Abstract
Purpose
The purpose of this study was to assess the value of isocentric C-arm three-dimensional (Iso-C 3D) fluoroscopy for the insertion of an anterior odontoid screw. The results of the Iso-C 3D group were compared with that of an historic control group using conventional fluoroscopy.
Methods
Twenty-nine patients diagnosed with type II or rostral-type III odontoid fractures were treated with a single anterior screw fixation in this study. The Iso-C 3D group included 13 patients and the other 16 patients were in the historic control group. All operations were performed by a single surgeon using standard procedure and manner. The clinical and radiographic results were recorded and compared between the two groups.
Results
The fluoroscopy time in the Iso-C 3D group was 42.9 s as compared to 68.1 s in the control group (P < 0.01). The mean operative time was 91.5 min in the Iso-C 3D group when compared with 81.6 min in the control group (P = 0.20). The rate of bony fusion was 96.6% (28/29), the failure rate of reduction or fixation was 13.8% (7.7% in Iso-C 3D group; 18.8% in control group). The Smiley–Webster scale showed that 90% of patients achieved good or better outcomes
Conclusions
In conclusion, this technique can be safely extended to the treatment of technically difficult to treat spinal injuries and at the same time reduce total radiation exposure time both for the patient and the surgeon.
Keywords: Odontoid fracture, Anterior screw fixation, Isocentric C-arm fluoroscopy, Three-dimensional fluoroscopy
Introduction
Anterior screw fixation, first introduced by Bohler [1], has been widely used to treat type II and rostral-type III odontoid fractures [2]. Anterior screw fixation provides immediate immobilization and a higher fusion rate than non-operative treatment [3, 4]. It also preserves motion, especially axial rotation at the C1–2 junction, unlike posterior surgical fixation which leads to loss of at least 50% of cervical rotation [3, 5].
Recently cannulated screw techniques have been introduced and have aided screw placement [6]. A guide wire for the cannulated screws is drilled into the odontoid process under intraoperative fluoroscopic control during an operation. When using conventional intraoperative fluoroscopy, only a single two-dimensional (2D) image plane is visualized at one time. At least two image planes, typically anteroposterior (AP) and lateral are required to allow accurate placement of the guide wire. This leads to repeat using of the conventional C-arm intraoperatively, resulting in a high radiation exposure for both patients and surgical teams [7, 8]. Despite the use of the fluoroscopic imaging, there remains a risk of screw misplacement [3].
The disadvantages of the conventional fluoroscopy may be solved by fluoroscopy-based computer-assisted surgery (CAS). The recent introduction of Iso-C 3D fluoroscopy (Siemens Medical Solutions, Erlangen, Germany) has been shown to enhance the safety and efficacy of pedicle screw placement and reduce intraoperative radiation doses in spine surgery [9, 10]. This navigational system acquires images automatically. Reformatted axial, coronal and sagittal images are automatically registered and transferred to a Stealth-Station Treatment Guidance Platform System (Medtronic, Sofamor Danek, Broomfield, CO, USA) to plan the optimal screw trajectory. Summers et al. [11] successfully applied the Iso-C 3D fluoroscopy to place anterior odontoid screws in nine patients. Their study showed a reduction in intraoperative registration time and immediate computed tomography (CT) imaging to verify screw position in the operating room.
The purpose of this study was to assess the value of Iso-C 3D fluoroscopy for insertion of odontoid screws in a clinical institution. The results of the Iso-C 3D fluoroscopy group were compared with that of a conventional C-arm fluoroscopy group. The aim was to compare total operative time, fluoroscopy time, operative complications and fusion rate in the two groups.
Materials and methods
Twenty-nine patients ranging in age from 14 to 59 years were included in this retrospective study from March 2003 to September 2009. Demographic data of the patients and clinical characteristics of their injuries are presented in Table 1. Fractures were defined through plain radiographs according to the Anderson-D’Alonzo classification [2]. The study comprised 24 patients with type II and 5 patients with type III fractures.
Table 1.
