Abstract
Background
War injury is a public health problem that warrants global attention. This study aims to determine the burden of injury during a complex emergency in sub-Saharan Africa.
Methods
To determine the magnitude, causes, distribution, risk factors and cumulative burden of injury in a population experiencing armed conflict in northern Uganda since 1986 and to evaluate the living conditions and access to care for injury victims, we took a multistage, stratified, random sampling from the Gulu district to determine the rates of injury from 1994 to 1999. The Gulu district is endemic for malaria, tuberculosis, HIV and malnutrition and has a high maternal death rate. It is 1 of 3 districts in northern Uganda affected by war since 1986. The study participants included 8595 people from 1475 households. Of these, 73.0% lived in temporary housing, 46.0% were internally displaced and 81.0% were under 35 years of age. Trained interviewers administered a 3-part household survey in the local language. Quantitative data on injury, household environment, health care and demography were analyzed. Qualitative data from part 3 of the survey will be reported elsewhere. A similar rural district (Mukono) not affected by war was used for comparison. We studied injury risk factors, mortality and disability rates, accumulated deaths, access to care and living conditions.
Results
Of the study population, 14% were injured annually: gunshot injuries were the leading cause of death. The annual death rate from war injury was 7.8/1000 (95% confidence interval [CI] 7.0–8.5) and the disability rate was 11.3/1000 (95% CI 10.4–12.2). The annual excess injury mortality was 6.85/1000. Only 4.5% of the injured were combatants. Fifty percent of the injured received first aid, but only 13.0% of those who died reached hospital. The injury mortality in Gulu was 8.35-fold greater than that for Mukono.
Conclusions
The crisis in Gulu can be considered a complex political emergency. Protracted conflicts should not be ignored because of a low rate of injury death since the cumulative total is high. Political emergencies should be monitored, and when the mortality exceeds 3.5%, international intervention is indicated. The international and national failings of this protracted conflict should be critically analyzed so that such political emergencies can be prevented or terminated.
Abstract
Contexte
Les blessures de guerre constituent un problème de santé publique qui justifie une attention mondiale. Cette étude vise à déterminer le fardeau des traumatismes au cours d'une urgence complexe en Afrique subsaharienne.
Méthodes
Afin de déterminer l'ordre de grandeur, les causes, la distribution, les facteurs de risque et le fardeau cumulatif des blessures dans une population aux prises avec un conflit armé dans le nord de l'Ouganda depuis 1986 et d'évaluer les conditions de vie et l'accès aux soins pour les victimes de blessures, nous avons procédé à un échantillonnage aléatoire, stratifié et multistades dans le district de Gulu pour déterminer les taux de blessures de 1994 à 1999. Le paludisme, la tuberculose, le VIH et la malnutrition y sont endémiques et le taux de mortalité maternelle y est élevé. Il s'agit de l'un des trois districts du nord de l'Ouganda où sévit la guerre. Les participants à l'étude comprenaient 8595 personnes de 1475 ménages, dont 73,0 % vivaient dans des logements temporaires, 46,0 % étaient des personnes déplacées à l'intérieur de leur pays et 81,0 % avaient moins de 35 ans. Des intervieweurs dûment formés ont administré un sondage domestique en trois volets dans la langue locale. On a analysé des données quantitatives sur les blessures, l'environnement domestique, les soins de santé et la démographie. Les données qualitatives du volet 3 de l'enquête feront l'objet d'un autre rapport. On a utilisé pour la comparaison un district rural (Mukono) semblable non touché par la guerre. Nous avons étudié les facteurs de risque de blessure, les taux de mortalité et d'invalidité, les décès cumulatifs, l'accès aux soins et les conditions de vie.
Résultats
Sur les membres de la population étudiée, 14 % étaient victimes d'une blessure chaque année : les blessures par balle étaient la principale cause de mortalité. Le taux annuel de mortalité attribuable à des blessures de guerre s'établissait à 7,75/1000 (intervalle de confiance [IC] à 95 %, 7,0–8,5) et le taux d'invalidité, à 11,3/1000 (IC à 95 %, 10,4–12,2). Le taux annuel de mortalité excessive attribuable aux blessures s'établissait à 6,8/1000. Seulement 4,5 % des blessés étaient des combattants. Cinquante pour cent des blessés ont reçu des premiers soins, mais 13,0 % seulement de ceux qui sont morts sont parvenus à l'hôpital. Le taux de mortalité attribuable aux blessures dans le district de Gulu était 8,35 fois plus élevé que dans celui de Mukono.
