Idiopathic lobular granulomatous mastitis (ILGM) is a rare chronic inflammatory disease of the breast that can clinically mimic breast carcinoma.1 Patients usually present with progressive onset of a breast lump. The most common clinical presentation is a firm unilateral, discrete breast mass, often associated with an inflammation of the overlying skin. Nipple retraction and even a sinus formation are present.1–3 Regional lymphadenopathy may be present in up to 15% of cases. In more than 50% of reported cases, the initial diagnosis was considered malignant or suspicious for breast carcinoma.4 The diagnosis of ILGM requires that other granulomatous lesions in the breast be excluded (Box 1). Tuberculosis (TB) of the breast is an uncommon disease that is often difficult to differentiate from cancer of the breast when it presents as a lump. Breast TB should be considered in differential diagnosis in people with clinically suspicious breast lumps who are from high-risk populations and/or endemic areas.
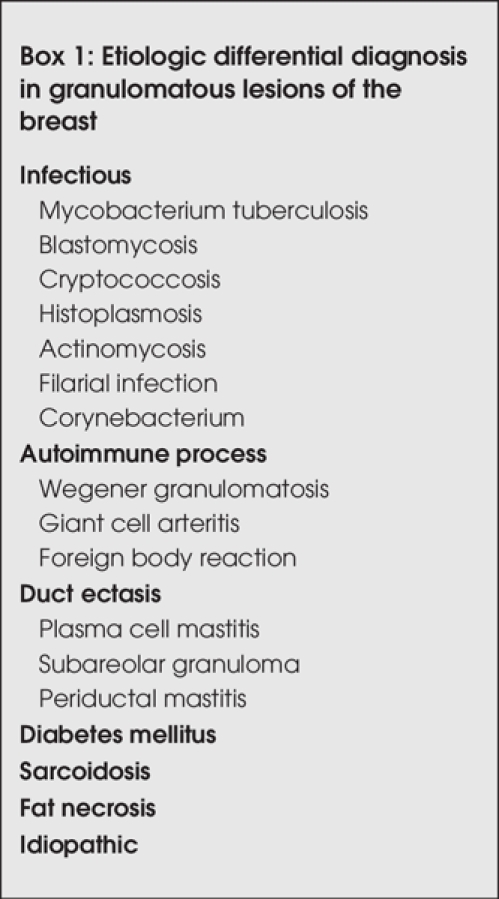
Box 1.
Here we report 3 cases of granulomatous mastitis (GM): 2 were ILGM and 1 was TB mastitis that occurs in women of reproductive age. These patients presented with breast masses of 3, 5 and 7 cm in diameter. All 3 patients were suspected of having malignant tumours. We hope this article will increase awareness of these interesting conditions.
Case reports
Case 1
A 27-year-old woman presented with a 2-month history of a left breast mass. She had a family history of breast cancer affecting her aunt. The patient had a 2-year-old child who had been breast-fed until the onset of the lesion, at which time breast-feeding was discontinued. There was no history of oral contraceptive use. The woman was afebrile, and on physical examination, there was a hard, painful, mobile mass, 3 cm in diameter, in the lower outer quadrant of her left breast. There was nipple discharge and skin retraction. The overlying skin showed signs of inflammation; palpable lymph nodes were present in the ipsilateral axilla. Intraoperatively, the surgeon noticed that the lesion was purulent and thought that it might be an abscess. Findings from cultures of purulent discharge remained sterile. The patient had been treated with multiple broad-spectrum antibiotics for 2 weeks, but the enduration persisted. Two weeks later, the size of the mass remained unchanged. The patient was seen in the casualty department, where an abscess of the breast was initially suspected. Mammography showed a focal asymmetric density associated with architectural distortion, skin thickening and retraction (Fig. 1). Sonographic images showed a hypoechoic lesion with indistinct border. Enlarged axillary lymph nodes were detected on sonography. The mass revealed malignant characteristics. Fine needle aspiration cytology (FNAC) was done on the lump, and granulomatous suppurative lesion was considered. The surgeon performed an excisional biopsy because the mass revealed highly malignant characteristics. The pathology of the lump showed areas of suppuration with micro-abscess and scattered granuloma. There were no signs of malignancy. After this report, detailed investigations were performed to determine the etiology of the lump. All microbiology tests were negative, and serological and hematological investigations were normal; the PCR test result for mycobacterium was also negative. A diagnosis of idiopathic lobular granulomatous mastitis was made. After treatment, the patient remained in good health, and there was no recurrence of breast lump after 5 years of follow-up.
