Abstract
Background
Observation and repeated examination may lead to favourable clinical outcomes in the ever-challenging diagnosis of appendicitis. The goal of this study was to evaluate clinical performance in the diagnosis of suspected appendicitis in a centre with limited access to medical imaging technologies and to identify factors associated with complicated cases.
Methods
A retrospective review of the medical records of 211 consecutive surgical cases of suspected appendicitis, spanning an 11-year period, was performed. The delays before treatment and the subsequent patient outcomes were evaluated.
Results
There were 8.1% of cases with negative findings on appendectomy, 75.8% with uncomplicated appendicitis, 12.3% with complicated appendicitis and 3.8% with other surgical conditions. The delay before the first medical consultation was significantly longer in patients with complicated appendicitis. The various delays after the first medical consultation did not differ significantly between the groups.
Conclusions
In the context of limited available medical imaging modalities, clinical observation was not associated with an increased incidence of complicated appendicitis. The presence of complicated appendicitis was associated with the delay before the patient's first medical consultation. Clinical judgment can be prioritized and can lead to good clinical performance in the management of patients with suspected appendicitis, with no significant increase in rates of complicated appendicitis and negative findings on appendectomy.
Abstract
Contexte
L'observation et les examens répétés peuvent produire des résultats cliniques favorables lorsqu'il s'agit du diagnostic, toujours difficile, de l'appendicite. Cette étude visait à évaluer le rendement clinique du diagnostic d'appendicite soupçonnée dans un centre ayant un accès limité à des technologies d'imagerie médicale, et à définir les facteurs associés aux cas compliqués.
Méthodes
On a procédé à une étude rétrospective des dossiers médicaux de 211 cas chirurgicaux consécutifs d'appendicite soupçonnée étalés sur une période de 11 ans. On a évalué les retards avant le traitement et l'évolution subséquente de l'état de santé du patient.
Résultats
Sur le total des cas, 8,1 % ont produit des résultats négatifs à l'appendicectomie, 75,8 % des sujets avaient une appendicite sans complication, 12,3 %, une appendicite avec complication et 3,8 %, d'autres problèmes chirurgicaux. La période écoulée avant la première consultation médicale était beaucoup plus longue chez les patients qui avaient une appendicite avec complication. Les divers retards après la première consultation médicale ne présentaient pas de différences significatives entre les groupes.
Conclusions
Dans un contexte de disponibilité limitée de technologies d'imagerie médicale, on n'a pas établi de lien entre l'observation clinique et une incidence accrue d'appendicite avec complication. On établit un lien entre la présence d'une appendicite avec complication et le temps écoulé avant la première consultation médicale du patient. Il est possible d'accorder la priorité au jugement clinique qui peut produire un bon rendement clinique dans la prise en charge de patients chez lesquels on soupçonne une appendicite, sans que le nombre d'appendicites avec complication et les taux d'appendicectomie négative augmentent de façon significative.
Appendicitis remains a difficult diagnosis.1 Physicians have long relied on clinical grounds to make this ever-challenging diagnosis. New diagnostic modalities have not yet been shown conclusively to improve the outcome in terms of negative findings on appendectomy and complicated appendicitis.2–10 The best results seem to involve algorithms that include some clinical score, even if ultrasonography or computed tomography (CT), or both, are used.11–13 The best use of ultrasonography and/or CT allows the physician to obtain additional information in equivocal cases.1,8,14,15
Observation and repeated clinical examination have been evaluated and have led to good clinical outcomes,12,16–24 whereas a false-negative clinical evaluation carries the potential of higher perforation rates.1,25 However, perforated and complicated appendicitis are associated more frequently with longer delays before first medical consultation.2,22,26,27 Negative findings on appendectomy are associated with non-negligible costs and potential morbidity.26
With a lifetime cumulative incidence of 8.6% and 6.7% for men and women, respectively,28 appendicitis is the most frequent abdominal emergency.2 Despite long experience with this diagnosis and a crowded literature on the subject, rates of negative findings on appendectomy have not decreased even today.26 Except for a few reports of rates of negative findings on appendectomy below 10%,22,29–31 most recent studies report rates between 15% and 34%.2,7,11,16,26,32–35 The situation is the same regarding the rate of complicated appendicitis, which has not changed substantially over time, remaining between 15% and 30%.2,11,22,27,29
Radiological diagnostic modalities are not consistently available.22 Whereas a sonogram or a CT scan may shorten delay in diagnosis in equivocal cases,1,31 these imaging modalities can, however, delay appropriate surgery,7,36 either while a patient is awaiting the examination or because of false-negative results. The importance and value of clinical judgment has been underlined by others.8,12,23,24 The goal of this study was to evaluate clinical performance in the diagnosis of suspected appendicitis in a centre with limited access to medical imaging technologies and to identify factors associated with complicated appendicitis.