Conclusions
On peut considérer la crise dans le district de Gulu comme une urgence politique complexe. Il ne faut pas oublier les conflits qui perdurent en raison d'un faible taux de mortalité attribuable aux blessures, puisque le total cumulatif est élevé. Il faut surveiller les urgences politiques et lorsque le taux de mortalité dépasse 3,5 %, une intervention internationale est indiquée. Il faudrait analyser de façon critique les défaillances internationales et nationales liées à ce conflit qui perdure afin de pouvoir prévenir de telles urgences politiques ou y mettre fin.
Armed conflict has been a major cause of ill health and death throughout history but has not received the same attention from public health practitioners and researchers as other causes of illness.1 Issues of violence and war began to be accepted as a public health problem only toward the end of the 20th century2 but has been projected to be the 8th most important cause of death by 2020.3 Genocide and mass violence perpetrated against vulnerable populations have been recommended as a legitimate area of inquiry for health professionals, as has the broader concept of complex emergencies.4,5,6
Complex emergencies are the result of failure in the political and diplomatic arenas, almost always include armed conflict and are characterized by the fact that prominent problems are unsolved. They are also associated with insecurity and population displacement. An increase in social spending with a decrease in military spending is one recommendation for preventing such emergencies.5 Complex emergencies by definition are associated with either a daily mortality of 1/10 000 people or a doubling of the baseline mortality. This mortality has been recommended as the threshold for international humanitarian intervention.6,7,8,9 „Silent emergencies” are complex emergencies that have been relatively ignored by the world political powers and mass media. The term „complex political emergencies” has been used to describe these crises when they are long term.6,10
There were an estimated 310 000 conflict-related deaths globally in 2000,1 whereas in 1990 the estimate was 502 000.11 These reports, although inconsistent, do agree that Africa contributes more to conflict-related deaths than any other region. The United Nations reported 21 neglected crises of which 17 were in Africa.12 The reduction of military conflict and the promotion of peace are requirements both for development and improved health in Africa.13,14 When the standard of care is acceptable, 3 people are permanently disabled for every injury death.15
There is extensive evidence on the indirect effects of war, and there are calls for evidence-based policy and practice. Research on injuries from firearms, landmines and interpersonal violence, the direct consequences of war, is insufficient.16 In a 1991 review it was noted that such research was dominated by military studies with little work done to evaluate the impact on noncombatants.17 A decade later, a similar review noted that there was limited information on the health consequences of conflict and called for better quantification. Household surveys using standardized data collection tools were recommended.1 The primary contribution of public health to the detection of violence is the assessment of bodily injury.5 In recent years, health professionals have organized to promote the protection of human health and respect for human rights.18 The Montreal Declaration19 asserts that people have a right to safety which must be guaranteed by government. Governments that cannot protect their people should request international assistance although this implies a national failure to provide for its citizens.5
Trauma, malnutrition and infectious disease are the most important public health risks during war.20,21 In low-income countries with pre existing malnutrition and low vaccination rates, infectious diseases are more prominent, whereas in middle-and high-income countries the proportion of trauma deaths is higher. During the conflict in Bosnia-Herzegovina trauma was the major cause of death,22 whereas in Somalia physical violence accounted for 13% of deaths and malnutrition for 41.3%.23 One of the few population-based studies of war-elated deaths was performed in Kosova in 1999. There, 64% of the total mortality (8.64/1000 annually) was due to trauma.24 During the 1994 civil war in Afghanistan, war-related trauma was the leading cause of death, with 43% (9.4/1000 annually) due to gunshots or rocket explosions.25 There are few reports of injury related deaths during war or civil conflict in Africa, and even the complex emergencies of Rwanda and Sierra Leone lack basic measurement.26 Evaluations conducted in eastern Congo (2000 and 2001) have reported millions of deaths, but the specific magnitude of violent deaths in that conflict is not clear.27
The proportion of civilian war-related deaths has increased from 19% in World War I, 48% in World War II, to more than 80% in the 1990s.13,17,20 Civilians are used as shields to protect the military, abducted, enslaved, tortured, raped and executed. They witness events that result in psychosocial problems that threaten long-term social stability.28 Civilians also suffer because of the destruction of hospitals, power facilities, communications, water purification facilities and sewage treatment plants.18,26 Large amounts of money are disbursed in response to complex emergencies, but there is little evaluation of the effectiveness of monetary aid and no studies on how aid influences the duration, magnitude and outcome of war.16 There is concern that humanitarian aid prolongs some conflicts.29