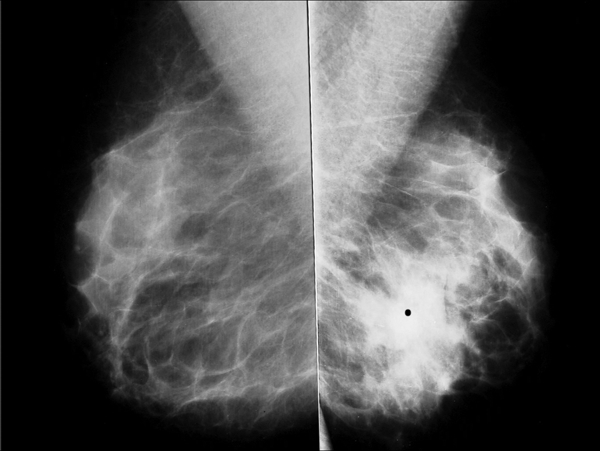
FIG. 1. Bilateral mediolateral oblique mammograms showing focal asymmetrical density with architectural distortion area (•) in the lower portion of the left breast.
Case 2
A 40-year-old woman presented to the outpatient clinic of obstetrics and gynecology, complaining of pain and a lump in the left breast for the past 3 months, following a trauma. She gave a history of low-grade evening fever with loss of weight and appetite for 7 months. She described a family history of breast cancer affecting her mother's sister. She had had 4 children (aged 18, 14, 12 and 6 years) before presentation, and all of them were breast-fed. The patient had taken no oral contraceptives. On physical examination, the left breast was very tender, and a diffuse, irregular mass was felt, mainly involving the lower inner quadrant and measuring 5 cm. The mass was firm and indurated, and purulent discharge from the left breast was found; there were no signs of infection or inflammation. There was no axillary or cervical lympadenopathy. The right breast was clinically normal. The ultrasonographic examination showed a hypoechoic heterogeneous mass measuring 5 cm in the lower quadrant of the left breast, with ill defined and mild posterior acoustic enhancement (Fig. 2). The mass appeared suspicious for malignancy or fat necrosis by ultrasonographic and clinical findings. To reach a definite diagnosis, FNAC was performed on the lump, and cytological findings were consistent with a granulomatous inflammatory lesion. A diagnosis of TB mastitis was made with a PCR test result after excisional biopsy. The chest x-ray was within normal limits. Thorough investigation for TB in other organs or body systems was negative.
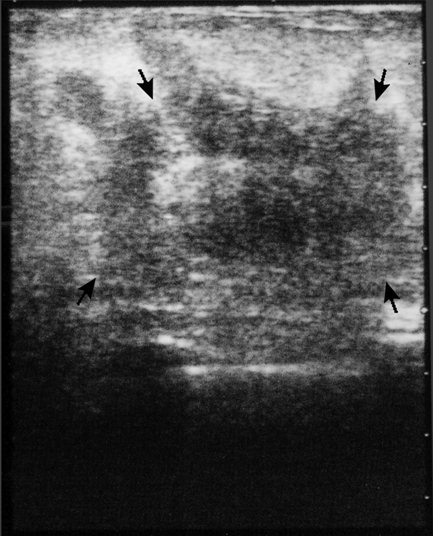
FIG. 2. Ultrasonographic examination of the left breast demonstrating a hypoechoic heterogeneous mass with irregular borders.
The patient was started on anti-TB therapy (3 drugs comprised the therapy) for 6 months. There has been no recurrence for 2 years of follow-up.
