Abstract
Introduction
Patients with os odontoideum always present instability in atlantoaxial joint and need atlantoaxial fixation. C2 pedicle or laminar screws fixation has proven to be efficient and reliable for atlantoaxial instability. However, os odontoideum is a congenital or developmental disease, featured with anomalous bony anatomies. The anatomic measurements and guidelines for C2 pedicle screw placement in general population tends to differ with those of os odontoideum patients, for whom C2 pedicle screws are often needed. The option and techniques of C2 fixation are still challenging and yet to be fully explored.
Material and methods
We recruited 29 adult patients with os odontoideum and measured the dimension of C2 pedicle and lamina for each patient to examine how well do they match with the screws anatomically. In order to access the intra-observer reliability and inter-observer repeatability of the measurements, the intraclass correlation coefficient (ICC) was also calculated.
Results
The results for reliability of the CT measurements showed excellent intraobserver (ICC = 0.95 and 0.96) and interobserver correlation coefficient (ICC = 0.93). The diameter and length of C2 pedicle were found to be 6.06 ± 1.37 and 24.05 ± 2.54 mm, while the corresponding figures of C2 laminar were 6.95 ± 0.82 and 25.60 ± 2.18 mm, respectively. In the measurements, all 29 cases had suitable diameter (larger than 5.5 mm) for C2 laminar screw (the laminar diameters ranged from 5.52 to 8.82 mm). In C2 pedicle measurements, the diameters of the 29 cases were from 3.50 to 9.86 mm, while 20 pedicles (34.5%) in 14 cases were less than 5.5 mm in diameter. Six had bilateral small pedicles where the diameter was less than 5.5 mm.
Conclusion
Anatomically, we found laminar screw is a better match in comparison with pedicle screw for C2 fixation in os odontoideum. The options for C2 fixation should be made based on careful preoperative imaging and thorough consideration. Preoperative reconstructive CT scan can offer great assistance for the choice of fixation in os odontoideum by revealing the anatomy of the C2 pedicles in detail.
Keywords: Os odontoideum pedicle screw, Laminar screw, C2 fixation
Introduction
Os odontoideum (OO) was defined as an ossicle with smooth cortical margins representing the odontoid process that has no osseous continuity with the body of C2 [29]. The etiology was unclear although often described as acquired (developmental) [9, 13] or congenitally originated [1, 8, 23, 33]. In pediatric patients OO is often seen in cases of Down syndrome and other congenital diseases such as opsismodysplasia and Kniset syndrome [1]. However, it has been widely noticed that OO patients always present with atlantoaxial instability that needs fixation [2, 5, 22]. Magerl [17] first described the transarticular screws for atlantoaxial fixation with traditional posterior wiring and bone grafting. It has since been widely used for C1–C2 posterior arthrodesis, yielding a high fusion rates as high as 100% [12, 30]. However, this technique is associated with the risk of VA injury. The risk could further increase due to anatomical discrepancies, which subsequently hence precluded the use of such screws in up to 26% of patients [20, 27, 28]. Nevertheless, C1 lateral mass and C2 pedicle screws fixation have been successfully used for the treatment of atlantoaxial instability in a few studies [6, 11, 14, 15, 21, 31, 35]. More recently, the anatomic suitability and guidelines for transarticular, C1 and C2 pedicle screw placement in the general adult population was established by Resnick et al. [27]. However, OO is a congenital or developmental disease, with the possibility of anomalous bony anatomies. The data from general population may not apply to patients with OO. In addition, the use of C2 laminar screws in atlantoaxial fixation in attempt to reduce the risk for the vertebral artery (VA), was first reported by Wright et al. [36] in 2004 and since became popular [18, 19, 38]. For OO patients, however, a couple of questions arise: can C2 pedicle screw be safely placed in every OO patient? Anatomically speaking, which technique is better for C2 fixation anatomically? From 2004 to 2010, we recruited 29 cases with os odontoideum and measured the C2 pedicles and lamina using constructive CT. To the best of our knowledge, few previous reports have specially focused on the anatomic suitability for C2 pedicle and laminar screw placement in os odontoideum patients.