Uganda is situated in East Africa with the river Nile, several of its tributaries and 6 great lakes inside its boundaries. Half of Uganda's state budget is provided by external donors.30 Northern Uganda bordering the Sudan has been involved in civil conflict since 1986.31 More than 1 million people in 3 districts (Gulu 479 496, Pader 311 888 and Kitgum 284 635) are affected.32 The combatants in the conflict are the Uganda Peoples' Defence Force and the rebel Lord's Resistance Army. Military and diplomatic attempts at resolution have failed for 18 years because of politics, economics and crime.30,33
The study site, Gulu district, is endemic for malaria, tuberculosis and HIV, and suffered an outbreak of Ebola virus.34,35,36 Gulu district has high levels of chronic malnutrition (32%)37 and a maternal mortality that is 1.3 times the level in the rest of Uganda.38
No studies of the magnitude of injury have been reported for Gulu district. The difficulties of conducting injury surveillance during war have been documented,26 but we were fortunate to be able to conduct a household survey in the district during a peaceful interval in 1999. Previously, we reported the magnitude of injury in an urban division (Kawempe) and a rural district (Mukono) both in central Uganda, using the same methodology.39 In the urban study, the annual injury mortality was 2.2/1000 people, with the leading cause being traffic collisions. In the rural district the annual injury mortality was 0.9/1000 people, with the leading cause being drowning.39 The global annual injury mortality of 0.97/1000 is similar to the rate for rural Uganda.40
Methods
Sampling techniques
A 3-stage sampling procedure was used to identify households needed to generate the required sample. In stage 1, the 5 counties in Gulu district were included, with 1 subcounty randomly selected from each county. There was no weighting as the sample was proportional to the population of the county. In stage 2, we randomly selected 50% of the villages in each subcounty. In stage 3, interviewers started at the village meeting ground and selected households randomly, until the required sample size was realized. In every village, a minimum of 20 households was visited. The nearest household was used as a replacement in the rare occurrence of refusal or absence of respondents.
Sample size
Population estimates were obtained from the 1991 Population and Housing Census Report and adjusted for projected population growth.41 Adjustment for population displacement was not necessary since displacement between 1991 and 1999 was internal. Sample sizes were determined according to a formula for cross-sectional surveys, with a 95% confidence interval (CI).42 Based on results of the urban survey, we used an estimated injury mortality of 2.2/1000 persons annually to calculate the required sample size, allowing for a maximum error of +1.1/1000. The minimum sample was 7000.
Data collection, instruments and statistical methods
This survey in Gulu used the same methodology as that of a similar rural Ugandan district (Mukono) not in conflict. Permission and ethical clearance was obtained from the Ministry of Health, Gulu District. A household was defined on the basis of shared cooking. Residents in displacement camps were defined as displaced. The questionnaire had 3 sections. The first included household information: number of persons, type of dwelling, types of energy used and dates of births and deaths. A home made of mud was defined as temporary. The second section included demographic data on each member of the household and whether they had suffered an injury. Respondents were specifically asked about injury deaths in the household, and those that had occurred in the 5 years preceding the survey were included. The third section included detailed qualitative information about land-mine injuries. The respondent was the most responsible adult present in the household. After establishing rapport and securing consent, interviewers explained injury using local words. A list of common external causes was read to the respondents. Outcomes were classified into death, disability or full recovery from injury. Data collection on fatal injuries was restricted to 5 years, and for fully recovered injuries to 6 months. Current disabilities were determined, and prevalence was calculated using 1999 population projections. Classifications of causes of injury were derived from the International Statistical Classification of Diseases and Related Health Problems, 10th rev, except for the simplifications of „blunt force” and „cuts/stabs.” Translation and back translation was done from the original English version to Acholi, the local language. The translated form was piloted, and data collectors underwent rigorous training in interviewing techniques. The raw data were entered twice, and the analysis was repeated using Epi Info 6 and SPSS 10. Multivariate analysis was used to determine injury risk factors. The excess mortality for the Gulu district over the Mukono district was calculated using the mortality in Mukono district as the baseline.
