Abstract
Background
Information is sparse regarding the association between international travel and hospitalization with non-typhoidal Salmonella bacteremia. The aim of this study was to determine the proportion, risk factors and outcomes of travel-related non-typhoidal Salmonella bacteremia.
Methods
We conducted a 10-year population-based cohort study of all patients hospitalized with non-typhoidal Salmonella bacteremia in three Danish counties (population 1.6 million). We used denominator data on Danish travellers to assess the risk per 100,000 travellers according to age and travel destination. We used patients contemporaneously diagnosed with travel-related Salmonella gastroenteritis as reference patients to estimate the relative risk of presenting with travel-related bacteremia as compared with gastroenteritis. To evaluate clinical outcomes, we compared patients with travel-related bacteremia and patients with domestically acquired bacteremia in terms of length of hospital stay, number of extraintestinal focal infections and mortality after 30 and 90 days.
Results
We identified 311 patients hospitalized with non-typhoidal Salmonella bacteremia of whom 76 (24.4%) had a history of international travel. The risk of travel-related bacteremia per traveller was highest in the age groups 15-24 years (0.8/100,000 travellers) and 65 years and above (1.2/100,000 travellers). The sex- and age-adjusted relative risk of presenting with bacteremia was associated with travel to Sub-Saharan Africa (odds ratio 18.4; 95% confidence interval [6.9-49.5]), the Middle East (10.6; [2.1-53.2]) and South East Asia (4.0; [2.2-7.5]). We found high-risk countries in the same three regions when estimating the risk per traveller according to travel destination. Patients hospitalized with travel-related bacteremia had better clinical outcomes than patients with domestically acquired bacteremia, they had a shorter length of hospital stay (8 vs. 11 days), less extraintestinal focal infections (5 vs. 31 patients) and a lower risk of death within both 30 days (relative risk 0.2; [0.1-0.7]) and 90 days (0.3; [0.1-0.7]). A healthy traveller effect was a plausible explanation for the observed differences in outcomes.
Conclusions
International travel is a notable risk factor for being hospitalized with non-typhoidal Salmonella bacteremia and the risk differs between age groups and travel destinations. Healthy travellers hospitalized with bacteremia are less likely to have poor outcomes than patients with domestically acquired bacteremia.
Background
International travel has increased manifold during the last decades as a consequence of increasing prosperity and reduced costs. Overseas destinations have become popular holiday resorts for Europeans, e.g., Thailand was visited by 758,000 Scandinavians in 2007 [1]. As a consequence there is increasing attention to the exposure to parasitic and viral infections including malaria, hepatitis, dengue fever, and HIV-infection [2-5]. Among travel-related bacterial infections, typhoid and paratyphoid fevers have been addressed in a number of studies [6-8]. Less information is available concerning invasive infections with non-typhoidal Salmonella enterica serovars (henceforth Salmonella) although they are common causes of gastrointestinal infections in travellers. In a recent Swedish study the highest risk of gastrointestinal salmonellosis was associated with travelling to East Africa and the Indian subcontinent [9]. In a Danish cohort study from the 1980's, 18% of Salmonella bacteremias were associated with travel [10].
European studies on travel-related risk of Salmonella bacteremia are few and either clinic-based [11,12] or confined to a particular serovar or travel destination [13]. Therefore, the proportion of patients hospitalized with travel-related bacteremia remains uncertain and knowledge of potential risk factors and outcomes are lacking. Such data would be of value for providers of guidance to travellers and for clinical decision making. The objective of this study was to determine the proportion of hospitalized patients with non-typhoidal Salmonella bacteremia related to international travel, to assess whether the risk of bacteremia was associated with the travel destination, age or sex, and to evaluate the clinical outcome.
Methods
Study population
We conducted a population-based cohort study in the three Danish counties of North Jutland, Aarhus and Funen from January 1999 through December 2008 (average population 1.6 million, i.e. approximately one third of the Danish population). The demographic composition was representative for all of Denmark.
The National Health Service provides tax-supported health care free of charge to all Danish residents, provided by general practitioners and public hospitals. People with Danish citizenship or permanent residency in Denmark are uniquely identifiable by a 10-digit civil registration number, which is recorded at all contacts with the health service allowing accurate linkage between health registries.
Data Sources
Local microbiological databases
In each county a single diagnostic laboratory processed all bacteriological samples submitted by general practitioners and hospitals. Information on blood isolates of Salmonella serovars were retrieved from the electronic laboratory information systems in each laboratory.