Materials and methods
A total of 29 patients with Os odontoideum (OO) were recruited consecutively in our center from 2004 to 2010 (showed in Table 1; Fig. 1). The medical history was reviewed to reveal any history of cervical trauma at the time when os odontoideum was first noticed. Twelve cases were previously diagnosed as os odontoideum (from 3 months to 15 years, averaged 2.5 years) before they were recruited in our study. Among them, only five had remote history of cervical trauma (>1 year before presentation). All five cases were associated with low energy trauma. All cases of acute odontoid fracture with sharp edges of the separation and absence of cortical sclerosis on the margins shown in the X-ray were excluded. Feilding’s criteria [9] was used to differentiate os odontoideum from non-union of odontoid fracture, where the fractured odontoid tends to retains its original size and shape, and the separation is narrower [9]. In addition, patients who were under 18 years of age or had other congenital deformities, i.e. opsismodysplasia, Down syndrome and Kniset syndrome were excluded from the present study in order to reduce undesired inference.
Table 1.
Measurements in all 29 patients
| No | Sex | Age | C2 pedicles (mm) | C2 lamina (mm) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Diameter (L) | Diameter (R) | Length (L) | Length (R) | Diameter (L) | Diameter (R) | Length (L) | Length (R) | |||
| 1 | M | 39 | 7.62 | 6.56 | 25.86 | 29.22 | 8.69 | 8.82 | 26.81 | 27.82 |
| 2 | M | 52 | 6.17 | 5.03a | 22.54 | 24.56 | 7.37 | 8.47 | 27.80 | 29.50 |
| 3 | M | 31 | 8.03 | 6.39 | 25.58 | 26.53 | 8.31 | 7.21 | 29.20 | 28.35 |
| 4 | M | 50 | 5.78 | 5.39a | 21.05 | 22.15 | 8.36 | 8.73 | 26.02 | 28.30 |
| 5 | F | 43 | 4.67a | 5.60 | 23.42 | 24.94 | 6.03 | 6.46 | 24.23 | 26.38 |
| 6 | M | 50 | 7.63 | 7.48 | 20.85 | 20.93 | 6.79 | 7.10 | 26.80 | 27.56 |
| 7 | M | 51 | 7.04 | 6.24 | 23.33 | 22.08 | 5.52 | 6.63 | 22.09 | 24.36 |
| 8 | M | 48 | 6.70 | 6.50 | 18.93 | 19.50 | 6.79 | 6.87 | 24.36 | 28.89 |
| 9 | F | 44 | 4.85a | 4.93a | 19.93 | 21.12 | 6.09 | 6.46 | 23.68 | 24.38 |
| 10 | M | 42 | 6.00 | 6.94 | 23.86 | 23.73 | 6.05 | 6.20 | 21.60 | 23.70 |
| 11 | F | 41 | 5.52 | 7.07 | 23.95 | 25.03 | 7.12 | 7.45 | 26.70 | 27.87 |
| 12 | M | 36 | 6.46 | 5.83 | 22.47 | 22.99 | 7.07 | 7.53 | 22.99 | 23.85 |
| 13 | M | 40 | 6.60 | 7.45 | 26.09 | 27.81 | 7.31 | 7.29 | 29.17 | 30.12 |
| 14 | F | 53 | 6.42 | 7.10 | 24.59 | 24.21 | 6.90 | 6.89 | 25.71 | 26.31 |
| 15 | M | 43 | 3.98a | 5.13a | 26.10 | 23.30 | 6.02 | 7.60 | 26.83 | 28.76 |
| 16 | F | 54 | 5.36a | 4.45a | 27.53 | 30.00 | 5.65 | 6.07 | 22.50 | 23.54 |
| 17 | M | 58 | 8.75 | 9.00 | 26.96 | 27.34 | 6.75 | 6.43 | 24.02 | 25.28 |
| 18 | M | 33 | 5.33a | 6.22 | 24.59 | 24.22 | 7.07 | 8.29 | 23.44 | 26.44 |
| 19 | M | 19 | 5.58 | 7.36 | 21.84 | 22.48 | 6.46 | 5.65 | 25.29 | 25.80 |
| 20 | M | 30 | 4.23a | 5.71 | 28.06 | 28.45 | 6.00 | 6.75 | 25.66 | 26.83 |
| 21 | M | 47 | 5.75 | 6.08 | 22.28 | 21.78 | 5.59 | 6.71 | 26.60 | 28.41 |
