Abstract
PURPOSE
To review the peritoneal dialysis (PD) catheter outcomes at our center and assess factors affecting the catheter survival.
METHODS
We carried out a retrospective study on 315 patients who had their first PD catheter placed between January 2001 and September 2009 at the UT Southwestern/DaVita Peritoneal Dialysis Clinic at Dallas, Texas. Medical records were reviewed for demographic and clinical information of the patients. The primary end point of the study was PD catheter failure, defined as removal of a dysfunctional PD catheter due to catheter-related complications. Catheter survival was estimated using Kaplan Meier method. Cox proportional hazard regression model was used to identify factors that are independently associated with catheter survival.
RESULTS
The mean age of the patients was 49.7 +/− 29 years. The study population included 54.6% females; 42.5% African American, 27.9% Caucasian and 22.9% Hispanic patients. Diabetes was the primary etiology of end-stage renal disease in 43.2% of patients. More than 90% of patients had one or more co-morbidities; and 57.5% had previous abdominal surgery. The mean BMI for the group was 28.6 +/− 13.8 kg/m2. Less than a quarter of the patients (24.1%) had non-infectious/mechanical catheter problems.
Overall PD catheter survival rates over 12, 24 and 36 months were 92.9%, 91.9% and 91.1%, respectively. PD catheter-related non-infectious problem was the only independent variable that was significantly associated with catheter survival (Hazard ratio 22.467; 95% CI 6.665– 75.732). No significant association was observed between the PD catheter survival and other risk factors including age, BMI, diabetic status, comorbidities, previous abdominal surgeries or infections.
CONCLUSIONS
Our study shows an excellent 3-year PD catheter survival (91.1%). Only PD catheter-related non-infectious problems are significantly associated with catheter failure. Other factors such as age, gender, race, BMI, diabetic status, comorbidities, previous abdominal surgeries, peritoneal infections or exit-site/ tunnel infections were not found to affect the PD catheter survival and should not be considered barriers to PD initiation.
Keywords: Peritoneal dialysis catheter, survival, risk factors
Introduction
Since its inception in the seventies, continuous ambulatory peritoneal dialysis (CAPD) has become a successful and effective form of therapy for end stage renal disease (ESRD) globally (1, 2). Peritoneal dialysis (PD) provides patients with ESRD the choice of an effective home dialysis modality with self-autonomy, and supports optimal quality of life (3–8). The three essential elements of PD are:
A viable peritoneal cavity lined by a functional membrane
Access to the peritoneal cavity, usually by means of indwelling catheter
Dialysis fluid and delivery mechanisms.
Numerous studies have examined the factors influencing peritoneal membrane viability and dialysis technique success. Majority of the data available is concentrated around the effect of peritonitis episodes on peritoneal membrane, dialysis technique and patient survival outcomes (9–13). Whereas free access to peritoneal cavity is essential for successful PD outcomes (14, 15), data on the factors affecting PD catheter survival are sparse.
The present study evaluates various risk factors associated with the survival of the first peritoneal dialysis catheter in PD patients.
Patients and methods
We retrospectively studied all PD patients at the Peritoneal Dialysis Clinic of DaVita/University of Texas Southwestern (UTSW) Medical Center at Dallas, Texas, who had their first PD catheter placed between January 1, 2001 and September 1, 2009. Inclusion criteria were insertion of a PD catheter at UT Southwestern hospitals during the study period. Those patients who had their PD catheter surgery elsewhere were excluded. The study was approved by the Institutional Review Board of the UT Southwestern Medical Center.
A total of 339 PD catheters were inserted over this period in 315 patients. For the 24 patients with repeated PD catheter insertion surgeries, only the first catheter was considered for the study. All catheters were double-cuffed, pig-tailed Tenckhoff catheters and were placed surgically by two surgeons. All patients were followed by a single nephrologist.
The medical records of the 315 patients included in the study were reviewed for their demographic and clinical characteristics including age, gender, race, body mass index (BMI), primary etiology of ESRD, co-morbidities and prior abdominal surgeries. The patients were followed up from the date of PD catheter insertion and data were collected regarding the infectious and non-infectious complications during the course of peritoneal dialysis. The primary end point of the study was PD catheter failure, defined as removal of a dysfunctional PD catheter due to various catheter-related causes (detailed under Definitions). Additional events like removal of functioning PD catheter due to other causes (see Definitions), discontinuation of PD due to renal transplant, transfer out to other centers and, deaths of the patient were also recorded. These were classified as the censoring events. We also reviewed the Primary and Secondary PD catheter failure events.
