The terminal objective of surgical training is to produce competent surgeons capable of meeting the health care needs of our society. Recently, several accrediting medical bodies in North America proposed a framework of essential competencies required of all specialist physicians. The Royal College of Physicians and Surgeons of Canada's CanMEDS 2000 Project endorsed the following 7 core competencies:1 medical expert/clinical decision-maker, communicator, collaborator, manager, health advocate, scholar, and professional.
Similarly, in 1999 in the United States, the Accreditation Council for Graduate Medical Education (ACGME) Outcome Project adopted the following 6 competencies for all doctors:2 patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism, and systems-based practice.
Surgical training programs emphasize the achievement of both cognitive and technical competence. The cognitive ability of surgical trainees is clearly captured under competency domains including medical knowledge, clinical decision-maker and medical expert.1,2 Cognitive competence requires mastery of a predefined body of knowledge. Traditionally, this is achieved through review of reference texts and medical journals, together with regular attendance at academic lectures, workshops, teaching rounds and conferences.
Despite their importance to surgeons, motor skills or technical competence have historically been ill defined and consequently poorly assessed.3 Technical competence is frequently not defined explicitly but hidden in definitions of core competencies under nonspecific, subcategories including “medical expert — therapeutic skills for effective treatment” (CanMEDS) and “patient care — the performance of medical procedures” (ACGME). Technical competence is typically achieved in a graduated fashion through repeated exposure and hands-on practice as the surgical trainee progresses through residency.
Despite increasing efforts to clearly define and assess the domains in which a surgeon must achieve competency, to date few surgical educators have studied precisely how such competencies are acquired over time. Here, we (a) introduce the concept of “trajectory” for competency achievement, (b) speculate as to the trajectories of important competency domains in surgical training, and (c) propose a new and distinct competency domain — “operative competence” — and hypothesize as to the trajectory for its achievement.
Cognitive competence
The current standards for assessing cognitive knowledge include performance-based Objective Structured Clinical Examination (OSCE) scores4,5 and structured short-answer and multiple-choice questions.6 On the basis of these standards, cognitive competence is typically acquired in an arithmetic fashion with a linear trajectory over the course of surgical training7,8 (Fig. 1).
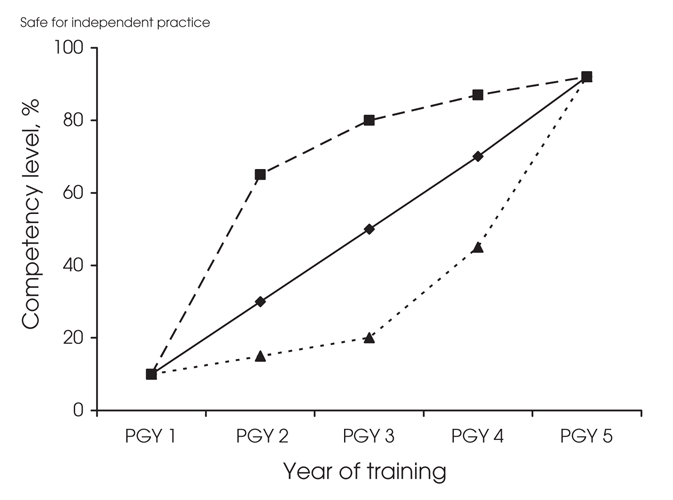
FIG. 1. Cognitive competence is achieved with a linear trajectory (diamonds); technical or motor skills competence is achieved in an exponential fashion with a negatively accelerating trajectory (squares); and operative competence is achieved in an exponential fashion with a positively accelerating trajectory (triangles) over the course of training.
Technical and motor skills competence
In contrast to cognitive competence, motor learning theory suggests that motor skills development and technical competence is achieved exponentially, with rapid initial improvements in performance followed by decreasing gains with practice over time — a negatively accelerating trajectory9–11 (Fig. 1).
Operative competence
Even as surgical educators better understand how to define and assess technical and cognitive competence, we hypothesize that there is a separate and distinct competency domain, operative competence, which is the ability to perform the entirety of an operative procedure. In contrast to pure technical competence and motor skills development which traditionally focuses on discrete motor skills or technical components of a larger operation (e.g., suturing, knot tying, stent or catheter placement),11 operative competence is a much broader, more global competency domain that captures the trainee's ability to perform the complete operation (from positioning the patient to wound closure), within the global concept of preoperative assessment and postoperative care. Whereas operative competence demands both cognitive and technical ability, it also requires other essential (yet difficult to measure) competencies, including opportunity and experience, clinical judgement, confidence and poise, communication skills and professionalism (Fig. 2).
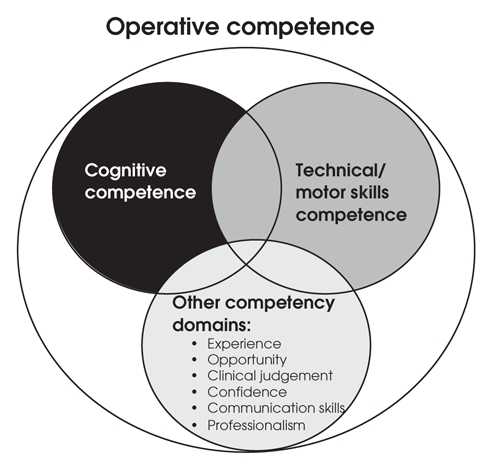
FIG. 2. In addition to cognitive and technical competence, operative competence requires other important competencies in surgical training.
