Abstract
Background
Surgical sphincterotomy for chronic anal fissure can cause fecal incontinence. This has led to the investigation of nonsurgical treatment options that avoid permanent damage to the internal anal sphincter.
Methods
We conducted a retrospective, ongoing chart review with telephone follow-up of 88 patients treated for chronic anal fissure between November 1996 and December 2002. During the first half of the study period, patients were treated with topical nitroglycerin and pneumatic dilatation. With the availability of new therapies in June 1999, subsequent patients received topical nifedipine and botulinum toxin injections (30–100 units). Lateral anal sphincterotomy was reserved for patients who failed medical treatment.
Results
In 98% of patients the fissure healed with conservative nonsurgical treatment. The combination of nifedipine and botulinum toxin was superior to nitroglycerin and pneumatic dilatation with respect to both healing (94% v. 71%, p < 0.05) and recurrence rate (2% v. 27%, p < 0.01). There was no statistical difference between the number of dilatations and botulinum toxin injections needed to achieve healing. Three patients who received botulinum toxin reported mild transient flatus incontinence. At an average telephone follow-up of 27 months, 92% of patients reported having no pain or only mild occasional pain with bowel movements.
Conclusions
Chronic anal fissures can be simply and effectively treated medically without the risk of incontinence associated with sphincterotomy. Topical nifedipine and botulinum toxin injections are an excellent combination, associated with a low recurrence rate and minimal side effects.
Abstract
Contexte
La sphinctérotomie chirurgicale pour traiter la fissure anale chronique peut causer de l'incontinence fécale, et c'est pourquoi on a étudié des traitements non chirurgicaux possibles qui évitent de causer des dommages permanents au sphincter anal interne.
Méthodes
Nous avons procédé à une étude rétrospective et continue de dossiers et à un suivi téléphonique auprès de 88 patients traités contre une fissure anale chronique entre novembre 1996 et décembre 2002. Au cours de la première moitié de la période d'étude, on a traité les patients avec de la nitroglycérine topique et par dilatation pneumatique. Comme de nouvelles thérapies étaient disponibles en juin 1999, les patients suivants ont reçu de la nifédipine topique et des injections de toxine botulinique (30 à 100 unités). On a réservé la sphinctérotomie anale latérale aux patients chez lesquels le traitement médical a échoué.
Résultats
Chez 98 % des patients, la fissure a guéri avec un traitement non chirurgical conservateur. La combinaison nifédipine et toxine botulinique s'est révélée supérieure à la nitroglycérine et à la dilatation pneumatique sur les plans à la fois de la guérison (94 % c. 71 %, p < 0,05) et du taux de récidive (2 % c. 27 %, p < 0,01). Il n'y avait pas de différence statistique entre le nombre de dilatations et d'injections de toxine botulinique nécessaires pour produire la guérison. Trois patients qui ont reçu la toxine botulinique ont signalé une incontinence transitoire bénigne à la flatuosité. Un suivi téléphonique moyen de 27 mois a révélé que 92 % des patients n'avaient pas de douleur ou avaient une douleur occasionnelle légère seulement causée par les selles.
Conclusions
Il est possible de traiter efficacement et simplement par des interventions médicales les fissures anales chroniques sans risquer l'incontinence associée à la sphinctérotomie. La nifédipine topique et les injections de toxine botulinique constituent une excellente combinaison qui produit un faible taux de récidive et des effets secondaires minimes.
Chronic anal fissure is a common benign anorectal condition that causes significant morbidity. Symptoms consist primarily of pain and bleeding during defecation. Fissures are predominantly located in the posterior midline, but 25% of women and 8% of men have anterior fissures.1 Multiple or other locations around the anal canal should raise the clinician's suspicion of inflammatory bowel disease, tuberculosis, leukemia, syphilis or infection with HIV.
It is generally accepted that the chronicity of anal fissures is the result of poor anodermal perfusion, especially at the posterior commissure. Local ischemia is likely a function of elevated resting anal pressures commonly associated with fissures, acting on an area that has inherently poor vascular supply. Treatments thus aim to lower resting sphincter pressures to increase perfusion and to promote wound healing.
Chronic anal fissures have traditionally been managed with lateral internal sphincterotomy or anal dilatation. Sphincterotomy, however, has been associated with incontinence in up to 35% of patients.2 Furthermore, this does not take into account normal weakening of the sphincter with age as well as the possibility of future anorectal surgery or obstetrical trauma. The risk of incontinence therefore is lifelong, to an often young, otherwise healthy person. Dilatation of the anal canal has also been associated with sphincteric tears and subsequent incontinence. Controlled pneumatic dilatation, however, is a variation to the technique that may reduce the risk of sphincter injury.