The median follow-up period was 19 months (Range 0.5 month to 102 months). Out of 315 patients, 235 (74.6%) patients had a follow-up time from 0.5 month to maximum of 33 months. The longer follow-up times were censored at 36 months for the purpose of analysis of PD catheter survival estimates.
Definitions
PD catheter failure was defined as removal of the dysfunctional PD catheter due to any catheter-related complication. The catheter-related complications were divided into infectious and non-infectious groups. PD catheter infectious group included exit-site infections (ESI), tunnel infections (TI) and peritonitis associated with ESI and/or TI. The non-infectious complications included intra-luminal/ extra-luminal obstruction, catheter mal-positioning, catheter migration, omental wrap around the catheter, catheter leakage and catheter extrusion.
Primary PD catheter failure was defined as the removal of PD catheter when the PD catheter never functioned due to any catheter-related problem. When the catheter functioned for some time and later became dysfunctional due to a catheter-related complication (infectious and/or non-infectious) and subsequently removed, it was referred to as Secondary PD catheter failure.
Removal of functioning PD catheter was designated to one of the censoring events. The causes for functioning PD catheter removal formed a whole spectrum of events including relapsing/ refractory/ fungal peritonitis, poor solute clearance on PD, idiopathic chronic abdominal pain, modality change to hemodialysis for any major surgery, prolonged hospitalization, and social issues like lack of family support, physical handicap, job demands, patient preference and non- adherence to treatment.
The co-morbidities taken into account for this study were hypertension, dyslipidemia, cardio-vascular diseases, cancer, Human Immunodeficiency Virus (HIV) positive status, chronic airway/ pulmonary disease, connective tissue disorders, inflammatory bowel disease and hernias.
The previous abdominal surgeries considered were cesarean-sections, total abdominal hysterectomy with or without salpingo-ophorectomy, laparotomy, cholecystectomy, appendectomy, hernia repair, previous peritoneal dialysis, nephrectomy and renal transplant.
Statistical Analysis
Catheter survival was analyzed by the Kaplan-Meier method. Cox proportional hazard regression model was used to identify factors that are independently associated with catheter survival. All demographic and clinical characteristics and complications during the PD were included as covariates. A p value of less than 0.05 was considered statistically significant. Statistical analyses were performed with SAS software, version 9.1 (SAS Institute, Inc, Cary, NC).
Results
Patient demographic and clinical characteristics
From January 2001 to September 2009, 315 patients had their first PD catheter inserted at UT Southwestern hospital. Table 1 lists the demographic and clinical characteristics of the patients. There were 172 (54.6%) female and 143 (45.4%) male patients. The mean age was 49.7 +/− 29 years. There were 134 (42.5%) African American, 21 (6.7%) Asian, 88 (27.9%) Caucasian and 72 (22.9%) Hispanic patients in the sample. The mean (± sd) BMI was 28.6 (±13.8) kg/m2 (range 14.4–54.5 kg/m2).
Table 1.
Patient demographic and clinical characteristics
| Number of patients (%) | |
|---|---|
| Gender | |
| Male | 143 (45.4) |
| Female | 172 (56.4) |
| Race | |
| African American | 134 (42.5) |
| Asian | 21 (6.7) |
| Caucasian | 88 (27.9) |
| Hispanic | 72 (22.9) |
| Etiology of ESRD | |
| Diabetes Mellitus | 136 (43.2) |
| Hypertension | 56 (17.8) |
| Lupus nephritis | 19 (6.0) |
| Focal segmental glomerulosclerosis | 15 (4.8) |
| Polycystic kidney disease | 13 (4.1) |
| Others | 76 (24.1) |
| Number of co-morbidities | |
| 0 | 20 (6.3) |
| 1 | 107 (34.0) |
| 2 | 110 (34.9) |
| >2 | 78 (24.8) |
| Number of previous abdominal surgeries | |
| 0 | 134 (42.5) |
| 1 | 85 (27.0) |
| 2 | 43 (13.7) |
| >2 | 53 (16.8) |
Diabetes Mellitus was the primary cause of ESRD in 136 (43.2%) patients. There were 20 (6.3%) patients who had no comorbid conditions, 107 (34.0%) patients had 1, 110 (34.9%) had 2, while 78 (24.8%) had more than 2 co-morbid conditions. We had 134 (42.5%) patients with no previous abdominal surgeries, while 85 (27.0%) had a single and 96 (30.5%) patients had multiple previous abdominal surgeries.