Case 3
A 38-year-old woman had a 1-month history of a right tender breast lump. The patient had no history of breast trauma or oral contraceptive use, and she had no family history of breast disease. She had 3 children, the youngest being 8 years old; all of them were breast-fed. On physical examination, there was a 7-cm mass in the inner (medial) central portion of the right breast, with induration of the overlying skin. The palpable lymph nodes were present in the ipsilateral axilla. Mammography revealed increased asymmetric density with no definite margins in a large volume of the right breast tissue, with thickening of the overlying skin (Fig. 3). Breast ultrasonographic examination showed increased echogenicity of the right side, compared with the left, with multiple hypoechoic areas. Several enlarged axillary lymph nodes were seen. Radiological examination showed a picture similar to that of an inflammatory breast carcinoma. FNAC was done on the lump, and cytological findings were consistent with a granulomatous inflammatory lesion. In this patient, the main histological feature was granulomatous inflammatory response centred on breast lobules, which confirmed the diagnosis of GM. On further investigation, we found no specific explanation of the etiology of the GM. PCR test results for mycobacterium were also negative.
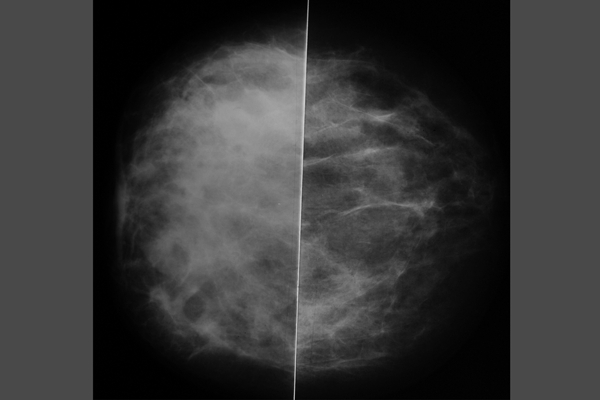
FIG. 3. Bilateral craniocaudal mammogram shows diffuse increased density in the right breast.
Pathology
FNAC of the lesions was characterized by the presence of scattered epithelioid histiocytes and multinucleated Langhans-type giant cells (Fig. 4). Neutrophilic polymorphs, lymphocytes, plasma cells and a few eosinophils were also observed in cases 1 and 3. In case 2, the cytological findings of epithelioid cell granulomas, Langhans' giant cells and lymphohistiocytic aggregates confirmed granulomas. There was no necrosis. Histology of the breast lesions showed similar appearances: florid granulomatous inflammation with well-formed granulomas in cases 1 and 3. The main histological feature was granulomatous inflammatory responses centred on breast lobules (Fig. 5). In affected lobules, there was a loss of acinar structures; the entire epithelial lining of the lobules was destroyed. Case 1 also showed areas of suppuration with micro-abscess formation. On the basis of these clinical, microbiological, radiological, cytological and histopathological findings, the final diagnosis was idiopathic lobular GM. In the second case, granulomatous lesions in TB mastitis were associated with ducts more than with lobules. Fibrosis may be prominent in chronic cases. The biopsy materials revealed numerous noncaseating granulomas. The PCR test result for mycobacterium was positive, and no malignant cells were identified in either the smears or the histological sections. There was no evidence of vasculitis or duct ectasia. Polarizing foreign material was not found in any of the cases. The clinical manifestation and mammographic findings were strongly suspicious for carcinoma.
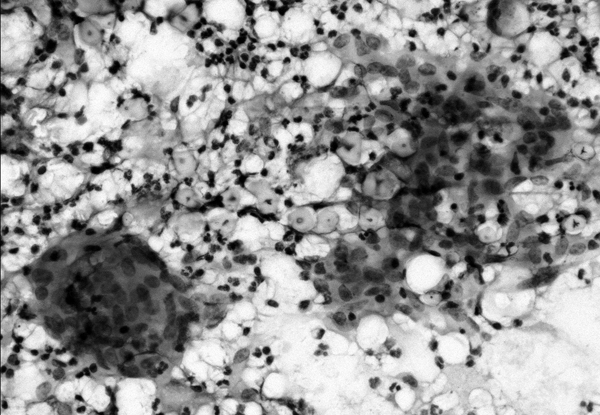
FIG. 4. Fine needle aspiration of granulomatous mastitis showing a multinucleate cell with epithelioid histiocytes and neutrophilic leukocytes (May–Grünwald-Giemsa stain, × 400).