The National Registry of Enteric Pathogens (REP)
Diagnostic laboratories mandatorily report Salmonella infections to the national reference center at Statens Serum Institut (SSI) and this information is recorded in the REP. If a Salmonella serovar is isolated more than once from the same person within six months, only the first positive sample is registered in the REP. Sample type (feces, blood or another usually sterile site) is not available for all isolates. For the years 2004-2008 the database holds information on international travel provided by the local laboratory on a voluntarily basis. In 2008 full travel information in REP was obtained by telephone interviews [14]. The travel information collected by telephone interviews and notified voluntarily has been found comparable with regard to the distribution of travel destinations. We identified patients with Salmonella infection who were residents in any of the three counties in the REP.
Hospital charts
For patients hospitalized with non-typhoidal Salmonella bacteremia, we extracted the following information: travel history, comorbidity, any extraintestinal site of infection, dates of admission and discharge, length of stay and time of death. Comorbidity was classified according to the Charlson comorbidity index and three levels of comorbidity were defined: low (0), corresponding to patients with no recorded underlying diseases; medium (1-2) and high (≥3) [15].
Demographic data
Number of citizens in the three counties according to age groups were available from Statistics Denmark and used as denominators to calculate incidence rates [16].
Data on international travel
Statistics Denmark obtains information on international travel from a random sample of approximately 500 Danish citizens contacted by telephone each month. Information in the database includes age groups, travel destinations, month of travel, type of travel (business or pleasure), and length of travel. We restricted our analyses to pleasure travellers as business travellers may have a different travel form and risk profile. To account for a large number of short trips to neighboring countries, we included only travellers staying abroad for at least three nights. We used the information in the database to estimate travel patterns in the study population. Estimated numbers by age group and country of travel were used as denominators to calculate the risk of bacteremia per 100,000 travellers.
Laboratory procedures
Blood culture systems and nominal volumes of blood per culture differed between regions (North Jutland County: BacT/Alert (bioMérieux, Marcy I'Etoile, France) with a blood volume of 3 × 10 mL; Aarhus County: BacT/Alert (bioMérieux, Marcy I'Etoile, France); 2 × 20 mL; Funen County: ESP (Trek Diagnostic Systems, Cleveland, Ohio, USA) until 2001, and BACTEC (Becton Dickinson, Franklin Lakes, NJ, USA) thereafter; 2 × 20 mL).
In North Jutland County fecal cultures were performed by the regional diagnostic laboratory throughout the study period [17]. In the counties of Aarhus and Funen the regional laboratories carried out the cultures from 2004 and 2006, respectively. Prior to that, fecal cultures were performed by SSI, Copenhagen.
All Salmonella isolates obtained locally were referred to the national reference laboratory at SSI for serotyping according to the Kauffman-White scheme [18].
Definitions
We defined travel-related Salmonella bacteremia (henceforth TRB) on the basis of information in the hospital chart regarding foreign travel prior to admission and lack of any indication of domestic exposure. The remaining bacteremias were defined as domestically acquired (henceforth DAB). If a patient had visited more than one destination, we defined the main travel destination as the country where the patient had had an episode of diarrhea. If this information was missing, the last visited country was defined as the travel destination.
A patient with Salmonella gastroenteritis was defined as a patient recorded with non-typhoidal Salmonella in the REP and no blood culture isolate recorded in the local microbiological database.
Data analysis
Clinical data retrieved from patient charts were tabulated in a spreadsheet. Relative prevalence proportions (RPP) with corresponding 95% confidence intervals were calculated to estimate differences in age, sex and comorbidity among patients with TRB compared to DAB. Risk estimates per 100,000 travellers were calculated according to travel destination and age groups (children 0-14, young adults 15-24, adults 25-44, middle-aged 45-64, and elderly ≥65 years).
In the subset of patients diagnosed in 2004-2008, we estimated the risk of TRB compared to travel-related gastroenteritis by calculation of odds ratios (ORs) with 95% confidence intervals (CI). Risk associated with travel region was estimated by logistic regression and age group (<65, ≥65 years) and gender were included as potential confounders.
STATA version 9.2 (College Station, Texas) was used for the statistical analyses.
Ethics
The study was approved by The Danish National Board of Health and the Danish Data Protection Agency (Record no. 2008-54-0474).
Results
Demographic, clinical and bacteriological characteristics
During the 10-year study period a total of 350 patients were hospitalized and diagnosed with Salmonella bacteremia. The following cases were excluded: Salmonella Typhi (15), Salmonella Paratyphi (14) and non-residents (10), leaving 311 patients with non-typhoidal Salmonella bacteremia.