Summary of patient data
| Characteristics | Group A | Group B |
|---|---|---|
| (C-arm) | (Iso-C 3D) | |
| Number of cases | 16 | 9/4 |
| Gender (male/female) | 11/5 | 9/4 |
| Mean age, years (range) | 33.6 (14–58) | 36.7 (23–59) |
| Standard deviation (SD) | 12.5 | 10.9 |
| 95% Confidence interval (years) | 27.0–40.3 | 30.1–43.2 |
| Mechanism of injury | ||
| Motor vehicle accident | 11 | 10 |
| Fall | 4 | 3 |
| Other | 1 | |
| Fracture type (Anderson-D’Alonzo) | ||
| Type II | 13 | 11 |
| Type III | 3 | 2 |
| Fracture displacement | ||
| No/slight displacement | 7 | 7 |
| Displacement >2 mm | 9 | 6 |
| Associated injuries | ||
| Yes | 5 | 4 |
| No | 11 | 9 |
| Neurologic deficits | ||
| Yes | 3 | 2 |
| No | 13 | 11 |
| Presentation | ||
| Neck pain | 16 | 13 |
| Upper extremity numbness | 3 | 2 |
| Neck tenderness | 14 | 12 |
All patients were acute trauma cases and underwent radiologic evaluation via plain spine radiographs (lateral and open-mouth views) and cervical spine CT scans. Patients with neurological deficits also had magnetic resonance imaging (MRI) scans, while patients with no neural deficit only underwent MRI scans if the X-ray showed evidence of fracture instability [12].
The time interval between the traumatic event and the patient presenting at casualty was between 4 h and 10 days (mean = 4.6 days). Operations were performed on an average of 3 days after admission. The average duration of hospitalization was 10 ± 0.6 days. The operations were performed by a senior spinal surgeon using a standard procedure.
According to the institution’s treatment protocol, one anterior screw was normally inserted in young patients with type II or rostral-type III reducible odontoid fractures, whereas, conservative treatment was adopted for older patients (>60 years). In older patients, bone quality is poorer rendering fluoroscopic imaging difficult. Positioning may also be problematic in older patients due to the loss of spinal extension limiting access to the upper cervical spine. Contraindications for the use of an anterior screw were a disruption of the atlantal transverse ligament, patients with a short neck and/or barrel chest, odontoid fractures associated with comminution of one or both atlantoaxial joints, a fracture line in the sagittal plane [3, 13], and pathologic fractures [14]. Patients who declined to undergo surgery or could not tolerate the surgical treatment because of pre-existing systemic diseases were also excluded.
Patients were divided into two groups: Group A (control group) consisted of 16 patients who underwent anterior screw fixation under conventional C-arm fluoroscopy from March 2003 to September 2006. Group B (Iso-C 3D fluoroscopy group) consisted of 13 patients in whom anterior screws were placed with the Iso-C 3D fluoroscopy from October 2006 to September 2009.
Surgical technique
All patients underwent reduction of fracture malalignment using skull traction, and serial cervical lateral radiographs were taken to confirm an anatomic or near-anatomic reduction of the fracture. After general endotracheal anesthesia was induced, the patient was positioned supine on a carbon fiber radiolucent operating tabletop (Hobo, China) with skull traction, and a folded blanket was placed under the shoulders to allow for neck extension.
Anterior screw instrumentation with conventional C-arm fluoroscopy (BV25 GOLD, Philips, The Netherlands)
A standard approach to the anterior cervical spine was performed, with a unilateral horizontal incision placed at approximately the C5–6 level. The interval between the carotid sheath laterally and the trachea and esophagus medially was opened with a blunt dissection, and the prevertebra fascia with a combination of blunt and sharp dissection up to the level of C2–3. The entry point for the screw was at the anterior aspect of the inferior endplate of C2, so that a small amount of the C2–3 disc was removed to create a recess. One conventional C-arm fluoroscopy was used, and with open-mouth and lateral fluoroscopic guidance, the guide wire was inserted from the anterior-inferior margin of the C2 body to the posterior odontoid process. The correct angle of the screw is nearly in line with the cervical spine and therefore adequate clearance of the sternum is needed. One 4.0-mm cannulated screw (Synthes, West Chester, PA, USA) was inserted under imaging control until it reached the posterior cortex of the odontoid process, avoiding proximal migration of the guide wire to prevent spinal cord injury [15].
