Abstract
Anterior screw fixation of Type II odontoid fractures has been recommended. Only few publications analyse the mechanism of failure in geriatric patients. We reviewed 18 male and 15 female patients aged 65 and above for parameters that influence the development of postoperative loss of correction, delayed union or non-union. Patients were stratified in two groups: 21 cases in Group A (union) and 12 patients in Group B (loss of correction, delayed union, non-union, revision surgery). Statistically significant correlation (p < 0.05) could be detected between failure to heal and: (1) degenerative changes in the atlanto-odontoid joint, (2) severity of osteoporosis in the odontoid process, (3) posterior oblique fracture type, (4) suboptimal fracture reduction, (5) suboptimal position of implant following demanding intraoperative conditions, (6) quality of fracture compression and (7) severity of fracture comminution. The overall morbidity and mortality rates were 29.0 and 8.6%, respectively. Our results indicate that these factors should be addressed regarding the selection of the operative treatment method in the geriatric patient.
Keywords: Odontoid fracture, Anterior screw fixation, Geriatric patient, Failure analysis
Introduction
Type II odontoid fractures are frequent in the elderly population. The prevalence of these injuries is expected to progressively increase. Concomitant diseases cause high perioperative morbidity and mortality and compromise the outcome in geriatric patients. Various studies have addressed the ideal management of these injuries [1–6]. Others covered the outcome following anterior screw fixation of Type II odontoid fractures and recommended the surgical strategy [4, 7–10]. Both younger and elderly patients revealed similar clinical results [4]. Nevertheless, recent publications reported that insufficient bony healing results from osteoporosis and diminished bone quality [1, 3, 4, 11]. Clinical routine confirms that fracture re-dislocation and healing disturbances are more common than preferable.
The purpose of this study was to determine influencing parameters for intra- and postoperative complications and fusion rates and to analyse the clinical outcome in patients aged 65 and above who underwent anterior screw fixation of Type II odontoid fractures. We, therefore, retrospectively tried to validate the presumption that concomitant cervical spine degeneration, fracture pattern, osteoporosis and suboptimal compression of the fracture gap may impair the development of union.
Materials and methods
Between February 2000 and July 2010 we performed 46 direct anterior screw fixations of unstable Type II odontoid fractures at our hospital on 35 patients aged 65 years or above. Two patients died within 2 weeks after surgery from heart failure and respiratory insufficiency following pneumonia, respectively, leaving a total of 33 patients who were enrolled in this study. For the collection of preoperative variables and the calculation of morbidity and mortality rates, the two patients that had deceased after surgery were included. Depending on specific fracture complications leading to re-operation, patients were stratified into two study groups: Group A (union) included 21 patients with an uneventful healing process. Group B (non-union) contained 12 patients with non-union, implant failure, secondary loss of correction and obligatory revision surgery. The separation was based on recent reports in literature, indicating a higher complication and non-union rate in the elderly and on the hypothesis that certain factors may influence an uncomplicated bony consolidation process. Clinical and radiographic records of all patients were reviewed on average 5.6 years (range 0.8–10.7 years) after operation.
We obtained pre- and postoperative CT scans and plain radiography with transoral and lateral views in all patients. Collected variables included age, gender, mechanism of injury, fracture type, fracture dislocation, presence of neurologic deficits, associated injuries, pre-existing systemic disease and surgical risk factors, method of surgical treatment, duration of operative procedure, demanding intraoperative conditions and difficulties (reduced cervical length and protruding thorax), severity of osteoporosis and cervical spine degeneration and radiographic outcome after surgery. The type of fracture was assessed according to the classification systems of Anderson and D’Alonso and of Roy-Camille. The severity of degenerative changes of the upper cervical spine was evaluated for the atlanto-odontoid joint, the atlanto-occipital joint and the lateral atlanto-axial joints (Table 1). Concomitant ankylosis was also documented. Severity of osteoporosis of the axis was graded at the dens-body junction and in the odontoid process as suggested by Lakshmanan et al. [2] (Table 1). Postoperative CT scans and plain radiographs were analysed for compression of the fracture gap and classified according to the correctness of fracture reduction achieved during surgery. Fracture reduction and compression were graded as correct (1), moderate (2) or poor (3). Primary dislocation and size of the fracture gap were measured in millimetres. The angulation between odontoid process and peripheral fragment was recorded and the amount of fracture comminution was graded none (1), minor (2) or severe (3). Clinical and radiographic follow-up examinations were reviewed for secondary loss of correction, implant malposition and implant failure as well as for patient satisfaction and limitations. Clinical results were assessed according to the Smiley-Webster functional outcome scale in patients with a minimum follow-up period of 24 months. Postoperative monitoring of the patients consisted of follow-up visits at 6, 12 and 24 weeks and further at 12 and 24 months after surgery.
