in the interpersonal problem space.
Figure 1. Interpersonal Circumplex.
Data on the IIP-C can be analyzed in a number of different ways. The simplest way is via scores on the axes (Dominance vs. Nonassertive and Cold vs. Overly-Nurturant), lower-order octant scores located around the circumplex, and total interpersonal problems score. Using this scoring method, individuals with GAD have reported more total interpersonal problems and higher scores on the nonassertive, exploitable, overly-nurturant, and intrusive problem subscales relative to non-anxious control participants (Eng & Heimberg, 2006). However, octant scores provide broad information regarding a group or individual's interpersonal problems without providing information regarding what problems are primary or the level of the individual's distress.
As opposed to octant scores, the structural summary method (Gurtman, 1994; Gurtman & Pincus, 2003) plots interpersonal data on a sinusoidal curve and provides information about the location of primary interpersonal problems within the circumplex, level of interpersonal distress, distinctiveness of primary interpersonal problem, and prototypicality of the data (Wright, Pincus, Conroy, & Hilsenroth, 2009). This method also provides information on measurement error or whether the data accurately represents the group. As such, the structural summary method provides much more detailed and clinically useful information regarding interpersonal problem subtypes in individuals and groups of individuals than octant scores.
Whereas some forms of psychopathology can be summarized by relatively uniform interpersonal features across similarly diagnosed patients, others seem to have a kaleidoscopic relationship with the interpersonal system, wherein personality and psychopathology intertwine to produce phenotypic variability in expression of the disorder. This interrelationship between an Axis I diagnosis and personality has been labeled interpersonal pathoplasticity.
Interpersonal Pathoplasticity
Interpersonal pathoplasticity refers to a mutually influencing, but non-etiological, relationship between the interpersonal system and psychopathology (Klein, Wonderlich, & Shea, 1993; Widiger & Smith, 2008). Pathoplasticity is thus part of the inextricable link between personality and psychopathology; the latter is always expressed within the larger context of the former (Millon, 2005), and it would be unreasonable to assume that the expression of pathology would not be influenced by one's characteristic manner of relating to others (and vice versa). Thus, pathoplasticity theory suggests that although individuals diagnosed with GAD may experience many of the same worry-related symptoms, based on dispositional tendencies, subgroups of individuals might cope with or act on these symptoms in different ways insofar as their interpersonal behavior is concerned. For example, an intrusive and warm individual with GAD may exhibit worry regarding others' health and safety through repeated expressions of concern about family members. Cold and intrusive individuals with GAD may express concerns for others' safety by criticizing what they view as reckless behavior. Although both individuals have similar worries, the manifestation of their worries is different, as is the impact of their worries on others. Information from the assessment of such interpersonal tendencies is distinct from information regarding the symptoms of Axis I diagnoses, and thus provides additional helpful clinical information about a particular individual and treatment of their symptoms. A pathoplastic model would suggest that although GAD and interpersonal functioning are distinct, they are mutually influencing; therefore, to truly understand the manifestation of individuals' GAD symptoms and psychological functioning and to identify the most appropriate treatment, it is essential to identify individuals' interpersonal subtype.
Demonstrations of a pathoplastic relationship between an Axis I diagnosis and interpersonal factors require the following: (a) distinct interpersonal subtypes in individuals with a primary Axis I diagnosis, (b) subtype classification cannot be accounted for by the symptom severity of the primary Axis I diagnosis, differential Axis I comorbidity, general interpersonal distress and (c) interpersonal factors, such as personality disorder symptoms and attachment, are associated differentially with interpersonal subtypes. Interpersonal pathoplasticity, as measured using the IIP-C, has only been examined in three studies of samples with anxiety disorders (Cain, Pincus, & Grosse Holtforth, 2010; Kachin, Newman, & Pincus, 2001; Salzer et al., 2008), with only one study examining interpersonal pathoplasticity in individuals with DSM-IV GAD (Salzer, et al., 2008).
In a German sample, Salzer and colleagues (2008)i identified four interpersonal subtypes: Intrusive, Cold, Nonassertive, and Exploitable. Clusters did not differ in gender composition, comorbid mood and anxiety disorders, or severity of anxiety and mood symptoms, supporting the application of a pathoplastic relationship between interpersonal problems and GAD. However, this study was limited by methodological concerns.
First, clusters were built using centroids of clusters from unpublished studies, rather than being derived independently. This methodology does not permit derivation of clusters that match the data best. Indeed, in Salzer and colleagues (2008) the circumplex profile of the intrusive cluster was not prototypical (R2 = .65), indicating that structural summary scores may not adequately represent data in this cluster (Wright, et al., 2009). This highlights the importance of data driven cluster derivation. Second, these authors excluded individuals who met criteria for eating disorders, major depression, or borderline personality disorder in the last year, or any Cluster A Axis II personality disorder. Given the high degree of comorbidity in GAD with many of these disorders (Newman, Przeworski, Fisher, & Borkovec, 2010; Sanderson, et al., 1994), these exclusion criteria limit the generalizability of their findings. Further, excluding individuals with Cluster A Axis II personality disorders and borderline personality disorder may have impacted the interpersonal styles reported in their sample. For example, schizoid personality disorder is often associated with IPC octants FG and HI (extreme and rigid introversion and submissiveness; Horowitz et al., 2006); therefore excluding this personality disorder may decrease the number of individuals reporting interpersonal problems in these octants. Indeed, in Salzer and colleagues (2008) sample only 10.5% fell in the nonassertive cluster.
Further, Salzer and colleagues (2008) study was conducted in Germany and interpersonal behavior can be culturally dependent (Triandis, Tanaka, & Shanmugam, 1966). Therefore, it is possible that different results would be identified in a sample collected in the United States. Affiliation/intimacy (Communion) and dominance/submissiveness (Agency) have been identified as universal dimensions of interpersonal behavior regardless of culture (Triandis, 1994; Wiggins, 1991); however, the particular association between these dimensions and GAD may differ cross-culturally.
In addition, Salzer and colleagues did not assess reliability of GAD diagnoses, which is important given that inter-rater agreement of GAD is lower than for other anxiety disorders (Brown, Campbell, Lehman, Grisham, & Mancill, 2001). Salzer and colleagues (2008) also neither provided information regarding rates of Axis II diagnoses in their sample, nor examined whether their interpersonal clusters of GAD patients differed in Axis II comorbidity. Given that 45% of the diagnostic criteria for personality disorders in the DSM are dysfunctional interpersonal behaviors (Pilkonis, 2002), and some personality disorders are associated with particular octants on the interpersonal circumplex (Horowitz, et al., 2006), one may expect to find differential rates of personality disorders in interpersonal clusters of GAD patients.
Salzer and colleagues (2008) also did not examine whether clusters differed in attachment, which has often been conceptualized as the basis for interpersonal behaviors. Insecure attachment is associated with GAD (Cassidy, et al., 2009) and associations between interpersonal problems and attachment have been found in unselected samples (Chen & Mallinckrodt, 2002; Horowitz, Rosenberg, & Bartholomew, 1993). Therefore, a pathoplastic model would predict that interpersonal subtypes would differ on various attachment variables.
The purpose of the current series of studies is to extend Salzer and colleagues (2008) findings to two treatment-seeking US samples of individuals with GAD. The current studies examined (a) interpersonal subtypes based on independently derived clusters in two samples of GAD and (b) the presence/absence of a pathoplastic association between GAD and interpersonal subtypes via comparison of clusters on symptom severity, Axis I and Axis II comorbidity and attachment styles. It was hypothesized that (a) homogenous intrusive, cold, nonassertive, and exploitable interpersonal subtypes would be reliably identified and differ on IIP-C scores in a manner consistent with the IPC model, and (b) a pathoplastic relationship would be demonstrated between interpersonal style and GAD such that interpersonal subtypes of GAD would not differ in symptom severity, broad measures of anxiety and depression, or Axis I comorbidity, but would exhibit substantively understandable differences in interpersonal variables such as Axis II comorbidity and attachment.
Study 1
Method
Participants
Forty-seven individuals with GAD who were recruited as part of a treatment outcome study (Borkovec, Newman, Pincus, & Lytle, 2002) participated. They completed a half-hour phone interview, a battery of self-report questionnaires, and an in-person diagnostic interview, which included the Anxiety Disorders Interview Schedule-Revised (ADIS-R; Di Nardo & Barlow, 1988), a clinical severity rating (CSR), the Hamilton Anxiety Rating Scale (HARS; Hamilton, 1959) and the Hamilton Depression Rating Scale (HDRS; Hamilton, 1960). An independent ADIS-R was given within 2 weeks of the first interview. Participants were admitted only if both interviewers agreed that GAD was the primary diagnosis and gave a CSR of 4 or higher. Participants were excluded if they met criteria for panic disorder, had other ongoing psychosocial therapy, had previously received an adequate trial of cognitive-behavioral treatment (CBT), had medical contributions to anxiety symptoms, were taking an antidepressant medication, or had severe depression, substance abuse, psychosis, or organic brain syndrome.