Anterior screw instrumentation with Iso-C 3D fluoroscopy
The image guidance dynamic reference array was secured tightly to the radiolucent head frame and placed on C5–6 vertebrae for registration. The isocentric C-arm was positioned so that the C2 vertebra was in the center of the AP and lateral views. The C2 vertebra was screened using isocentric C-arm and the acquired images were transferred to the Stealth-Station Treatment Guidance Platform System. During the image acquisition, the motorized C-arm moved continuously around 190°, and then 100 fluoroprojection images were acquired at equidistant angles. Accurate coronal, transverse and sagittal images of the C2 vertebra were produced. The accuracy of the image was checked using a tool navigator. The tool navigator was used along with 3D fluoroscopic real-time images (Fig. 1) to determine the entry point and direction of the screw. A guide wire was then calibrated to the navigation system so that the real-time navigation images could be obtained during the drilling of the bones. The drilling was performed in stages, taking care to verify and check the accuracy of the trajectory frequently using the calibrated tool (Fig. 2). The computer measured the length of the screw after the guide wire application. The position of the guide wire was validated with isocentric C-arm in different views. One 4.0-mm cannulated screw was placed cautiously. The accuracy of the placement of the screw was again verified by acquiring coronal and sagittal images using Iso-C 3D fluoroscopy.
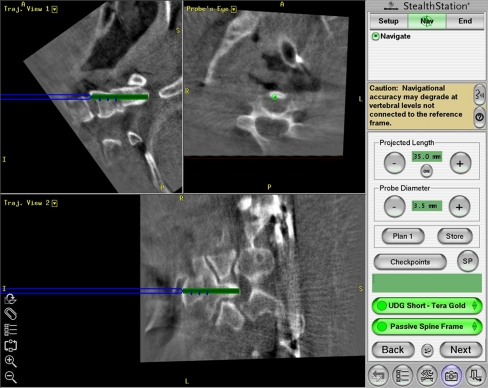
Fig. 1.
Reconstructed multiplanar images obtained by the isocentric C-arm and used for imaged-guided navigation during odontoid screw placement in the sagittal trajectory, coronal probe’s eye, and axial trajectory planes. The blue line is used to prepare the pilot holes for odontoid screw
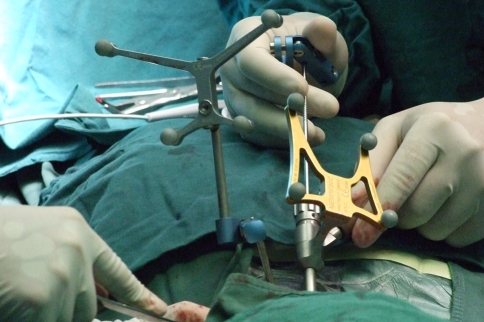
Fig. 2.
During drilling of the odontoid process, a calibrated tool navigator was used to determine the accuracy of the trajectory along with 3D fluoroscopic real-time images
The set-up time of Iso-C 3D fluoroscopy, intraoperative fluoroscopy time and total operative time were recorded. The operative time was defined from the skin incision for the anterior internal fixation at the C5–6 level to incision closure. Postoperatively, the patients were followed up for operation-related complications. Radiographs and CT scans of the cervical spines were performed postoperatively to reassess the position of the screw (Fig. 3). Each patient was placed with a cervical collar for 4 weeks.
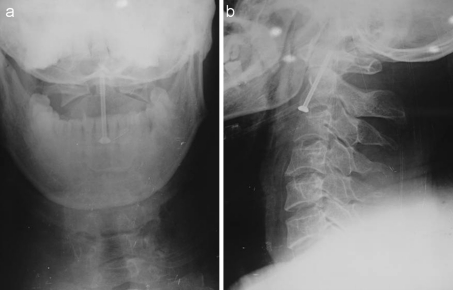
Fig. 3.
Postoperative open-mouth (a) and lateral (b) cervical spine radiographs after a single cannulated screw placement
All patients were reviewed at 6 weeks, 3 months, 6 months and 1 year after surgery. After 1 year, the outcomes were verified by radiological and physical examination every 6 months. Radiographic assessment consisted of lateral and open-mouth views of cervical spine plain films. Flexion–extension views were performed at 3 and 6 months after surgery. The images of CT scans were obtained at 6 months after surgery or if the fusion of the fractures could not be determined on the conventional radiographs. Union of the fractured odontoid was defined as the presence of bony trabeculation and existence of bony bridges [16].