Complications during peritoneal dialysis
Table 2 shows the number of infectious and non-infectious complications during the study period. One hundred and ninety (60.3%) patients did not have any episode of peritoneal infection, while 66 (21.0%) had a single episode and 59 (18.7%) had multiple episodes of peritonitis. There were, 243 (77.1%) patients with no PD catheter related exit site or tunnel infection while 54 (17.1%) had a single infection and only 18 (5.8%) had more than 1 infectious episodes. The review of PD catheter-related non-infectious complications showed that 239 (75.9%) patients had no problems whereas 66 (20.9%) patients had a single non-infectious problem and only 10 (3.2%) patients had problems more than once during the follow up period. Table 3 gives an account of various non-infectious complications related to PD catheter.
Table 2.
Peritoneal dialysis complications
| Number of patients (%) | |
|---|---|
| Infectious complications | |
| Number of peritonitis | |
| 0 | 190 (60.3) |
| 1 | 66 (21.0) |
| >1 | 59 (18.7) |
| Number of exit-site & tunnel infections | |
| 0 | 243 (77.1) |
| 1 | 54 (17.1) |
| >1 | 18 (5.8) |
| Number of non-infectious complications | |
| 0 | 239 (75.9) |
| 1 | 66 (20.9) |
| >1 | 10 (3.2) |
Table 3.
Non-infectious complications related to PD catheter: 76 patients experienced 87 episodes of non-infectious complications.
| No. of episodes (N=87) |
No. of patients (N=76) |
Reason for PD catheter removal from non- infectious complications (N=21)* |
|
|---|---|---|---|
| Mal-positioning/Tip migration | 28 | 25 | 8 |
| Obstruction | 11 | 11 | 6 |