Participants ranged in age from 18-65 years old (M = 39.43, SD = 12.32). Sixty-five percent of the sample was female. The sample was 87.2% Caucasian, 5.1% Latino, 5.1% Indian, and 2.6% African American. Approximately 4% were on psychotropic medications.
Measures
Inventory of Interpersonal Problems—Circumplex (IIP-C; Alden, et al., 1990)
This 64-item scale assesses interpersonal dysfunction based on the interpersonal circumplex model. Respondents rate distress experienced in relation to a variety of interpersonal deficits (e.g., “It is hard for me to show affection to other people”) and excesses (e.g., “I open up to people too much”) on a 0 (no distress) to 4 (extremely distressing) scale. Eight subscales correspond to the octants of the IPC including (too) domineering, vindictive, cold, socially-avoidant, nonassertive, exploitable, overly nurturant, and intrusive. The IIP-C has good retest reliability (total r = 0.98; average subscale r = 0.81) and reliability for the octant scales (αs ranging from 0.72-0.85), and shows strong convergence between self-, therapist-, and peer-rating profiles (Alden & Phillips, 1990; Horowitz, Rosenberg, Baer, Ureño, & Villaseñor, 1988; Kachin, et al., 2001). Internal consistency in the current sample was excellent (α =.92).
Perceptions of Adult Attachment (PAAQ; Lichtenstein & Cassidy, 1991)
This 60-item measure assesses retrospective report and current views of childhood relationships with a primary caregiver. Items are rated on a five-point scale ranging from 1 (strongly disagree) to 5 (strongly agree). It has three theoretically and factor analytically-derived subscales: rejection/neglect (e.g., “When I was a child, my mother sometimes told me that if I was not good, she would stop loving me”), being loved (e.g., “In childhood I felt like I was really treasured by my mother”), and role-reversal/enmeshment (e.g., “I often felt responsible for my mother's welfare”), as well as five scales reflecting current view of attachment: vulnerable (e.g., “My mother's issues are still interfering with my life”), balancing/forgiving (e.g., “Even with all our past difficulties, I realize my mother did the best for me that she could”), angry (e.g., “No one gets under my skin like my mother”), dismissing/derogating (e.g., “My family was not particularly intimate, but this has never bothered me”), and lacking in memory (e.g., “I have forgotten what most of my early childhood was like”) (Lichtenstein & Cassidy, 1991). Subscales show good internal consistency (α = .72 in the current sample), retest reliability and construct validity (Cassidy, et al., 2009; Lichtenstein & Cassidy, 1991).
Anxiety Disorders Interview Schedule-III-R (ADIS-R; Di Nardo & Barlow, 1988)
This structured interview assesses DSM diagnoses of anxiety disorders, mood disorders, substance abuse, and psychosis. Interviewers also complete a clinical severity rating (CSR), ranging from 0 (none) to 8 (very severe) for each diagnosis. A rating of 4 or above indicates the presence of the diagnosis. Twenty percent of pre-treatment interview audiotapes randomly chosen for reliability purposes indicated excellent agreement for specific diagnoses with kappa coefficients ranging from .68 (Social Phobia) to 1.0 (GAD, Dysthymia and Specific Phobia).
Hamilton Anxiety Rating Scale (HARS; Hamilton, 1959)
This 14-item clinician administered scale assesses the severity of anxiety. Internal consistency (α = .92), retest reliability (ICC = .86) and interrater-reliability (ICCs of .74 -.96) are all good (Bruss, Gruenberg, Goldstein, & Barber, 1994; Kobak, Reynolds, & Greist, 1993).
Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960)
This 13-item clinician administered scale of depression has good internal consistency (α = .73 to .81), interrater reliability (.78 - .82), convergent and discriminant validity (Moras, Di Nardo, & Barlow, 1992; Steer, McElroy, & Beck, 1983).
Data Analysis Strategy
The structural summary method is the most comprehensive way of summarizing IIP-C data (Gurtman, 1994; Gurtman & Balakrishnan, 1998; Gurtman & Pincus, 2003). This method uses a sinusoidal profile, which can be summarized by profile elevation, amplitude, angular displacement, and goodness of fit (Gurtman & Balakrishnan, 1998). Elevation, the mean level of the profile, represents mean interpersonal distress of all eight IIP-C subscales (Tracey, Rounds, & Gurtman, 1996). Amplitude, the difference between the mean and peak value, represents degree of profile differentiation, with higher amplitude reflecting more distinct ratings of interpersonal problems that are distressing relative to those that are not distressing to the respondent. An amplitude value of 0 indicates a flat (i.e., undifferentiated) profile; high amplitude indicates a profile with a clear interpersonal peak and trough (Gurtman & Balakrishnan, 1998). Angular displacement (Θ) is the angular distance from 0° for the peak of the curve, representing the section of the circumplex with the individual's most salient interpersonal problems. Goodness of fit (R2) indicates profile prototypicality, meaning how well scores for octants of the profile fit a perfect cosine curve (and therefore the degree of correspondence to circumplex theory). An R2 <.70 reflects a complex profile in which the information cannot be represented accurately by the profile's elevation, amplitude, and displacement (Wright, et al., 2009).
Structural summary scores may also be calculated for an entire group (Wright, et al., 2009). These scores represent the entire group's averaged octant scores. Elevation scores indicate the level of interpersonal distress for the group as a whole. Amplitude scores indicate degree of group differentiation of the dominant interpersonal problem from other interpersonal problems on the circumplex. Low amplitude indicates no identifiable peak in the group. Instead, the cosine profile is flattened, reflecting few distinct interpersonal problems in the group. Angular displacement represents the section of the circumplex with the group's most salient interpersonal problems. R2 indicates how well the entire group's data fits a cosine curve, and therefore, how well elevation, amplitude, and displacement represent the group's data. A poor group fit may be indicative of measurement error, heterogeneity of individual profiles composing the group, or profiles that are homogenous but which violate circumplex assumptions. Analyses examining individual profile prototypicality and the presence of interpersonal subtypes can help to determine the reason for undifferentiated IIP-C profiles (Wright, et al., 2009).
Pathoplasticity Analyses
After examining the sample structural summary profile, a series of cluster analyses was conducted on IIP-C data to determine whether non-random interpersonal variation in GAD clients was present.ii Presence of distinct interpersonal clusters provides initial support for a pathoplastic relationship between GAD and interpersonal problems. Using recommendations of Milligan (1980). the sample was first cluster analyzed using Ward's hierarchical clustering procedure with the squared Euclidean distance measure. To confirm the final cluster solution, the K-Means procedure with the squared Euclidean distance measure was conducted.iii Structural summary parameters were compared across GAD clusters using analyses of variance. Subsequent multivariate analyses of variance (Wilks Lambda) compared participants' cluster membership on GAD severity, Hamilton depression and anxiety scales, and rates of comorbid Axis I diagnoses. Multivariate analyses of variance also compared participants' cluster membership on PAAQ scales. Bonferroni corrections were used only in instances where we predicted differences across clusters.
Results
Using the structural summary method to analyze group level scores, the angular displacement for the GAD group fell at 301.9° on the circumplex, placing them in the JK (exploitable) octant. Elevation was 0.62 indicating moderate interpersonal distress.
Hypothesis 1
Intrusive, cold, nonassertive, and exploitable interpersonal subtypes will be identified and will differ on IIP scores in a manner consistent with the IPC model As expected, group amplitude (.27) and R2 (.69) indicated low profile protoypicality, suggesting that angular locations, elevation, and amplitude scores cannot sufficiently represent the groups. To examine whether this low prototypicality was due to true interpersonal heterogeneity, cluster analyses were conducted based on scores on the IIP-C dimensions of Dominance and Love.
A clear four-cluster solution was revealed by the agglomeration schedule and dendogram produced by the Ward's procedure and was also replicated by the K-means procedure. Across procedures, 75% of those in Ward's cluster 1 were also in K-Means cluster 1, 93% of those in Ward's cluster 2 were also in K-Means cluster 2, 100% of those in Ward's cluster 3 were also in K-Means cluster 3, and 90% of those in Ward's cluster 4 were also in K-Means cluster 4. Highly convergent angular locations were found for the four clusters across the Ward's and K-Means solutions: Cluster 1 (44.33°/39.02°), Cluster 2 (320.83°/317.95°), Cluster 3 (168.07°, 165.20°), and Cluster 4 (248.38°/249.55°). Thus, across both procedures, the clusters consistently fell into the intrusive (NO) octant, the exploitable (JK) octant, the cold (DE) octant, and the nonassertive (HI) octant. The K-Means solution was chosen as the final cluster solution and used in subsequent validation analyses.
Examining Group-Level IIP-C Structural Summaries
Group level structural summary scores were calculated for the clusters. The intrusive (R2 = .92; Θ = 39.02°; amp = .75; e = .77), exploitable (R2 = .90; Θ = 317.95°; amp = .68; e = .70), nonassertive (R2 = .99; Θ = 249.55°; amp = 1.26; e = .42), and cold (R2 = .83; Θ = 165.20°; amp = .49; e = .51) clusters all exhibited highly prototypical interpersonal styles with moderate to large problem differentiation and notable interpersonal distress. Each of the clusters had higher group R2 and group level amplitude than the full GAD sample, indicating that individuals within clusters reported distinct interpersonal problems. The decrease in group R2 and group amplitude scores, which occurred when clusters were combined into a single sample, demonstrated that this variation was lost when examined as a combined group.