We identified 76 (24.4%) patients hospitalized with TRB. Most (68/76, 89%) were admitted to hospital within two weeks after returning to Denmark; patients admitted later (8/76, 11%) had had diarrhea during travel and fever after the return. Four of these patients had been treated with antibiotics by their general practitioner before hospital admission.
Table 1 presents key characteristics for patients with TRB and DAB. In the group of patients with TRB there was a majority of males and patients with TRB were younger than patients with DAB (RPP for males in TRB compared to DAB was 1.3; 95% CI[1.0-1.6]; RPP for age <65 years was 1.6; [1.4-1.9]). Seventy one percent of patients with TRB had no comorbidities according to the Charlson index compared with 29% of patients with DAB (RPP 2.4; [1.9-3.1]).
Table 1.
Characteristics of patients with travel-related (TRB) and domestically acquired (DAB) bacteremia
| Characteristics | TRB (n = 76) | DAB (n = 235) | ||
|---|---|---|---|---|
| Age | ||||
| Median (years, range) | 36 | (0-79) | 64 | (0-96) |
| <65 years (numbers, percent) | 64 | (84.2) | 123 | (52.3) |
| ≥65 years | 12 | (15.8) | 112 | (47.7) |
| Sex | ||||
| Males | 49 | (64.5) | 118 | (50.2) |
| Admitted to an infectious diseases unita | 29/64 | (45.3) | 8/163 | (4.9) |
| Comorbidity indexb | ||||
| 0 | 54 | (71.1) | 69 | (29.4) |
| 1-2 | 11 | (14.5) | 91 | (38.7) |
| ≥3 | 11 | (14.5) | 75 | (31.9) |
| Individuals with malignancy | ||||
| Hematological malignanciesc | 3 | (3.9) | 23 | (9.8) |
| Other malignancies | 6 | (7.9) | 36 | (15.3) |
| Other comorbidities | ||||
| Dialysisd | 0 | (0.0) | 3 | (1.3) |
| Organ transplantation | 0 | (0.0) | 2 | (0.9) |
| Alcoholisme | 3 | (3.9) | 21 | (8.9) |
| Previous gastric surgeryf | 3 | (3.9) | 5 | (2.1) |
| Drug therapy | ||||
| Chemotherapy & immunomodulatory agents | 5 | (6.6) | 33 | (14.0) |
| Corticosteroid therapy | 2 | (2.6) | 30 | (12.8) |
| PPI & H2-antagonist | 7 | (9.2) | 66 | (28.1) |
| Antacids | 0 | (0.0) | 8 | (3.4) |
| Length of hospital stay (median, IQR) | 8 days | (5-11) | 11 days | (6-17) |
| An extraintestinal site of infection | 5 | (6.6) | 31 | (13.2) |
| Mortality by age group | ||||
| <65 years | ||||
| 30-day | 3 | (4.7) | 11 | (8.9) |
| 90-day | 4 | (6.3) | 12 | (9.8) |
| ≥65 years | ||||
| 30-day | 0 | (0.0) | 30 | (26.8) |
| 90-day | 1 | (8.3) | 40 | (35.7) |
| Overall | ||||
| 30-day | 3 | (3.9) | 41 | (17.4) |
| 90-day | 5 | (6.6) | 52 | (22.1) |
a Only numbers from North Jutland and Aarhus Counties.
b Charlson comorbidity index.
c Lymphoma, leukaemia and myeloma; Patients with myeloproliferative disease or myelodysplastic syndrome also included.
d Dialysis due to complications to the bacteremia not included.
e Both history of present and previous alcoholism included.
f Gastrectomy, vagotomy, gastric bypass.
There were also notable differences in outcome between the two groups of patients. Patients with TRB had shorter length of hospital stay and fewer extraintestinal sites of infection than patients with DAB, e.g. osteomyelitis, infected aortic aneurysm, intraabdominal abscess, or pleural empyema. The relative risk (RR) of death within 30 days was lower among patients with TRB (RR 0.2; [0.1-0.7]; RR of death after 90 days: 0.3; [0.1-0.7]). This was due to a high mortality among patients with DAB aged 65 years and above.
S. Enteritidis and S. Thyphimurium were among the most common serovars identified from both patients with DAB and TRB, together they counted for 55% and 37%, respectively. S. Dublin was the second most common serovar from patients with DAB (20%), but was rare among patients with TRB. Conversely, few patients with DAB had S. Virchow, which accounted for 10% of the serovars from patients with TRB. In total, 34 different serovars were identified among the domestically acquired infections, and 30 among the group of travel-related infections (Table 2).
Table 2.