Table 1.
Grading of degeneration and osteoporosis
| Grading of severity of degenerative changes in the C0–C2 joints (according to Lakshmanan et al. [2]) |
| None (1): normal joint space with no osteophyte formation |
| Mild (2): narrowed joint space or normal joint space with osteophyte formation |
| Moderate (3): obliterated joint space with or without osteophyte formation |
| Severe (4): completely obliterated joint space, ankylosis or fusion of the joint |
| Grading of severity of osteoporosis in C2 (according to Lakshmanan et al. [2]) |
| None (1): normal trabecular pattern with normal cortical thickness |
| Mild (2): decrease in the amount of trabeculae with no areas of holes and normal cortical thickness |
| Moderate (3): absent trabeculae (holes) involving less than 25% of the transverse diameter of the bone with cortical thinning |
| Severe (4): absent trabeculae (holes) involving more than 50% of the transverse diameter of the bone with cortical thinning |
Statistical analysis
Pre-, intra- and postoperative variables were compared between the two groups. To compare quantitative data, we performed the Wilcoxon Sum-of-Ranks test. For categorical data the Fisher Exact test was used. Statistical significance was defined as p < 0.05.
Results
18 male and 15 female patients with an average age of 79.6 years (range 65.1–94.0 years) were enrolled in the study. Solid bony union was achieved in 21 patients, who entered study Group A. A total of 12 patients (36.4%) presented with early re-dislocation, unstable delayed unions or non-unions and were included in Group B. The injuries resulted from low energy falls in 26 patients (74.3%), traffic accidents in 4 patients (11.4%), falls from a considerable height in 4 patients (11.4%) and from other causes in 1 patient (2.9%). According to the classification of Anderson and D’Alonso all patients had sustained a Type II odontoid fracture. Using the system of Roy-Camille we found 17 patients (48.6%) with a horizontal fracture and 18 patients (51.4%) with a posterior oblique fracture. Initial displacement was slight (<2 mm) in 10 cases and significant (≥2 mm) in 25 cases. The average displacement before surgery was 3.20 mm (range 0–9 mm). On Comparing between the two study groups, we found no statistically significant difference regarding trauma mechanism and amount of initial fracture displacement (Table 2). Regarding to the fracture type we observed a statistically significant accumulation of posterior oblique fractures in study Group B (p < 0.05). The size of the fracture gap averaged to 2.51 mm (range 0.3–5.0 mm) in Group A and to 2.48 mm (range 0.5–4.9 mm) in Group B. Fracture angulation was on average 15.7° (range 0°–38°) in Group A and 15.3° (range 3°–38°) in Group B (Table 2). Severe fracture comminution was more frequent in study Group B (p < 0.05).
Table 2.