| 22 | F | 46 | 3.85a | 5.40a | 25.53 | 24.26 | 6.86 | 6.94 | 23.86 | 25.46 |
| 23 | F | 34 | 3.50a | 5.22a | 25.23 | 24.30 | 6.42 | 6.08 | 24.75 | 26.24 |
| 24 | F | 61 | 4.31a | 5.82 | 24.89 | 24.11 | 7.37 | 7.78 | 22.57 | 23.73 |
| 25 | F | 38 | 8.80 | 7.64 | 26.95 | 26.52 | 6.95 | 6.99 | 26.67 | 24.35 |
| 26 | M | 63 | 5.20a | 4.89a | 20.98 | 20.15 | 6.39 | 7.00 | 25.42 | 24.65 |
| 27 | M | 41 | 5.60 | 5.55 | 21.40 | 20.70 | 8.06 | 7.58 | 21.77 | 22.00 |
| 28 | M | 25 | 4.49a | 9.86 | 22.82 | 26.32 | 6.25 | 7.68 | 25.98 | 27.36 |
| 29 | F | 20 | 6.52 | 3.65a | 23.85 | 24.56 | 6.24 | 7.12 | 22.63 | 23.52 |
aThe trajectory diameter is less than 5.5 mm)
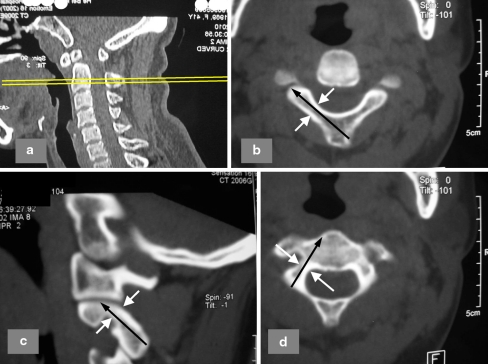
Fig. 1.
A 41 years old lady with os odontoideum was shown. a Lateral X-ray revealed os and atlantoaxial instability; b reconstructive CT; c, d MRI showed compression and high signal of the cervical spinal cord
Among these patients, 19 were male and 10 were female, aged from 19 to 63 years (averaged 42.4 years). The clinical symptoms and signs included: neck movement restriction in 26 cases, neck pain in 25, extremities weakness in 22, numbness in 21, pyramidal signs in 16 and sphincter disturbances in 6 cases.
Prior to surgery, reconstructive computed tomography (CT) was performed for all 29 patients. Three-dimensional (3D) CT was performed using a 64-slice scanner. The CT parameters were: 120 kV, 500 mA, 0.6 s/rotation, table speed with 0.5 mm/rotation and 1.0 mm slice interval. Three sagittal slices were obtained for each lateral mass of C2, and three axial slices obtained for C2 laminar. The slice with the thickest isthmus and laminar of C2 were selected for the measurement. The method recommended by Neo et al. [24] and Wang et al. [34] was used to determine the diameters and length for the ideal screw trajectory from the CT images, i.e. along the ideal screw trajectory in the sagittal and axial planes, the maximum possible diameters and length of lamina and pedicle screws were measured (Fig. 2). The trajectory diameter of at least 5.5 mm wide is considered suitable to place a pedicle or laminar screw, allowing 1 mm tolerance of error on either side of a 3.5 mm diameter screw.
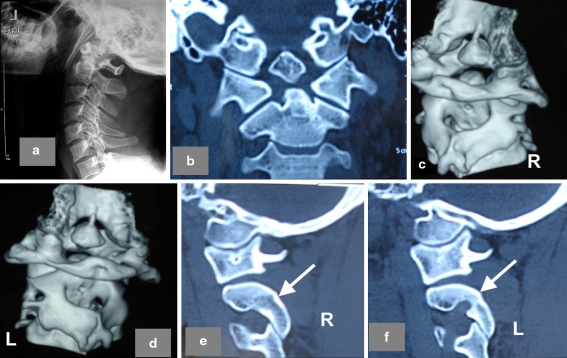
Fig. 2.
Measurement of C2 pedicle and laminar. a Sagittal plane. b In the axial plane, measurement for laminar screw was shown. c, d Ideal diameter (white arrows) and length (black arrow) of the C2 pedicle were determined from the sagittal and the axial plane
The data was measured on PACS (Version 2.1.2.1, GE, Germany). Two senior spine surgeons each measured the diameter of C2 pedicle for all 29 patients independently before the results were averaged. Each measurement was made twice by the same surgeon at a 2-week’s interval. The intra-observer reliability and inter-observer repeatability of the measurements was assessed using intraclass correlation coefficient (ICC), which was calculated using SPSS (version 15.0).