Serovars isolated from patients with travel-related (TRB) and domestically acquired (DAB) bacteremia
| Serovar | TRB Number (%) (n = 78)* | Serovar | DAB Number (%) (n = 235) | ||
|---|---|---|---|---|---|
| S. Enteritidis | 23 | (29.5) | S. Enteritidis | 84 | (35.7) |
| S. Virchow | 8 | (10.3) | S. Dublin | 48 | (20.4) |
| S. Typhimurium | 6 | (7.7) | S. Typhimurium | 46 | (19.6) |
| S. Newport | 4 | (5.1) | S. Bovismorbificans | 6 | (2.6) |
| S. Panama | 4 | (5.1) | S. Newport | 5 | (2.1) |
| S. Aviana | 3 | (3.8) | S. Agona | 4 | (1.7) |
| S. Saint-Paul | 3 | (3.8) | S. Java | 4 | (1.7) |
| S. Corvallis | 2 | (2.6) | S. Oranienburg | 4 | (1.7) |
| S. Haifa | 2 | (2.6) | S. Infantis | 3 | (1.3) |
| S. Heidelberg | 2 | (2.6) | S. Chester | 2 | (0.9) |
| S. Java | 2 | (2.6) | S. Hadar | 2 | (0.9) |
| S. Poona | 2 | (2.6) | S. Heidelberg | 2 | (0.9) |
| Others | 17 | (21.8) | S. Poona | 2 | (0.9) |
| S. Saint-Paul | 2 | (0.9) | |||
| S. Thompson | 2 | (0.9) | |||
| Others | 19 | (8.1) | |||
*Two patients had double infections with different serovars.
Incidence and trends
Overall, the proportion of TRB was higher in the second 5-year period, 28.3% [range 25.7-32.5%], compared with the first 5-year period, 20.8% [range 15.6-28.2%] (RPP 1993-2003 vs. 2004-2008: 1.4; [0.9-2.0]). Higher annual numbers of DAB during the first period contributed to this difference. The overall incidence rate of TRB was 0.5/100,000 person-years, with the highest incidence rate in the age group 15-24 years (0.8/100,000 person-years).
Seasonal patterns
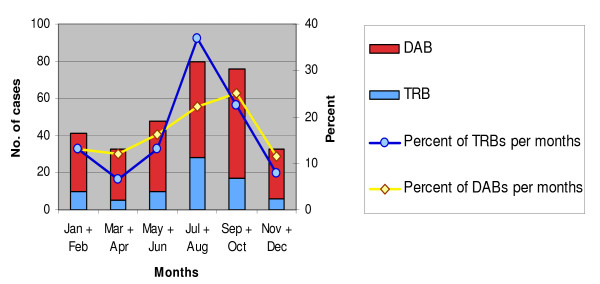
Both DABs and TRBs showed a seasonal variation when estimated within six periods of two months each. Most cases of DABs were found in the autumn months, September-October (59/235, 25%) and summer months, July-August (52/235, 22%). Travel-associated cases had a distinct peak in July-August (28/76, 37%), which were the months with most travellers (Figure 1).
Figure 1.
Seasonal pattern of travel-related (TRB) and domestically acquired (DAB) bacteremias, 1999-2008.
Travel duration and destinations
Information on the duration of stay was available in (53/76, 70%) of the TRB cases. The majority of patients had travelled for less than three weeks (40/53, 75%), giving a median stay of fourteen days (interquartile range (IQR) 9-21 days).
Patients hospitalized with TRB had travelled to 30 different countries. The highest numbers of TRBs were contracted in Thailand (16), followed by Greece (6), Spain (6), Egypt (5) and Turkey (5). Using data on travel patterns for Danish tourists as denominator, we found that the risk of hospitalization with Salmonella bacteremia were different between age groups and travel destinations (Table 3).
Table 3.
