Abstract
Introduction
The ability to mentally rotate an object in 3 dimensions has been shown to correlate with an individual's score on the Vandenberg and Kuse Mental Rotations Test. The goal of this study was to determine whether this Mental Rotations Test could be used to predict performance of a spatially complex surgical skill — the tying of a 1-handed surgical reef knot. In addition, we assessed whether learning a spatially complex surgical skill could be achieved more effectively via a computer-based self-directed learning approach than with a didactic lecture-based teaching method.
Methods
Sixty preclerkship medical students at the University of Western Ontario were randomized into 2 groups: a computer-based self-directed learning group and a didactic lecture-style learning group. Following the administration of the Mental Rotations Test, the students were taught how to tie a 1-handed surgical reef knot via the learning modality assigned to their respective group.
Results
Students with superior Mental Rotations Test scores were able to tie more surgical knots in the allocated time (p < 0.001). Students learning how to tie the surgical knot via the computer-based self-directed learning modality showed improvement on their knot tying abilities more rapidly than their didactically trained colleagues.
Conclusion
The ability to mentally rotate an object in 3 dimensions played an important role in the initial learning of a spatially complex surgical technical skill. Our data demonstrated that self-directed learning was as effective and more practical than traditional lecture-based learning.
Abstract
Introduction
On a démontré qu'il existe un lien entre la capacité d'une personne à faire tourner mentalement un objet tridimensionnel et le résultat qu'elle obtient au test de rotation mentale de Vandenberg et Kuse. Cette étude visait à déterminer si ce test de rotation mentale pourrait servir à prédire l'exécution d'une technique chirurgicale complexe sur le plan spatial : nouer d'une seule main un nœud plat chirurgical. Nous avons en outre évalué s'il serait possible d'apprendre plus efficacement une technique chirurgicale complexe sur le plan spatial par une méthode informatisée d'apprentissage autodirigé plutôt que par une méthode didactique.
Méthodes
On a affecté par randomisation à deux groupes 60 étudiants en médecine de l'Université Western Ontario qui n'avaient pas encore fait leur stage : un groupe d'apprentissage autodirigé par ordinateur et un groupe d'apprentissage didactique. À la suite de l'administration du test de rotation mentale, on a appris aux étudiants à nouer d'une seule main un nœud plat chirurgical par la technique d'apprentissage affectée à leur groupe respectif.
Résultats
Les étudiants qui ont obtenu des résultats supérieurs au test de rotation mentale ont pu nouer davantage de nœuds chirurgicaux pendant la période prescrite (p < 0,001). Les étudiants qui apprenaient à nouer le nœud chirurgical par la méthode informatisée d'apprentissage autodirigé ont vu leur technique s'améliorer plus rapidement que celle de leurs collègues qui ont suivi une formation didactique.
Conclusion
L'incapacité de produire la rotation mentale d'un objet tridimensionnel a joué un rôle important dans l'apprentissage initial d'une technique chirurgicale complexe sur le plan spatial. Nos données ont démontré que l'apprentissage autogéré était efficace et plus pratique que l'apprentissage didactique traditionnel.
As new surgical technologies evolve that require new skill sets, it is essential that we identify the factors that influence how we teach trainees surgical procedures. Although numerous influences on surgical technical skill acquisition have been described,1 only the impact of visual-spatial ability has been consistently related.2–4 Visual-spatial ability — or more specifically, the skill of mentally manipulating an object in 3 dimensions — appears to be consistently related to the initial acquisition of a surgical technical skill.2,3 Wanzel and colleagues2 compared several tests of visual-spatial ability and determined that the Vandenberg and Kuse Mental Rotations Test5 was most reliable in relating this ability (specifically, end-point visualization) to the acquisition of a spatially complex surgical technical skill. We applied this finding to the ability to tie a 1-handed surgical reef knot and hypothesized that the step-by-step end-product visualization is related to the Mental Rotations Test score and, ultimately, one's visual-spatial ability. Thus the primary goal of this study was to determine whether the Mental Rotations Test can be extended to assess visual-spatial ability as it relates to learning to tie a 1-handed surgical reef knot. This finding further validates the relation between visual-spatial ability and initially learning a surgical technical skill.
Currently, preclerkship medical students at our institution learn to tie surgical knots via both didactic and self-directed learning modalities. Both of these approaches provide a medium by which students can acquire this surgical skill, but few studies have compared the effectiveness of the 2 techniques in teaching a set skill. Thus, this study also seeks to identify whether learning a spatially complex surgical skill can be more easily attained through a computer-based self-directed learning strategy or a didactic lecture-based approach.