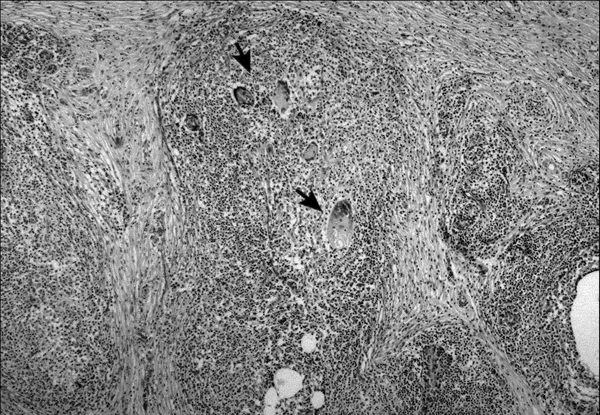
FIG. 5. Granulomatous inflammation with multinucleate giant cell formation (arrows) but without any caseous necrosis involving a breast lobule (Haematoxylin and eosin, × 200).
Discussion
ILGM is an uncommon breast lesion that is well known for its worrisome clinical presentations as a hard breast lump, particularly in younger women. Affected women are nearly always parous and usually present in their early thirties.4 On the whole, unilateral involvement of the breasts is typical, although bilateral disease has been described.5 A tender extra-areola lump is the usual presentation associated with fixation to the skin or to the underlying pectoralis muscle. Occasionally, nipple retraction and lymphadenopathy is seen, and regional lympadenopathy may be present in up to 15% of cases.4 Patients will have a breast mass that can vary in size from 0.5 to 9 cm, and often the overlying skin is inflamed.1,5 Inflammatory breast lesions of this kind may be clinically mistaken for malignancy, particularly if reactive draining lymph nodes are enlarged. In 2 of these cases, patients presented with tender and enlarged nodes. Thus, a mammogram can be misleading when the symptoms demonstrate no abnormality but more often suggest carcinoma.4 As a result of the sinister nature of these signs, there is often a strong suspicion of breast cancer.
The origin of ILGM is unknown, and its diagnosis rests on demonstrating a characteristic histological pattern, combined with the exclusion of other possible causes of granulomatous lesions in the breast3,4 (Box 1) and of breast cancer.1,3,4 TB is an important differential diagnosis because of the implications of corticosteroid therapy; however, the histological features of ILGM differ from those of typical TB. TB and other infections need to be excluded by serological tests and histological study of the affected tissue with special stains and by examining cultures of the affected tissue for aerobic and anaerobic bacteria, mycobacteria and fungi.6,7 In 2 of the cases presented here (case 1 and 3), the radiological findings, PPD skin test, histopathological picture, absence of acid-fast bacilli and fungi in the tissue, and negative result of the culture, ruled out these possibilities. Also, a woman in the reproductive age group who presents with a palpable lump in her breast might have TB; this must be considered, especially because the incidence of breast TB may increase with the global spread of AIDS. Physicians must also be cautious when examining patients from high-risk populations or endemic areas, like our region. Uncommon sites and similarities with other diseases clinically and radiographically occasionally lead to diagnostic and therapeutic delays.
The etiology of ILGM is unclear. The postulated causes include autoimmune disease, undetected organisms, reaction to childbirth and the use of oral contraceptives, but there are reports of ILGM occurring in patients who have not received oral contraceptives.1,2,6,8 Further, not all patients have a history of childbirth, and some have hyperprolactinemia.9 Our patients had normal serum prolactin concentrations, and there was no history of oral contraceptive use. Fletcher and colleagues5 suggested that the initial event was damage to ductular epithelium by infection, trauma or chemically induced inflammation, which allowed luminal secretion to escape into the lobular connective tissue, where it stimulated a granulomatous response and further damaged the lobular structures.