Comparing GAD Clusters on the IIP-C
Comparisons of each of the final clusters on elevation (interpersonal distress) yielded no significant differences (F(3,43) = .592, p = .623, η2p = .04) whereas comparisons on amplitude (profile differentiation) indicated significant differences (F(3,43) = 7.69, p < .0003, η2p = .349. Those in the nonassertive cluster had significantly higher amplitude scores than those in the cold and exploitable clusters (ps < .002)(see Table 1), indicating more distinct distressing interpersonal problems in the nonassertive cluster than in the cold or exploitable clusters. Omnibus comparisons of the four clusters on Dominance, Love and octant scores were also significant (ps < .008; as shown in Table 1), exhibiting the expected pattern of differences. Thus, suggesting that each of the clusters reflected distinct interpersonal problems.
Table 1. Study 1: Comparison of GAD Clusters.
| Study 1: Comparisons of Final Four GAD Clusters. | Intrusive Cluster (N = 13) |
Exploitable Cluster (N = 15) |
Cold Cluster (N = 10) |
Nonassertive Cluster (N = 9) |
F-value | η2p |
|---|---|---|---|---|---|---|
| Elevation | 0.77a | 0.70a | 0.51a | 0.42a | .592 | .040 |
| Amplitude | 0.81ab | 0.74a | 0.60a | 1.32b | 7.69* | .349 |
| Octants: | F-value | |||||
| PA (Domineering) | 1.33a | 0.28b | 0.39ab | -0.76c | 15.34* | .517 |
| BC (Vindictive) | 0.56a | 0.16a | 1.18a | -0.02a | 3.25 | .185 |
| DE (Cold) | 0.18a | 0.05a | 1.04a | 0.85a | 3.61 | .201 |
| FG (Socially-Avoidant) | -0.06a | 0.49ab | 0.51ab | 1.43b | 4.72* | .248 |
| HI (Nonassertive) | 0.60a | 1.49a | 0.47a | 1.69a | 4.67 | .246 |
| JK (Exploitable) | 0.65a | 1.28a | 0.18a | 1.09a | 3.78 | .209 |
| LM (Overly-Nurturant) | 1.21a | 1.10ab | -0.02bc | -0.21c | 8.83* | .381 |
| NO (Intrusive) | 1.67a | 0.74abc | 0.32abc | -0.68c | 9.87* | .408 |
| Axes: | ||||||
| Dominance | 0.47a | -0.46 | 0.12a | -1.18 | 49.40* | .775 |
| Love | 0.58a | 0.50a | -0.48b | -0.44b | 32.02* | .691 |
Note:
Values sharing superscripts across rows are not statistically significant.
p<.006
Hypothesis two: There is a pathoplastic relationship between GAD and interpersonal subtypes
The predicted result showing nonsignificant differences between IIP-C clusters on elevation, provides necessary, but not sufficient evidence for the pathoplasticity of GAD. To further evaluate this hypothesis, clusters were compared on symptom severity, attachment style, and comorbid diagnoses. As predicted, the four clusters were neither significantly different from one-another (F(3,36) = .24, p = .87, η2p = .02) on GAD severity (as indicated by the CSR rating on the ADIS; Intrusive M = 5.54, SD = 1.16; Exploitable M = 5.32, SD = 1.03; Cold M = 5.46, SD = .82; Nonassertive M = 5.7, SD = .91), nor did they differ from one another on the HARS (Intrusive M = 26.46, SD = 6.15; Exploitable M = 25.05, SD = 6.84; Cold M = 27.71, SD = 11.40; Nonassertive M = 26.06, SD = 7.10) and HRSD (Intrusive M = 15.19, SD = 6.33; Exploitable M = 12.14, SD = 6.00; Cold M = 19.29, SD = 9.11; Nonassertive M = 13.94, SD = 5.02) (F(6,70) = .93, p = .48, η2p = .074). A Fisher's exact test for overall rates of comorbidity did not show a significant difference between clusters (p = .17); however, there were low rates of various comorbid diagnoses, including dysthymia, OCD, and PTSD; which could have contributed to this finding. Social phobia was the most common comorbid diagnosis in this sample (38.3%), followed by specific phobia (12.77%). As predicted, Fisher's exact tests revealed no significant differences between clusters in rates of social (p = .07) and specific phobia (p = .28), although there was a trend towards significance for social phobia. Contrary to prediction, an omnibus test of attachment did not show significant differences between the clusters (F(24, 82) = .77, p = .76, η2p = .179), although there was a large effect size.iv.
Study 1 Discussion
Results support a pathoplasticity model of GAD. Participants were not homogenous in interpersonal problems and four prototypical interpersonal subtypes were reliably derived: an intrusive subtype, exploitable subtype, cold subtype, and nonassertive subtype. Categorizing individuals with GAD into these subtypes more accurately fit the data than considering the interpersonal characteristics of GAD as a unified diagnostic group. Support indicating a pathoplastic relationship was found between GAD and interpersonal problems, and as predicted, interpersonal subtypes did not differ from one another in level of interpersonal distress, severity of GAD or other symptoms, or Axis I comorbidity. This suggests that interpersonal dimensions may provide new diagnostic information, above and beyond Axis I symptom measures.
Contrary to our hypothesis, there were no significant differences in attachment variables across interpersonal subtypes; however, the result demonstrated a large effect size. Because effect sizes are independent of sample size it is possible that the discrepancy between the p-value and the effect size is due to sample size. Alternatively, it is possible that the maladaptive attachment variables assessed in the current study were associated with more than one subtype of interpersonal problems. For example, an individual who does not perceive that he/she was loved during childhood may not desire interpersonal relationships or be somewhat cold in these relationships or could respond by being overly warm and nurturing in relationships out of anxiety that the relationship will end. The specific attachment variables examined in the current study have neither been examined in relation to IIP variables in the past, nor have they been compared to attachment styles that have previously been associated with specific IIP octants.
Results of this study, replicated those of Salzer et al. (2008), however, in the current study, clusters were more evenly divided among participants with 27.7% falling in the intrusive cluster, 31.9% in the exploitable cluster, 21.28% in the cold cluster, and 19.15% in the nonassertive cluster. In contrast, Salzer and colleagues (2008) found a relatively small percentage in the intrusive cluster (14.5%), over 50% in the exploitable cluster (52.6%), 22.4% in the cold cluster, and only 10.5% in the nonassertive cluster. This may be due to their exclusion of individuals with Cluster A Axis II diagnoses, such as schizoid personality disorder, which is associated with interpersonal problems in the hostile submissive quadrant, a quadrant where the nonassertive cluster fell (only 10.5% of the Salzer et al, 2008 sample) and exclusion of other disorders, such as eating disorders and borderline personality disorder.
In the current study participants with GAD were excluded for the presence of severe major depressive disorder and panic disorder, which also limits the generalizability of the findings. Further, the sample size for the current study was somewhat small (47 individuals with GAD). The use of a larger sample with fewer exclusion criteria could provide more generalizable findings. Additionally, only Axis I comorbidity and attachment were assessed. As nearly 50% of individuals with GAD have comorbid personality disorders (Sanderson, et al., 1994), examination of rates of personality disorders within different interpersonal subtypes provides a richer understanding of the functioning of GAD patients.
Study 2
The purpose of study 2 was to replicate and extend the results of study 1 in a larger and more generalizable sample of individuals with GAD (n = 83). In this study, participants were not excluded for the presence of severe major depressive disorder or panic disorder, and Axis II comorbidity was examined across clusters to provide additional information regarding the functioning of individuals with GAD.
Method
Participants
Participants were recruited in the same manner as in Study 1; however, they were not excluded for comorbid severe major depression or panic disorder. Eighty-three individuals with GAD were part of two larger treatment outcome studies, one which was an open trial of an integrative psychotherapy (Newman, Castonguay, Borkovec, Fisher, & Nordberg, 2008), and one which was a randomized controlled trial of the integrative psychotherapy versus CBT plus supportive listening (Newman et al., in press). Participants ranged in age from 18-65 years old (M = 38.21, SD = 11.82). Women comprised 74.7% of the sample. The sample was 92.8% Caucasian, 2.4% Latino, 3.6% Asian, and 1.2% African American. Thirty two percent of participants were on psychotropic medications.
Measures
Subjects completed the same assessment battery as in study one except that the Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV; Brown, Di Nardo, & Barlow, 1994) and the Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II; First, Gibbon, Spitzer, Williams, & Benjamin, 1997) were administered. As in study one, two independent assessors administered the ADIS to ensure a primary diagnosis of GAD. Kappa agreement for the current interviewers was .78 for the presence of GAD and .68-1 for comorbid diagnoses. For each current diagnosis, interviewers assigned a 0-8 Clinicians' Severity Rating (CSR) indicating the degree of distress and interference in functioning associated with the disorder (0 = none to 8 = very severely disturbing/disabling). Reliability of client severity ratings for GAD using Finn's r (Whitehurst, 1984), which corrects for a restricted range, was .74.v There was also very good agreement on CSRs of comorbid disorders with intraclass correlations ranging from .77 to 1. For the HARS (α = . 87 and ICC = .89) and HRSD (α = .78 and ICC = .86), internal consistency and interrater reliability were very good. Internal consistency was also good for the IIP (α = .95) and PAAQ (α = .70).