Methods
The operating room registry of the Centre de santé Ste-Famille of Ville-Marie, Quebec, was reviewed to identify all cases with a preoperative and/or postoperative diagnosis of appendicitis. A case was considered
if the preoperative diagnosis was appendicitis, possibility of appendicitis or abdominal pain of unknown origin;
if planned surgery was appendectomy or exploratory laparotomy or laparoscopy; and
if the postoperative diagnosis was appendicitis.
The medical records of all these cases were then individually reviewed. The patients with either a possible or a confirmed diagnosis of appendicitis were then included in the study. The study period was from April 1991 to March 2002. Before this period, all files had been cleared except for administrative information.
Two-hundred and eleven consecutive cases with a preoperative and/or postoperative diagnosis of appendicitis were retrieved. Demographic data, clinical signs, various delays and hospital stay were collected from the records. The initial decision of the surgeon was divided into 2 categories: surgery and observation. The delays were categorized as follows:
(1) delay occurring before first medical consultation (which is related to the patient); and
(2) delay occurring after first medical consultation (which is related to medical care).
The delay after the first medical visit was further divided into
(2.1) delay between first primary care physician visit and surgical consultation;
(2.2) delay between the surgical consultation and the decision to operate; and
(2.3) delay between the decision to operate and the surgical intervention.
The delay before the first medical consultation was estimated from the patient's history of the beginning of symptoms, as noted in the medical records. The first visit to the emergency department was used as the first medical consultation even if the patient had been discharged and had returned for subsequent visits.
The status of the appendix at the time of the operation was obtained from the operative protocol and the pathology report. It was classified as uncomplicated (inflamed, gangrenous without perforation), complicated (perforation, abscess, peritonitis) and normal. Other postoperative diagnoses obtained were divided into surgical and nonsurgical diseases.
Multiple logistic regression analysis was carried out to identify which factors could predict the presence of complicated appendicitis. Multiple stepwise logistic regression, χ2 and Student's t test were applied when appropriate. Statistical significance was established at p < 0.05.
Results
The following demographic and clinical data were extracted. There were 82 women (38.9%) and 129 men (61.1%). The proportion of women was slightly higher in the group with negative findings on appendectomy (52.9%), but this difference was not statistically significant compared with their proportions of 37.5% in the group with uncomplicated appendicitis, 38.5% in the group with complicated appendicitis and 37.5% in the group with other pathology. However, the difference attained a statistical significance when the proportion of women who had negative findings on exploration was compared with the rest of the study population (p = 0.047). The mean age of the study population was 25.5 (standard deviation [SD] 14.6) years for the study population. It was 26.5 (SD 10.2) years for the group with negative findings on appendectomy, 24.1 (SD 14.7) years for the group with uncomplicated appendicitis, 29.6 (SD 21.1) years for the group with complicated appendicitis and 32.5 (SD 13.2) years for the group with other pathology. There was no statistically significant difference in age between groups.