Comparison of results between the study groups
| Group A | Group B | p value | |
|---|---|---|---|
| Low energy trauma | 71.4% | 83.3% | |
| Fracture type (Roy-Camille) | |||
| Posterior oblique | 33.3% | 83.3% | p < 0.01040 |
| Initial displacement | |||
| Slight | 23.8% | 33.3% | |
| Significant | 76.2% | 66.7% | |
| Fracture gap (mm) | 2.51 | 2.48 | |
| Angulation (°) | 15.7 | 15.3 | |
| Severe comminution | 50.0% | 13.3% | p < 0.04544 |
| Severity of osteoporosis | 2.47 | 3.00 | p < 0.02435 |
| Severity of osteoarthritis | |||
| Atlanto-dental | 2.38 | 3.25 | p < 0.00661 |
| Atlanto-occipital | 2.20 | 2.33 | |
| Atlanto-axial | 2.13 | 2.08 | |
| Ankylosis | 6.3% | 25.0% | |
| Number of screws | |||
| 2 | 85.7% | 58.3% | |
| 1 | 14.3% | 41.7% | |
| Demanding surgical conditions | 9.5% | 25.0% | |
| Duration of surgery (min) | 79.7 | 71.6 | |
| Delay of treatment (days) | 6.8 | 6.0 | |
| Optimal fracture compression | 81.0% | 25.0% | p < 0.00629 |
| Optimal fracture reduction | 85.0% | 41.6% | p < 0.03075 |
| Optimal implant positioning | 90.1% | 41.6% | p < 0.00460 |
| Associated injuries | 33.3% | 33.3% | |
| Pre-existing diseases | 38.1% | 41.6% | |
| Morbidity | 23.8% | 16.7% | |
12 patients presented with associated injuries. Four patients had a severe head or thorax injury, three patients sustained significant fractures of the extremities and five patients presented with minor injuries of head, thorax or extremities. None of the patients showed neurologic deficits at the time of admission to the hospital, corresponding to grade E in the ASIA classification. Postoperative deterioration of the neurologic status was never recorded. Pre-existing systemic diseases were found in 42.9% of the patients (chronic cardiac insufficiency in eight, chronic renal insufficiency in seven, obstructive pulmonary disease in four, cardiac arrhythmia in five and diabetes mellitus in three cases). Comparing the two study groups, no statistically significant difference regarding associated injuries or pre-existing diseases could be detected (Table 2).
All patients underwent operative treatment on average 6.1 days (range 0–28) after the trauma. Three patients were initially treated with a halo fixateur but, as they did not tolerate the external fixation, were submitted to an operation within 4 weeks. Operation time averaged to 79.1 min (range 35–188). 26 patients received a single, 9 patients a double lag screw fixation. Postoperative immobilisation was routinely accomplished by a soft collar for 6 weeks. The interval between trauma and operation, the number of implants and the duration of surgery were distributed similarly between the two study groups without statistically significant differences (Table 2).
Eight cases underwent revision surgery with posterior atlanto-axial fusion in seven and occipito-cervical C0–C4 fusion in one patient on average 51.4 weeks (range 4.9–268.9 weeks) after the initial operation. All of them had developed unstable delayed union or non-union with redislocation. Occipito-cervical fusion was performed in a patient with a concomitant fracture of the posterior arch of the atlas. Five patients developed non-unions with absence of bony consolidation after 6 months leading to a total non-union rate of 15.2%. Secondary loss of correction within 12 weeks after screw fixation was documented in seven patients, leading to an early postoperative complication rate of 21.2%. Loosening or cut-out of the implants was found in 13 patients (39.4%). Four patients in Group A and nine patients in Group B presented with a loosening of the implant. In 27.3% of the cases a malposition of the screws was documented on postoperative radiographs and CT scans. Fracture reduction was classified as poor in two cases and moderate in eight cases. Fracture compression was sufficient in 20 patients, moderate in 12 patients and poor in 1 patient.
Malposition of the implants, suboptimal or incorrect fracture reduction as well as insufficient fracture compression revealed a statistically significant influence on the development of non-union and secondary loss of correction (p < 0.05, Table 2).
Degenerative changes and osteoporosis of the upper cervical spine were present in all patients. Severity of osteoporosis averaged to 2.47 in Group A and to 3.00 in Group B (p < 0.05). The average severity of degeneration in the atlanto-odontoid joint was graded 2.38 in Group A and 3.25 in Group B (p < 0.05). Degeneration of the atlanto-axial and the atlanto-occipital joint and the presence of ankylosis of the upper cervical spine did not show any relevant influence on the postoperative outcome (Table 2).
Demanding intraoperative conditions and anatomical variations were recorded in six patients (18.2%) without any significant difference in distribution between the study groups.