With respect to diagnoses of personality disorders, participants first completed the SCID-II screening questionnaire. An interviewer then completed the SCID II interview modules for which participants endorsed symptoms on the screening questionnaire. Inter-rater reliability is generally adequate for the SCID II (Cohen's K ranging from .48-.98 for categorical diagnoses; Maffei et al., 1997), but for our raters was good to excellent across personality disorder diagnoses (kappas ranging from .64 to 1.0).
Data Analytic Plan
The same data analytic strategy that was employed in study one was used.
Results
Hypothesis one
Intrusive, cold, nonassertive, and exploitable interpersonal subtypes will be identified and will differ on IIP scores in a manner consistent with the IPC model We again used the structural summary method for analyzing circumplex data to examine group profiles. Angular displacement fell at 260.34° on the circumplex, which is in the HI (Nonassertive) Octant. However, group amplitude (.26) and R2 (R2 = .63) indicated that the GAD group is not prototypical, and therefore the angular displacement, elevation, and amplitude are not representative of the sample.
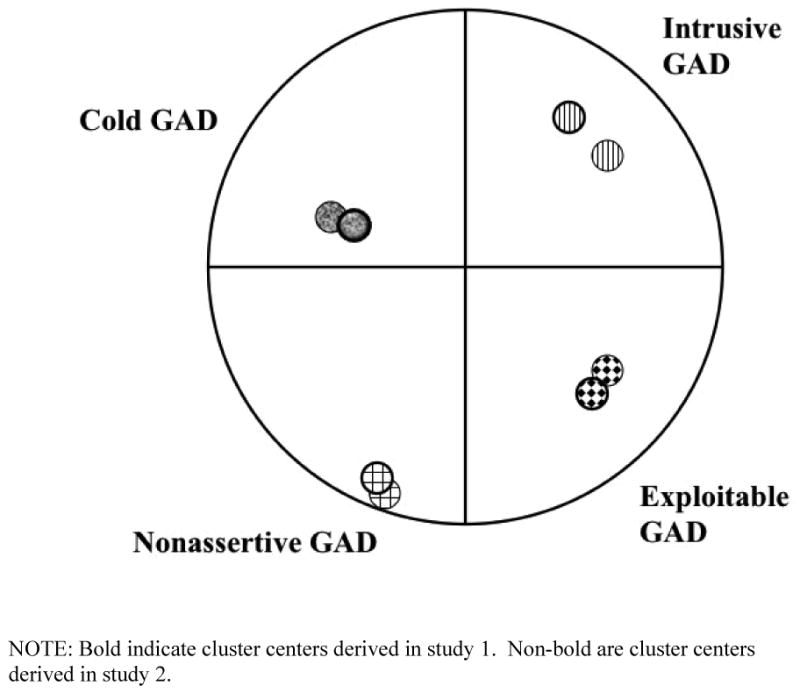
Patients were cluster analyzed based on the IIP-C dimensions of Dominance and Love. As in study one, the first discontinuity in the agglomeration schedule produced by the Ward's procedure occurred when four clusters were combined into three, suggesting a latent four-cluster solution which converged well with Study 1. Given the degree of convergence between the cluster center placements from Study 1 and Study 2, and the more rigorous method of identifying clusters used in Study 1, cluster centers from the final cluster solution in Study 1 were entered as the starting values for the final K-Means cluster solution in Study 2 and results were highly convergent across samples (See Figure 2).
Figure 2. Cluster centers derived in Studies 1 and 2.
Examining Group-Level IIP-C Structural Summaries
The intrusive (R2 = .87; Θ = 51.41°; amp = .80; e = .40), exploitable (R2 = .77; Θ = 308.41°; amp = .75; e = .33), nonassertive (R2 = .99; Θ = 251.73°; amp = 1.18; e = .62), and cold (R2 = .78; Θ = 165.93°; amp = .39; e = .31) clusters exhibited highly prototypical interpersonal styles with moderate to large problem differentiation and moderate interpersonal distress. Consistent with study 1, each cluster has higher group R2 and amplitude than the full GAD sample, indicating that the clusters are more prototypical and differentiated than is the group as a whole. The reliability of angular displacement of clusters across studies demonstrates that there is not a random distribution of interpersonal problems. Instead, interpersonal problems of individuals with GAD fall into reliable subtypes—intrusive, exploitable, cold, and nonassertive with each cluster reporting distinct interpersonal problems.
Comparing GAD Clusters on the IIP-C
Consistent with study 1, there were no differences between the four clusters on IIP-C elevation (distress; F(3,79) = .64, p = .591; η2p = .024); however, clusters differed on amplitude (profile differentiation; F(3,79) = 12.01, p<.00001, η2p = .313). Similar to Study 1, those in the nonassertive cluster had significantly higher amplitude scores than those in all other clusters (ps <.005) except the intrusive cluster (p = .06) (see Table 2). This indicates that the nonassertive cluster had more distinct distressing interpersonal problems than the other clusters, except the intrusive cluster. Omnibus comparisons of the four clusters on Dominance and Love scores and on octant scores were also significant (ps <.001as shown in Table 2). Consistent with Study 1, these scores exhibited the expected pattern of differences, confirming that individuals within each of the clusters were reporting distinct interpersonal subtypes.
Table 2. Study 2: Comparison of GAD Clusters.
| Intrusive Cluster (N = 14) |
Exploitable Cluster (N = 18) |
Cold Cluster (N = 31) |
Nonassertive Cluster (N = 20) |
F-value | η2p | |
|---|---|---|---|---|---|---|
| Elevation | .40a | .33a | .31a | .62a | .641 | .024 |
| Amplitude | .89ab | .80a | .57a | 1.25b | 12.01*** | .313 |
| Octants: | F-value | |||||
| PA (Domineering) | 1.31a | -.10bc | .61ab | -.43c | 11.63*** | .306 |
| BC (Vindictive) | 0.32a | -.08a | .61a | .23a | 1.69 | .060 |
| DE (Cold) | -0.30ab | -.31a | .72ab | .86b | 6.98*** | .209 |
| FG (Socially-Avoidant) | -0.33a | -.003a | .28a | 1.64 | 14.67*** | .358 |
| HI (Nonassertive) | 0.08a | 1.37bc | .43ab | 1.80c | 12.05*** | .314 |
| JK (Exploitable) | 0.22abc | 1.04bc | -.01a | 1.15c | 8.04*** | .234 |
| LM (Overly-Nurturant) | 0.57a | .84a | -.11a | .33a | 3.08 | .105 |
| NO (Intrusive) | 1.34a | -.12b | -.06b | -.62b | 9.82*** | .272 |
| Axes: | ||||||
| Dominance | .62 | -.59 | .10 | -1.12 | 65.70*** | .714 |
| Love | .50a | .47a | -.38b | -.37b | 31.10*** | .542 |
Note:
Values sharing superscripts across rows are not statistically significant.
p < .001
Hypothesis two: There is a pathoplastic relationship between GAD and interpersonal subtypes
Consistent with our hypotheses, we found 4 interpersonally distinct clusters of GAD individuals with similar levels of interpersonal distress. As noted earlier, this provides necessary but not sufficient evidence for pathoplasticity. To further evaluate this hypothesis, we examined the clusters on symptom severity, psychiatric comorbidity, and attachment. As predicted, there were no differences across the four clusters on GAD severity (as indicated by the CSR rating on the ADIS) (Intrusive M = 6.36, SD = 1.01; Exploitable M = 5.97, SD = .74; Cold M = 5.92, SD = .84; Nonassertive M = 6.28, SD = .64; F(3,79) = 1.46, p = .23, η2p = .052), HARS (Intrusive M = 24.91, SD = 7.09; Exploitable M = 25.72, SD = 5.83; Cold M = 21.44, SD = 7.18; Nonassertive M = 24.40, SD = 6.69) or HRSD Intrusive M = 19.18, SD = 7.15; Exploitable M = 18.56, SD = 6.78; Cold M = 16.56, SD = 8.83; Nonassertive M = 15.95, SD = 4.22; F(6,156) = 1.28, p = .270, η2p = .047). Frequency of Axis I comorbid diagnoses are presented in Table 3. A Fisher's exact test comparing the clusters on presence vs. absence of any Axis I comorbid diagnosis was nonsignificant but indicated a trend toward significance (p = .07). Percentages with comorbid Axis I diagnoses within the intrusive, exploitable, cold and nonassertive clusters were 78.6% (n = 11), 83.3% (n = 15), 64.5% (n = 20), and 95% (n = 19) respectively. Separate Fisher's exact tests were performed for all comorbid Axis I diagnoses, with the exception of Specific Phobia, where a Chi-Square analysis was performed (see Table 3), indicating no significant differences between clusters for any comorbid diagnosis (ps ≥.38), with the exception of social phobia (p < .001). The non-assertive cluster had higher rates of social phobia than all other clusters (Fisher's exact test Intrusive p = .0006; Exploitable p = .002; Cold p = .001). Ninety percent of the non-assertive cluster met criteria for social phobia, whereas 45.2% of the cold cluster, 38.9% of the exploitable cluster and 28.6% of the intrusive cluster met criteria for this disorder.