| Catheter leak | 8 | 7 | 1 |
| Cather extrusion | 7 | 7 | 1 |
| Hole in the external part | 15 | 14 | 0 |
| Hematoma around the exit-site | 6 | 6 | 0 |
| Trauma | 3 | 3 | 0 |
| Chronic abdominal pain | 2 | 2 | 1 |
| Mal-functioning due to undocumented reasons | 7 | 7 | 4 |
2 additional catheters were removed due to persistent ESI/TI (catheter-related infectious complications).
PD catheter survival analysis
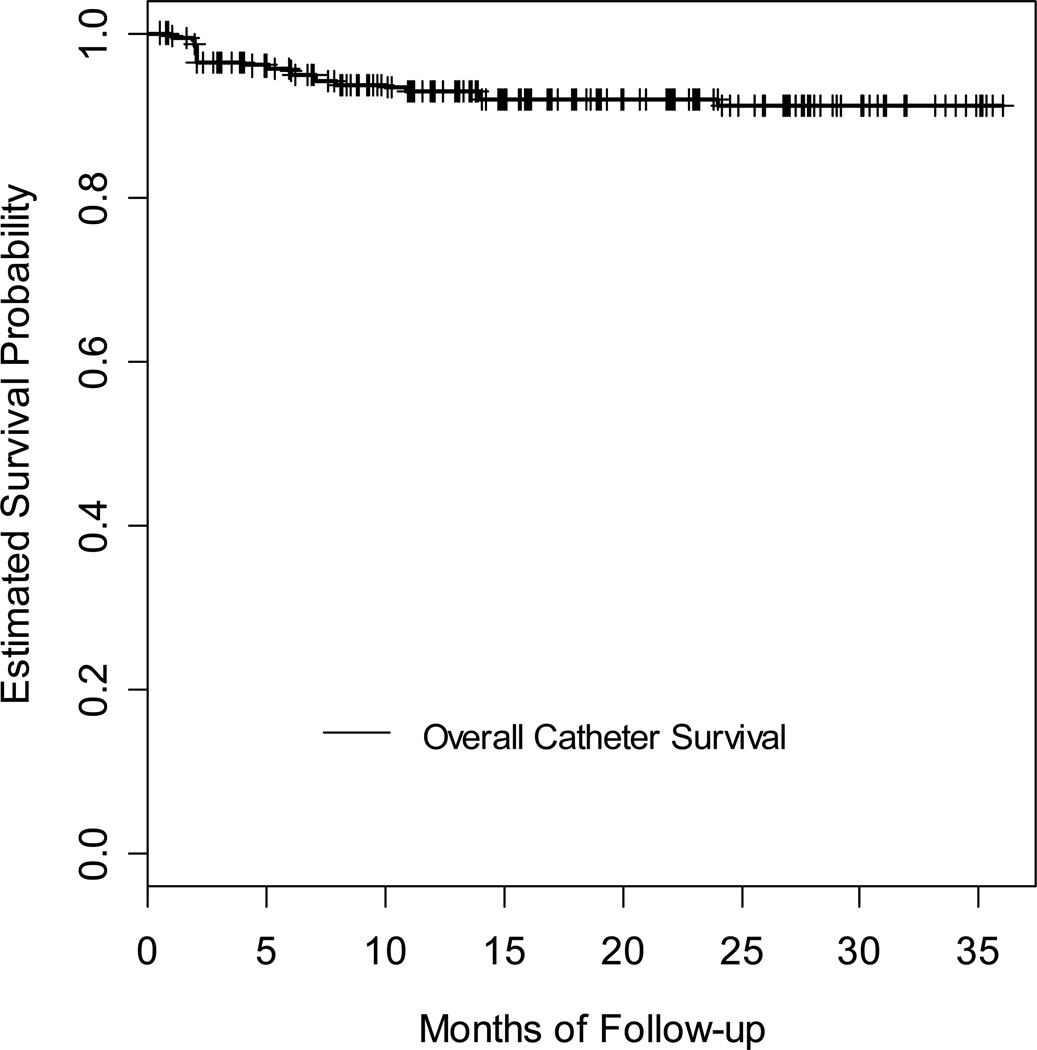
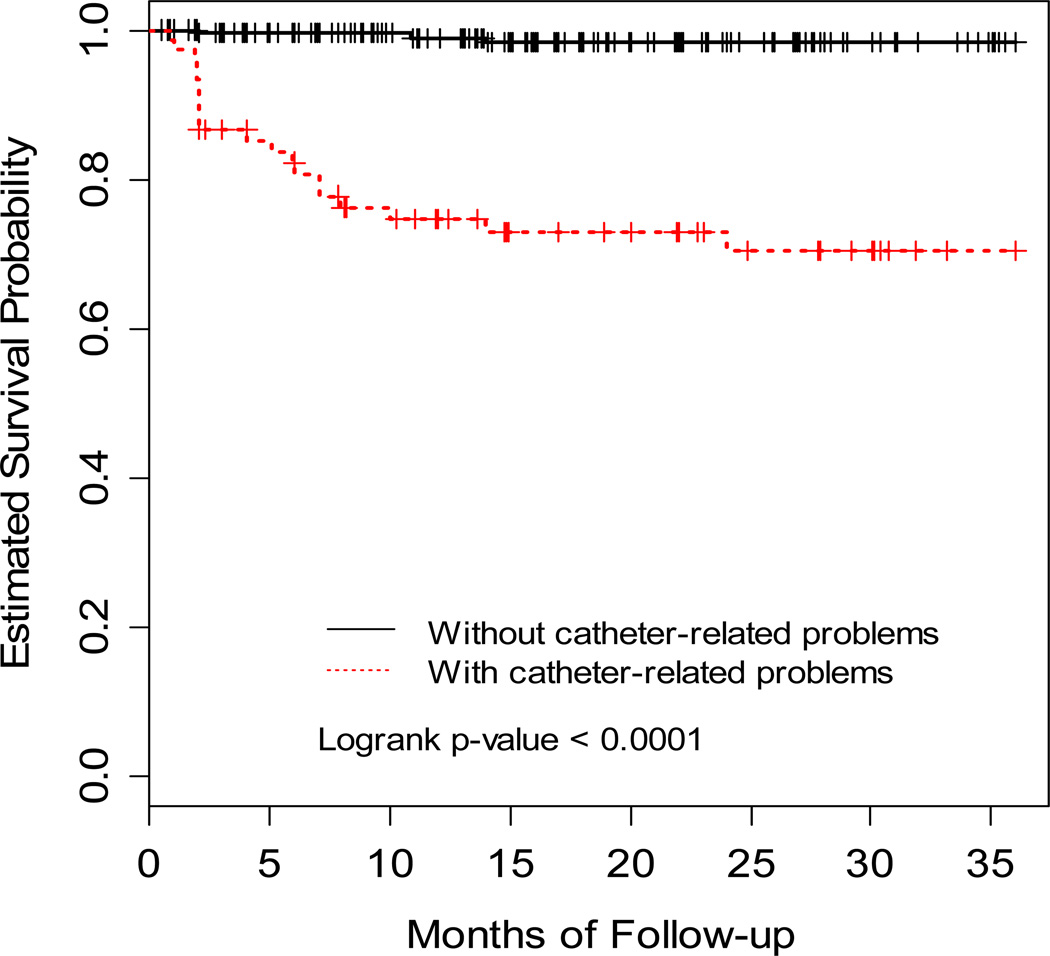
Overall PD catheter survival rate at 12, 24 and 36 months were 92.9%, 91.9% and 91.1% respectively (Fig. 1) Altogether, we observed 23 catheter failures within the 3 years of the follow up period. A descriptive analysis of these 23 catheter failures showed that 13 (13/23, 56.5%) catheters did not function at all, leading to primary PD catheter failure. The remaining 10 catheters (10/23, 43.5%) functioned for some time before developing secondary PD catheter failure. Table 4 demonstrates the association between the PD catheter survival times with various covariates. PD catheter-related non-infectious problem was the only independent variable that significantly affected the catheter survival time (Hazard ratio 22.467; 95% CI 6.665– 75.732). (Fig. 2) Having a PD catheter non-infectious problem increased the risk of catheter failure more than 22 times compared to the patients who did not have any non-infectious complication related to the PD catheter. We did not observe any significant association between the PD catheter survival and other risk factors like age, BMI, diabetic status, co-morbidities, previous abdominal surgeries or infections (Table 4).