Results
Demographic data
We surveyed 1475 households (8595 people). The average age was 20.8 (95% CI 20.4–21.2) years, 4246 (49.4%) were 15 years or younger and 6988 (81.3%) were under 35 years of age. Males accounted for 52% of the population. The average number of people per household was 5.8 (95% CI 5.7–5.9). Of the 1261 victims (killed, disabled or recovered), 579 (45.9%) were displaced civilians, 472 (37.4%) were nondisplaced civilians and 57 (4.5%) were military personnel. Almost half the injury victims were internally displaced citizens and more than three-quarters of the population were crowded into temporary shelters. Of those injured, the principal occupation was peasant farmer in 499 (39.6%), followed by student in 280 (22.2%) and housewife in 189 (15.0%). Male sex and increasing age were significantly associated with injury (Table 1). Occupation and combatant status were not significant risk factors. Of 1261 injured, excluding preschool children, 241 (19.1%) had no formal education, 736 (60.6%) had attended primary school, 212 (17.5%) had attended secondary school and 25 (2.0%) had postsecondary education.
Table 1
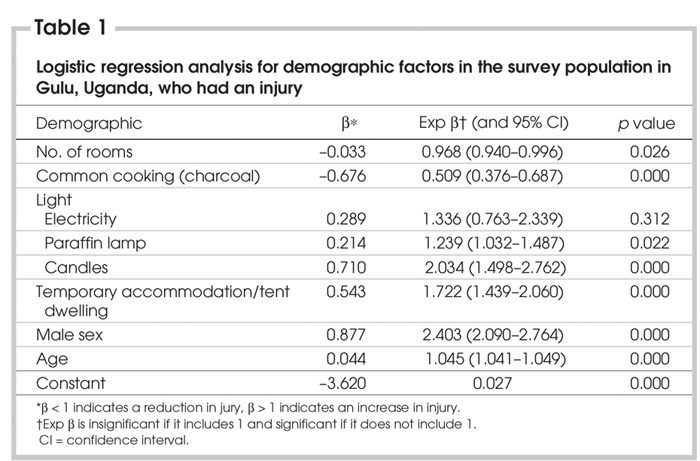
Household environment
Of the 1475 households surveyed 877 (59.4%) lived in homes with 1 or 2 rooms. Homes were classified as temporary for 1077 (73.0%) households and semipermanent for 324 (22.0%). Wood is the most common fuel for cooking, and electric lighting is uncommon; 1313 (89.0%) households cooked with wood and the rest used charcoal. Only 46 (3.1%) households had electricity. Fewer rooms and the use of charcoal were significantly related to injury as were the use of paraffin lamps and candles for lighting. Temporary housing was associated with increased injury. No protective relationship with the availability of electricity was defined; however, the number of homes with electricity was small (Table 1).
Injury cause and outcome
Summary rates of injury, death and disability, and recovered injury were determined as were the rates for specific external causes (Table 2). In the 5 years between 1994 and 1999, 397 fatal injuries occurred, an annual injury death rate of 7.8/1000 (95% CI 7.0–8.5) (835% higher than that in Mukono district, a similar Ugandan district that does not have armed conflict), and 579 disabilities occurred due to injury, giving an annual prevalence rate of 11.3/1000 (95% CI 10.4. In the 6 months preceding the survey, 1307 fully recovered injuries occurred giving an annual rate of minor injury of 25.5/1000. The prevalence of injury was 44.6/1000 per year (95% CI 43.0–46.13). The ratio of injury deaths to disabilities is about 1.5:1. The excess injury mortality in Gulu district over Mukono was 6.8/1000 annually.