Table 3. Study 2: Frequency of Axis I Comorbid Diagnoses in GAD group at Pre-Therapy (N = 83).
| Intrusive Cluster (N = 14) |
Exploitable Cluster (N = 18) |
Cold Cluster (N =31) |
Nonassertive Cluster (N =20) |
|||||
|---|---|---|---|---|---|---|---|---|
| Diagnosis | # who met criteria | % who met criteria | # who met criteria | % who met criteria | # who met criteria | % who met criteria | # who met criteria | % who met criteria |
| Substance abuse | 0 | 0 | 0 | 0 | 1 | 3.2 | 0 | 0 |
| Panic disorder | 3 | 21.4 | 4 | 22.2 | 5 | 16.1 | 1 | 5.0 |
| Agoraphobia | 3 | 21.4 | 1 | 5.6 | 3 | 9.7 | 4 | 20.0 |
| Social phobia | 4 | 28.6 | 7 | 38.9 | 14 | 45.2 | 18 | 90.0** |
| PTSD | 1 | 7.1 | 0 | 0 | 3 | 9.7 | 2 | 10.0 |
| OCD | 0 | 0 | 0 | 0 | 1 | 3.2 | 0 | 0 |
| Specific phobia | 7 | 50 | 9 | 50 | 9 | 29.0 | 7 | 35.0 |
| Major Depressive Dis. | 6 | 42.9 | 5 | 27.8 | 7 | 22.6 | 5 | 25.0 |
| Dysthymia | 1 | 7.1 | 2 | 11.1 | 3 | 9.7 | 4 | 20.0 |
| Hypochondriasis | 0 | 0 | 1 | 5.6 | 3 | 9.7 | 0 | 0 |
| Depressive disorder | 0 | 0 | 1 | 5.6 | 0 | 0 | 0 | 0 |
| Pain disorder | 0 | 0 | 1 | 5.6 | 3 | 9.7 | 0 | 0 |
| Bipolar I hypomanic | 1 | 7.1 | 0 | 0 | 0 | 0 | 0 | 0 |
Note:
p <.001 on a Fisher's exact test.
No participant met criteria for Alcohol Abuse, Alcohol Dependence, Substance Dependence, Acute Stress Disorder, Mania, Somatization Disorder, and Body Dysmorphic Disorder, therefore they were not included in this table.
Contrary to our prediction, there were no significant differences between clusters on the omnibus test of attachment subscales (F(24, 209) = 1.52, p = .06, η2p=.144), although there was a trend toward significance and a large effect size. However, there was a significant difference between clusters on percentage of individuals who met criteria for an Axis II disorder (Fisher's exact test p = .009). The nonassertive cluster had a higher rate of Axis II disorders than the cold (Fisher's exact test p = .02) or exploitable clusters (Fisher's exact test p = .002) and there was a trend toward significance when compared to the intrusive cluster (Fisher's exact test p = .06). Rates of Axis II within the intrusive, exploitable, cold and nonassertive clusters were 64.3% (n = 9), 47.1% (n = 8), 64.5% (n = 20), and 95% (n = 19), respectively.
Significant differences were found between the clusters on avoidant personality disorder (Fisher's exact test p = .00003), but no other differences across clusters in rates of specific personality disorders (Fisher's exact test ps ≥ .31)(see Table 4). The nonassertive cluster had higher rates of avoidant personality disorder than all other clusters (Fisher's exact test Intrusive p = .001; Exploitable p =.008; Cold p = .00004).
Table 4. Study 2: Frequency of Axis II Comorbid Diagnoses in GAD at Pre-Therapy (N = 82).
| Intrusive Cluster (N = 14) |
Exploitable Cluster (N = 17) |
Cold Cluster (N = 31) |
Nonassertive Cluster (N = 20) |
|||||
|---|---|---|---|---|---|---|---|---|
| Diagnosis | # who met criteria | % who met criteria | # who met criteria | % who met criteria | # who met criteria | % who met criteria | # who met criteria | % who met criteria |
| Any PD | 9 | 64.3 | 8 | 47.1 | 20 | 64.5 | 19 | 95 |
| Avoidant PD | 2 | 14.3 | 3 | 17.6 | 5 | 16.1 | 15 | 75.0*** |
| Dependent PD | 2 | 14.3 | 1 | 5.9 | 1 | 3.2 | 1 | 5.0 |
| Obsessive-Compulsive PD | 6 | 42.9 | 4 | 23.5 | 14 | 45.2 | 9 | 47.4 |
| Passive-Aggressive PD | 3 | 21.4 | 1 | 5.9 | 3 | 9.7 | 1 | 5.0 |
| Depressive PD | 6 | 42.9 | 5 | 29.4 | 9 | 29.0 | 6 | 30.0 |
| Paranoid PD | 2 | 14.3 | 0 | 0 | 3 | 10.0 | 2 | 10.0 |
| Schizotypal PD | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 5.0 |
| Schizoid PD | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 5.0 |
| Narcissistic PD | 0 | 0 | 0 | 0 | 3 | 9.7 | 0 | 0 |
| Borderline PD | 0 | 0 | 0 | 0 | 2 | 6.5 | 1 | 5 |
p = .00003 on a Fisher's exact test
Note: No participant met criteria for Histrionic Personality Disorder or Antisocial Personality Disorder, therefore, they were not included in this table.
Study 2 Discussion
Results of Study 2 generally replicated those of study 1 and the work of Salzer et al. (2008), supporting a pathoplastic relationship between interpersonal problems and GAD and providing strong evidence for interpersonal subtypes within GAD. Percentages of individuals falling in each cluster were fairly similar to that of study 1 and similarly clusters did not differ on severity of GAD, anxiety, or depression, attachment variables, or Axis I comorbidity (with the exception of social phobia). There was a significant difference between clusters on percentage of individuals meeting criteria for personality disorders with 95% of those in the nonassertive cluster meeting criteria for a personality disorder (versus 47.1% of those in the exploitable cluster, and 64% in the intrusive and cold clusters).
General Discussion
In this series of studies, the nature of interpersonal functioning in GAD was examined and an interpersonal pathoplasticity model was applied. The pathoplasticity model suggests that individuals' personalities and Axis I disorders are largely independent, but affect one another's manifestation, course, and treatment. The current study results support the application of this model to GAD.
Four homogenous interpersonal subtypes were reliably derived in independent samples of individuals with GAD. The subtypes identified were the intrusive, exploitable, cold, and nonassertive groups. As evidence of the strength of the subtypes, high levels of interpersonal prototypicality and profile differentiation were found within identified clusters, indicating that each cluster exhibits a consistent dysfunctional interpersonal theme. When the GAD group was examined as a whole, low prototypicality and profile differentiation were found, indicating no consistent interpersonal theme and an underlying complexity of the data. The strong emergence of four clusters suggests that GAD, although categorized as a single Axis I entity in DSM-IV, has a significant amount of reliable, within-group variation in interpersonal functioning. As such, assumptions about the interpersonal functioning of individuals with GAD as a single unit may be at the cost of truly understanding people with this diagnosis.
The identification of these subtypes is noteworthy for its replication of those identified by Salzer and colleagues (2008) in a German patient sample. However, as detailed earlier, the current study improves upon Salzer and colleagues (2008) in a number of ways. In addition to solidifying the presence of the four interpersonal subtypes of GAD, the current series of studies also extends previous research by examining associations between interpersonal subtypes of GAD, attachment, and comorbid Axis II disorders. Consistent with theories of pathoplasticity, the four interpersonal subtypes did not differ in GAD severity (as indicated by the CSR). Furthermore, they did not differ on the HRSD and HARS. This supports one aspect of the pathoplasticity theory—namely that differences in interpersonal functioning across individuals with GAD cannot be accounted for by differences in Axis I symptoms.
As also expected, rates of Axis I comorbidity across the two studies were largely consistent across GAD subtypes, providing further evidence for independence of Axis I diagnoses and interpersonal functioning. However, one exception to this was found; there were no differences in Axis I comorbidity in Study 1 (other than a trend toward significance for social phobia), whereas in Study 2 there was a significant difference in rates of social phobia across interpersonal subtypes. Ninety percent of the nonassertive cluster met criteria for Social Phobia (as compared with 45.2% of the cold cluster, 38.9% of the exploitable cluster, and 28.6% of the intrusive cluster). This is probably due to the combination of larger rates of social phobia in study 2 (51.8% vs. 38.3% in study 1) as well as a much larger sample in Study 2. The exclusion of participants with panic disorder and severe major depression from study 1 and not from study 2 may also have impacted these results.