For clinical evaluation, the patient’s functional outcome was assessed using the Smiley–Webster scale (Table 2) [17]. The range of motion was determined by evaluation of flexion–extension, lateral inclination and rotation of the cervical spine using a goniometer at the last follow-up.
Table 2.
Smiley–Webster scale used to assess functional results
| Scale | Description |
|---|---|
| I: Excellent | Patient returned to full-time work/activity as before onset of symptoms; no pain medication required |
| II: Good | Patient returned to full-time work/activity; occasional consumption of pain medication |
| III: Fair | Patient not able to return to former level of work/activity; occasionally pain medication; improved over |
| IV: Poor | Patient not able to return to work/former activity level; regular consumption of pain medication |
Statistical analysis
All results were evaluated with SPSS 13.0 for Windows (SPSS, Inc., Chicago, IL, USA). Differences in preoperative variables, such as fracture types, operative complications, as well as clinical and radiographic results, were compared and evaluated with the Fisher’s exact test. The distribution of the patient sample in each group was assessed by Minitab 15 (Minitab Inc., PA, USA). A Student t test was performed to test the hypothesis of no difference in fluoroscopy time and operative time. Statistical significance was defined as P < 0.05.
Results
The average age in Group A was 34 years ranging from 14 to 58 years with a male/female ratio of 2.2:1 (Table 1). Group B had an average age of 37 ranging from 23 to 59 years with a similar male/female ratio to Group A. Minitab 15 was used to assess the distribution of the two groups, which indicated a normal distribution in both groups. There was no significant difference in terms of age and gender composition (P = 0.58 and P = 1.00, respectively). Significant associated injuries were noted in 9 patients, whereas isolated injuries of the odontoid process were observed in 20 patients (Table 3). In Group A, five patients had associated injuries, including two patients with fractures of ulna and ribs, two patients with head and thoracic injuries, and 1 patient with traumatic deafness of right ear. In Group B, associated injuries were recorded in four patients, including one patient with scapular and lower leg fractures, and three patients with fractures of lumbar vertebrae, fibula, clavicle and femur.
Table 3.
Associated injuries in two study groups
| Associated injuries | Group A (C-arm) | Group B (Iso-C 3D) |
|---|---|---|
| Head injury | 1 | |
| Thoracic injury | 1 | |
| Traumatic deafness | 1 | |
| Fractures | ||
| Scapula and left leg | 1 | |
| Clavicle and femur | 1 | |
| Ulna | 1 | |
| L2 lumber | 1 | |
| Fibula | 1 | |
| Ribs | 1 | |
Preoperatively, five patients had neurologic deficits related to the odontoid fractures. Sensory deficits were found in three patients, motor deficit in one patient, and motor and sensory deficits in one patient. None of the patients had a complete tetraplegia. The incidence of neurologic impairment was similar between the two study groups (Group A: 3; Group B: 2). After surgery, sensory deficit resolved incompletely in one patient. All other patients with neurologic deficits recovered completely.
The fluoroscopy time in Group A was 68.1 s as compared to 42.9 s in Group B (P < 0.01). The mean operative time in Group A was 81.6 min; 91.5 min in Group B (P = 0.18). The mean blood loss in Group A was 93.8 ml (50–250 ml) and 92.3 ml (50–200 ml) in Group B (P = 0.95) (Table 4).
Table 4.
Operative records of patients in the two groups
| Operative records | Group A | Group B | P value |
|---|---|---|---|
| (C-arm) | (Iso-C 3D) | ||
| Operative time (min) | 81.6 ± 5.0 | 91.5 ± 5.7 | n.s. |
| Fluoroscopy time (s) | 68.1 ± 8.0 | 42.9 ± 0.3 | 0.0085 |
| Blood loss (ml) | 93.8 ± 15.7 | 92.3 ± 13.7 | n.s. |
| Operative complications | |||
| Yes | 2 | 1 | n.s. |
| No | 14 | 12 | |
n.s. no significant difference
The total time spent for the navigated procedure was 660 s on average (range 450–1,400 s). The average time for the preparation of the Iso-C 3D and placement of the reference array was 390 s (range 250–1,000 s). The average time of acquiring images and calculation of the system after scanning was 210 s (range 160–270 s). Panning of the trajectory took an average of 60 s (range 40–130 s).