Estimated number of travellers and risk of bacteremia per 100,000 travellers by age groups and country (> 3 night stay)
| Age group/Country* | Number of travel-related bacteremias (TRB) (1999-2008) | Estimated number of travellers† (1999-2008) | Risk per 100,000 travellers (95% CI) | |
|---|---|---|---|---|
| 0-14 years | 13 | 3,300,000 | 0.4 | (0.2-0.7) |
| 15-24 years | 15 | 1,800,000 | 0.8 | (0.5-1.4) |
| 25-44 years | 16 | 3,730,000 | 0.4 | (0.3-0.7) |
| 45-64 years | 20 | 3,860,000 | 0.5 | (0.3-0.8) |
| ≥65 years | 12 | 980,000 | 1.2 | (0.7-2.2) |
| Spain | 6 | 1,340,000 | 0.4 | (0.2-1.0) |
| Sweden | 1 | 780,000 | 0.1 | (0.0-0.9) |
| Germany | 3 | 690,000 | 0.4 | (0.1-1.4) |
| Greece | 6 | 670,000 | 0.9 | (0.4-2.0) |
| Turkey | 5 | 440,000 | 1.1 | (0.5-2.8) |
| Poland | 2 | 340,000 | 0.6 | (0.1-2.4) |
| Portugal | 3 | 310,000 | 1.0 | (0.3-3.0) |
| Thailand | 16 | 300,000 | 5.3 | (3.3-8.7) |
| Egypt | 5 | 260,000 | 1.9 | (0.8-4.7) |
| Czech Republic | 2 | 220,000 | 0.9 | (0.2-3.7) |
| Bulgaria | 2 | 130,000 | 1.5 | (0.4-6.3) |
| Croatia | 1 | 90,000 | 1.1 | (0.2-8.1) |
| Vietnam | 4 | 75,000 | 5.3 | (1.9-15.0) |
| India | 1 | 75,000 | 1.3 | (0.2-9.7) |
| Mexico | 1 | 60,000 | 1.7 | (0.2-12.3) |
| United Arab Emirates | 1 | 35,000 | 2.9 | (0.4-21.7) |
| Ukraine | 1 | 35,000 | 2.9 | (0.4-21.5) |
| China | 1 | 30,000 | 3.3 | (0.4-25.5) |
| Tanzania | 1 | 25,000 | 4.0 | (0.5-31.2) |
| Malta | 1 | 8000 | 12.5 | (1.4-114.6) |
| Malaysia | 1 | 7000 | 14.3 | (1.5-137.3) |
| Ghana | 2 | 6000 | 33.3 | (5.6-199.5) |
| Senegal | 1 | 6000 | 16.7 | (1.7-160.2) |
*Number of travellers to Kenya, Cambodia, Guatemala, Indonesia, Iraq, Somalia and Uganda were not available. Three cases of TRB were contracted in Kenya and one case in each of the other countries.
† Numbers for the age group 0-14 years were based on the proportion of adults travelling with children
Relative risk of TRB compared to travel-related gastroenteritis 2004-2008
From 2004-2008, we identified 2865 patients with Salmonella gastroenteritis in the REP after exclusion of patients with bacteremia and cases of typhoid or paratyphoid fever. All patients were residents in one of the three counties at the time of positive fecal cultures. Of these, 527 (18.4%) patients were recorded as having travel-related Salmonella gastroenteritis.
We found Sub-Saharan Africa, the Middle East, and South East Asia to be high-risk regions for contracting TRB when compared to contemporary cases of travel-associated Salmonella gastroenteritis. An increased risk was also found in the age group of 65 years and above, but there were no difference related to sex (Table 4).
Table 4.
Relative risk of travel-related bacteremia (TRB) compared to travel-related gastroenteritis, 2004-2008*
| Variable | Number of TRBs (n = 43) | Odds ratio† | 95% CI |
|---|---|---|---|
| Male | 28 | 1.0 | 0.7-1.4 |
| Age ≥65 years | 6 | 5.3 | 3.7-7.6 |
| Travel region‡ | 7 | 18.4 | 6.9-49.5 |
| Sub-Saharan Africa | 2 | 10.6 | 2.1-53.2 |
| Middle East | 14 | 4.0 | 2.2-7.5 |
| South East Asia |
*Both voluntary and interview-based information were available during this period
†Adjusted for other risk factors in the model
‡Travel regions included in the analyses: East Asia & India, Eastern Europe & Russia, Middle East, Northern Africa, South East Asia, Southern Europe & Eastern Mediterranean, Sub-Saharan Africa, The Americas, Western Europe & Nordic countries
Discussion
In this cohort study, we found that the overall incidence of patients hospitalized with travel-related non-typhoidal Salmonella bacteremia was low (0.5/100,000 person-years). Still, one in four cases hospitalized with Salmonella bacteremia in Denmark was associated with travel. The risk was most pronounced for the elderly and the young adult travellers and for travellers to countries in the regions of Sub-Saharan Africa, the Middle East and South East Asia. However, patients with travel-related infections were less likely to have poor outcomes than patients with domestically acquired infections. Our data also suggested an increasing trend in the proportion of TRBs, which is further supported by the previous Danish population-based study from the 1980s [10]. One crucial factor is probably the major reduction in the incidence of domestically acquired Salmonella infections which followed implementation of a national Salmonella control program in 1997 [19,20]. During the last three decades the popularity of overseas travel has been increasing and together these two trends are likely to have changed the national 'balance sheet' for invasive Salmonella infections.