One possible explanation for differences between interpersonal subtypes in rates of social phobia in study 2 (and the trend toward significance in study 1) is that social phobia is a disorder for which the central features are about a particular type of interpersonal dysfunction. Symptoms of social phobia center around fear and avoidance of interacting with or being the focus of attention of other people. Also, individuals with social phobia tend to be nonassertive (Alden & Phillips, 1990; Kashdan, McKnight, Richey, & Hofmann, 2009). Further, two studies examining interpersonal pathoplasticity in social phobia found friendly-submissive clusters (Cain, et al., 2010; Kachin, et al., 2001). In both samples, the largest percentage of individuals fell in the nonassertive and submissive quadrants of the circumplex. In fact, Cain and colleagues (2009) found that all socially phobic outpatients reported interpersonal problems with nonassertiveness and submission. Therefore, it is not surprising that most individuals with social phobia in the current sample fell in the nonassertive cluster. Further examination of the effects of comorbidity of GAD and social phobia on interpersonal functioning appears warranted.
In contrast to the stability of rates of Axis I disorders which are theorized to be largely independent of interpersonal functioning in a pathoplasticity model, other aspects of functioning, are expected to vary between interpersonal subtypes, especially measures that are interpersonal in nature. Axis II disorders and attachment variables are two such measures of interpersonal functioning. Study 2 indicated that GAD subtypes did, in fact, differ in rates of Axis II diagnoses. For example, ninety-five percent of those in the nonassertive cluster met criteria for a personality disorder, as compared with 64.5% of the cold cluster, 64.3% of the intrusive cluster, and 47.1% of the exploitable cluster, providing support for the pathoplasticity model in GAD. Whereas avoidant personality disorder (AvPD) was the predominant personality disorder (75%), only 17.6% of the exploitable cluster, 16.1% of the cold cluster, and 14.3% of the intrusive cluster met criteria for AvPD. This suggests that the nonassertive cluster captured a selection of individuals with a tendency toward an Axis II diagnosis of AvPD, indicating again, that pathology in GAD varies by subtype. This is also consistent with Alden and Capreol's (1993) finding that participants with AvPD scored very highly in non-assertive problems on the IIP-C.
Contrary to our hypotheses, there were no significant differences in attachment variables across interpersonal subtypes in either study, although there was a trend toward significance in study 2 with large effect sizes in both studies. It is possible that we did not have sufficient power for this difference to achieve significance. Previous research has demonstrated an association between attachment styles and specific IIP octants (Chen & Mallinckrodt, 2002; Horowitz, et al., 1993); however, no prior study had examined whether there were differences in attachment across IIP clusters. Instead, extant studies have examined correlations between scores on measures of attachment styles and various IIP octant scores. This method of scoring the IIP may not accurately represent samples in which there are subgroups of interpersonal clusters, such as those with GAD. Further, the attachment variables examined in the current study have not been examined in association with interpersonal problems and it is possible that these attachment variables may be associated with multiple interpersonal problems.
The current series of studies contribute to our understanding of the interplay between interpersonal behaviors and GAD and provide support for the application of the interpersonal pathoplasticity model to individuals with this diagnosis. We also extended existing research on GAD and interpersonal functioning; however, the results are subject to a number of limitations. One such limitation is the exclusion of individuals with substance use disorders. Although the pathoplasticity model would suggest that such comorbidity would not impact interpersonal subtypes, the exclusion of these individuals limits the generalizability of our findings. In addition, in order to examine whether our results would be consistent with a pathoplasticity model some of our predictions were in the direction of suggesting support for the null hypothesis. However, failing to reject the null hypothesis does not prove that the null hypothesis is true and therefore, findings supporting these predictions should be interpreted with caution. Another limitation of the current series of studies is the lack of ethnic and racial diversity in the samples. Given the association between culture and interpersonal dynamics, it is possible that different results would be identified in a more diverse sample. Further, because perceived racial stress, which is interpersonal in nature, is associated with worry (Rucker, West, & Roemer, 2010) and individuals from diverse backgrounds worry about different topics than Caucasians (Scott, Eng, & Heimberg, 2002), GAD symptoms and associated interpersonal styles may manifest differently in a more diverse sample. This study was also limited by the small number of individuals who met criteria for some comorbid Axis I and II disorders. Future research should examine larger samples with a greater number of individuals with various types of comorbid disorders, particularly Axis II.
An additional area for future exploration is related to treatment. Changes in some interpersonal problems have been associated with GAD symptom reduction in response to treatment (Borkovec, et al., 2002; Crits-Christoph, Gibbons, Narducci, Schamberger, & Gallop, 2005; Salzer, Pincus, Winkelbach, Leichsenring, & Leibing, in press), and interpersonal problems change as a result of treatment for GAD (Borkovec, et al., 2002; Crits-Christoph, Connolly, Azarian, Crits-Christoph, & Shappell, 1996; Newman, et al., 2008). However, the pathoplasticity model would predict that those with differing interpersonal styles would also have differential treatment outcome, because interpersonal problems and Axis I disorders affect one another's manifestation and course. Therefore, it may be that interpersonal problems change differentially as a result of various forms of therapy for GAD, such as cognitive-behavioral, interpersonal, and emotion-based approaches. If that is the case, then the assessment of interpersonal problems prior to the start of therapy may assist therapists in choosing the most appropriate therapeutic techniques to use. For example, in the case of clients with GAD who fall into the intrusive cluster, therapists may choose to discuss ways in which clients' worries may be related to their feelings of being responsible for solving others' problems. Cognitive-restructuring may be important to examine and alter schemata related to excessive responsibility for others. Therapists may also discuss the impact of clients' intrusive worrying and problem solving on others as this may affect clients' relationships. Further, therapists may encourage clients to learn appropriate coping skills to manage worries and regulate emotions independently, rather than divulging worries and other feelings to others. However, clients with GAD who fall into the nonassertive cluster may benefit more if therapists address worries about what may happen in their relationships if they are assertive or express their needs. Further, therapists may consider the importance of having clients set the agenda for therapy sessions, create homework assignments, or identify therapeutic goals to encourage them to be more assertive about their desires and to take a more dominant role in relationships. Such integrative therapy, combining CBT and interpersonal conceptualization and techniques, may provide a means of treating clients as a whole, rather than focusing primarily on symptoms or relationships (e.g., Newman, et al., in press; Newman, et al., 2008). Thus, the application of the pathoplasticity model to GAD may have large implications for improving therapy for the disorder by providing important information for treatment planning beyond DSM diagnosis.
Acknowledgments
The authors would like to thank Nicole Cain and Aidan Wright for their help in the preparation of this manuscript. This research was supported in part by National Institute of Mental Health Research Grants R01 MH039172-01, 2RO1MH39172-12, and R01 MH058593-02.
Footnotes
It may appear somewhat confusing that Salzer and colleagues (2008) refer to their study as a replication of conference papers by Pincus et al., (2005) and Kasoff and Pincus, (2002). The current series of studies incorporate the data from the two conference presentations that Salzer and colleagues (2008) reference. However, this is the first time this data has been submitted for publication. Given that Salzer and colleagues (2008) study was published first, we refer to our study as a replication and extension of their study.
There is an empirical justification to cluster analysis with a smaller sample study. Clatworthy, Hankins, Buick, Weinman, & Horne (2007) found that identifying cluster centroids and the number of clusters using Ward's method of cluster analysis followed by K-Means cluster analysis to refine the results correctly identified 80% of cases into clusters in a sample size as small as 42. This is also the procedure recommended for cluster analyses by Milligan (1980) and the method that was employed in the current study. Clatworthy and colleagues concluded “This indicates that K-means is an acceptable method for use in samples as small as 42 cases. This is of particular importance because multivariate inferential statistics would often not have sufficient power in such small sample sizes. (Clatworthy et al., 2007, p 138). The replication of the clusters in two separate samples with different inclusion/exclusion criteria further supports the interpersonal subtypes derived in our studies.
Although mixture modeling is generally the most appropriate analytic strategy for determining whether unobserved subtypes exist within a heterogeneous sample; Monte Carlo analyses indicated that the sample size in the current series of studies does not permit the use of such analyses. Cluster analysis, specifically Ward's method to identify the number of clusters and cluster centroids, has been demonstrated to accurately identify subtypes in samples of data as small as 42 (Clatworthy et al, 2007) therefore, this analysis was used in the current series of studies.
Effect sizes are reported in addition to the statistical test results to provide evidence (independent of sample size) for whether an effect is non-trivial or not (see Zumbo & Hubley, 1998 for a discussion of power and effect size). A small effect size is considered to be .010 to .058, a medium effect, .059 to .137, and large effect = > .137 (Kirk, 1996). Kirk's criteria are for omega-sq.; however, these criteria may be appropriately applied to interpreting partial eta-squared which is a similar measure of strength of association.
The use of Finn's r was necessary due to the fact that we recruited only individuals with severity ratings of 4 or higher for GAD (necessary for diagnosis) leading to a restricted range in severity for this disorder only.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/abn
Contributor Information
Amy Przeworski, Case Western Reserve University.