More recently, less invasive strategies have been adopted to induce sphincter relaxation. Topical agents including nitroglycerin, diltiazem hydrochloride or nifedipine, reduce internal sphincter pressures, resulting in a temporary or „medical sphincterotomy” until the fissure heals. Botulinum toxin injected into the internal sphincter also causes a reversible sphincterotomy and is gaining increasing popularity for the treatment of anal fissures.
With so many potentially conservative options, we investigated the roles of various nonsurgical modalities in the treatment of chronic anal fissure at our institution through a retrospective, ongoing chart review with telephone follow-up.
Methods
All patients referred to the senior author (J.B.F.) between November 1996 and December 2002 for a chronic anal fissure were included in the study. We defined chronic anal fissure as an ulcer with indurated edges and exposure of the horizontal fibres of the internal anal sphincter. Typical symptoms were present for at least 2 months. Data extracted from patient charts related to age, sex, clinic visits, treatments and procedures, healing of fissures, complications, recurrence and incontinence.
At the first clinic visit, all patients received an information pamphlet on chronic anal fissures and fibre supplementation. From November 1996 to June 1999, patients were initially treated with topical 0.2% nitroglycerin applied 3 times daily. The addition of controlled pneumatic dilatation was used for patients with persistent pain (nitroglycerin–dilatation [NT-D] group). In June 1999, topical nifedipine and botulinum toxin became available for the management of anal fissures at the Ottawa Hospital. Treatment thereafter changed to topical 0.2% nifedipine applied 3 times daily and botulinum toxin injections when pain continued to be a troublesome symptom (nifedipine–botulinum toxin [NF-B] group).
Pneumatic dilatation (Microvasive Rigiflex Rectosigmoid Dilator #5136; Boston Scientific, Boston, Mass.) was performed under perineal block and conscious sedation with the patient in the left lateral decubitus position. Balloon pressures were sustained at 40 psi for 45–120 seconds, depending on the clinical history relating to continence. Botulinum toxin (Botox A; Allergan, Markham, Ont.) was injected into the internal anal sphincter after application of a topical anesthetic. Equal doses were injected on both sides of the fissure for total doses ranging from 30 to 100 units.
Telephone follow-up involved informed verbal consent and a standardized questionnaire. Patients were asked about presence of pain, incontinence to flatus or stool and whether other physicians were consulted to treat their fissures. The study was reviewed and approved by an ethics committee.
Differences in the demographic variables (age and sex) between treatment groups were examined by the t and χ2 tests, respectively. The associations between treatment regimen and healing outcomes (overall, without recurrence and with single v. multiple treatments) were examined by Fisher's exact test because of small cell sample sizes. Fisher's exact test was also used to examine the relationship between treatment and fissure recurrence. Exact p values are reported and associations are considered significant at the p < 0.05 level. All analyses were conducted using SAS 8.2 (Cary, NC). Odds ratios and 95% confidence limits were constructed for all associations.
Results
Eighty-eight patients (41 females, 47 males) made up the study group. The mean age was 43 (standard deviation [SD] 12). Treatment modalities, healing and recurrences are schematically represented in Fig. 1.

FIG. 1. Schematic representation of study data including patient treatments, healing and recurrences. NT-D = nitroglycerin and dilatation, NF-B = nifedipine and botulinum toxin.
From November 1996 to June 1999, 31 patients were treated with topical nitroglycerin. Of these, 10 (32%) healed with nitroglycerin alone, whereas 21 also required pneumatic dilatation. This resulted in healing of the fissure in 15 (71%) of 21 patients. Four of the 6 patients in whom dilatation failed were successfully treated with botulinum toxin injections when it became available. The 2 remaining patients had surgical sphincterotomy. In 1 patient both dilatation and botulinum toxin injections failed, and the other had 3 failed trials of dilatation at a time when botulinum toxin was not available.
From June 1999 to December 2002, 57 patients were treated initially with topical nifedipine. Of these, 7 (12%) had healing of their fissure with nifedipine alone whereas 50 also received botulinum toxin injections. Of these 50 patients, 47 (94%) had healing of their fissure with the addition of botulinum toxin injections. Two patients whose injections failed were successfully treated with pneumatic dilatation. The other patient sought medical treatment at another hospital and had healing of the fissure with nonsurgical treatment.