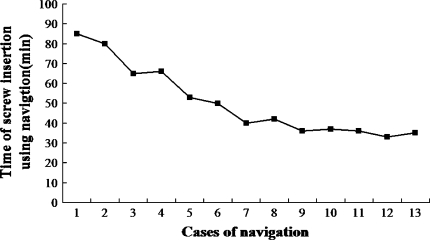
The time of screw insertion using Iso-C 3D fluoroscopy was recorded, and the learning curve was plotted (Fig. 4). In the initial cases, it took approximately 85 min. The time was decreased significantly in the subsequent cases. Mean time of screw insertion was approximately 36 min after eight cases.
Fig. 4.
Learning curve of navigation system
In Group B, one patient had transient superior laryngeal nerve paralysis after surgery, but recovered completely without intervention. Two patients developed a complication in Group A. One patient had a superficial wound infection after surgery, which was treated with a course of intravenous antibiotics without instrumentation removal. The other patient had a postoperative hematoma, which was allowed to resolve without surgery. The Fisher’s exact test showed no difference in complication rate between the two groups (P = 1.00). One patient in Group A had lower cervical spine degenerative disease, for which the patient underwent C6–7 level anterior cervical discectomy and fusion.
The period of follow-up varied from 6 to 30 months (mean 13.5 months). Solid bony fusion was radiographically evident in 28 patients (96.6%), and was achieved within an average 5.4 months (from 3 to 12 months). In one patient in Group A, non-union was diagnosed by standard radioscopy and CT scans at 12 months after surgery. No motion was seen in the dynamic radiographs in this patient, and fibrous pseudarthrosis was established at the fracture site. Based on the clinical and radiographic findings, no further surgical intervention was required.
Failures of reduction and fixation were noted in four patients. In the first patient, the fractured odontoid was not reduced with a gap of 1 mm (non-union). In the second patient, the screw did not reach the apical cortical surface of the odontoid process, but crossed the fracture line. In the third patient, odontoid fragment was left in slight posterior displacement (2 mm). A posterior angular deformity was observed in the last patient (Group B). In these four cases, the fractures had healed in three patients and not healed in one patient. When comparing the two groups, there was a failure rate of 7.7% (1/13) in Group B and 18.8% (3/16) in Group A (P = 0.60) (Table 4).
Clinical outcome
In this series, 26 (90%) patients had returned to their pre-injury activity level at the end of follow-up. Three patients complained about a decrease in cervical spine motion. Two patients had approximately a 25% limitation on range of motion and one had more than 25% limited range of motion in the cervical spine. The Smiley–Webster scale was used to quantify the clinical outcome of the patients. In Group B, nine patients achieved clinically excellent outcomes, three good and one fair. In Group A, excellent outcomes were achieved in nine patients, good in five patients and fair in two patients.
Discussion
Anterior screw fixation of odontoid fracture has become a successful and widely accomplished treatment option in cervical spine surgery since its introduction [1, 3, 5, 15, 18, 19]. This approach can provide immediate stabilization, restore the normal C1–2 joint, and preserve motion, especially rotatory motion. It has been reported that anterior screw fixation of odontoid fractures achieves high rates of bony fusion with only a few complications, especially in younger patients (<60 years). Likewise, patients have achieved a good recovery of cervical spine function [3, 5, 18, 19]. In this study, we had an overall fusion rate of 96.5% in all patients studied. There was no difference in union rates comparing the two methods of surgery. At the end of follow-up, 26 patients (90%) had returned to their pre-injury activity level, and achieved clinically excellent or good outcomes in total according to the Smiley–Webster scale.
Screw placement can be technically challenging, particularly to surgeon without extensive surgical experience. Traditionally, conventional C-arm fluoroscopy is used to place the guide wire and cannulated screw. Sometimes, it is difficult to check the inserted screw or guide wire via the open-mouth view in patients during an operation. There is also increasing concern about exposure to radiation of operating teams and patients with extensive use of intraoperative fluoroscopy.
The Iso-C 3D fluoroscopy has been applied to many orthopedic surgical operations, such as spinal procedures, foot and ankle surgeries. This system can collect coronal, sagittal and axial images and upload them to a workstation to reconstruct 3D images for use during surgery. It can also provide additional useful information that cannot be obtained from plain films or C-arm fluoroscopy alone [20]. During operation, the Iso-C 3D simultaneously provided real-time monitor and a three-dimensional mapping of the fractured odontoid process. Therefore, it could allow surgeons to determine the insertion of the guide wire and cannulated screw easily and precisely.