Michelle G. Newman, The Pennsylvania State University
Aaron L. Pincus, The Pennsylvania State University
Michele B. Kasoff, The Pennsylvania State University
Alissa S. Yamasaki, The Pennsylvania State University
Louis G. Castonguay, The Pennsylvania State University
Kristoffer S. Berlin, Ohio University
References
- Alden LE, Capreol MJ. Avoidant personality disorder: Interpersonal problems as predictors of treatment response. Behavior Therapy. 1993;24:357–376. doi: 10.1016/S0005-7894(05)80211-4. [DOI] [Google Scholar]
- Alden LE, Phillips N. An interpersonal analysis of social anxiety and depression. Cognitive Therapy and Research. 1990;14(5):499–512. doi: 10.1007/bf01172970. [DOI] [Google Scholar]
- Alden LE, Wiggins JS, Pincus AL. Construction of circumplex scales for the Inventory of Interpersonal Problems. Journal of Personality Assessment. 1990;55:521–536. doi: 10.1207/s15327752jpa5503&4_10. [DOI] [PubMed] [Google Scholar]
- Beck JG, Stanley MA, Zebb BJ. Characteristics of generalized anxiety disorder in older adults: a descriptive study. Behaviour Research and Therapy. 1996;34(3):225–234. doi: 10.1016/0005-7967(95)00064-X. [DOI] [PubMed] [Google Scholar]
- Biederman J, Rosenbaum JF, Chaloff J, Kagan J. Behavioral inhibition as a risk factor for anxiety disorders. In: March JS, editor. Anxiety disorders in children and adolescents. New York: Guilford; 1995. pp. 61–81. [Google Scholar]
- Borkovec TD, Newman MG, Pincus AL, Lytle R. A component analysis of cognitive-behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. Journal of Consulting and Clinical Psychology. 2002;70(2):288–298. doi: 10.1037/0022-006X.70.2.288. [DOI] [PubMed] [Google Scholar]
- Breitholtz E, Johansson B, Ost LG. Cognitions in generalized anxiety disorder and panic disorder patients. A prospective approach. Behaviour Research and Therapy. 1999;37(6):533–544. doi: 10.1016/S0005-7967(98)00147-8. [DOI] [PubMed] [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB. Current and Lifetime Comorbidity of the DSM-IVAnxiety and Mood Disorders in a Large Clinical Sample. Journal of Abnormal Psychology. 2001;110(4):585–599. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- Brown TA, Di Nardo PA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV. Albany, New York: Graywind Publications; 1994. [Google Scholar]
- Bruss GS, Gruenberg AM, Goldstein RD, Barber JP. Hamilton anxiety rating scale interview guide: Joint interview and test-retest methods for interrater reliability. Psychiatry Research. 1994;53(2):191–202. doi: 10.1016/0165-1781(94)90110-4. [DOI] [PubMed] [Google Scholar]
- Buss AH, Plomin R. A temperament theory of personality development. New York: Wiley; 1975. [Google Scholar]
- Cain NM, Pincus AL, Grosse Holtforth M. Interpersonal subtypes in social phobia: Diagnostic and treatment implications. Journal of Personality Assessment. 2010;92:514–527. doi: 10.1080/00223891.2010.513704. [DOI] [PubMed] [Google Scholar]
- Cassidy J, Lichtenstein-Phelps J, Sibrava NJ, Thomas CL, Borkovec TD. Generalized Anxiety Disorder: Connections With Self-Reported Attachment. Behavior Therapy. 2009;40(1):23–38. doi: 10.1016/j.beth.2007.12.004. [DOI] [PubMed] [Google Scholar]
- Cassidy J, Shaver PR. Handbook of attachment: Theory, research, and clinical applications. 1st ed. New York: Guilford; 1999. [Google Scholar]
- Chen EC, Mallinckrodt B. Attachment, Group Attraction, and Self-Other Agreement in Interpersonal Circumplex Problems and Perceptions of Group Members. Group Dynamics. 2002;6(4):311–324. doi: 10.1037/1089-2699.6.4.311. [DOI] [Google Scholar]
- Clatworthy J, Hankins M, Buick D, Weinman J, Horne R. Cluster analysis in illness perception research: A Monte Carlo study to identify the most appropriate method. Psychology & Health. 2007;22(2):123–142. doi: 10.1080/14768320600774496. [DOI] [Google Scholar]
- Crits-Christoph P, Connolly MB, Azarian K, Crits-Christoph K, Shappell S. An open trial of brief supportive-expressive psychotherapy in the treatment of generalized anxiety disorder. Psychotherapy: Theory, Research, Practice & Training. 1996;33(3):418–430. doi: 10.1037/0033-3204.33.3.418. [DOI] [Google Scholar]
- Crits-Christoph P, Gibbons MBC, Narducci J, Schamberger M, Gallop R. Interpersonal problems and the outcome of interpersonally oriented psychodynamic treatment of GAD. Psychotherapy: Theory, Research, Practice, & Training. 2005;42(2):211–224. doi: 10.1037/0033-3204.42.2.211. [DOI] [Google Scholar]
- Di Nardo PA, Barlow DH. Anxiety Disorders Interview Schedule-Revised (ADIS-R) Albany: Center for Stress and Anxiety Disorders; 1988. [DOI] [PubMed] [Google Scholar]
- Eng W, Heimberg RG. Interpersonal correlates of generalized anxiety disorder: Self versus other perception. Journal of Anxiety Disorders. 2006;20(3):380–387. doi: 10.1016/j.janxdis.2005.02.005. [DOI] [PubMed] [Google Scholar]
- Erickson TM, Newman MG. Interpersonal and Emotional Processes in Generalized Anxiety Disorder Analogues During Social Interaction Tasks. Behavior Therapy. 2007;38(4):364–377. doi: 10.1016/j.beth.2006.10.005. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Guide for the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- Gurtman MB. The circumplex as a tool for studying normal and abnormal personality: A methodological primer. In: Strack S, Lorr M, editors. Differentiating normal and abnormal personality. New York: Springer; 1994. pp. 243–263. [Google Scholar]
- Gurtman MB, Balakrishnan JD. Circular Measurement Redux: The Analysis and Interpretation of Interpersonal Circle Profiles. Clinical Psychology: Science and Practice. 1998;5(3):344–360. doi: 10.1111/j.1468-2850.1998.tb00154.x. [DOI] [Google Scholar]
- Gurtman MB, Pincus AL. The Circumplex Model: Methods and Research Applications. John Wiley & Sons, Inc.; 2003. [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry. 1960;23:56–61. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoehn-Saric R, Hazlett RL, McLeod DR. Generalized anxiety disorder with early and late onset of anxiety symptoms. Comprehensive Psychiatry. 1993;34(5):291–298. doi: 10.1016/0010-440x(93)90013-t. [DOI] [PubMed] [Google Scholar]
- Horowitz LM. Interpersonal foundations of psychopathology. Washington DC: American Psychological Association; 2004. [Google Scholar]
- Horowitz LM, Rosenberg SE, Baer BA, Ureño G, Villaseñor VS. Inventory of Interpersonal Problems: Psychometric Properties and Clinical Applications. Journal of Consulting and Clinical Psychology. 1988;56(6):885–892. doi: 10.1037//0022-006X.56.6.885. [DOI] [PubMed] [Google Scholar]
- Horowitz LM, Rosenberg SM, Bartholomew K. Interpersonal problems, attachment styles, and outcome in brief dynamic psychotherapy. Journal of Consulting and Clinical Psychology. 1993;61(4):549–560. doi: 10.1037/0022-006X.61.4.549. [DOI] [PubMed] [Google Scholar]
- Horowitz LM, Wilson KR, Turan B, Zolotsev P, Constantino MJ, Henderson L. How interpersonal motives clarify the meaning of interpersonal behavior: A revised circumplex model. Personality and Social Psychology Review. 2006;10(1):67–86. doi: 10.1207/s15327957pspr1001_4. [DOI] [PubMed] [Google Scholar]
- Kachin KE, Newman MG, Pincus AL. An interpersonal problem approach to the division of social phobia subtypes. Behavior Therapy. 2001;32(3):479–501. doi: 10.1016/s0005-7894(01)80032-0. [DOI] [Google Scholar]
- Kashdan TB, McKnight PE, Richey JA, Hofmann SG. When social anxiety disorder co-exists with risk-prone, approach behavior: Investigating a neglected, meaningful subset of people in the National Comorbidity Survey-Replication. Behaviour Research and Therapy. 2009;47(7):559–568. doi: 10.1016/j.brat.2009.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasoff MB, Pincus AL. Interpersonal pathoplasticity in generalized anxiety disorder. Paper presented at the American Psychological Association; Chicago, IL. 2002. [Google Scholar]
- Kirk RE. Practical Significance: A Concept Whose Time Has Come. Educational and Psychological Measurement. 1996;56(5):746–759. doi: 10.1177/0013164496056005002. [DOI] [Google Scholar]
- Klein MH, Wonderlich S, Shea MT. Models of relationships between personality and depression: Toward a framework for theory and research. In: Klein M, Kupfer D, Tracie M, editors. Personality and depression: A current view. New York: Guilford Press; 1993. pp. 1–54. [Google Scholar]