Overall, fissures healed in 86 (98%) of 88 patients without surgical sphincterotomy.
Six recurrences were documented during the study period after complete healing. Four of the 6 recurrences occurred in the NT-D group (recurrence rate 4 of 15, 27%) and 1 from the NF-B group (recurrence rate 1 of 47, 2%). The sixth recurrence occurred in a patient who had healing with nitroglycerin alone. Of the 6 recurrences, 4 had rehealing with further medical treatment, and 2 required sphincterotomy.
Statistical analysis to compare the NT-D and NF-B groups revealed no significant difference with respect to age and sex (Table 1). The mean ages were 41 (SD 10) and 45 (SD 13) for NT-D and NF-B, respectively. The NF-B group had a significantly higher healing rate (94% v. 71%, p < 0.05) and lower recurrence rate (2% v. 27%, p < 0.01). Furthermore patients in the NF-B group were more than 10 times as likely to have both healing of their fissure and nonrecurrence (95% confidence interval [CI] for OR 2.76–39.65).
Table 1
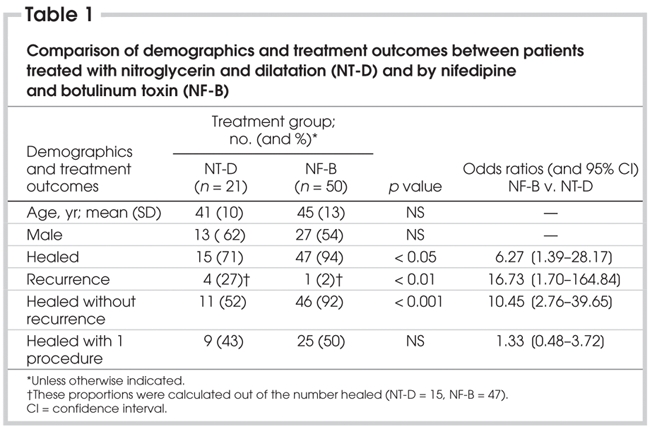
There was no statistical difference between the number of dilatations and botulinum toxin injections required to achieve healing. Among the 15 patients who had healing with pneumatic dilatation, 9 (60%) needed only 1 dilatation whereas the remainder (40%) required 2 dilatations. Botulinum toxin yielded comparable results. Of the 47 patients successfully treated with botulinum toxin, 25 (53%) had 1 injection, 18 (38%) had 2 injections and 4 (9%) had 3 injections.
Telephone follow-up was attempted in all patients. Contact was successful in 78 (89%) of 88 patients, but 2 chose not to participate in the study. The 12 patients who did not complete the follow-up questionnaire comprised 6 who were treated with only nifedipine or nitroglycerin (2 and 4, respectively), 3 in the NT-D group and 3 in the NF-B group. At follow-up, an average of 27 months since the last clinic visit, the majority of patients (92%) reported having no pain or only mild occasional pain with bowel movements. The remainder had no change in pain. No patient reported having an increase in pain. All but 1 patient (already mentioned) confirmed that they had not consulted another physician or received other treatment for their fissure. Three cases of transient flatus incontinence were documented.
Discussion
The standard management of chronic anal fissure with lateral internal sphincterotomy has recently been challenged with nonsurgical alternatives. These new modalities have gained popularity since they are not associated with irreversible damage or deformity to the internal anal sphincter. Although surgical sphincterotomy achieves a high rate of healing, incontinence to either flatus or feces, up to 35% and 5.3% respectively, has been reported.2 Patients affected by anal fissures are often young, and there is some concern regarding long-term incontinence rates after sphincterotomy. Normal weakening of the sphincter with age and the possibility of future anorectal procedures, obstetrical trauma or radiation may contribute to an even higher rate of incontinence later in life on an already compromised sphincter.
Dilatation of the anal canal has also long been used to treat chronic anal fissure with generally good results. However, dilatation may also result in sphincter tears and incontinence. In one study, sphincter defects were detected by endoanal ultrasonography in 13 (65%) of 20 patients who had undergone dilatation.3 Likely, it is the uncontrolled nature and poorly standardized techniques of anal dilatation that are mainly responsible for sphincter damage. In response to this, variations to the procedure have been developed. Pneumatic dilatation utilizes a balloon that is inflated in a controlled fashion to a standard pressure for a fixed duration of time. Sohn and colleagues4 used a 40-mm rectosigmoid balloon inflated to 20 psi for 5 minutes. They achieved a 94% healing rate. Although follow-up was short, there were no cases of incontinence. Balloon dilatation was well tolerated in our patients using a similar technique but with a perineal block, and there were no instances of flatus or fecal incontinence. The role of controlled balloon dilatation in chronic anal fissures and risk of incontinence have yet to be clarified.