Figure 1. Kaplan Meier curve for overall catheter survival probability.
One, two and three year catheter survival rates were 92.9% (20 catheter failures), 91.9% (22 catheter failures) and 91.1% (23 catheter failures) respectively.
Table 4.
Analysis of PD catheter survival with various covariates according to Cox proportional hazard model
| Variable | Beta Estimate |
SE | Chi-square (p-value) |
Hazard Ratio (HR) |
95% Confidence Interval for HR |
|---|---|---|---|---|---|
| Age | 0.017 | 0.01 | 1.29 (0.256) | 1.017 | 0.997, 1.037 |
| Gender | 0.28 (0.594) | 1.256 | |||
| Female | 0.228 | 0.43 | 0.541, 2.918 | ||
| Race | 0.65 (0.885) | ||||
| Hispanic | 0.463 | 1.10 | 1.589 | 0.184, 13.722 | |
| White | 0.689 | 1.06 | 1.992 | 0.249, 15.904 | |
| African American | 0.408 | 1.05 | 1.504 | 0.192, 11.775 | |
| BMI | 0.014 | 0.03 | 0.26 (0.609) | 1.013 | 0.956, 1.076 |
| Etiology of ESRD (Diabetes) |
0.545 | 0.42 | 1.70 (0.193) | 1.724 | 0.757, 3.928 |
| Co-morbidities | −0.066 | 0.20 | 0.11 (0.743) | 0.745 | 0.633, 1.385 |
| Previous Abdominal Surgeries |
0.000 | 0.14 | 0.00 (0.999) | 1.000 | 0.760, 1.316 |
| Peritoneal Infections | 3.57 (0.168) | ||||
| 1 Infection | −0.858 | 0.63 | 0.424 | 0.123, 1.458 | |
| 2 or more infections |
−0.847 | 0.63 | 0.429 | 0.125, 1.474 | |
| Exit-site/ Tunnel Infection |
−0.193 | 0.51 | 0.151 (0.698) | 0.825 | 0.303, 2.240 |
| Non-infectious Catheter Problem |
3.112 | 0.62 | 42.71 (<0.001) |
22.467 | 6.665, 75.732 |
Figure 2. Kaplan Meier curve for catheter survival times for the patients with and without PD catheter-related non-infectious problems.