Method
We selected the 1-handed surgical reef knot because of its spatial complexity and practicality for medical students approaching their clerkship training.
We invited first-and second-year medical students at the University of Western Ontario (2003) to participate in the study. We distributed information about the study in the informed consent form to all invited classes via email. Interested individuals were asked to contact one of the authors. Once contact was made, we entered the individual into a confidential database. Sixty preclerkship medical students agreed to participate in the study. We used the confidential database to randomly divide subjects into either the didactic teaching group or the computer-based learning group. This database was kept strictly confidential and was destroyed immediately after study administration.
On the day of the study, we printed 1 data sheet containing individuals' names and the group to which they were placed. We randomly assigned an identification sticker with 6 arbitrary numbers to each individual; these numbers could not identify the study participants.
After distributing the numbers, and on the basis of prewritten instructions, each group was greeted, provided with information on the study methods and asked to fill out an informed consent form. The students were then allowed to ask procedure-oriented clarification questions. After this initial introduction, the Mental Rotations Test was administered according to the instructions outlined in the testing package provided by Dr. M. Peters and colleagues6 — a sample item from the test appears in Figure 1. Students were asked to affix one of their identification labels to the test, allowing us to match subjects' test scores with their surgical knot tying performance while maintaining their anonymity.
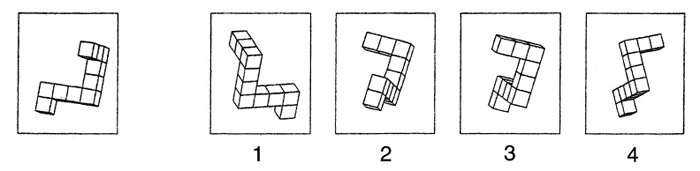
FIG. 1. Sample item from the Mental Rotations Test. This is a sample item appearing on the redrawn Vandenberg and Kuse Mental Rotations Test Version A by Peters and colleagues. 6 The medical students were asked to identify which of the 4 items depicted on the right match the reference object on the left. (Reprinted with permission from Peters et al. 6 ©1995 Elsevier.)
The computer-based learning module involved a computer presentation that comprised 13 procedural steps with both 2-dimensional images and written instructions on tying a 1-handed surgical reef knot. Students were seated at computers preloaded with the computer-based presentation software and were instructed on how to go through the presentation. They were then given three 45-cm 2.0 black braided surgical suture ties and a knot tying board provided by Ethicon Inc.; the board comprised 2 opposing rubber bands, firmly secured to a plastic surface. These were fastened to each student's work table via suction cups (Fig. 2). Based on prewritten instructions, students were allowed to go through the computer-based presentation for 10 minutes, during which time they could practise tying 1 surgical reef knot. After the 10-minute training period, students had 1 minute to tie as many knots as possible (repetition time). The training and repetition sequences were repeated 3 times in total. After each sequence, the student's identification label was fixed to a free end of the suture, and a member of the research team removed the suture from the knot. The training/repetition trial number and the total number of knots appearing on the suture (including the 1 practice knot tied during the training session) was recorded on the labelled suture (for example, one–3). For this particular trial, we counted only the knots that were laid square, with both throws of the 1-handed reef knot, toward the total number of knots tied.
FIG. 2. Suture tying board provided by Ethicon Incorporated. Preclerkship medical students were instructed on how to tie a surgical knot across the 2 opposing rubber bands.
The didactic lecture was presented in conjunction with the same presentation provided to the computer-based learning group. Students were seated in a traditional lecture theatre and were given three 45-cm 2.0 black braided surgical suture ties and an Ethicon Inc. knot-tying board, as previously described. The lecture was prewritten and comprised the verbal instructions supplied in the written text of the computer-based presentation, along with a live demonstration that sequentially followed the 13 steps outlined in the presentation. The presentation lasted approximately 10 minutes, and students were instructed to practise tying 1 surgical reef knot. After the 10-minute training time, students were given a 1-minute repetition time, during which they could tie as many knots as possible. Student performance was labelled as described in the computer-based situation, and the lecture/repetition sequence was repeated 3 times.
We quantified and recorded Mental Rotations Test scores along with the number of knots tied in each training/repetition sequence and the total number tied across all training/repetition sequences. We made statistical comparisons between the computer-based group and the didactically trained group on several variables, including between-group Mental Rotations Test scores, between-group total number of knots tied, between-group total number of knots tied per training/repetition sequence and overall total number of knots tied versus Mental Rotations Test scores.