Results
Reliability test of the CT scan measurements: intraobserver (ICC = 0.95 and 0.96) and interobserver correlation coefficient (ICC = 0.93).
The lengths and diameters for the ideal C2 pedicles and laminar trajectory of all the cases are shown in Table 1.
Both mean diameters and lengths of the C2 laminar screw trajectory are significantly larger than those of a C2 pedicle screw (Table 2).
In each of the 29 cases the diameter of the lamina (from 5.52 to 8.82 mm) is larger than 5.5 mm (sufficient for C2 laminar screw implantation). For the C2 pedicle, the diameters range from 3.50 to 9.86 mm, with 20 pedicles (34.5%) from 14 patients (6 are bilateral) less than 5 mm in diameter (Fig. 3; Table 1).
Table 2.
The values of C2 pedicles and lamina (no significant difference was found in any of the measurements from either side of the patients)
| C2 pedicle trajectory (mm) | C2 laminar trajectory (mm) | P value | |
|---|---|---|---|
| Diameter | 6.06 ± 1.37 | 6.95 ± 0.82 | 0.000 |
| Length | 24.05 ± 2.54 | 25.60 ± 2.18 | 0.001 |
Independent T test (SPSS, Version15.0)
Fig. 3.
A 25-year-old male with incomplete paralysis was diagnosed as os odontoideum. a Lateral X-ray revealed os and atlantoaxial instability; b coronal plane of CT showed the ossicle; c, d C2 pedicles were showed on the 3D CT; e on the sagittal CT plane, the right C2 pedicle was efficient for a 3.5 mm screw; f diameter of his left C2 pedicle was only 4.4 mm, and placement of C2 pedicle screw would risk the vertebral artery
Discussion
The guideline for the use of C2 pedicle and laminar screws has been established based on epidemiological method. For an average adult, the mean diameter and length of C2 pedicle are 5.8–8 and 24–31 mm, respectively [25, 27, 34, 37], and those of C2 lamina are 5.75–6.3 and 24.6–31.6 mm [4, 7, 32]. These parameters should allow the use of both pedicle and laminar screws for C2 fixation. However, our experience suggests that patients with os odontoideum often had small and thin pedicles, which increases the risk of vertebral artery injury. Although the etiology remains unclear [2, 9, 22], it is commonly observed that patients with os odontoideum are likely to have multiple bony anomalies in the vertebral elements, for developmental or congenital reasons. It is therefore presumed that the guidelines based on the measurements obtained from the general population may not apply to OO patients. The results of the present study indicates that nearly half of our patients (14/29) have at least one of their pedicles less than 5.5 mm in diameter with the smallest being 3.5 mm (Fig. 3f), where the use of the 3.5 mm pedicle screw must be abandoned. In contrast, according to the measurements, the use of C2 laminar screw is not an issue for any of the patient as far as the dimension is concerned. It appears that C2 laminar screw provides a reliable alternative method of fixation for OO patients when the pedicle screw cannot be used. Another advantage in the use of C2 laminar screw is that it remarkably reduces the risk of vertebral artery injury. However, disadvantages of laminar screw are not to be ignored. Fin [10] reported several drawbacks of the C2 laminar screw including associated reduced the surface of fusion bed and biomechanically weaker than the C2 pedicle screws. It was also indicated by Wang et al. [34] that the C2 laminar screw had less force when act as a posterior anchor in comparison with the pedicle screw. In the present study, 20 C2 pedicles from 14 patients were found to have a diameter less than 5.5 mm. For these cases, C2 laminal screw is the only option if it is to avoid VA injury. Even among the 14 patients with mal-developed C2 pedicles (Φ < 3.5 mm), there were 8 patients to whom the pedicle screw can be applied unilaterally, which provides enough strength even if not as strong as bilateral use of pedicle screws. For those patients (6/29) who have both C2 pedicles less than 3.5 mm, bilateral use of laminal screw is the only but not necessarily the worst option. Based on a large series of 167 consecutive cases, Parkers et al. reported that C2 laminar screw was equally effective with pedicle screw for axial cervical fusion [26].