Patients with catheters that have non-infectious complication experience significantly more catheter failure (RED line) as compared to patients without any non-infectious complication (Beta-estimate 3.112; Hazard ratio 42.71, 95% C.I. 6.665, 75.732)
Discussion
This is a retrospective study examining various risk factors associated with the survival of first PD catheters placed at UT Southwestern/ DaVita PD center between January 2001 and September 2009. The 1-year, 2-year and 3-year PD catheter survival was 92.9%, 91.9% and 91.1%, respectively. This is a superior PD catheter outcome than that observed in some previous studies (16, 17). A prospective study done on 72 patients who had their first PD catheters (double-cuff Tenchkoff catheters) surgically inserted between 1992 and 1995, showed that the 1-year, 2-year and 3-year survivals were 62.5%, 41.5% and 36%, respectively (16). However, unlike the present study, persistent peritonitis leading to removal of functioning PD catheter was considered as one of the causes of catheter failure. This would have contributed to their increased catheter failure rate. A larger study with 203 patients carried out over a period from 1982 to 1995 and including mechanical problems and catheter infections with/without associated peritonitis as the cause of PD catheter-failure, reported 1 a n d 3-year survivals of the first catheters as 75% and 37%, respectively (17). The outcome was far below our success rate. Our data however is comparable to the PD catheter survival demonstrated in a more recent prospective study enrolling 120 patients between 1996 and 2003 with similar study design and end-points as ours. It demonstrated 97% PD catheter survival at 2 years and 92.2% at 5 years (18). All these results when put together exhibit an improvement in the survival of the PD catheters over the last decade likely due to improved surgical techniques and post-operative care in the recent years. Further investigation is warranted to examine the changing pattern of surgical techniques and post-operative care and their effect on PD catheter survival.
On further investigation of different variables in our study, we observed that PD catheter-related non-infectious complication was the single covariate that significantly reduced the catheter survival time (Fig. 2). Each PD catheter-related problem increased the risk of catheter failure more than 22 times (Hazard ratio 22.467). Further analysis of the PD catheter survival revealed a steep decline in catheter survival about 3 months following the catheter placement in patients with any PD catheter related non-infectious problems as compared to those without any non-infectious complications (Fig. 2). This suggests that the maximum impact of the non-infectious PD catheter complications leading to PD catheter failure ensues in the early stages of PD, presumably in the first 3 months following surgery. This is comprehensible as the immediate post-operative period is a crucial stage following introduction of the PD catheter into the peritoneal cavity. It is reasonable to believe that the risks of mal-positioning, migration, extrusion, kinking, obstruction due to fibrin clots and non-functioning would be utmost in the early period following the operative procedure. To our knowledge, this is the first study showing the effect of PD catheter-related non-infectious problems on the catheter survival.
None of the other demographic (age, gender, race) or clinical characteristics (BMI, diabetic status, co-morbidities, previous abdominal surgeries or any infections (peritonitis, exit-site or tunnel infections) were found to be significantly associated with the PD catheter survival.
It has been perceived that abdominal surgeries are associated with mechanical complications of PD catheters and may affect their survival (19). To our surprise, we did not find any significant association between abdominal surgeries and PD catheter survival. Our data is in concurrence with the results of another large study that examined the outcomes of 436 catheters placed between 2000 and 2007. It did not find any significance of previous abdominal surgeries on catheter survival (13). Thus history of abdominal surgeries does not adversely affect the PD catheter outcome, and should not be considered a barrier to patient selection for PD.
Obesity is frequently considered as an impediment for PD catheter surgery. There is limited data on the effect of obesity on PD catheter survival. While a large study done on 9679 PD patients showed adverse effect of obesity on PD technique and patient survival, the effect of body mass on PD catheter survival was not studied separately (20). The present study included patients with a wide range of BMI, but did not reveal any significant risk of higher BMI on PD catheter outcomes. Similar results were observed in a previous study on 351 PD catheters, which showed that body weight has no significant correlation with PD catheter removal due to non-infectious/mechanical causes (21). Based on these results, BMI should not be used as a factor negatively influencing the eligibility of a patient to perform PD.
Presence of co-morbidities is an important attribute considered at the time when dialysis modality for a patient with chronic kidney disease (CKD) is being contemplated. However, to our knowledge, no previous data is available that examines the effect of comorbidities on PD catheter survival. Our study did not find any association between comorbidities and PD catheter survival suggesting that co-morbidities should not be used as an index during patient selection for PD.
Another factor commonly considered before initiating a patient on PD is age. A large study done over a period of 10 years exclusively on second PD catheters showed age to be the only factor significantly associated with reduced catheter survival (22). Other covariates like gender, primary renal disease, or PD catheter-related problems were not significantly associated with catheter survival (22). Our study, however, did not show any significant association between age and PD catheter survival. It is plausible that age may be a significant risk factor for the survival of subsequent catheters in PD patients who had their first catheters removed for various reasons.