Based on our collective experiences and observations as surgical educators, we hypothesize that the trajectory for the achievement of operative competence represents a composite (not necessarily the sum) of multiple and overlapping competencies (Fig. 2). Consequently, the trajectory for the achievement of operative competence differs from the trajectory of motor skills development and may be depicted by a positively accelerating trajectory with more gradual increases in performance early in training (and therefore more difficult to identify, assess and remediate by surgical educators, [see Fig. 1, triangles]).
Implications of competency trajectories on surgical education
Enhancing our understanding of the trajectories for important competency domains in surgical training may have significant implications on how surgical educators approach the assessment, evaluation, methods and timing of remediation for surgical trainees. For example, the trajectory for achieving operative competence (positively accelerating trajectory) may delay the identification of a trainee in need of corrective action because the slope of the trajectory curve may be too gradual or occur too late in the course of surgical training. This may not be a problem for other competency domains, including cognitive competence (linear trajectory) and motor skills or technical competence (negatively accelerating trajectory) whose performance trajectories rise earlier in the course of training. The identification of strengths and weaknesses in individual residents allows for appropriate goal-directed remediation. The early identification of trainees at risk for failure affords greater opportunity for corrective measures.
Several exciting strategies exist that can potentially alter the trajectory for the achievement of operative competence:
the use of laboratory based surgical skills training12
repetitive practice on virtual reality surgical simulators13
curriculum innovation, novel methods of exposing trainees to surgical mentors14
early and more meaningful participation in the operating room
timely and objective evaluation and feedback to trainees.
The concept of operative competence and its trajectory for achievement is both novel and complex, and it is perhaps the most important competency for surgical educators to appreciate as it represents an amalgamation of many of the essential competency domains in surgical training. Clearly, further work is needed to better understand and validate the concept of the trajectory of competency achievement. Such validation by surgical educators is increasingly possible with the use of scientifically and psychometrically valid and reliable assessments tools to evaluate both clinical (OSCE)5,15 and technical (OSATS) skills.3 Through such understanding, surgical training programs and trainees alike will be in a better position to optimize the learning environment and maximize the achievement of operative competence.
Competing interests: None declared.
Correspondence to: Dr. Michael A.S. Jewett, Division of Urology, University of Toronto, 610 University Ave., 3-124, Toronto ON M5G 2C4; fax 416 598-9997; m.jewett@utoronto.ca
References
- 1.Frank JR, Jabbour M, Tugwell P, et al. Skills for the new millenium: report of the societal needs working group, CanMEDS 2000 Project. Ann R Coll Physicians Surg Can 1996;29:206-16.
- 2.Accreditation Council for Graduate Medical Education (ACGME) General Competencies. Version 1.3. September 28, 1999. Chicago (IL): ACGME; 2000. (www.acgme.org).
- 3.Martin JA, Regehr G, Reznick RK, et al. Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg 1997;84:273-8. [DOI] [PubMed]
- 4.Harden R, Stevenson M, Downie W, et al. Assessment of clinical competence using an objective structured examination. BMJ 1975;1:447-51. [DOI] [PMC free article] [PubMed]
- 5.Sloan DA, Donnelly MB, Schwartz RW, et al. The Objective Structured Clinical Examination. The new gold standard for evaluating postgraduate clinical performance. Ann Surg 1995;222:735-42. [DOI] [PMC free article] [PubMed]
- 6.Hammond EJ, MeIndoe AK, Sansome AJ, et al. Multiple-choice examinations: adopting an evidence-based approach to exam technique. Anaesthesia 1998;53:1105-8. [DOI] [PubMed]
- 7.Blake JM, Norman GR, Keane DR, et al. Introducing progress testing in McMaster University's problem-based medical curriculum: psychometric properties and effect on learning. Acad Med 1996;71:1002-7. [DOI] [PubMed]
- 8.Baverstock RJ, MacNeily AE, Cole G. The American Urological Association In-Service Examination: performance correlates with Canadian and American specialty examinations. J Urol 2003;170:527-9. [DOI] [PubMed]
- 9.Kopta JA. An approach to the evaluation of operative skills. Surgery 1971;70:297-303. [PubMed]
- 10.Reznick R, Regehr G, MacRae H, et al. Testing technical skill via an innovative “bench station” examination. Am J Surg 1997;173:226-30. [DOI] [PubMed]
- 11.Risucci D, Cohen JA, Garbus JE, et al. The effects of practice and instruction on speed and accuracy during resident acquisition of simulated laparoscopic skills. Curr Surg 2001;58:230-5. [DOI] [PubMed]
- 12.Grober ED, Wanzel KR, Hamstra SJ, et al. Laboratory based training in urological microsurgery with bench model simulators: a randomized controlled trial evaluating the durability of technical skill. J Urol 2004;172:378-81. [DOI] [PubMed]
- 13.Derossis AM, Bothwell J, Sigman HH, et al. The effect of practice on performance in a laparoscopic simulator. Surg Endosc 1998;12:1117-20. [DOI] [PubMed]
- 14.Ephgrave KS, Ferguson K, Kreiter C, et al. Team-based versus preceptor-based assignment of junior surgery students. Am J Surg 1997;173:333-7. [DOI] [PubMed]
- 15.Regehr G, MacRae H, Reznick RK, et al. Comparing the psychometric properties of checklists and global rating scales for assessing performance on a OSCE-format examination. Acad Med 1998;73:993-7. [DOI] [PubMed]