Using a CT study, Yoshida et al. [37] deemed a trajectory of 4 mm in diameter as risky for C2 pedicle screw placement and 3 mm or less as unacceptable. In another CT study [34], a 4.5 mm diameter was considered sufficient for a safe C2 pedicle screw placement. Wang [32] suggested that the diameter of C2 lamina less than 5.5 mm was too small to accommodate a 3.5 mm screw based on a cadaveric morphometric study. We used 5.5 mm as the criteria in the present study according to our experience that a 1 mm tolerance of error on each side of the pedicle or laminar screw should be allowed. Although 3.5 mm screw is still being used on pedicles with less than 5.5 mm diameter by some experienced surgeons [34], it is our recommendation to replace it with laminal screw as it is safer and anatomically sound.
This study can be criticized in that measurements were performed using CT scan rather than directly on cadaveric specimens. Nevertheless, several previous reports have used preoperative CT scan to establish the guidelines for pedicle or laminar screw placement [3, 16, 34, 37]. Moreover, Dean [7] compared direct anatomic measurement with CT measurement and demonstrated measurement obtained from CT was significantly correlated with the true anatomic measurements of C2 laminar thickness and length. In addition, the data from cadaveric specimens may have overrepresentation of elder population and introduce morphological changes secondary to age-related processes such as arthritis and degeneration [16]. Alternatively, CT measurements in our patients represent the data from a broad range of age (from 19 to 63 years).
In summary, we found 34.5% of the C2 pedicles in os odontoideum patients could be insufficient for pedicle screw implantation. Laminar screw is more anatomically suitable than pedicle screw for C2 fixation in OO patients. The options for C2 fixation should be determined based on careful preoperative imaging and thorough consideration. Preoperative reconstructive CT is an excellent and important method to reveal the anatomy of the C2 segment before the choice of fixation is made.
Conflict of interest
None.
References
- 1.Al Kaissi A, Chehida FB, Ghachem MB, Grill F, Klaushofer K. Atlanto-axial segmentation defects and os odontoideum in two male siblings with opsismodysplasia. Skeletal Radiol. 2009;38:293–296. doi: 10.1007/s00256-008-0623-4. [DOI] [PubMed] [Google Scholar]
- 2.Arvin B, Fournier-Gosselin MP, Fehlings MG. Os odontoideum: etiology and surgical management. Neurosurgery. 2010;66:22–31. doi: 10.1227/01.NEU.0000366113.15248.07. [DOI] [PubMed] [Google Scholar]
- 3.Bhatnagar R, Yu WD, Bergin PF, Matteini LE, O’Brien JR. The anatomic suitability of the C2 vertebra for intralaminar and pedicular fixation: a computed tomography study. Spine J. 2010;10:896–899. doi: 10.1016/j.spinee.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 4.Cassinelli EH, Lee M, Skalak A, Ahn NU, Wright NM. Anatomic considerations for the placement of C2 laminar screws. Spine (Phila Pa 1976) 2006;31:2767–2771. doi: 10.1097/01.brs.0000245869.85276.f4. [DOI] [PubMed] [Google Scholar]
- 5.Dai L, Yuan W, Ni B, Jia L (2000) Os odontoideum: etiology, diagnosis, and management. Surg Neurol 53:106–108 (discussion 108–109) [DOI] [PubMed]
- 6.Iure F, Donthineni R, Boriani S. Outcomes of C1 and C2 posterior screw fixation for upper cervical spine fusion. Eur Spine J. 2009;18(Suppl 1):2–6. doi: 10.1007/s00586-009-0981-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dean CL, Lee MJ, Robbin M, Cassinelli EH. Correlation between computed tomography measurements and direct anatomic measurements of the axis for consideration of C2 laminar screw placement. Spine J. 2009;9:258–262. doi: 10.1016/j.spinee.2008.06.454. [DOI] [PubMed] [Google Scholar]