Peritonitis has been demonstrated in many studies as a major cause of catheter and technique failure in PD patients, both for the present and future catheters (11, 23–26). A large study done on 473 CAPD patients revealed that peritonitis was the major cause of PD catheter removal (11). It was proposed that the formation of bio-film around the PD catheter is an obstacle to the continuation of PD. However, another group of researchers studied the effect of 579 peritonitis episodes on PD catheters and found that only 12% of the peritonitis episodes led to PD catheter removal (23). More importantly, the study showed that concomitant tunnel or exit-site infections and abdominal catastrophes were more likely to proceed to catheter loss. Other studies evaluated the effect of peritonitis on technique outcome and patient mortality (24, 25), and on peritonitis as a risk factor for future catheters (13, 26). Their results could not be used for comparison with our study due to different study objectives and methods. Our study shows that peritoneal infections are not significantly associated with PD catheter survival. The most plausible reason would be prompt and efficient treatment and care for the infectious episodes that might have minimized any adverse effect on the catheter outcome. Further studies are needed to assess the effect of peritoneal infections on PD catheter outcomes.
In summary, our study demonstrated 92.9% 1-year, 91.9% 2-year and 91.1% 3-year survival of PD catheters placed surgically at our institution. Only PD catheter-related non-infectious problems (intra-luminal/ extra-luminal obstruction, mal-positioning, migration, omental wrap, leakage and extrusion) were significantly associated with catheter failure. Other factors such as age, gender, race, BMI, diabetic status, comorbidities, previous abdominal surgeries, peritoneal infections or exit-site/ tunnel infections did not affect the PD catheter survival.
Based on our study results, we propose that age, obesity, previous abdominal surgeries, and co-morbidities should not be considered as barriers in selecting patients for peritoneal dialysis.
Acknowledgements
This study was supported by a grant from the George M. O’Brien Kidney Research Core Center NIH P30DK079328
References
- 1.Popovich RP, Moncrief JW, Nolph KD, Ghods AJ, Twardoski ZJ, Pyle WK. Continuous ambulatory peritoneal dialysis. Ann Intern Med. 1978;88:449–456. doi: 10.7326/0003-4819-88-4-449. [DOI] [PubMed] [Google Scholar]
- 2.Popovich RP, Moncrief JW. Kinetic modeling of peritoneal transport. Contrib Nephrol. 1979;17:59–72. doi: 10.1159/000402981. [DOI] [PubMed] [Google Scholar]
- 3.Fenton SS, Schaubel DE, Desmeules M, Morrison HI, Mao Y, Coplestone P, et al. Hemodialysis versus peritoneal dialysis: A comparison of adjusted mortality rates. Am J Kidney Dis. 1997;30:334–342. doi: 10.1016/s0272-6386(97)90276-6. [DOI] [PubMed] [Google Scholar]
- 4.Vonesh EF, Snyder JJ, Foley RN, Collins AJ. The differential impact of risk factors on mortality in hemodialysis and peritoneal dialysis. Kidney Int. 2004;66:2389–2401. doi: 10.1111/j.1523-1755.2004.66028.x. [DOI] [PubMed] [Google Scholar]
- 5.Merkus MP, Jager KJ, Dekker FW, Boeschoten EW, Stevens P, Krediet RT. Quality of life in patients on chronic dialysis: Self-assessment 3 months after the start of treatment. The Necosad Study group. Am J Kidney Dis. 1997;29:58–92. doi: 10.1016/s0272-6386(97)90342-5. [DOI] [PubMed] [Google Scholar]
- 6.Coles GA, Williams JD. What is the place of peritoneal dialysis in the integrated treatment of renal failure? Kidney Int. 1998;54:2234–2240. doi: 10.1046/j.1523-1755.1998.00183.x. [DOI] [PubMed] [Google Scholar]
- 7.Rubin HR, Fink NE, Plantinga LC, Sadler JH, Kliger AS, Powe NR. Patient ratings of dialysis care with peritoneal dialysis vs hemodialysis. JAMA. 2004;291:697–703. doi: 10.1001/jama.291.6.697. [DOI] [PubMed] [Google Scholar]