Iso-C 3D fluoroscopy has been reported to significantly increase the accuracy of screw placement in spinal surgeries [9, 21]. Rajasekaran et al. [9] found that the rate of pedicle breaches was 23% in the non-navigation group when compared with 2% in the navigation (Iso-C 3D) group in thoracic deformity corrections. Nakashima reported that the frequency of screw misplacement using Iso-C 3D fluoroscopy-based image-guide assistance was significantly lower than using fluoroscopy in percutaneous posterior lumbar pedicle screws placement [21]. Anterior screw fixation using Iso-C 3D fluoroscopy was successfully placed in nine patients diagnosed with odontoid fractures in Summer’s study [11].
In this study, there was no significant difference in the failure rate of reduction and fixation for odontoid fractures between the two groups, which indicated that Iso-C 3D fluoroscopy was in our experience at least equivalent to using conventional C-arm fluoroscopy in the treatment of these injuries.
During conventional C-arm fluoroscopy screening, the surgeons need to be in the operating field, thus increasing the radiation exposure. In this study, the operative team was not in the operating room during Iso-C 3D C-arm automatic screening. This shortened the radiation exposure time for the surgical team and provided a safer operating procedure compared with the conventional C-arm fluoroscopy in odontoid screw placement. Previous studies have showed that the radiation doses from Iso-C 3D are significantly less than conventional C-arm fluoroscopy in different spinal surgeries [10, 22, 23]. For design reasons, this retrospective study only detected total radiation time. This is not an exact measure of the total radiation dose. However, it is proportional to the total radiation dose and as such is a suitable surrogate measure.
The use of intraoperative Iso-C 3D fluoroscopy may slightly extend operative time [24]. When compared with conventional fluoroscopy, it costs additional initial time to set-up the Iso-C 3D system before starting the operation. However, in Summer’s study, it was found that this system could reduce intraoperative registration time, and not add to the operative time [11]. Our set-up time of Iso-C 3D fluoroscopy averaged 660 s, but the total operative time was not significantly different between the two groups. The navigation system is relatively complex and the learning curve is significant. Time must be taken in this learning curve to ensure that all steps are completed and to ensure that patient safety is not compromised. Our series includes our learning curve as demonstrated in Fig. 4. With the initial cases, we spent more time inserting the odontoid screw with the navigation system than we did in the conventional fluoroscopy. After we gained experience with the navigation system (after about 8 cases), the time to insert the screw using Iso-C 3D was significantly shortened. Our learning curve was similar to other studies on the computer-assisted navigation system [25].
The rate of postoperative complications was not significantly different between the two groups. In Group B, one patient had a transient superior laryngeal nerve paralysis after operation, but recovered spontaneously 2 days later. Excessive traction, accidental ligation, or postoperative swelling may damage this nerve [26]. In Group A, a superficial wound infection was found in one patient after surgery.
One potential disadvantage of the Iso-C 3D fluoroscopy was that the collected images may not match the patient’s anatomic structures of the surgical site if there was loosening the image guidance dynamic reference array during surgery [27]. In such a situation, the surgeon would follow an incorrect trajectory provided by the Iso-C 3D system to place the guide wire and the cannulated screw. In our Iso-C 3D group, there was no loosening the image guidance dynamic reference array reported during operation and screw placement was successful.
The average hospital cost of patients with isolated odontoid fracture in Group B was greater than the cost of patients in Group A. Using Iso-C 3D fluoroscopy may be a burden on patients.
This study has some limitations: first, as this study was a retrospective study, patients were not randomly recruited to each group as this could only be done in a prospective study. Despite the lack of randomization, the two study groups were well matched. Second, the patients included in this study were under 60 years of age. Odontoid fractures in elderly patients are technically more difficult to treat operatively than in young patients. In this study, the patient’s age, gender and fracture type in the two groups were not significantly different. Following on from this study, further research on the use of Iso-C 3D fluoroscopy in elderly patients with odontoid fractures would be valuable. In a retrospective study, it is difficult to avoid selection bias. Our historic design, we believe is reflective of real-world practice, where units will adopt new technologies. In our series, there was no difference in successful placement of screws. The contraindications of this operation apply to both techniques. These include those patients who could not undergo anterior screw fixation of the odontoid fractures because of fracture morphology, fracture type (type I and some type III), patient’s body habitus (short neck or/and barrel chest), and pathological fractures.