Our study has a number of important limitations. First, our study design only allowed for detection of Salmonella infections among hospitalized patients and our results were therefore based on estimates of the risk of being hospitalized with bacteremia and not on the risk of falling ill for which no data were available. Although, we believe that our study included all severe cases of invasive Salmonella infections, patients with a fever and a history of international travel may have been hospitalized at a lower threshold of clinical suspicion than patients with domestically acquired infections. This would lead to a potential overestimation of the proportion of TRB as compared with DABs. Second, we only included patients with bacteremia diagnosed after their return to Denmark. Travellers who were diagnosed and treated for bacteremia abroad therefore did not appear in the data. Admission and treatment at local hospitals may be more likely for travellers staying abroad for extended periods and the risk of bacteremia may therefore be biased towards destinations typically associated with shorter stays. Third, we were not able to validate the travel information given in hospital charts which relied on the clinicians' notes. If bias were introduced, it would most likely be in the form of 'missing data' on foreign travel. This would entail a potential underestimation of the proportion of TRBs. However, when considering the potential for misclassification of the travel information, we still believe that the different risk estimates reflect genuine differences in exposure.
Previous studies have shown the greatest risk of non-typhoidal Salmonella bacteremia at the extremes of age and we expected to find the same age distribution among patients with TRB [21]. Several predisposing comorbidities are acknowledged risk factors for Salmonella bacteremia, e.g. chronic or immunosuppressing conditions, including malignancy, rheumatological disease, liver disease, and diabetes [22-24], and it is likely that the elevated risk of TRB in the elderly reflected an increased prevalence of comorbidities in this age group. We used the Charlson comorbidity index as a summary measure of the patients' comorbidities, which includes 19 major disease categories, several of which are known risk factors for Salmonella bacteremia. Comparison of the burden of comorbidity in patients ≥65 years with that of patients <65 years (data not included in the results) showed that 67% (8/12) of patients ≥65 years had one or more diseases registered in the Charlson index compared with only 22% (14/64) in patients <65 years (RPP for ≥1 comorbid disease: 3.0 [95% CI: 1.7-5.6]).
A previous study suggested that accommodation, travel characteristics, and dietary hygiene are important factors for the evaluation of traveller's risk of diarrhea [25] and that the higher risk of traveller's diarrhea found in young adults may be associated with ingestion of larger volumes of potentially contaminated food and an adventurous lifestyle in this age group [26]. These behavioural factors would be important for the higher risk of Salmonella bacteremia in young adults, although the risk was only marginally higher than that reported for other age groups. A formal analysis was not possible as we had no data on behavioral factors or precise data on travel form.
Comparison of the characteristics between patients hospitalized with TRB and DAB (Table 1) illustrated that the two groups were fundamentally different. There were major differences in clinical outcomes between the groups. Thus, patients with TRB had a shorter length of hospital stay, fewer complications, and lower mortality than patients with DAB. The explanation for the latter observation is likely to be a "healthy traveller effect" as illustrated by the lower prevalence of comorbidities in the group of patients infected abroad. This is consistent with a Swedish study on Salmonella-associated deaths where persons infected domestically had a much more severe prognosis than those infected abroad [27].
Earlier studies have shown that the distribution of serovars may vary much by geographic location and time [28,29]. Overall, S. Enteritidis was the predominant serovar in Denmark throughout the study period, even though S. Typhimurium was the most frequent serovar in the last year of the study (2008) because of an unprecedented, large nationwide outbreak [14]. S. Enteritidis was also the most common serovar in Europe and dominant in most of the travel regions [9]. This is in accordance with our finding that S. Enteritidis was the most frequent serovar both in patients with TRB and DAB. S. Virchow and S. Dublin were the second most common serovars isolated from patients with TRB or DAB, even though S. Typhimurium were a much more common serovar in most regions of the world. Both S. Virchow and S. Dublin show a higher propensity for causing bacteremia and more severe infections than S. Typhimurium [21,30]. This suggests that the distribution of serovars was due to both the overall abundance of serovars as well as the exposure to more invasive serovars.
Conclusions
International travel is an acknowledged risk factor for non-typhoidal Salmonella gastroenteritis, however, little is known regarding the risk of potentially more severe invasive Salmonella infections. This study demonstrated that international travel is a notable risk factor for being hospitalized with non-typhoidal Salmonella bacteremia and the risk differs among travellers according to age and travel destination. Still, the overall risk is low and healthy travellers with bacteremia are less likely to have poor outcomes compared to patients with domestically acquired bacteremia. Our findings may be useful for the clinical evaluation of travellers presenting with fever and may also support pre-travel counselling.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
KK participated in the study design, was responsible for data collection, statistical analysis and interpretation of data and drafted the manuscript. BK and HMH assisted in data collection and interpretation of data. SE and KM participated in the design, data collection and analysis and critically reviewed the manuscript. HCS was responsible for the study design and assisted with data collection, statistical analysis, interpretation of data and drafting the manuscript. All authors reviewed and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Kristoffer Koch, Email: k.koch@rn.dk.