- 8.Saxena R. Peritoneal dialysis: A viable renal replacement therapy option. Am J Med Sci. 2005;330:36–47. doi: 10.1097/00000441-200507000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Viglino G, Cancarini G, Caltizone L, Cocchi R, de Vecchi A, Lupo A, et al. The impact of peritonitis on CAPD results. Adv Perit Dial. 1992;8:269–275. [PubMed] [Google Scholar]
- 10.Woodrow G, Turney JH, Brownjohn AM. Technique failure in peritoneal dialysis and its impact on patient survival. Perit Dial Int. 1997;17:360–364. [PubMed] [Google Scholar]
- 11.Nodaira Y, Ikeda N, Kobayashi K. Risk factors and cause of removal of peritoneal dialysis catheter in patients on continuous ambulatory peritoneal dialysis. Adv Perit Dial. 2008;24:65–68. [PubMed] [Google Scholar]
- 12.Cox SD, Walsh SB, Yaqoob MM, Fan SL. Predictors of survival and technique success after re-insertion of peritoneal dialysis catheter following severe peritonitis. Perit Dial Int. 2007;27(1):67–73. [PubMed] [Google Scholar]
- 13.Crabtree JH, Burchette RJ. Effect of prior abdominal surgery, peritonitis, and adhesions on catheter function and long-term outcome on peritoneal dialysis. Am Surg. 2009;75(2):140–147. doi: 10.1177/000313480907500206. [DOI] [PubMed] [Google Scholar]
- 14.Khanna R. Peritoneal dialysis access. In: Nolph KD 3rd, editor. Peritoneal dialysis. Kluwer Academie: Dordrecht; 1989. pp. 319–342. [Google Scholar]
- 15.Ash SR. Chronic peritoneal dialysis catheters: effects of catheter design, materials and location. Seminars in Dialysis. 1990;3:39–46. [Google Scholar]
- 16.Gadallah MF, Pervez A, el-Shahawy MA, Sorrells D, Zibari G, McDonald J, et al. Peritoneoscopic versus surgical placement of peritoneal dialysis catheters: a prospective randomized study on outcome. Am J Kidney Dis. 1999;33:118–122. doi: 10.1016/s0272-6386(99)70266-0. [DOI] [PubMed] [Google Scholar]
- 17.Apostolidis NS, Panoussopoulos DG, Manouras AJ, Pararas BN, Voudiklari SG, Zirogiannis PN. The use of TWH catheters in CAPD patients: fourteen-year experience in technique, survival, and complication rates. Perit Dial Int. 1998;18:424–428. [PubMed] [Google Scholar]
- 18.Ortiz AM, Fernandez MA, Troncoso PA, Guzman S, Del Campo F, Morales RA. Outcome of peritoneal dialysis: Tenckhoff catheter survival in a prospective study. Adv Perit Dial. 2004;20:145–149. [PubMed] [Google Scholar]
- 19.Garcia Falcon T, Rodriguez-Carmona A, Perez Fontan M, Fernandez Rivera C, Bouza P, Rodriguez Lozano I, et al. Complications of permanent catheter implantation for peritoneal dialysis: Incidence and risk factors. Adv Perit Dial. 2004;20:145–149. [PubMed] [Google Scholar]
- 20.McDonald SP, Collins JF, Johnson DW. Obesity is associated with worse peritoneal dialysis outcomes in the Australia and New Zealand patient populations. J Am Soc Nephrol. 2003;14(11):2894–2901. doi: 10.1097/01.asn.0000091587.55159.5f. [DOI] [PubMed] [Google Scholar]
- 21.Piraino B, Bernardini J, Centa PK, Johnston JR, Sorkin MI. The effect of body weight on CAPD related infections and catheter loss. Perit Dial Int. 1991;11(1):64–68. [PubMed] [Google Scholar]
- 22.Sahu KM, Walele A, Liakopoulos V, Bargman JM. Analysis of factors predicting survival of a second peritoneal dialysis catheter. Adv Perit Dial. 2003;19:252–254. [PubMed] [Google Scholar]
- 23.Yang CY, Chen TW, Lin YP. Determinants of catheter loss following continuous ambulatory peritoneal dialysis peritonitis. Perit Dial Int. 2008;28(4):361–370. [PubMed] [Google Scholar]
- 24.Moon SJ, Han SH, Kim DK, Lee JE, Kim BS, Kang SW, et al. Risk factors for adverse outcomes after peritonitis-related technique failure. Perit Dial Int. 2008;28(4):352–360. [PubMed] [Google Scholar]
- 25.Sipahioglu MH, Aybal A, Unal A, Tokgoz B, Oymak O, Utas C. Patient and technique survival and factors affecting mortality on peritoneal dialysis in Turkey: 12 years’ experience in a single center. Perit Dial Int. 2008;28(3):238–245. [PubMed] [Google Scholar]
- 26.Szeto CC, Chow KM, Wong TY, Leung CB, Wang AY, Lui SF, et al. Feasibilty of resuming peritoneal dialysis after severe peritonitis and Tenckhoff catheter removal. J Am Soc Nephrol. 2002;13:1040–1045. doi: 10.1681/ASN.V1341040. [DOI] [PubMed] [Google Scholar]