Statistical analysis
We used a Levene F-test to test the variability of the 2 samples. We then compared the groups, using t tests based on this variability. If the 2 samples had equal variability (Levene's F-test value of p > 0.01), we recorded the value of the t test. Conversely, the value of the t test for samples with nonequal variability was recorded for F-tests with p values less than 0.01.
We used a log-transformed repeated-measures analysis of variance to determine the difference between the didactic and the computer-based groups in terms of their Mental Rotations Test scores. These data were log-transformed to minimize the effects of outliers, as well as to correct for unidentified inequality or skewness of the data sets.
A linear regression model was used to compare the average Mental Rotations Test scores of all students with their respective total number of knots tied. A log-transformed Pearson correlation was done on the log-transformed data to identify the correlation coefficient. Log-transformed Pearson correlations were also performed for both the didactic and the computer-based groups. We did a statistical analysis in consultation with the Biostatistical Support Unit of the University of Western Ontario, using the SAS System.
Results
The data obtained in our study revealed that the visual-spatial abilities of the medical students, as measured by the Mental Rotations Test, did not differ significantly across the computer-based or the didactically trained groups. The mean test score of the computer-based group was 5.92 (95% confidence interval [CI] 5.21–6.62), and for the didactic group was 5.35 (95% CI 4.47–6.23). Within both groups, medical students with higher scores tied a significantly greater total number of surgical knots. The log-transformed Pearson correlation of the didactic group was r = 0.45, p < 0.01, whereas the log-transformed Pearson correlation of the computer-based group was r = 0.42, p < 0.05 (Fig. 3). There was no significant difference between these 2 results. The Pearson correlation of the relation between test score and total number of knots tied, irrespective of learning modality, was r = 0.45, p < 0.001.
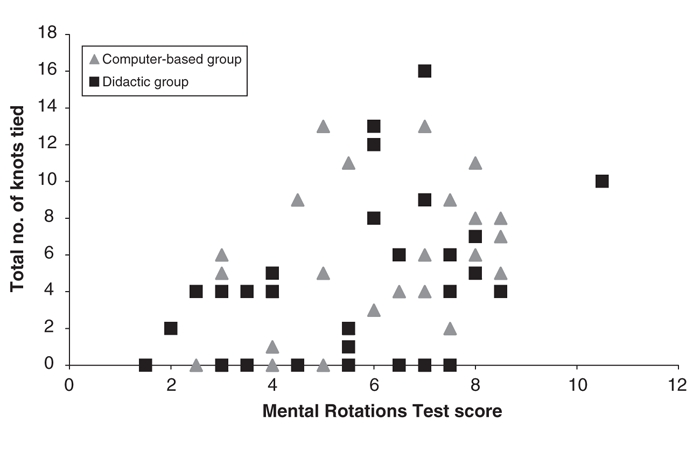
FIG. 3. Total number of knots tied versus Mental Rotations Test score. A regression plot illustrating the total number of 1-handed surgical reef knots tied during three 10-minute training/repetition sequences versus the Vandenberg and Kuse Mental Rotations Test scores of preclerkship medical students in both the computer-based self-directed learning group (grey) and the didactically trained group (black). The log-transformed Pearson correlations were r = 0.42, p < 0.05; r = 0.45, p < 0.01) for the computer-based and didactic groups, respectively. Fifty-one points are shown as a result of 9 individuals having equivalent Mental Rotations Test scores and total number of knots tied.
The total number of knots tied did not differ significantly among the self-directed and didactically trained groups. On average, across all 3 trials, subjects in the computer-based group tied a total of 5.30 knots (95% CI 3.84–6.75), whereas subjects in the didactically trained group tied a total of 4.20 knots (95% CI 2.56–5.84). Both groups had a similar portion of individuals who did not tie a surgical knot during the first training sequence (56.7% in the computer group, 60.0% in the didactic group). The computer-based group improved more significantly (p < 0.04) than the didactically trained group during the second training/repetition sequence (Fig. 4, Fig. 5).