Brian Kristensen, Email: brian.kristensen@skejby.rm.dk.
Hanne M Holt, Email: hanne.holt@ouh.regionsyddanmark.dk.
Steen Ethelberg, Email: set@ssi.dk.
Kåre Mølbak, Email: krm@ssi.dk.
Henrik C Schønheyder, Email: hcs@rn.dk.
Acknowledgements
This study was in part funded by the North Denmark Region and the private foundation of Heinrich Kopp which supports health care research. The funders had no role in study design, in the analysis and interpretation of data, in writting the manuscript, or in the decision to submit the manuscript for publication.
References
- Tourism Authority of Thailand (TAT), Tourism Statistics. http://www2.tat.or.th/stat/web/static_index.php
- Askling HH, Rombo L, Andersson Y, Martin S, Ekdahl K. Hepatitis A risk in travelers. J Travel Med. 2009;16:233–238. doi: 10.1111/j.1708-8305.2009.00307.x. [DOI] [PubMed] [Google Scholar]
- Leggat PA, Zwar NA, Hudson BJ. Hepatitis B risks and immunisation coverage amongst Australians travelling to southeast Asia and east Asia. Travel Med Infect Dis. 2009;7:344–349. doi: 10.1016/j.tmaid.2009.03.008. [DOI] [PubMed] [Google Scholar]
- Cobelens FG, Groen J, Osterhaus AD, Leentvaar-Kuipers A, Wertheim-van Dillen PM, Kager PA. Incidence and risk factors of probable dengue virus infection among Dutch travellers to Asia. Trop Med Int Health. 2002;7:331–338. doi: 10.1046/j.1365-3156.2002.00864.x. [DOI] [PubMed] [Google Scholar]
- Thomson MM, Najera R. Travel and the introduction of human immunodeficiency virus type 1 non-B subtype genetic forms into Western countries. Clin Infect Dis. 2001;32:1732–1737. doi: 10.1086/320764. [DOI] [PubMed] [Google Scholar]
- Lynch MF, Blanton EM, Bulens S, Polyak C, Vojdani J, Stevenson J, Medalla F, Barzilay E, Joyce K, Barrett T, Mintz ED. Typhoid fever in the United States, 1999-2006. JAMA. 2009;302:859–865. doi: 10.1001/jama.2009.1229. [DOI] [PubMed] [Google Scholar]
- Lester A, Mygind O, Jensen KT, Jarlov JO, Schønheyder HC. [Typhoid and paratyphoid fever in Denmark 1986-1990. Epidemiologic aspects and the extent of bacteriological follow-up of patients] Ugeskr Laeger. 1994;156:3770–3775. [PubMed] [Google Scholar]
- Ekdahl K, de JB, Andersson Y. Risk of travel-associated typhoid and paratyphoid fevers in various regions. J Travel Med. 2005;12:197–204. doi: 10.2310/7060.2005.12405. [DOI] [PubMed] [Google Scholar]
- Ekdahl K, de JB, Wollin R, Andersson Y. Travel-associated non-typhoidal salmonellosis: geographical and seasonal differences and serotype distribution. Clin Microbiol Infect. 2005;11:138–144. doi: 10.1111/j.1469-0691.2004.01045.x. [DOI] [PubMed] [Google Scholar]
- Lester A, Eriksen NH, Nielsen H, Nielsen PB, Friis-Møller A, Bruun B, Scheibel J, Gaarslev K, Kolmos HJ. Non-typhoid Salmonella bacteraemia in Greater Copenhagen 1984 to 1988. Eur J Clin Microbiol Infect Dis. 1991;10:486–490. doi: 10.1007/BF01963934. [DOI] [PubMed] [Google Scholar]
- Ispahani P, Slack RC. Enteric fever and other extraintestinal salmonellosis in University Hospital, Nottingham, UK, between 1980 and 1997. Eur J Clin Microbiol Infect Dis. 2000;19:679–687. doi: 10.1007/s100960000341. [DOI] [PubMed] [Google Scholar]
- Matheson N, Kingsley RA, Sturgess K, Aliyu SH, Wain J, Dougan G, Cooke FJ. Ten years experience of Salmonella infections in Cambridge, UK. J Infect. 2010;60:21–25. doi: 10.1016/j.jinf.2009.09.016. [DOI] [PubMed] [Google Scholar]