General complications occurred in ten patients (cardiac failure in 4, respiratory failure in 6, pneumonia in 5 and renal failure in 7 cases), leading to an overall morbidity rate of 29.0%. Three patients died on average 9 days (range 6–13) after the operation. The causes of death were cardiac arrest in two cases and pneumonia with respiratory insufficiency in one case. The overall mortality rate was 8.6%. Comparing the two study groups, we found no statistically significant influence on fracture healing with regard to morbidity and mortality rates (Table 2).
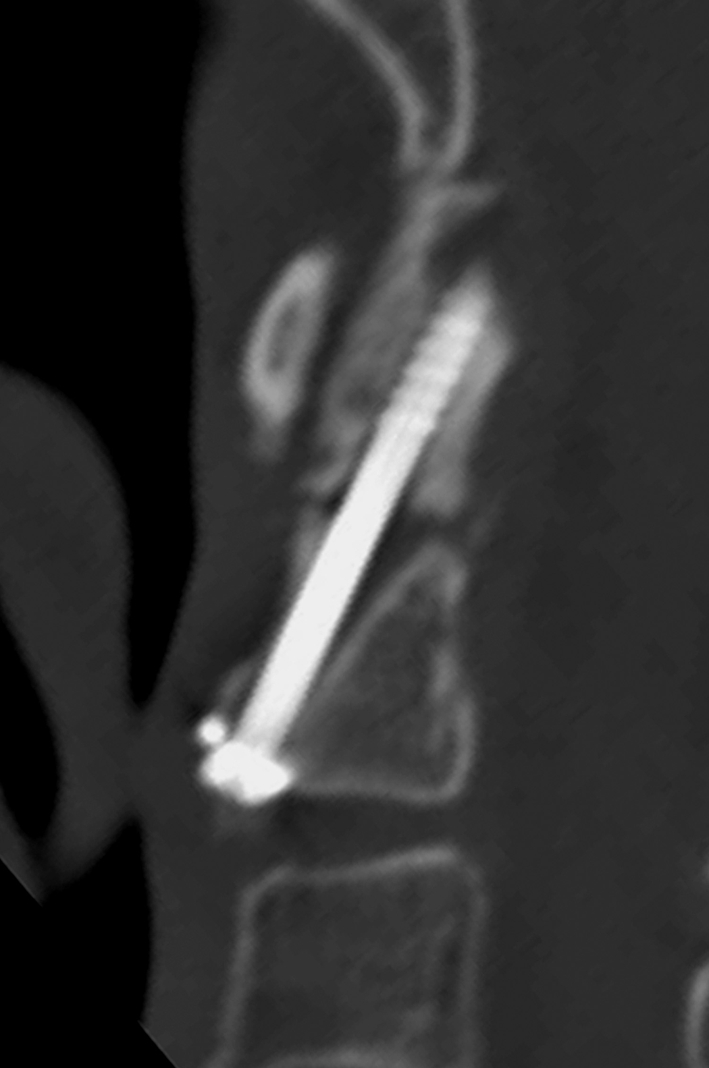
Clinical results were obtained in 25 patients (75.8%) with a complete follow-up of at least 2 years after the initial operation (average 6.2 years, range 2.7–10.7 years). The Smiley-Webster functional outcome scale, grading the results from excellent (1) to poor (4), averaged to 1.65 for all patients. We found a return to pre-injury activity levels in 71.4%. Cervical spine movement was normal in 57.1%. 10.7% of the patients complained a restriction of cervical range of motion of more than 30%. None of the patients presented with neurologic deficits, regular pain or severe symptoms. A bony fracture union, documented by plain transoral and lateral radiographs, was achieved in 18 of these patients (72.0%) on average 7.5 weeks (range 5.1–11.0 weeks) after the operation (Fig. 1).
Fig. 1.