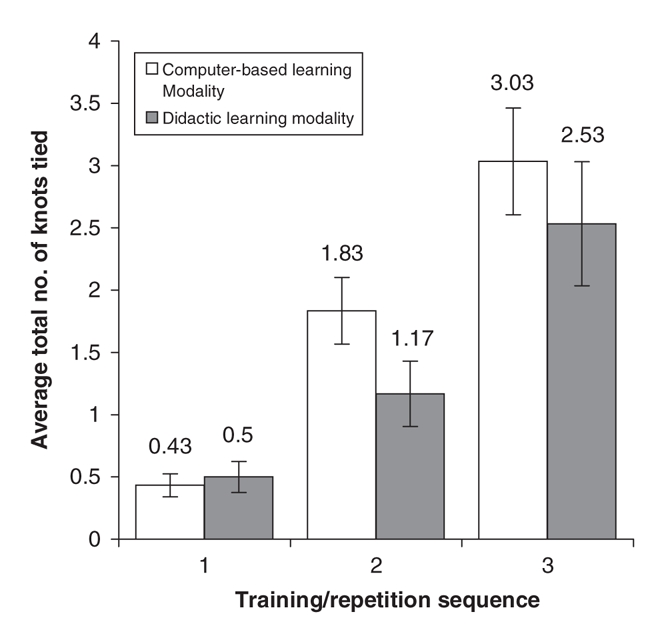
FIG. 4. Average number of knots tied per training/repetition sequence. A comparison of the average number of knots tied by preclerkship medical students within each of three 10-minute training/repetition sequences between the computer-based self-directed learning group and the didactically trained group. Error bars correspond to the standard error of the mean shown.
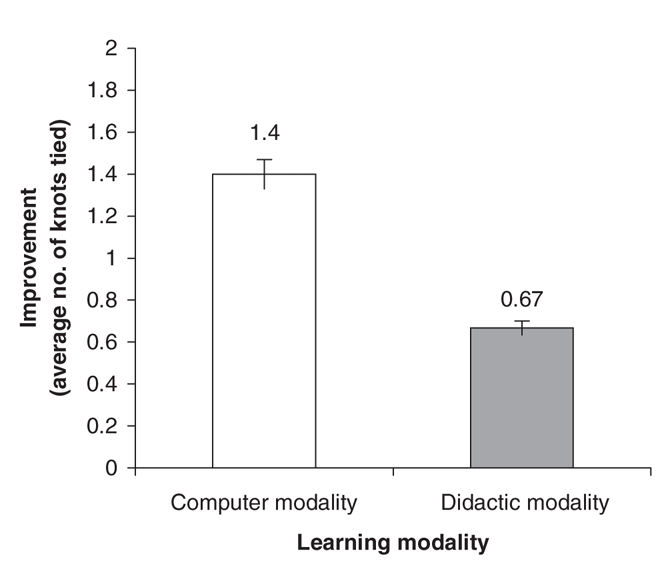
FIG. 5. Improvement in the number of knots tied between the first and second training/repetition sequence. A comparison of the improvement (in average number of knots tied by preclerkship medical students) between the first and second training/repetition sequence in both the computer-based self-directed learning group and the didactically trained group. A significant ( p < 0.04) difference was observed. Error bars correspond to the standard error of the mean shown.
Discussion
Our results demonstrated that Mental Rotations Test scores positively correlate with the total number of surgical knots tied (r = 0.45, p < 0.001); students with superior visual-spatial ability tied more surgical knots. This relation was found among medical students in both the computer-based learning group (p < 0.05) and the didactically trained group (p < 0.01). The similar results between the 2 groups suggests that learning modality was an independent factor; students with higher visual-spatial ability succeeded irrespective of the learning modality under which they trained.
Our findings support those of Wanzel and colleagues, who found scores on the Mental Rotations Test to positively predict performance of a 2- and 4-flap z-plasty.2 In a separate study, Wanzel and colleagues3 identified the relation between higher-order visual-spatial ability and performing a rigid fixation of a fractured anterior mandible (inanimate bench model).Thus visual-spatial ability appears to play an important role in the initial learning of a spatially complex surgical technical skill among surgical residents,2,3 senior dentistry students3 and preclerkship medical students.
The role of visual-spatial ability in the technical performance of a senior surgeon, or in predicting future aptitude for becoming a technically proficient surgeon, are contentious issues. Wanzel and colleagues3 suggest that visual-spatial ability may not be related to a surgeon's overall technical competency and thus conclude that it cannot be used as an independent predictor of future surgical aptitude. Although we agree with Wanzel and colleagues, we propose that the proficiency of learning a new spatially-complex surgical skill remains an important issue.