- 8.Fagan AB, Askin GN, Earwaker JW. The jigsaw sign. A reliable indicator of congenital aetiology in os odontoideum. Eur Spine J. 2004;13:295–300. doi: 10.1007/s00586-004-0732-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fielding JW, Hensinger RN, Hawkins RJ. Os Odontoideum. J Bone Joint Surg Am. 1980;62:376–383. [PubMed] [Google Scholar]
- 10.Finn MA, Fassett DR, McCall TD, Clark R, Dailey AT, Brodke DS. The cervical end of an occipitocervical fusion: a biomechanical evaluation of 3 constructs. Laboratory investigation. J Neurosurg Spine. 2008;9:296–300. doi: 10.3171/SPI/2008/9/9/296. [DOI] [PubMed] [Google Scholar]
- 11.Goel A, Desai KI, Muzumdar DP (2002) Atlantoaxial fixation using plate and screw method: a report of 160 treated patients. Neurosurgery 51:1351–1356 (discussion 1356–1357) [PubMed]
- 12.Grob D, Bremerich FH, Dvorak J, Mannion AF. Transarticular screw fixation for osteoarthritis of the atlanto axial segment. Eur Spine J. 2006;15:283–291. doi: 10.1007/s00586-005-0963-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hammerstein J, Russo S, Easton K. Atlantoaxial dislocation in a child secondary to a displaced chondrum terminale. A case report. J Bone Joint Surg Am. 2007;89:413–417. doi: 10.2106/JBJS.E.00595. [DOI] [PubMed] [Google Scholar]
- 14.Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976) 2001;26:2467–2471. doi: 10.1097/00007632-200111150-00014. [DOI] [PubMed] [Google Scholar]
- 15.Heuer GG, Hardesty DA, Bhowmick DA, Bailey R, Magge SN, Storm PB. Treatment of pediatric atlantoaxial instability with traditional and modified Goel-Harms fusion constructs. Eur Spine J. 2009;18:884–892. doi: 10.1007/s00586-009-0969-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoh DJ, Liu CY, Wang MY. A radiographic computed tomography-based study to determine the ideal entry point, trajectory, and length for safe fixation using C-2 pars interarticularis screws. J Neurosurg Spine. 2010;12:602–612. doi: 10.3171/2009.12.SPINE09543. [DOI] [PubMed] [Google Scholar]
- 17.Jeanneret B, Magerl F. Primary posterior fusion C1/2 in odontoid fractures: indications, technique, and results of transarticular screw fixation. J Spinal Disord. 1992;5:464–475. doi: 10.1097/00002517-199212000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Lu S, Xu YQ, Zhang YZ, Xie L, Guo H, Li DP. A novel computer-assisted drill guide template for placement of C2 laminar screws. Eur Spine J. 2009;18:1379–1385. doi: 10.1007/s00586-009-1051-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ma W, Feng L, Xu R, Liu X, Lee AH, Sun S, Zhao L, Hu Y, Liu G. Clinical application of C2 laminar screw technique. Eur Spine J. 2010;19:1312–1317. doi: 10.1007/s00586-010-1447-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Madawi AA, Casey AT, Solanki GA, Tuite G, Veres R, Crockard HA. Radiological and anatomical evaluation of the atlantoaxial transarticular screw fixation technique. J Neurosurg. 1997;86:961–968. doi: 10.3171/jns.1997.86.6.0961. [DOI] [PubMed] [Google Scholar]
- 21.Melcher RP, Puttlitz CM, Kleinstueck FS, Lotz JC, Harms J, Bradford DS. Biomechanical testing of posterior atlantoaxial fixation techniques. Spine (Phila Pa 1976) 2002;27:2435–2440. doi: 10.1097/00007632-200211150-00004. [DOI] [PubMed] [Google Scholar]
- 22.Menezes AH. Pathogenesis, dynamics, and management of os odontoideum. Neurosurg Focus. 1999;6:e2. doi: 10.3171/foc.1999.6.6.5. [DOI] [PubMed] [Google Scholar]
- 23.Morgan MK, Onofrio BM, Bender CE. Familial os odontoideum. Case report. J Neurosurg. 1989;70:636–639. doi: 10.3171/jns.1989.70.4.0636. [DOI] [PubMed] [Google Scholar]