Table 2
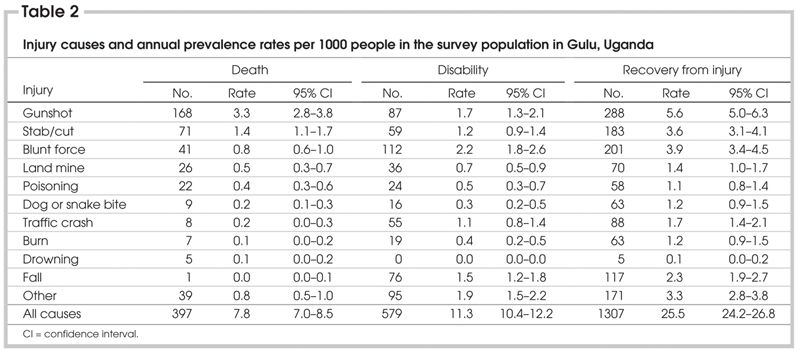
Gunshots were the leading cause of injury death and recovered injury. Stabs and cuts were the second leading cause of injury death and were not significantly different from gunshots, which were the second leading cause of injury disability. Blunt force was the primary cause of injury disability, the second leading cause of recovered injury and third as a cause of injury mortality. Land mines came in fourth as a cause of death and traffic collisions fourth as a cause of injury disability. Of the 397 injury deaths, 306 (77.1%) were due to gunshots, stabbings, blunt force and land mines, all of which are considered intentional violence. At least 63.2% of injuries associated with death, disablity and recovery were intentional.
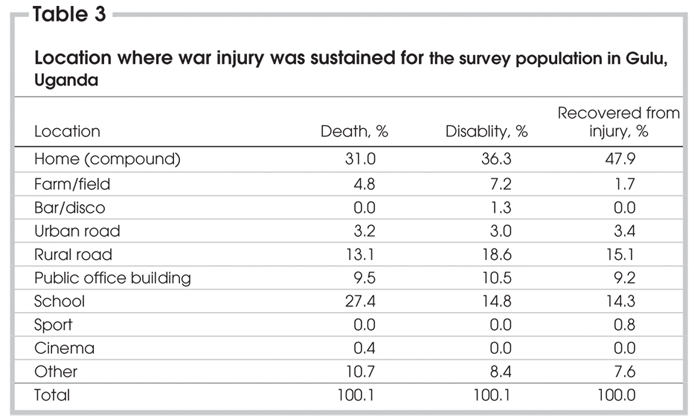
Site, care and social burden
The leading location of injury occurrence (Table 3) was the home, followed by schools, rural roads and public buildings. Just over 50% of all the injury victims received first aid. Of 384 fatally injured people, 252 (65.6%) died at the scene with only 50 (13.0%) surviving to reach hospital. Of 810 survivors who reached a health facility, 553 (68.3%) did so within 24 hours. Only 131 (16.2%) arrived within 1 hour. Only 65 (22.9%) of 284 amputees received a prosthesis. To finance care, families of the injured borrowed money in 446 (38%) 0f 1166 cases. Of 1201 injury victims, 216 (18.0%) returned to their previous work, 492 (41.0%) could do some work, but 486 (40.5%) were no longer able to work.
Table 3
Discussion
This study, which used a household survey to determine the burden of injury during war, is a unique response to the call for epidemiologic evaluation of war injury in Africa. The injury death rate for Gulu is similar to that reported for Kosovo in 1999 and Afghanistan in 1994. We have confirmed that the civilian population bears most of the burden of injury death in current conflicts. The people in Gulu have been experiencing war since 1986; many are internally displaced and most live in temporary housing. The majority, who are under 15 years of age, have never experienced peace. The most common sites for injury occurrence are homes, schools and public roads, so these people cannot safely carry out basic activities of daily living.