In an era of continual technological advances, the ability to acquire new technical skills sets will identify future surgeons. Surgeons who fail to acquire these new skills or who have difficulty adapting to change may be restricted in their future practice, and those who have difficulty mastering a simple skill may not progress to more advanced skills in a timely manner. Improved visual-spatial ability and increased proficiency in learning surgical techniques will undoubtedly play a strong role in both surgical residency training and in maintaining a progressive surgical practice. The role of visual-spatial ability in predicting future surgical aptitude, both in the technical competence of a senior surgeon and in predicting that same surgeon's ability to learn new techniques, cannot be discounted and requires further investigation.
The role of learning modality in surgical skill acquisition has not been a heavily investigated area. Rogers and colleagues identified that a computer-based self-directed learning approach yielded similar results to a lecture and feedback seminar. Our findings are consistent: medical students in both the computer-based and the didactic groups tied a similar number of surgical knots. It appears that students learn equally well in self-directed and teacher-centred learning situations.
Despite the uniformity in performance across learning modalities, students in the computer-based group acquired the measured skill with fewer repetitions than their didactically trained colleagues. This result is most clearly illustrated by the average total number of knots tied during the first and second training/repetition sequences and by the computer-based groups' improvement from their first iteration scores (Fig. 4, Fig. 5). It appears that the students in the computer-based group became more proficient at tying a surgical knot sooner than the didactically trained group. This improved proficiency is at odds with the results of Rogers and colleagues,7 who found that the performance of their computer-based group was of lower quality. Unfortunately, our outcome measure was limited to the total number of square knots thrown and did not evaluate performance quality. An assessment tool, such as an objective structured assessment of technical skills exam, may be more sensitive to these parameters and provides room for further investigation. Despite this limitation, and based on the equivalency of performance as assessed by our outcome measure, it appears that self-directed learning may be more practical and less time-and resource-intensive than a traditional didactic teaching approach.
A balance must be reached in teaching a basic concept that can be further refined through practice and one-on-one teaching (for example, in the senior year of clinical clerkship). From our perspective, self-directed learning affords a worthwhile balance between resource intensiveness and the practical acquisition of knowledge. Further, since lectures are typically given to students on a single occasion (not the 3 training/ repetition sequences seen in this study), the results suggest that self-directed skill acquisition may be a more practical learning modality.
Acknowledgments
No funding was required for the execution of this study. Suture and knot-tying boards were graciously provided by Ethicon, Inc. This sponsor had no role in the study design, data collection, analysis, interpretation or writing of this report. We thank St. Joseph's Health Care London for providing us with the rooms and computers used in this study, as well as Vicki Oliver for her help with administering the study. Thanks also to Dr. Michael Peters, University of Guelph, for supplying redrawn figures for the Mental Rotations Test and Larry Stitt, Department of Epidemiology and Biostatistics, Biostatistical Support Unit, University of Western Ontario, for his assistance with data analysis.
Presented at the 2004 Annual Meeting of the Royal College of Physicians and Surgeons of Canada.
Competing interests: None declared.
Correspondence to: Dr. Michael Brandt, Department of Otolaryngology, Schulich School of Medicine & Dentistry, London Health Sciences Centre—Victoria Hospital, 800 Commissioners Rd. E, London ON N6A 5W9; mbrandt2005@meds.uwo.ca
References
- 1.Wanzel KR, Ward M, Reznick RK. Teaching the surgical craft: from selection to certification. Curr Probl Surg 2002;39:573-659. [DOI] [PubMed]
- 2.Wanzel KR, Hamstra SJ, Anastakis DJ, et al. Effect of visual-spatial ability on learning of spatially-complex surgical skills. Lancet 2002;359:230-1. [DOI] [PubMed]
- 3.Wanzel KR, Hamstra SJ, Caminiti MF, et al. Visual-spatial ability correlates with efficiency of hand motion and successful surgical performance. Surgery 2003;134:750-7. [DOI] [PubMed]
- 4.Anastakis DJ, Hamstra SJ, Matsumoto ED. Visual-spatial abilities in surgical training. Am J Surg 2000;179:469-71. [DOI] [PubMed]
- 5.Vandenberg SG, Kuse AR. Mental rotations: a group test of three-dimensional spatial visualization. Percept Mot Skills 1978;47:599-604. [DOI] [PubMed]
- 6.Peters M, Laeng B, Latham K, et al. A redrawn Vandenberg & Kuse Mental Rotations Test: different versions and factors that affect performance. Brain Cogn 1995;28:39-58. [DOI] [PubMed]
- 7.Rogers D, Regehr G, Yeh KA, et al. Computer-assisted learning versus a lecture and feedback seminar for teaching a basic surgical technical skill. Am J Surg 1998;175:508-10. [DOI] [PubMed]