- 24.Neo M, Matsushita M, Iwashita Y, Yasuda T, Sakamoto T, Nakamura T. Atlantoaxial transarticular screw fixation for a high-riding vertebral artery. Spine (Phila Pa 1976) 2003;28:666–670. doi: 10.1097/01.BRS.0000051919.14927.57. [DOI] [PubMed] [Google Scholar]
- 25.Panjabi MM, Duranceau J, Goel V, Oxland T, Takata K. Cervical human vertebrae. Quantitative three-dimensional anatomy of the middle and lower regions. Spine (Phila Pa 1976) 1991;16:861–869. doi: 10.1097/00007632-199108000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Parker SL, McGirt MJ, Garces-Ambrossi GL, Mehta VA, Sciubba DM, Witham TF, Gokaslan ZL, Wolinksy JP (2009) Translaminar versus pedicle screw fixation of C2: comparison of surgical morbidity and accuracy of 313 consecutive screws. Neurosurgery 64:343–348 (discussion 348–349) [DOI] [PubMed]
- 27.Resnick DK, Lapsiwala S, Trost GR. Anatomic suitability of the C1-C2 complex for pedicle screw fixation. Spine (Phila Pa 1976) 2002;27:1494–1498. doi: 10.1097/00007632-200207150-00003. [DOI] [PubMed] [Google Scholar]
- 28.Sciubba DM, Noggle JC, Vellimana AK, Alosh H, McGirt MJ, Gokaslan ZL, Wolinsky JP. Radiographic and clinical evaluation of free-hand placement of C-2 pedicle screws. Clinical article. J Neurosurg Spine. 2009;11:15–22. doi: 10.3171/2009.3.SPINE08166. [DOI] [PubMed] [Google Scholar]
- 29.Spierings EL, Braakman R. The management of os odontoideum. Analysis of 37 cases. J Bone Joint Surg Br. 1982;64:422–428. doi: 10.1302/0301-620X.64B4.7096415. [DOI] [PubMed] [Google Scholar]
- 30.Wang C, Yan M, Zhou H, Wang S, Dang G. Atlantoaxial transarticular screw fixation with morselized autograft and without additional internal fixation: technical description and report of 57 cases. Spine (Phila Pa 1976) 2007;32:643–646. doi: 10.1097/01.brs.0000257539.75693.cc. [DOI] [PubMed] [Google Scholar]
- 31.Wang C, Yan M, Zhou HT, Wang SL, Dang GT. Open reduction of irreducible atlantoaxial dislocation by transoral anterior atlantoaxial release and posterior internal fixation. Spine (Phila Pa 1976) 2006;31:E306–E313. doi: 10.1097/01.brs.0000217686.80327.e4. [DOI] [PubMed] [Google Scholar]
- 32.Wang MY (2006) C2 crossing laminar screws: cadaveric morphometric analysis. Neurosurgery 59:ONS84–88 (discussion ONS84–88) [DOI] [PubMed]
- 33.Wang S, Wang C. Familial dystopic os odontoideum: a report of three cases. J Bone Joint Surg Am. 2011;93:e44. doi: 10.2106/JBJS.J.01018. [DOI] [PubMed] [Google Scholar]
- 34.Wang S, Wang C, Passias PG, Yan M, Zhou H. Pedicle versus laminar screws: what provides more suitable C2 fixation in congenital C2-3 fusion patients? Eur Spine J. 2010;19:1306–1311. doi: 10.1007/s00586-010-1418-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang S, Wang C, Wood KB, Yan M, Zhou H. Radiographic evaluation of the technique for c1 lateral mass and c2 pedicle screw fixation in three hundred nineteen cases. Spine (Phila Pa 1976) 2011;36:3–8. doi: 10.1097/BRS.0b013e3181c97dc7. [DOI] [PubMed] [Google Scholar]
- 36.Wright NM. Posterior C2 fixation using bilateral, crossing C2 laminar screws: case series and technical note. J Spinal Disord Tech. 2004;17:158–162. doi: 10.1097/00024720-200404000-00014. [DOI] [PubMed] [Google Scholar]
- 37.Yoshida M, Neo M, Fujibayashi S, Nakamura T. Comparison of the anatomical risk for vertebral artery injury associated with the C2-pedicle screw and atlantoaxial transarticular screw. Spine (Phila Pa 1976. 2006;31:E513–E517. doi: 10.1097/01.brs.0000224516.29747.52. [DOI] [PubMed] [Google Scholar]
- 38.Yue B, Kwak DS, Kim MK, Kwon SO, Han SH. Morphometric trajectory analysis for the C2 crossing laminar screw technique. Eur Spine J. 2010;19:828–832. doi: 10.1007/s00586-010-1331-z. [DOI] [PMC free article] [PubMed] [Google Scholar]