The ratio of 1.5 disabilities for each injury death in Gulu is half of that expected if there was adequate care. This ratio reflects the lack of accessibility to care of the injured in Gulu district. The majority of those who died of injury did not survive to receive treatment at a health institution. If basic clinical care had been available the deaths would have been fewer and the number of disabled survivors increased.
The economic implications to individual people are important as most survivors of injury could not return to their former employment. Family members had to interrupt their work and many borrowed money to provide care. Military intervention by the Ugandan government has resulted in reduced social spending nationally, a weak currency and has elevated the cost of living for all Ugandans.43 Social financing (50% of which is provided by donation from the West) has been diverted to the military. This is contrary to recommendations for the prevention of complex emergencies5 and means that aid to the Ugandan government by external donors has in part funded this conflict.
A limitation of this study is that household information is based on self-reporting, which makes misclassification possible. However, the methodology used is the same as in 2 peaceful districts of Uganda, making comparison to these studies unbiased. Survivor bias could not be determined, but if it was present it would result in an underestimate of the mortality. The 4.6% of the injured who are reported as combatants is likely an underestimate, as admission of rebel activity would put a household at risk. If 50% underreporting is postulated, the civilian death toll would still represent 90% of the injury burden in Gulu district. Mortality at 5 years was determined because our previous study39 found that this avoided recall bias.
The excess injury mortality of Gulu district over Mukono district was 6.8/1000 annually. The annual injury mortality of 7.8/1000 in Gulu district is 835% higher than that in Mukono district, which is similar economically and was war affected before 1986.
The overall picture for the Gulu population is one of deprivation, underdevelopment and vulnerability to disease, injury and famine. Complex emergencies have diverse presentations, and the prolonged low-intensity war, characterized by that in Gulu, is an example of this diversity. The injury, infectious disease, maternal mortality, population displacement, malnutrition and the prolonged conflict present in Gulu characterize the district as a complex political emergency.
The use of specific rates or changes in baseline rates neglects the importance of duration and therefore underestimates the magnitude of protracted conflicts. We propose that the excess mortality also be used to evaluate crises of long duration. Any threshold is arbitrary, but it would be hard to argue that the loss of 3.5% of the population is too low. The excess mortality due to injury in Gulu over Mukono, a district not in conflict, is 12.3%.
Although this study was conducted in Gulu district, it is valid to generalize the results to the neighbouring Pader and Kitgum districts, which are ethnically similar and have been affected by war for the same time period. The war in the 3 districts of northern Uganda, a total of 1 million Ugandans, has caused at least 100 000 injury deaths. These projections do not include the war-injury death toll in the bordering districts of Lira, Apach and Teso, which have been periodically affected by war.
War in low-income countries is associated with a higher mortality from infectious diseases than injury; therefore, it is likely that the excess deaths from infectious diseases due to war in northern Uganda is at least equal the injury total. The complex political emergency in northern Uganda has been going on for almost 2 decades. The end of the war would be the most important means of reversing economic and social underdevelopment and reducing the excess mortality. This would be good news, but every time in the past such hopes have been ill founded.
Formal monitoring by international bodies with no political or economic interest in a conflict should have been initiated in Uganda at least a decade ago. It is clear that the government has not been able to protect the people of the north. If there had been international intervention in 1991 when „only” 3.5% of the Gulu population had died due to war injury the present total of 12.3% might have been avoided.
The war in northern Uganda is not unusual, being only 1 of 17 such African conflicts. Independent analysis of the underlying causes prolonging this war is urgently required.44 The political, economic and criminal profiteering on both sides, and the collusion, unwittingly or otherwise, of external donors should be studied. Much has been learned about the national and international failings associated with the Rwandan genocide, and the war in northern Uganda should be subjected to similar scrutiny so that complex political emergencies can be prevented or more efficiently terminated.
Acknowlegements: We recognize the contributions of Dr. Christopher Orach to the translation of the survey instrument, Ms. Elizabeth Shaeffer and Shaghayegh (Natasha) Dehghan for library research, the support of the Canadian Network for International Surgery and the Injury Control Center Uganda and the funding of the Canadian International Development Agency.
Competing interests: None declared.