Five patients (2.4%) had a comorbidity. Eight patients (3.8%) had other surgical conditions. There were 2 cases of Meckel's diverticulum and 1 case of each of the following conditions: intestinal duplication, perforated carcinoma of the cecum, torsion of the epiploic appendage, pelvic abscess, hemorrhagic oviarian cyst and torsion of an ovarian cyst. Among the remaining 203 patients (96.2%), there were 17 cases (8.4%) of negative findings on appendectomy, 160 cases (78.8%) of uncomplicated appendicitis and 26 cases (12.8%) of complicated appendicitis. For the whole group, the rate of negative findings on exploration was 8.1% (17/211). In these patients, there were 4 cases of adenitis, 2 cases of enteritis, 1 case of typhlitis, 1 case of endometriosis and 9 cases with no diagnosis.
In patients with appendicitis (uncomplicated and complicated), loss of appetite was present in 171 cases (91.9%), nausea and/or vomiting in 139 cases (74.7%), migrating pain in 147 cases (79.0%) and rebound tenderness in 146 cases (78.5%). Mean temperature was 36.8°C (SD 0.6°C) in the group with negative findings on appendectomy, 37.0°C (SD 0.7°C) in the group with uncomplicated appendicitis and 37.2°C (SD 0.8°C) in the group with complicated appendicitis (p = 0.18). Temperature was ≥ 37.5°C in 17.6%, 23.7% and 38.5% of cases in each group, respectively. The mean leukocyte count was 0.010 (SD 0.002) × 109/L in the group with negative findings on appendectomy, 0.015 (SD 0.005) × 109/L in the group with uncomplicated appendicitis and 0.016 (SD 0.004) × 109/L in the group with complicated appendicitis (p < 0.001). It was 0.011 × 109/L or higher in 50.0%, 85.5% and 84.7% of each group, respectively. Sonograms were obtained for 6 patients (2.8%) when a radiologist was present: 1 showed positive findings, 2 showed doubtful findings and 3 showed negative findings.
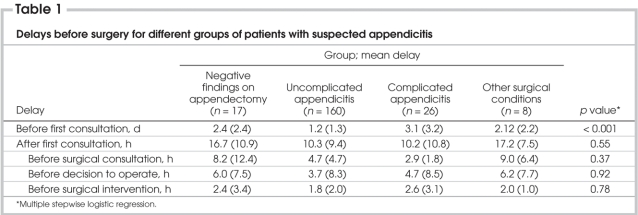
For the entire group, the mean delay before first medical consultation was 1.6 (SD 1.9) days, and the mean delay between first medical consultation and definitive treatment was 11.0 (SD 9.8) hours. The mean time lapse between the first medical visit and surgical consultation was 5.0 (SD 5.7) hours. The mean delay between surgical consultation and decision to operate was 4.1 (SD 8.2) hours. The mean delay between decision to operate and surgical intervention was 2.0 (SD 2.3) hours. Clinical observation was initially recommended after surgical consultation in 53.0% of cases of negative findings on appendectomy, in 30.0% of uncomplicated cases of appendicitis, in 30.8% of complicated cases, and in 50.0% of patients with other surgical conditions (p = 0.25). For each group, the various delays are presented in Table 1. After multiple stepwise logistic regression, the sole significant factor associated with the presence of complicated appendicitis was the delay before first medical consultation. This finding was given greater weight by the fact that none of the other delays reached statistical significance (Table 1).
Table 1
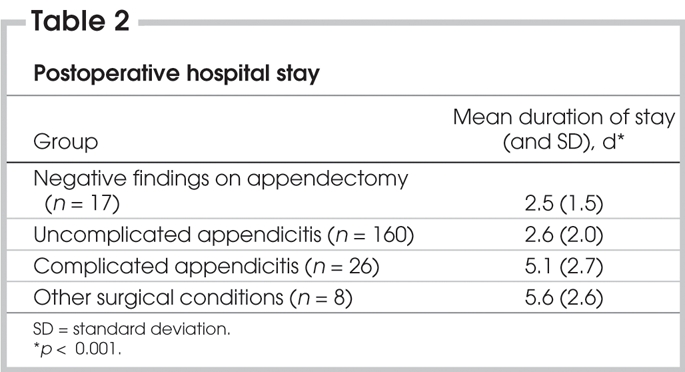
Diagnostic laparoscopy was carried out in 6 cases (2.8%): 5 cases of uncomplicated appendicitis and 1 case of complicated appendicitis. Table 2 shows the mean postoperative hospital stays, which were significantly longer in patients with complicated appendicitis and in patients with other surgical conditions. The difference in postoperative hospital stay in patients with negative findings on appendectomy compared with patients with uncomplicated appendicitis was not statistically significant. No deaths had occurred in this retrospective study. Three patients were readmitted to hospital for abscess, and all of these were complicated cases.