Among the large series describing the FNAC features of GM in the literature, the usefulness of FNAC in GM has been debated, with some authors confirming the useful role of FNAC10 and others concluding that the various causes of granulomatous inflammation cannot be confidently differentiated by FNAC.11 However, FNAC may not always differentiate between ILGM and other granulomatous diseases of the breast, and a confident diagnosis may require histological samples, negative microbiological investigations and clinical correlation. Adequate tissue specimens are therefore needed to differentiate IGM from other pathologies, including cancer and other causes of GM, such as TB, sarcoidosis and ductular ectasis. Combining the cytological features seen in the aspiration biopsy material with the histological appearance of the lesion led us to favour the diagnosis of IGM. In these 3 cases, breast carcinoma was ruled out by FNA, and the diagnosis of tuberculous mastitis was made after an excisional biopsy.
The treatment of choice for ILGM is unclear. Wide surgical resection of breast masses has been recommended, but corticosteroids have been reported to be useful and may avoid the disabling surgery that most patients with ILGM undergo. In patients with recurrence after biopsy or delayed wound healing, re-excision and a short therapy of high-dose steroids can be efficient. If there is no delayed wound healing or recurrence, no further therapy is required. Recurrence, fistula formation and secondary infection are well-known complications of idiopathic GM, thus long-term follow-up is recommended. Neither wound complication nor recurrence has been identified in the 3 cases, although corticosteroids were not used postoperatively. Most surgeons have limited experience in managing this clinical entity, and it is difficult to choose an appropriate treatment because none seem to be ideal.
In conclusion, ILGM and breast TB are rare inflammatory diseases of the breast that can clinically mimic malignancy and which may be misdiagnosed as carcinoma. The diagnosis of ILGM must be based on a multidisciplinary approach. None of these cases were diagnosed clinically and radiologically before FNAC and biopsy, which emphasizes the awareness among surgeons, radiologists and pathologists of this unusual but distinctive disorder. Increased awareness of these diseases will improve understanding and management of them.
Competing interests: None declared.
Correspondence to: Dr. Sevgi Bakaris, Kahramanmaras Sütcüimam Universitesi, Tip Fakültesi Patoloji ABD, 46050 Kahramanmaras, Turkey; fax +90 344 2212371; sevgiba@superonline.com, sbakaris@yahoo.com
References
- 1.Kessler E, Wolloc Y. Granulomatous mastitis: a lesion clinically simulating carcinoma. Am J Clin Pathol 1972;58:642-6. [DOI] [PubMed]
- 2.Going JJ, Anderson TJ, Wilkinson S, et al. Granulomatous lobular mastitis. J Clin Pathol 1987;40:535-40. [DOI] [PMC free article] [PubMed]
- 3.Donn W, Rebbeck P, Wilson C, et al. Idiopathic granulomatous mastitis: a report of three cases and review of the literature. Arch Pathol Lab Med 1994;118:822-5. [PubMed]
- 4.Jorgensen MB, Nielsen DM. Diagnosis and treatment of granulomatous mastitis. Am J Med 1992;93:97-101. [DOI] [PubMed]
- 5.Fletcher A, Magrath IM, R?ddell RH, et al. Granulomatous mastitis: a report of seven cases. J Clin Pathol 1982;35:941-5. [DOI] [PMC free article] [PubMed]
- 6.Osborne BM. Granulomatous mastitis by histoplasma and mimicking inflammatory breast carcinoma. Hum Pathol 1989;20:47-53. [DOI] [PubMed]
- 7.Wilson JP, Chapman SW. Tuberculous mastitis. Chest 1990;98:1505-9. [DOI] [PubMed]
- 8.Davies JD, Burton PA. Postpartum lobular granulomatous mastitis. J Clin Pathol 1983;36:363. [DOI] [PMC free article] [PubMed]
- 9.Rowe PH. Granulomatous mastitis associated with a pituitary prolactinoma. Br J Clin Pract 1984;38:32-4. [PubMed]
- 10.Kumarasinghe MP. Cytology of granulomatous mastitis. Acta Ctyol 1997;41:727-30. [DOI] [PubMed]
- 11.Martinez-Parra D, Nevado-Santos M, Melendez-Guerrero B, et al. Utility of fine-needle aspiration in the diagnosis of granulomatous lesions of the breast. Diagn Cytopathol 1997;17:108-14. [DOI] [PubMed]