Nitoglycerin ointment, a nitric oxide donor, improves anodermal perfusion and lowers elevated resting pressures. Although Lund and Scholefield5 reported healing in 68% of patients using glyceryl trinitrate for 8 weeks, a more recent study demonstrated much lower healing rates of 30% at 6 weeks.6 Its efficacy is limited by side effects, of which the most important is headache, occurring in up to 72% of patients.7 Nifedipine, a calcium channel blocker, has also been used in topical ointment form to reduce sphincter hypertonia and promote fissure healing. Perrotti and colleagues8 reported that fissures healed with topical nifedipine in 94% of patients while documenting a decrease in resting sphincter pressures. No systemic side effects were reported. Recently, nifedipine was found to be significantly superior to glyceryl trinitrate with respect to both healing (89% v. 58%) and side effects (5% v. 40%).9
The healing rates in our study for topical nitroglycerin and nifedipine were 32% and 12%, respectively. Our values are not accurate indicators of these agents' effectiveness as monotherapy since a full trial of 6–8 weeks was almost never completed. Instead, because of persistent pain, patients received either pneumatic dilatation or botulinum toxin injections, sometimes within a week of starting the topical agent. Therefore, healing rates for nitroglycerin or nifedipine as solitary modalities were not included in the statistical analysis. Instead, we compared the combination of NT-D versus NF-B. But although headaches were a common complaint from patients applying nitroglycerin ointment, nifedipine was well tolerated in our study without side effects.
Botulinum toxin is a potent inhibitor of acetylcholine release from presynaptic nerve terminals. Brisinda and associates10 found it to be more effective than topical glyceryl trinitrate (96% v. 60% healing rates). Although the optimal dose of botulinum toxin has not been established, it has been suggested that greater doses can produce higher success rates with minimal increases in side effects.11 Indeed, doses of 100 units, given up to 3 times, were found to be effective and safe in our study. Similar to rates in the literature, our patients who received botulinum toxin had a 6% rate of incontinence (3 of 50 patients); all were mild flatus incontinence that resolved within 2–3 months. In keeping with other studies,12 we also found no association of incontinence with the dosage of botulinum toxin injections. There were no other side effects or complications from the injections. Moreover, we noted no statistical difference between the number of dilatations or injections needed to achieve healing. From the patient's perspective, the minimal time of a single injection of botulinum toxin can reduce pain and sphincter hypertonia for up to 4 months and is well tolerated with the use of only topical anesthetic.
In the present study, 98% of patients presenting with a chronic anal fissure were successfully cured medically, avoiding the potential risk of permanent sphincter damage associated with surgery. In only 2 patients did a combination medical treatment fail to heal the fissure and they required sphincterotomy. In regard to recurrence, however, 2 of 6 patients did not respond to further nonsurgical modalities and required sphincterotomy. We recommend that lateral anal sphincterotomy be reserved for the minority of patients with fissures or fissure recurrences refractory to current medical therapy. Telephone follow-up at an average of 27 months confirmed symptomatic healing in 92% of patients, who reported having no pain or only mild occasional pain with bowel movements.
It has recently been suggested that combination therapy may be more effective than single agents in the treatment of chronic anal fissures.13 By acting through different mechanisms of action simultaneously, 2 agents may elicit a greater reduction in sphincter hypertonia, which may in turn allow more effective fissure healing. To our knowledge, this is the only study comparing 2 combination regimens for the management of anal fissures. The combination of topical nifedipine and botulinum toxin was significantly superior to nitroglycerin and dilatation (healing and recurrence rate of 94% and 2% v. 71% and 27%, respectively). Only a few studies using botulinum toxin injections as monotherapy report such high rates of healing,10 and recurrence rates have been as high as 41%.14 Unfortunately, because this study is retrospective, it is uncertain whether these high healing and low recurrence rates were due to the added effect of topical nifedipine or higher doses of botulinum toxin (100 units), or both.