Fracture reduced and compressed after anterior screw fixation. Mild osteoarthritic changes at C0–C2 levels. Signs of mild osteoporosis in axis body and odontoid process. Uneventful bony consolidation
Conclusion
The technique of direct anterior screw fixation has been widely accepted as the treatment of choice for Type II fractures of the odontoid process. Other options, available for the management of these injuries, include atlantoaxial fusion with posterior transarticular screw fixation of C1 and C2 and combination with interlaminar bone grafting, posterior fusion utilizing a screw-rod-system in C1 and C2 and direct anterior transarticular screw fixation [12–16, 19–23].
Several authors have suggested posterior cervical fusion as the method of choice for the treatment of odontoid fractures in elderly patients, whereas others found successful results using anterior screw fixation [1, 4, 12, 16, 19–23].
The influence of determining factors that may compromise fracture healing in geriatric patients remains a controversial issue. The most recent study on this topic was published by Cho et al. [17], who found a statistically significant correlation between fusion failure and delayed surgery (≥1 week) and a fracture gap ≥2 mm, whereas no association with patient age and fracture displacement was detected. This confirms the observation of Koivikko et al. [18], who reported a significant correlation between non-union and a fracture gap size >1 mm, a posterior displacement >5 mm and a delayed start of treatment >4 days in conservatively treated patients. In our study, initial displacement, fracture angulation and size of the fracture gap tended to be larger.
The correlation shown in our study suggests an association between fracture type, severity of fracture comminution, postoperative quality of fracture compression, severity of concomitant osteoporosis and degeneration of the atlanto-odontoid joint. Anatomical variations in cervical length and construction of the anterior thoracic wall present demanding intraoperative preconditions that may further negatively impair effective fracture healing.
Hypothetically, the avoidance of a rigid fixation of the atlanto-axial joint by posterior or anterior fusion techniques to preserve cervical spine movement without noticeable restrictions, may not necessarily imply a crucial benefit on geriatric patients’ subjective outcome [13].
With physiological cervical spine motion, osteoporotic bone promotes the formation a cone-shaped excavation around the screw shank that may reduce the anchorage of the screw at dens-body junction (Fig. 2). These conditions may facilitate an oscillating movement of the odontoid fragment and the implants related to the axis body which interferes with fracture compression and fixation (Fig. 3).
Fig. 2.
Odontoid non-union with anterior screw in situ. Screw thread anchored in sclerotic bone at apex. Cone-shaped excavation at axis body and dens-body junction opening into fracture gap
Fig. 3.
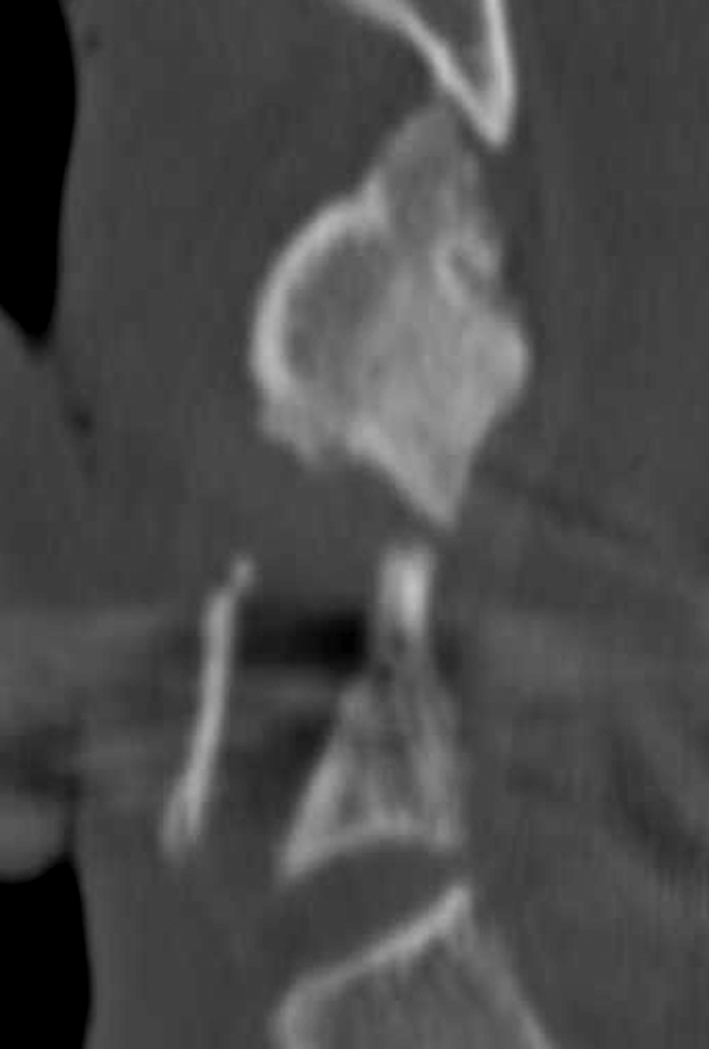
Odontoid non-union after anterior screw fixation. Obliteration of atlanto-odontoid joint space and calcification of the apical and transverse odontoid ligaments. Cone-shaped excavation at axis body and dens-body junction
Demographical data, association to additional injuries, fracture type, displacement of the fracture after trauma and pre-existing diseases were distributed similar to previous reports in literature. The functional outcome assessed by the Smiley-Webster scale was only slightly poorer compared to results in recent publications. If bony consolidation occurs, our clinical results are comparable to literature [4].