Table 2
Discussion
Ville-Marie is a small town on the western border of the province of Quebec with a population of 17 000. General surgery and anesthesiology represent the only permanent attending specialties. A radiologist is available 1 or 2 days each month and only during the daytime. The nearest hospital is 150 km away. The practitioners in such a centre must rely on clinical judgment when facing the possibility of a diagnosis of appendicitis. Unfortunately, it is not possible to know the exact number of patients who consulted with a possible diagnosis of appendicitis if they were discharged after a negative evaluation by the surgeon. In addition, it cannot be assumed that no patients were lost to follow-up after a first consultation. This constitutes a potential limitation of this study. However, considering the low incidence of appendicitis and the great distance to the next centre, the number of patients who presented first at this centre and consulted in another centre thereafter is probably low. A retrospective study of the patients with possible appendicitis in this setting may thus represent a good model with which to evaluate the clinical performance of the team.
An 8.1% rate of negative exploration represents a good clinical performance, because a rate of 15% is still considered acceptable.37 Despite many trials to improve these results, it has become apparent that, in most units, the rate of normal appendix removal remains around 15%.1,2,7,33,34 Unlike previous reports,38 recent reviews have found no link between the frequency of perforation and misdiagnosis.2 In the present review, a rate of complicated appendicitis (perforated and/or with peritonitis or abscess) of 12.3% overall also represents a good performance when compared with the rates in the recent literature of between 15% and 30%.2,11,22,27,29
In this review and others,2,22,26,27 the presence of complicated appendicitis is related to factors controlled by the patients as represented by a significantly longer delay before the first medical consultation. The observation of patients with repeated clinical evaluations was of great value, because no other delays showed statistically significant differences between groups (Table 1). Clinical observation led to longer preoperative delays in cases of normal appendix and other surgical conditions (Table 1). Even though the difference in these delays was not significant, it underlines the suspicion of other processes than appendicitis.
It is possible that ultrasonography and/or CT could have identified appendicitis earlier, as suggested elsewhere.1,14,30,31,34 However, false-negative results may increase the rate of complicated cases.7,25 The problem resides in the fact that patients with persisting pain and negative findings on investigation cannot be discharged without great confidence that a dangerous process is not ongoing. Today, laparoscopy may aid in the management of these patients.8,22 However, the best recent results incorporate various clinical scores,11–13 demonstrating that diagnostic imaging modalities should be reserved for equivocal cases or to rule out other diagnosis such as a gynecological condition.1,8,14 Clinical judgment and repeated physical examinations still have an essential and valuable role in the diagnosis of appendicitis.8,15,38
In this review, the hospital stay was not longer for patients with a negative exploration, contrary to the findings of other authors.25,33 The delay was the same for patients with a normal appendix as for patients with uncomplicated appendicitis (Table 2). The significantly longer delays were for patients with complicated appendicitis and patients with other surgical pathologies. The length of hospital stay for patients with negative exploration may be the result not only of the surgical intervention itself but also of the underlying disease.
This study was undertaken to demonstrate that clinical judgment remains valid in the diagnosis of appendicitis by using data from a centre that represents a good natural set-up. The limited availability of medical imaging technologies and confinement to a rural region make clinical evaluation a primary diagnostic tool. This review is from a different, but similar, centre from that reviewed in a previous study22 but reveals the same observations and allows the same conclusions to be drawn.
The results of this study suggest that in the context of limited available medical imaging modalities clinical observation was not associated with an increased incidence of complicated appendicitis. The presence of complicated appendicitis was associated with the delay before the patient's first medical consultation. In conclusion, clinical judgment can be prioritized and can lead to good clinical performance in the management of patients with suspected appendicitis, with no significant increase in rates of complicated appendicitis and negative findings on appendectomy.