- Kobak KA, Reynolds WM, Greist JH. Development and Validation of a Computer-Administered Version of the Hamilton Anxiety Scale. Psychological Assessment. 1993;5(4):487–492. doi: 10.1037/1040-3590.5.4.487. [DOI] [Google Scholar]
- Leary T. Interpersonal diagnosis of personality. New York: Ronald Press; 1957. [Google Scholar]
- Lichtenstein J, Cassidy J. The Inventory of Adult Attachment: Validation of a new measure. Paper presented at the Biennial Meeting of the Society for Research in Child Development; Seattle. 1991. [Google Scholar]
- Maffei C, Fossati A, Agostoni I, Barraco A, Bagnato M, Deborah D, et al. Interrater reliability and internal consistency of the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II), version 2.0. Journal of Personality Disorders. 1997;11(3):279–284. doi: 10.1521/pedi.1997.11.3.279. [DOI] [PubMed] [Google Scholar]
- McLeod JD. Anxiety Disorders and Marital Quality. Journal of Abnormal Psychology. 1994;103(4):767–776. doi: 10.1037/0021-843X.103.4.767. [DOI] [PubMed] [Google Scholar]
- Mikulincer M, Shaver PR. Attachment patterns in adulthood: Stucture, dynamic, and change. New York: Guilford Press; 2007. [Google Scholar]
- Milligan G. An examination of the effect of six types of error perturbation on fifteen clustering algorithms. Psychometrika. 1980;45(3):325–342. doi: 10.1007/bf02293907. [DOI] [Google Scholar]
- Millon T. Reflections on the future of personology and psychopathology. In: Strack S, editor. Handbook of personology and psychopathology. Hoboken: John Wiley and Sons, Inc.; 2005. pp. 527–546. [Google Scholar]
- Moras K, Di Nardo PA, Barlow DH. Distinguishing anxiety and depression: reexamination of the reconstructed Hamilton Scales. Psychological Assessment. 1992;4(2):224–227. doi: 10.1037/1040-3590.4.2.224. [DOI] [Google Scholar]
- Newman MG, Castonguay LG, Borkovec TD, Fisher AJ, Boswell J, Szkodny L, et al. A randomized controlled trial of cognitive-behavioral therapy with integrated techniques from emotion-focused and interpersonal therapies. Journal of Consulting and Clinical Psychology. doi: 10.1037/a0022489. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Castonguay LG, Borkovec TD, Fisher AJ, Nordberg SS. An open trial of integrative therapy for generalized anxiety disorder. Psychotherapy Theory, Research, Practice, & Training. 2008;45:135–147. doi: 10.1037/0033-3204.45.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Erickson TM. Generalized anxiety disorder. In: Beck JG, editor. Interpersonal processes in the anxiety disorders: Implications for understanding psychopathology and treatment. Washington, DC: American Psychological Association; 2010. [Google Scholar]
- Newman MG, Przeworski A, Fisher AJ, Borkovec TD. Diagnostic comorbidity in adults with generalized anxiety disorder: impact of comorbidity on psychotherapy outcome and impact of psychotherapy on comorbid diagnoses. Behavior Therapy. 2010;41(1):59–72. doi: 10.1016/j.beth.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilkonis PA. Identification of risk factors in borderline personality disorder: The example of interpersonal functioning. Paper presented at the New Directions in Borderline Personality II Conference; Minneapolis, MN. 2002. [Google Scholar]
- Pincus AL. A contemporary intergrative interpersonal theory of personality disorders. In: Lenzenweger ML, Clarkin JF, editors. Major theories of personality disorder. New York: Guilford Press; 2005. pp. 282–331. [Google Scholar]
- Pincus AL, Przeworski A, Yamasaki A, Kasoff MB, Newman MG, Castonguay LG, et al. Interpersonal pathoplasticity in generalized anxiety disorder: A cluster analytic replication. Paper presented at the Society for Interpersonal Theory and Research; Montreal, Quebec, Canada. 2005. [Google Scholar]
- Rapee RM. Distinctions Between Panic Disorder and Generalised Anxiety Disorder: Clinical Presentation. Australian and New Zealand Journal of Psychiatry. 1985;19(3):227–232. doi: 10.3109/00048678509158827. [DOI] [PubMed] [Google Scholar]
- Roemer L, Molina S, Borkovec TD. An investigation of worry content among generally anxious individuals. Journal of Nervous and Mental Disease. 1997;185(5):314–319. doi: 10.1097/00005053-199705000-00005. [DOI] [PubMed] [Google Scholar]
- Rothbart MK. Temperament and development. In: Kohnstamm GA, Bates JE, Rothbart MK, editors. Temperament in childhood. Chichester, England: Wiley; 1989. pp. 187–247. [Google Scholar]
- Rucker LS, West LM, Roemer L. Relationships Among Perceived Racial Stress, Intolerance of Uncertainty, and Worry in a Black Sample. Behavior Therapy. 2010;41(2):245–253. doi: 10.1016/j.beth.2009.04.001. [DOI] [PubMed] [Google Scholar]
- Salzer S, Pincus AL, Hoyer J, Kreische R, Leichsenring F, Leibing E. Interpersonal subtypes within generalized anxiety disorder. Journal of Personality Assessment. 2008;90(3):292–299. doi: 10.1080/00223890701885076. [DOI] [PubMed] [Google Scholar]
- Salzer S, Pincus AL, Winkelbach C, Leichsenring F, Leibing E. Interpersonal subtypes and change of interpersonal problems in the treatment of patients with generalized anxiety disorder: a pilot study. Psychotherapy: Theory, Research, Practice & Training. doi: 10.1037/a0022013. in press. [DOI] [PubMed] [Google Scholar]
- Sanderson WC, Wetzler S, Beck AT, Betz F. Prevalence of personality disorders among patients with anxiety disorders. Psychiatric Research. 1994;51(2):167–174. doi: 10.1016/0165-1781(94)90036-1. [DOI] [PubMed] [Google Scholar]
- Scott EL, Eng W, Heimberg RG. Ethnic differences in worry in a nonclinical population. Depression and Anxiety. 2002;15(2):79–82. doi: 10.1002/da.10027. [DOI] [PubMed] [Google Scholar]
- Steer RA, McElroy MG, Beck AT. Correlates of self-reported and clinically assessed depression in outpatient alcoholics. Journal of Clinical Psychology. 1983;39(1):144–149. doi: 10.1002/1097-4679(198301)39:1<144::aid-jclp2270390128>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Sullivan HS. Conceptions of modern psychiatry. New York: Norton; 1953. [Google Scholar]
- Tracey TJ, Rounds J, Gurtman MB. Examination of the general factor with the interpersonal circumplex structure: application of the Inventory of Interpersonal Problems. Multivariate Behavioral Research. 1996;31:441–466. doi: 10.1207/s15327906mbr3104_3. [DOI] [PubMed] [Google Scholar]
- Triandis HC. Culture and social behavior. New York: McGraw-Hill; 1994. [Google Scholar]
- Triandis HC, Tanaka Y, Shanmugam A. Interpersonal attitudes among American, Indian, and Japanese students. International Journal of Psychology. 1966;1(3):177–206. doi: 10.1080/00207596608247155. [DOI] [Google Scholar]
- Whisman MA, Sheldon CT, Goering P. Psychiatric disorders and dissatisfaction with social relationships: Does type of relationship matter? Journal of Abnormal Psychology. 2000;109(4):803–808. doi: 10.1037/0021-843X.109.4.803. [DOI] [PubMed] [Google Scholar]
- Whitehurst GJ. Interrater agreement for journal manuscript reviews. American Psychologist. 1984;39:22–28. doi: 10.1037/0003-066X.39.1.22. [DOI] [Google Scholar]
- Widiger TA, Smith GT. Personality and psychopathology. In: John OP, Robins RW, Pervin LA, editors. Handbook of personality psychology: Theory and research. 3rd. New York: Guilford Press; 2008. pp. 743–769. [Google Scholar]
- Wiggins JS. Agency and communion as conceptual coordinates for the understanding and measurement of interpersonal behavior. In: Cicchetti D, Grove WM, editors. Thinking clearly about psychology: Essays in honor of Paul E Meehl, Vol 2: Personality and psychopathology. Minneapolis: University of Minnesota Press; 1991. pp. 89–113. [Google Scholar]
- Wiggins JS. An informal history of the interpersonal circumplex tradition. Journal of Personality Assessment. 1996;66:217–233. doi: 10.1207/s15327752jpa6602_2. [DOI] [PubMed] [Google Scholar]
- Wiggins JS. Paradigms of personality assessment. New York: Guilford; 2003. [DOI] [PubMed] [Google Scholar]
- Wittchen HU, Hoyer J. Generalized anxiety disorder: Nature and course. Journal of Clinical Psychiatry. 2001;62(Suppl 11):15–19. [PubMed] [Google Scholar]
- Wright AGC, Pincus AL, Conroy DE, Hilsenroth MJ. Integrating methods to optimize circumplex description and comparison of groups. Journal of Personality Assessment. 2009;91:311–322. doi: 10.1080/00223890902935696. [DOI] [PubMed] [Google Scholar]
- Zumbo BD, Hubley AM. A note on misconceptions concerning prospective and retrospective power. Journal of the Royal Statistical Society, Series D: The Statistician. 1998;47:385–388. doi: 10.1111/1467-9884.00139. [DOI] [Google Scholar]