Conclusions
This study demonstrated encouraging clinical and radiographic outcomes using anterior screw fixation for type II and rostral-type III odontoid fractures, both in the Iso-C 3D and the conventional C-arm fluoroscopy groups. When comparing the two fluoroscopy techniques, there were similar results in terms of accuracy of odontoid screw placement and clinical outcomes. The value and relevance of this study is that it demonstrates that the technique can be safely extended to the treatment of technically difficult to treat spinal injuries and at the same time reduce total radiation exposure time both for the patient and the surgeon.
Conflict of interest
None.
References
- 1.Bohler J. Screw-osteosynthesis of fractures of the dens axis (author’s transl) Unfallheilkunde. 1981;84:221–223. [PubMed] [Google Scholar]
- 2.Anderson LD, D’Alonzo RT (2004) Fractures of the odontoid process of the axis. J Bone Joint Surg Am 86-A:2081 [PubMed]
- 3.Subach BR, Morone MA, Haid RW Jr, McLaughlin MR, Rodts GR, Comey CH (1999) Management of acute odontoid fractures with single-screw anterior fixation. Neurosurgery 45:812–819 (discussion 9–20) [DOI] [PubMed]
- 4.Nourbakhsh A, Shi R, Vannemreddy P, Nanda A. Operative versus nonoperative management of acute odontoid type II fractures: a meta-analysis. J Neurosurg Spine. 2009;11:651–658. doi: 10.3171/2009.7.SPINE0991. [DOI] [PubMed] [Google Scholar]
- 5.Fountas KN, Kapsalaki EZ, Karampelas I, Feltes CH, Dimopoulos VG, Machinis TG, Nikolakakos LG, Boev AN, 3rd, Choudhri H, Smisson HF, Robinson JS (2005) Results of long-term follow-up in patients undergoing anterior screw fixation for type II and rostral type III odontoid fractures. Spine (Phila Pa 1976) 30:661–669 [DOI] [PubMed]
- 6.Borm W, Konig RW, Albrecht A, Richter HP, Kast E. Percutaneous transarticular atlantoaxial screw fixation using a cannulated screw system and image guidance. Minim Invasive Neurosurg. 2004;47:111–114. doi: 10.1055/s-2004-818449. [DOI] [PubMed] [Google Scholar]
- 7.Sanders R, Koval KJ, DiPasquale T, Schmelling G, Stenzler S, Ross E. Exposure of the orthopaedic surgeon to radiation. J Bone Joint Surg Am. 1993;75:326–330. doi: 10.2106/00004623-199303000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Rampersaud YR, Foley KT, Shen AC, Williams S, Solomito M (2000) Radiation exposure to the spine surgeon during fluoroscopically assisted pedicle screw insertion. Spine (Phila Pa 1976) 25:2637–2645 [DOI] [PubMed]
- 9.Rajasekaran S, Vidyadhara S, Ramesh P, Shetty AP (2007) Randomized clinical study to compare the accuracy of navigated and non-navigated thoracic pedicle screws in deformity correction surgeries. Spine (Phila Pa 1976) 32: E56–E64 [DOI] [PubMed]
- 10.Gebhard FT, Kraus MD, Schneider E, Liener UC, Kinzl L, Arand M (2006) Does computer-assisted spine surgery reduce intraoperative radiation doses? Spine (Phila Pa 1976) 31:2024–2027 (discussion 8) [DOI] [PubMed]
- 11.Summers LE, Kouri JG, Yang M, Patrick Jacob R. Odontoid screw placement using isocentric 3-dimensional C-arm fluoroscopy. J Spinal Disord Tech. 2008;21:45–48. doi: 10.1097/BSD.0b013e31805777da. [DOI] [PubMed] [Google Scholar]
- 12.Shetty A, Kini AR, Prabhu J. Odontoid fractures: a retrospective analysis of 53 cases. Indian J Orthop. 2009;43:352–360. doi: 10.4103/0019-5413.55975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aebi M, Etter C, Coscia M (1989) Fractures of the odontoid process. Treatment with anterior screw fixation. Spine (Phila Pa 1976) 14:1065–70 [DOI] [PubMed]