Competing interests: None declared.
Correspondence to: Dr. Eric Bergeron, 3120 blvd. Taschereau, Greenfield Park QC J4V 2H1; eric.bergeron@traumaquebec.org
References
- 1.Beasly SW. Can we improve diagnosis of acute appendicitis? BMJ 2000;321:907-10. [DOI] [PMC free article] [PubMed]
- 2.Flum DR, Morris A, Koepsell T, et al. Has misdiagnosis of appendicitis decreased over time? A population-based analysis. JAMA 2001;286:1748-53. [DOI] [PubMed]
- 3.Morris KT, Kavanagh M, Hansen P, et al. The rational use of computed tomography scans in the diagnosis of appendicitis. Am J Surg 2002;183:547-50. [DOI] [PubMed]
- 4.Orr RK, Porter D, Hartman D. Ultrasonography to evaluate adults for appendicitis: decision making based on meta-analysis and probabilistic reasoning. Acad Emerg Med 1995;2:644-50. [DOI] [PubMed]
- 5.Franke C, Bohner H, Yang Q, et al. Ultrasonography for diagnosis of acute appendicitis: results of a prospective multicenter trial. Acute Abdominal Pain Study Group. World J Surg 2000;24:496-7. [DOI] [PubMed]
- 6.Ford RD, Passinault WJ, Morse ME. Diagnostic ultrasound for suspected appendicitis: Does the added cost produce a better outcome? Am Surg 1994;60:895-8. [PubMed]
- 7.Perez J, Barone JE, Wilbanks TO, et al. Liberal use of computed tomography scanning does not improve diagnostic accuracy in appendicitis. Am J Surg 2003;185:194-7. [DOI] [PubMed]
- 8.Paulson EK, Kalady MF, Pappas TN. Suspected appendicitis. N Engl J Med 2003;348:236-42. [DOI] [PubMed]
- 9.Lee SL, Walsh AJ, Ho HS. Computed tomography and ultrasonography do not improve and may delay the diagnosis and treatment of acute appendicitis. Arch Surg 2001;136:556-62. [DOI] [PubMed]
- 10.Rao PM, Rhea JT, Rattner DW, et al. Introduction of appendiceal CT: impact on negative appendectomy and appendiceal pêrforation rates. Ann Surg 1999;229:344-9. [DOI] [PMC free article] [PubMed]
- 11.Zielke A, Sitter H, Rampp TA, et al. Clinical decision-making, ultrasonography, and scores for evaluation of suspected acute appendicitis. World J Surg 2001;25:578-84. [DOI] [PubMed]
- 12.Zielke A, Sitter H, Rampp TA, et al. Validation of a diagnostic scoring system (Ohmann score) in acute appendicitis. Chirurg 1999;70:777-83. [DOI] [PubMed]
- 13.Ohmann C, Yang Q, Franke C. Diagnosis scores for acute appendicitis. Abdominal Pain Study Group. Eur J Surg 1995;161:273-81. [PubMed]
- 14.Rice HE, Arbesman M, Martin DJ, et al. Does early ultrasonography affect management of pediatric appendicitis? A prospective analysis. J Pediatr Surg 1999;34:754-8. [DOI] [PubMed]
- 15.Hong JJ, Cohn SM, Ekeh AP, et al. Miami Appendicitis Group. A prospective randomized study of clinical assessment versus computed tomography for the diagnosis of acute appendicitis. Surg Infect (Larchmt) 2003;4:231-9. [DOI] [PubMed]
- 16.Andersson RE, Hugander A, Ravn H, et al. Repeated clinical and laboratory examinations in patients with an equivocal diagnosis of appendicitis. World J Surg 2000;24:479-85. [DOI] [PubMed]
- 17.Jones PF. Suspected acute appendicitis: trends in management over 30 years. Br J Surg 2001;88:1570-7. [DOI] [PubMed]
- 18.Jones PF. Active observation in management of acute abdominal pain in childhood. BMJ 1976;2:551-3. [DOI] [PMC free article] [PubMed]
- 19.Thomson HJ, Jones PF. Active observation in acute abdominal pain. Am J Surg 1986;152:522-5. [DOI] [PubMed]