- Sirichote P, Hasman H, Pulsrikarn C, Schønheyder HC, Samulioniene J, Pornruangmong S, Bangtrakulnonth A, Aarestrup FM, Hendriksen RS. Molecular characterization of extended-spectrum cephalosporinase-producing Salmonella enterica serovar Choleraesuis isolates from patients in Thailand and Denmark. J Clin Microbiol. 2010;48:883–888. doi: 10.1128/JCM.01792-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ethelberg S, Müller L, Mølbak K, Nielsen EM. [Salmonella and campylobacter infections in 2008] Ugeskr Laeger. 2010;172:1451–1455. [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Statistics Denmark, StatBank Denmark. http://www.statistikbanken.dk
- Blom M, Meyer A, Gerner-Smidt P, Gaarslev K, Espersen F. Evaluation of Statens Serum Institut enteric medium for detection of enteric pathogens. J Clin Microbiol. 1999;37:2312–2316. doi: 10.1128/jcm.37.7.2312-2316.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popoff MY, Le Minor L. Antigenic formulas of the Salmonella serovars. WHO Collaborating Centre for Reference and Research on Salmonalle, Institut Pasteur, Paris, France; 1997. [Google Scholar]
- Wegener HC, Hald T, Lo Fo WD, Madsen M, Korsgaard H, Bager F, Gerner-Smidt P, Mølbak K. Salmonella control programs in Denmark. Emerg Infect Dis. 2003;9:774–780. doi: 10.3201/eid0907.030024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korsgaard H, Madsen M, Feld NC, Mygind J, Hald T. The effects, costs and benefits of Salmonella control in the Danish table-egg sector. Epidemiol Infect. 2009;137:828–836. doi: 10.1017/S0950268808000903. [DOI] [PubMed] [Google Scholar]
- Jones TF, Ingram LA, Cieslak PR, Vugia DJ, Tobin-D'Angelo M, Hurd S, Medus C, Cronquist A, Angulo FJ. Salmonellosis outcomes differ substantially by serotype. J Infect Dis. 2008;198:109–114. doi: 10.1086/588823. [DOI] [PubMed] [Google Scholar]
- Dhanoa A, Fatt QK. Non-typhoidal Salmonella bacteraemia: epidemiology, clinical characteristics and its' association with severe immunosuppression. Ann Clin Microbiol Antimicrob. 2009;8:15. doi: 10.1186/1476-0711-8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon MA. Salmonella infections in immunocompromised adults. J Infect. 2008;56:413–422. doi: 10.1016/j.jinf.2008.03.012. [DOI] [PubMed] [Google Scholar]
- Hsu RB, Lin FY. Risk factors for bacteraemia and endovascular infection due to non-typhoid salmonella: a reappraisal. QJM. 2005;98:821–827. doi: 10.1093/qjmed/hci126. [DOI] [PubMed] [Google Scholar]
- Kollaritsch H. Traveller's diarrhea among Austrian tourists in warm climate countries: I. Epidemiology. Eur J Epidemiol. 1989;5:74–81. doi: 10.1007/BF00145049. [DOI] [PubMed] [Google Scholar]
- De Las CC, Adachi J, Dupont H. Review article: travellers' diarrhoea. Aliment Pharmacol Ther. 1999;13:1373–1378. doi: 10.1046/j.1365-2036.1999.00638.x. [DOI] [PubMed] [Google Scholar]
- Ternhag A, Torner A, Ekdahl K, Giesecke J. Salmonella-associated deaths, Sweden, 1997-2003. Emerg Infect Dis. 2006;12:337–339. doi: 10.3201/eid1202.050867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendriksen RS, Bangtrakulnonth A, Pulsrikarn C, Pornruangwong S, Noppornphan G, Emborg HD, Aarestrup FM. Risk factors and epidemiology of the ten most common Salmonella serovars from patients in Thailand: 2002-2007. Foodborne Pathog Dis. 2009;6:1009–1019. doi: 10.1089/fpd.2008.0245. [DOI] [PubMed] [Google Scholar]
- de Jong B, Ekdahl K. The comparative burden of salmonellosis in the European Union member states, associated and candidate countries. BMC Public Health. 2006;6:4. doi: 10.1186/1471-2458-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schønheyder HC, Ejlertsen T. Survey of extraintestinal nontyphoid Salmonella infections in a Danish region. Inverse relation of invasiveness to frequency of isolation. APMIS. 1995;103:686–688. doi: 10.1111/j.1699-0463.1995.tb01423.x. [DOI] [PubMed] [Google Scholar]