- 14.Martin GJ Jr, Haid RW Jr, MacMillan M, Rodts GE Jr, Berkman R (1999) Anterior cervical discectomy with freeze-dried fibula allograft. Overview of 317 cases and literature review. Spine (Phila Pa 1976) 24:852–858 (discussion 8–9) [DOI] [PubMed]
- 15.Song KJ, Lee KB, Kim KN. Treatment of odontoid fractures with single anterior screw fixation. J Clin Neurosci. 2007;14:824–830. doi: 10.1016/j.jocn.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 16.Tuli SK, Chen P, Eichler ME, Woodard EJ (2004) Reliability of radiologic assessment of fusion: cervical fibular allograft model. Spine (Phila Pa 1976) 29:856–860 [DOI] [PubMed]
- 17.Webster FS, Smiley DP. End result study of a series of operations for herniated intervertebral lumbar discs. Am J Surg. 1960;99:27–32. doi: 10.1016/0002-9610(60)90244-0. [DOI] [PubMed] [Google Scholar]
- 18.Julien TD, Frankel B, Traynelis VC, Ryken TC. Evidence-based analysis of odontoid fracture management. Neurosurg Focus. 2000;8:e1. doi: 10.3171/foc.2000.8.6.2. [DOI] [PubMed] [Google Scholar]
- 19.Muller EJ, Wick M, Russe O, Muhr G. Management of odontoid fractures in the elderly. Eur Spine J. 1999;8:360–365. doi: 10.1007/s005860050188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Richter M, Geerling J, Zech S, Goesling T, Krettek C. Intraoperative three-dimensional imaging with a motorized mobile C-arm (SIREMOBIL ISO-C-3D) in foot and ankle trauma care: a preliminary report. J Orthop Trauma. 2005;19:259–266. doi: 10.1097/01.bot.0000151822.10254.db. [DOI] [PubMed] [Google Scholar]
- 21.Nakashima H, Sato K, Ando T, Inoh H, Nakamura H. Comparison of the percutaneous screw placement precision of isocentric C-arm 3-dimensional fluoroscopy-navigated pedicle screw implantation and conventional fluoroscopy method with minimally invasive surgery. J Spinal Disord Tech. 2009;22:468–472. doi: 10.1097/BSD.0b013e31819877c8. [DOI] [PubMed] [Google Scholar]
- 22.Zwingmann J, Konrad G, Kotter E, Sudkamp NP, Oberst M. Computer-navigated iliosacral screw insertion reduces malposition rate and radiation exposure. Clin Orthop Relat Res. 2009;467:1833–1838. doi: 10.1007/s11999-008-0632-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smith HE, Welsch MD, Sasso RC, Vaccaro AR. Comparison of radiation exposure in lumbar pedicle screw placement with fluoroscopy vs computer-assisted image guidance with intraoperative three-dimensional imaging. J Spinal Cord Med. 2008;31:532–537. doi: 10.1080/10790268.2008.11753648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Citak M, Kendoff D, Kfuri M, Jr, Pearle A, Krettek C, Hufner T. Accuracy analysis of Iso-C3D versus fluoroscopy-based navigated retrograde drilling of osteochondral lesions: a pilot study. J Bone Joint Surg Br. 2007;89:323–326. doi: 10.1302/0301-620X.89B3.18424. [DOI] [PubMed] [Google Scholar]
- 25.Luo CF, Zhou KH, Gao H, Hu CF, Chen J, Zeng BF. Minimally invasive surgery of pelvic-acetabular fractures with fluoro-navigation. Zhonghua Yi Xue Za Zhi. 2007;87:3030–3034. [PubMed] [Google Scholar]
- 26.Melamed H, Harris MB, Awasthi D (2002) Anatomic considerations of superior laryngeal nerve during anterior cervical spine procedures. Spine (Phila Pa 1976) 27:E83–E86 [DOI] [PubMed]
- 27.Atesok K, Finkelstein J, Khoury A, Peyser A, Weil Y, Liebergall M, Mosheiff R. The use of intraoperative three-dimensional imaging (ISO-C-3D) in fixation of intraarticular fractures. Injury. 2007;38:1163–1169. doi: 10.1016/j.injury.2007.06.014. [DOI] [PubMed] [Google Scholar]