The number of patients included in our study is small, the retrospective approach to an intuitive presumption might be problematic but, nevertheless, we believe that our data support the results of previous investigations in literature as well as might serve as a useful basis for the selection of the operative treatment method in geriatric patients.
Our study suggests that failure to heal following direct anterior screw fixation of the odontoid process is associated to (1) suboptimal fracture reduction, (2) suboptimal position of implant following demanding intraoperative conditions and (3) quality of fracture compression. We prefer primary posterior atlanto-axial fusion in cases with (1) moderate degenerative changes in the atlanto-odontoid joint, (2) moderate osteoporosis in the odontoid process, (3) posterior oblique fracture type and (4) severe fracture comminution.
Conflict of interest
None.
References
- 1.Anderson S, Rodrigues M, Olerud C. Odontoid fractures: high complication rate associated with anterior screw fixation in the elderly. Eur Spine J. 2000;9:56–60. doi: 10.1007/s005860050009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lakshmanan P, Jones A, Howes J, Lyons K. CT evaluation of the pattern of odontoid fractures in the elderly—relationship to upper cervical spine osteoarthritis. Eur Spine J. 2005;14:78–83. doi: 10.1007/s00586-004-0743-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Müller EJ, Wick M, Russe O, Muhr G. Management of odontoid fractures in the elderly. Eur Spine J. 1999;8:360–365. doi: 10.1007/s005860050188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Platzer P, Thalhammer G, Ostermann R, Wieland T, Vecsei V, Gaebler C. Anterior screw fixation of odontoid fractures comparing younger and elderly patients. Spine. 2007;32:1714–1720. doi: 10.1097/BRS.0b013e3180dc9758. [DOI] [PubMed] [Google Scholar]
- 5.Pal D, Sell P, Grevitt M. Type II odontoid fractures in the elderly: an evidence-based narrative review of management. Eur Spine J. 2010;20(2):195–204. doi: 10.1007/s00586-010-1507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.White AP, Hashimoto R, Norvell DC, Vaccaro AR. Morbidity and mortality related to odontoid fracture surgery in the elderly population. Spine. 2010;35:146–157. doi: 10.1097/BRS.0b013e3181d830a4. [DOI] [PubMed] [Google Scholar]
- 7.Börm W, Kast E, Richter HP, Mohr K. Anterior screw fixation in Type II odontoid fractures: is there a difference in outcome between age groups? Neurosurgery. 2003;52:1089–1092. doi: 10.1227/01.NEU.0000057697.62046.16. [DOI] [PubMed] [Google Scholar]
- 8.Fountas KN, Kapsalaki EZ, Karampelas I, Feltes CH, Dimopoulos VG, Machinis TG, Nikolakakos LG, Boev AN, Choudhri H, Smisson HF, Robinson JS. Results of long-term follow-up in patients undergoing anterior screw fixation of type II and rostral type III odontoid fractures. Spine. 2005;30:661–669. doi: 10.1097/01.brs.0000155415.89974.d3. [DOI] [PubMed] [Google Scholar]
- 9.Lennarson PJ, Mostafavi H, Traynelis VC, Walters BC. Management of type II dens fractures. Spine. 2000;25:1234–1237. doi: 10.1097/00007632-200005150-00006. [DOI] [PubMed] [Google Scholar]