Correspondence to: Dr. Ronald R. Lett, 205–1037 West Broadway, Vancouver BC V6H 1E3; fax 604 739-4788; lett@cnis.ca
References
- 1.Murray CJ, King G, Lopez AD, Tomijima N, Krug EG. Armed conflict as a public health problem. BMJ 2002;324:346-9. [DOI] [PMC free article] [PubMed]
- 2.Winett LB. Constructing violence as a public health problem. Public Health Rep 1998;113:498-507. [PMC free article] [PubMed]
- 3.World Health Organization (WHO). World report on violence and health. Geneva: WHO; 2002.
- 4.Willis BM, Levy BS. Recognizing the public health impact of genocide. JAMA 2000;284:612-4. [DOI] [PubMed]
- 5.Gellert GA. Humanitarian responses to mass violence perpetrated against vulnerable populations. BMJ 1995;311:995-1001. [DOI] [PMC free article] [PubMed]
- 6.Waldman R, Martone G. Public health and complex emergencies: new issues, new conditions. Am J Public Health 1999;89: 1483-5. [DOI] [PMC free article] [PubMed]
- 7.Toole MJ, Waldman RJ. Prevention of excess mortality in refugee and displaced populations in developing countries. JAMA 1990;263:3296-302. [PubMed]
- 8.Burkholder BT, Spiegel P, Salama P. Methods of determining mortality in the mass displacement and return of emergency-affected populations in Kosovo, 1998–99. In: Reed HE, Keely CB, editors. Forced migration and mortality. Washington: National Academies Press; 2001. Available: www.nap.edu/books/0309073340/html/86.html (accessed 2005 Sept 26).
- 9.Toole MJ. Mass population displacement. A global public health challenge. Infect Dis Clin North Am 1995;9:353-66. [PubMed]
- 10.Sandorp E, Zwi AB. Complex political emergencies. BMJ 2002:324:310-1. [DOI] [PMC free article] [PubMed]
- 11.Reza A, Mercy JA, Krug E. Epidemiology of violent deaths in the world. Inj Prev 2001;7:104-11. [DOI] [PMC free article] [PubMed]
- 12.Forgotten disasters. A United Nations appeal. Economist (US) 2003;369(8351):46.
- 13.Elmore-Meegan M, O'Riorden T. Africa on the precipice. An ominous but not yet hopeless future. JAMA 1993;270:629-31. [DOI] [PubMed]
- 14.Comninellis N. War and health — a view of Africa. Trop Doct 1994;24:1-3. [DOI] [PubMed]
- 15.Trunkey DD. Trauma — a public health problem. In: Moore EE, editor. Early care of the injured patient. Toronto: BC Decker; 1990. p. 3-11.
- 16.Banatvala N, Zwi AB. Public health and humanitarian interventions: developing the evidence base. BMJ 2000;321:101-5. [DOI] [PMC free article] [PubMed]
- 17.Garfield RM, Neugut AI. Epidemiologic analysis of warfare: a historic review. JAMA 1991;266:688-92. [PubMed]
- 18.Geiger HJ, Cook-Deegan RM. The role of physicians in conflicts and humanitarian crises. Case studies from the field missions of Physicians for Human Rights. JAMA 1993;270:616-20. [PubMed]
- 19.Mitka M. WHO declares the individual's right to be safe. JAMA 2002;288:305-6. [PubMed]
- 20.Aboutanos MB, Baker SP. Wartime civilian injuries: epidemiology and intervention strategies. J Trauma 1997;43:719-26. [DOI] [PubMed]
- 21.Brennan RJ, Burkle FM, Burkholder BT, Lilibridge SR. Wartime civilian injuries: epidemiology and intervention strategies [letter]. J Trauma 1998;45:175-6. [DOI] [PubMed]
- 22.Centers for Disease Control and Prevention (CDC). Status of public health —Bosnia and Herzegovina, August–September 1993. MMWR Morb Mortal Wkly Rep 1993;42:973, 979-82. [PubMed]
- 23.Manoncourt S, Doppler B, Enten F, Nur AE, Mohamed AO, Vial P, et al. Public health consequences of the civil war in Somalia. Lancet 1992;340:176-7. [DOI] [PubMed]
- 24.Spiegel PB, Salama P. War and mortality in Kosovo, 1998–99: epidemiological testimony. Lancet 2000;355:2204-9. [DOI] [PubMed]
- 25.Gessner BD. Mortality rates, causes of death, and health status among displaced and resident populations of Kabul, Afghanistan. JAMA 1994;272: 382-5. [PubMed]
- 26.Weinberg J, Simmonds S. Public health, epidemiology and war. Soc Sci Med 1995;40:1663-9. [DOI] [PubMed]
- 27.IRC. Mortality in eastern republic of Congo: results from eleven mortality surveys. Final draft 2001. Prepared by L. Roberts, IRC Health Unit. Available: www.grandslacs.net/doc/3741.pdf (accessed 2005 Nov. 15).