This study confirms that most chronic anal fissures can be successfully treated nonsurgically without risk of permanent damage to the internal sphincter. Various combination therapies, which may be superior to monotherapy regimens, need further investigation. The combination of topical nifedipine and botulinum toxin injections used in our study was highly effective and associated with low recurrence rates and virtually no side effects.
Abstract presented at the Canadian Surgery Forum, London, Ont., Sept. 20, 2002.
Competing interests: None declared.
Correspondence to: Dr. Philippe Tranqui, 76 Springfield Rd., Ottawa ON K1M 1C7; fax 613 741-8998; ptranqui@hotmail.com
References
- 1.Hananel N, Gordon PH. Re-examination of clinical manifestations and response to therapy of fissure-in-ano. Dis Colon Rectum 1997;40:229-33. [DOI] [PubMed]
- 2.Khubchandani IT, Reed JF. Sequelae of internal sphincterotomy for chronic fissure in ano. Br J Surg 1989;76:431-4. [DOI] [PubMed]
- 3.Nielsen MB, Rasmussen OO, Pedersen JF, Christiansen J. Risk of sphincter damage and anal incontinence after anal dilatation for fissure-in-ano. An endosonographic study. Dis Colon Rectum 1993;36:677-80. [DOI] [PubMed]
- 4.Sohn N, Eisenberg MM, Weinstein MA, Lugo RN, Ader J. Precise anorectal sphincter dilatation — its role in the therapy of anal fissures. Dis Colon Rectum 1992;35:322-7. [DOI] [PubMed]
- 5.Lund JN, Scholefield JH. A randomised, prospective, double-blind, placebo-controlled trial of glyceryl trinitrate ointment in treatment of anal fissure. Lancet 1997;349:11-4. [DOI] [PubMed]
- 6.Richard CS, Gregoire R, Plewes EA, Silverman R, Burul C, Buie D, et al. Internal sphincterotomy is superior to topical nitroglycerin in the treatment of chronic anal fissure: results of a randomized, controlled trial by the Canadian Colorectal Surgical Trials Group. Dis Colon Rectum 2000;43:1048-57. [DOI] [PubMed]
- 7.Carapeti EA, Kamm MA, McDonald PJ, Chadwick SJ, Melville D, Phillips RK. Randomised controlled trial shows that glyceryl trinitrate heals anal fissures, higher doses are not more effective, and there is a high recurrence rate. Gut 1999;44:727-30. [DOI] [PMC free article] [PubMed]
- 8.Perrotti P, Bove A, Antropoli C, Molino D, Antropoli M, Balzano A, et al. Topical nifedipine with lidocaine ointment vs. active control for treatment of chronic anal fissure: results of a prospective, randomized, double-blind study. Dis Colon Rectum 2002;45:1468-75. [DOI] [PubMed]
- 9.Ezri T, Susmallian S. Topical nifedipine vs. topical glyceryl trinitrate for treatment of chronic anal fissure. Dis Colon Rectum 2003;46:805-8. [DOI] [PubMed]
- 10.Brisinda G, Maria G, Bentivoglio AR, Cassetta E, Gui D, Albanese A. A comparison of injections of botulinum toxin and topical nitroglycerin ointment for the treatment of chronic anal fissure. N Engl J Med 1999;341:65-9. [DOI] [PubMed]
- 11.Brisinda G, Maria G, Sganga G, Bentivoglio AR, Albanese A, Castagnet M. Effectiveness of higher doses of botulinum toxin to induce healing in patients with chronic anal fissures. Surgery 2002;131:179-84. [DOI] [PubMed]
- 12.Minguez M, Melo F, Espi A, Garcia-Granero E, Mora F, Lledo S, et al. Therapeutic effects of different doses of botulinum toxin in chronic anal fissure. Dis Colon Rectum 1999;42:1016-21. [DOI] [PubMed]
- 13.Lysy J, Israelit-Yatzkan Y, Sestiery-Ittah M, Weksler-Zangen S, Keret D, Goldin E. Topical nitrates potentiate the effect of botulinum toxin in the treatment of patients with refractory anal fissure. Gut 2001;48:221-4. [DOI] [PMC free article] [PubMed]
- 14.Minguez M, Herreros B, Espi A, Garcia-Granero E, Sanchiz V, Mora F, et al. Long-term follow-up (42 months) of chronic anal fissure after healing with botulinum toxin. Gastroenterology 2002;123:112-7. [DOI] [PubMed]