- 20.Dolgin SE, Beck AR, Tartter PI. The risk of perforation when children with possible appendicitis are observed in the hospital. Surg Gynecol Obstet 1992;175:320-4. [PubMed]
- 21.Jones PF. Practicalities in the management of the acute abdomen. Br J Surg 1990;77:365-7. [DOI] [PubMed]
- 22.Bergeron E, Richer B, Gharib R, et al. Appendicitis is a place for clinical judgement. Am J Surg 1999;177:460-2. [DOI] [PubMed]
- 23.Graff L, Radford MJ, Werne C. Probability of appendicitis before and after observation. Ann Emerg Med 1991;20:503-7. [DOI] [PubMed]
- 24.Colson M, Skinner KA, Dunnington G. High negative appendectomy rates are no longer acceptable. Am J Surg 1997;174:723-7. [DOI] [PubMed]
- 25.Graff L, Russell J, Seashore J, et al. False-negative and false-positive errors in abdominal pain evaluation: failure to diagnose acute appendicitis and unnecessary surgery. Acad Emerg Med 2000;7:1244-55. [DOI] [PubMed]
- 26.Flum DR, Koepsell T. The clinical and economic correlates of misdiagnosed appendicitis: nationwide analysis. Arch Surg 2002;137:799-804. [DOI] [PubMed]
- 27.Pittman-Waller VA, Myers JG, Stewart RM, et al. Appendicitis: Why so complicated? Analysis of 5755 consecutive appendectomies. Am Surg 2000;66:548-54. [PubMed]
- 28.Addiss DG, Shaffer N, Fowler BS, et al. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 1990;132:910-25. [DOI] [PubMed]
- 29.Richter M, Laffer U, Ayer G, et al. Is appendectomy really performed too frequently? Results of the prospective multicenter study of the Swiss Society of General Surgery. Swiss Surg 2000;6:101-7. [DOI] [PubMed]
- 30.Van Breda Vriesman AC, Kole BJ, Puylaert JB. Effect of ultrasonography and optional computed tomography on the outcome of appendectomy. Eur Radiol 2003;13:2278-82. [DOI] [PubMed]
- 31.Douglas CD, Macpherson NE, Davidson PM, et al. Randomized controlled trial of ultrasonography in diagnosis of acute appendicitis, incorporating the Alvarado score. BMJ 2000;321:919-22. [DOI] [PMC free article] [PubMed]
- 32.Koch A, Marusch F, Schmidt U, et al. Appendicitis in the last decade of the 20th century. Zentralbl Chir 2002;127:290-6. [DOI] [PubMed]
- 33.Blisard D, Rosenfeld JC, Estrada F, et al. Institutioning a clinical guideline practice to decrease the rate of normal appendectomies. Am Surg 2003;69:796-8. [PubMed]
- 34.Rettenbacher T, Hollerweger A, Greitzmann N, et al. Appendicitis: Should diagnostic imaging be performed if the clinical presentation is highly suggestive of the disease? Gastroenterology 2002;123:992-8. [DOI] [PubMed]
- 35.Poortman P, Lohle PN, Schoemaker CM, et al. Comparison of CT and sonography in the diagnosis of acute appendicitis: a blinded prospective study. AJR Am J Roentgenol 2003;181:1355-9. [DOI] [PubMed]
- 36.Roosevelt GE, Reynolds SL. Does the use of ultrasonography improve the outcome of children with appendicitis? Acad Emerg Med 1998;5:1071-5. [DOI] [PubMed]
- 37.Korner H, Sondenaa K, Soreide JA, et al. Incidence of acute nonperforated and perforated appendicitis: age-specific and sex-specific analysis. World J Surg 1997;21:313-7. [DOI] [PubMed]
- 38.Benjamin IS, Patel AG. Managing acute appendicitis: laparoscopic surgery is particularly useful in women. BMJ 2002;325:505-6. [DOI] [PMC free article] [PubMed]