- 28.de Jong K, Mulhern M, Ford N, van der Kam S, Kleber R. The trauma of war in Sierra Leone. Lancet 2000;355:2067-8. [DOI] [PubMed]
- 29.Sondorp E, Kaiser T, Zwi A. Beyond emergency care: challenges to health planning in complex emergencies. Trop Med Int Health 2001;6:965-73. [DOI] [PubMed]
- 30.Tangi R, Mwenge A. Military corruption and Ugandan politics since the late 1990's. Rev Afr Polit Econ 2004;98:365-78.
- 31.Omona G, Matheson KE. Uganda: stolen children, stolen lives. Lancet 1998;351:442. [DOI] [PubMed]
- 32.Wakike A. Buganda gets fewest kids: northern population grows most, Buganda least. Sunday Vision 2002 Oct. 6;11:40.
- 33.Okello L. Protracted conflict, elusive peace: initiatives to end the violence in northern Uganda. Conciliation Resources Accord 2002;11. Available: www.c-r.org/accord/uganda/accord11/index.shtml (accessed 2005 Sept 26).
- 34.Francesconi P, Fabiani M, Dente MG, Lukwiya M, Okwey R, Ouma J, et al. HIV, malaria parasites, and acute febrile episodes in Ugandan adults: a case-control study. AIDS 2001;15:2445-50. [DOI] [PubMed]
- 35.Accorsi S, Fabiani M, Lukwiya M, Onek PA, Mattei PD, Declich S, et al. The increasing burden of infectious diseases on hospital services at St. Mary's Hospital Lacor, Gulu, Uganda. Am J Trop Med Hyg 2001;64:154-8. [DOI] [PubMed]
- 36.Okware SI, Omaswa FG, Zaramba S, Opio A, Lutwama JJ, Kamugisha J, et al. An outbreak of ebola in Uganda. Trop Med Int Health 2002;7:1068-75. [DOI] [PubMed]
- 37.Uganda Monthly Report. High malnutrition rates in Gulu camps. USAID Famine Early Warning System Network; 2003 Feb 27. Available: www.fews.net/centers/innerSections.aspx?f=ug&m=1000832&pageID=monthliesDoc (accessed 2005 Sept 26).
- 38.Orach CG. Maternal mortality estimated using the sisterhood method in Gulu district, Uganda. Trop Doct 2000;30:72-4. [DOI] [PubMed]
- 39.Kobusingye O, Guwatudde D, Lett R. Injury patterns in rural and urban Uganda. Inj Prev 2001;7:46-50. [DOI] [PMC free article] [PubMed]
- 40.Krug EG, Gyanendra SK, Lozana R. The global burden of injuries. Am J Public Health 2000;90:523-6. [DOI] [PMC free article] [PubMed]
- 41.Louis MR, Richard AP. Designing and conducting survey research: a comprehensive guide. 2nd ed. San Francisco: Jossey-Bass Publishers; 1997.
- 42.Kish L. Survey sampling. New York: John Wiley & Sons; 1965.
- 43.Mulumga B. Will shilling keep falling? The Monitor (Kampala) 2003 Mar 19. 4. Stewart F. Root causes of violent conflict in developing countries. BMJ 2002;324:342-5. [DOI] [PMC free article] [PubMed]
- 44.Stewart F. Root causes of violent conflict in developing countries. BMJ 2002;324:342-5. [DOI] [PMC free article] [PubMed]