- 10.Apfelbaum RI, Lonser RR, Veres R, Casey A. Direct anterior screw fixation for recent and remote odontoid fractures. J Neurosurg. 2000;93:227–236. doi: 10.3171/spi.2000.93.2.0227. [DOI] [PubMed] [Google Scholar]
- 11.Harrop JS, Przybylski GJ, Vaccaro AR, Yalamanchili K. Efficiacy of anterior odontoid screw fixation in elderly patients with Type II odontoid fractures. Neurosurg Focus. 2000;8:1–4. [PubMed] [Google Scholar]
- 12.Magerl F, Seeman PS. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In: Kehr P, Weidner A, editors. Cervical spine I. New York: Springer; 1986. pp. 322–327. [Google Scholar]
- 13.Frangen TM, Zilkens C, Muhr G, Schinkel C. Odontoid fractures in the elderly: dorsal C1/C2 fusion is superior to halo-vest immobilisation. J Trauma. 2007;63:83–89. doi: 10.1097/TA.0b013e318060d2b9. [DOI] [PubMed] [Google Scholar]
- 14.Maak TG, Grauer JN. The contemporary treatment of odontoid injuries. Spine. 2006;31:53–60. doi: 10.1097/01.brs.0000217941.55817.52. [DOI] [PubMed] [Google Scholar]
- 15.Platzer P, Vecsei V, Thalhammer G, Oberleitner G, Schurz M, Gaebler C. Posterior atlanto-axial arthrodesis for fixation of odontoid non-unions. Spine. 2008;33:624–630. doi: 10.1097/BRS.0b013e318166dfb8. [DOI] [PubMed] [Google Scholar]
- 16.Aebi M, Etter C, Coscia M. Fractures of the odontoid process. Treatment with anterior screw fixation. Spine. 1989;14:1065–1070. doi: 10.1097/00007632-198910000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Cho DC, Sung JK (2011) Analysis of risk factors associated with fusion failure after anterior odontoid screw fixation. Spine. doi:10.1097/BRS.0b013e31820e6418 [DOI] [PubMed]
- 18.Koivikko M, Kiuru MJ, Koskinen SK, Myllynen P, Santavirta S, Kivisaari L. Factors associated with non-union in conservatively-treated Type II fractures of the odontoid process. J Bone Joint Surg. 2004;86B:1146–1151. doi: 10.1302/0301-620X.86B8.14839. [DOI] [PubMed] [Google Scholar]
- 19.Sen MK, Steffen T, Bechman L, Tsantrizos A, Reindl R, Aebi M. Atlanto-axial fusion using anterior transarticular screw fixation of C1/C2. Technical innovation and biomechanical study. Eur Spine J. 2005;14:512–518. doi: 10.1007/s00586-004-0823-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stulik J, Vyskocil T, Sebesta P, Kryl J. Atlantoaxial fixation using the polyaxial screw-rod system. Eur Spine J. 2007;16:479–484. doi: 10.1007/s00586-006-0241-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilke HJ, Fischer K, Kugler A, Magerl F, Claes L, Wörsdörfer O. In vitro investigations of internalfixation systems of the upper cervical spine. II. Stability of posterior atlanto-axial fixation techniques. Eur Spine J. 1992;1:191–199. doi: 10.1007/BF00301312. [DOI] [PubMed] [Google Scholar]
- 22.Grob D, Crisco JJ, 3rd, Panjabi MM, Wang P, Dvorak J. Biomechanical evaluation of four different posterior atlantoaxial fixation techniques. Spine. 1992;17:480–490. doi: 10.1097/00007632-199205000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Harms J, Melcher PM. Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine. 2001;26:2467–2471. doi: 10.1097/00007632-200111150-00014. [DOI] [PubMed] [Google Scholar]


