Abstract
Background
Occult cystobiliary communication (CBC) presents with biliary leakage, if the cystobiliary opening cannot be detected and repaired at operation. We investigated the clinical signs associated with the risk of occult CBC in the preoperative period by studying patients who developed biliary leakage after hydatid liver surgery.
Methods
We analyzed the records of 191 patients treated for hydatid liver cyst. Postoperative biliary leakage developed in 41 patients (21.5%). Independent predictive factors were established by logistic regression analysis using clinical parameters, whose cutoff values were determined by receiver operating characteristic (ROC) curves.
Results
Postoperative biliary leakage presented as external biliary fistula in 31 (75.6%) of 41 patients, as biliary peritonitis in 6 (14.6%) and as cyst cavity biliary abscess in 4 (9.8%). Independent clinical predictors of occult CBC, represented by biliary leakage, were alkaline phosphatase > 250 U/L, total bilirubin > 17.1 μmol/L, direct bilirubin > 6.8 μmol/L, γ-glutamyl transferase > 34.5 U/L, eosinophils > 0.09 and cyst diameter > 8.5 cm. Multilocular or degenerate cysts increased the risk of biliary leakage (p = 0.012). Postoperative complication rates were 53.7% in the patients with biliary leakage, and 10.0% (p < 0.001) in those without. The mean postoperative hospital stay was longer in patients with biliary leakage (14.3 [and standard deviation {SD} 1.9] d) than in those without (7.3 [SD 2.3] d) (p < 0.001). Nineteen (61.3%) of 31 biliary fistulae closed spontaneously within 10 days. The remaining 12 (38.7%) fistulae closed within 7 days after endoscopic sphincterotomy.
Conclusion
Factors that predict occult CBC due to hydatid liver cyst were identified. These factors should allow the likelihood of CBC to be determined and, thus, indicate the need for additional procedures during operation to prevent the complications of biliary leakage.
Abstract
Contexte
Une communication biliaire cystique (CBC) occulte se présente comme un épanchement biliaire si l'ouverture kystobiliaire ne peut être détectée et réparée à l'opération. Nous avons examiné les signes cliniques associés aux risques de CBC occulte durant la période préopératoire en étudiant des patients qui avaient développé un épanchement biliaire après une chirurgie du foie hydatique.
Méthodes
Nous avons analysé les dossiers de 191 patients traités pour des kystes hydatiques du foie. Un épanchement biliaire post-opératoire s'est formé chez 41 patients (21,5 %). Les prédicteurs indépendants ont été établis par analyse de régression logistique en utilisant les paramètres cliniques, dont les valeurs seuils ont été déterminées par les courbes de la fonction d'efficacité du récepteur.
Résultats
L'épanchement biliaire post-opératoire s'est présenté comme une fistule biliaire externe chez 31 (75,6 %) des 41 patients, comme une péritonite biliaire chez 6 patients (14,6 %) et comme une infection de la cavité biliokystique chez 4 patients (9,8 %). Les prédicteurs cliniques indépendants d'une CBC occulte, représentée par un épanchement biliaire, étaient : phosphatase alcaline > 250 U/L, bilirubine totale > 17,1 μmol/L, bilirubine directe > 6,8 μmol/L, gamma-glutamyl-transférase > 34,5 U/L, polynucléaires éosinophiles > 0,09 et diamètre du kyste > 8,5 cm. Les kystes multiloculaires ou dégénérés augmentent le risque d'épanchement biliaire (p < 0,012). Les taux de complication post-opératoires étaient de 53,7 % chez les patients avec épanchement biliaire et de 10,0 % (p < 0,001) chez les patients sans épanchement biliaire. Le séjour post-opératoire moyen à l'hôpital a été plus long chez les patients avec épanchement biliaire (14,3 [et écart-type {ET} 1,9] j) que chez les patients sans épanchement biliaire (7,3 [ET 2,3] j) (p < 0,001). Dix-neuf (61,3 %) des 31 fistules biliaires se sont refermées spontanément dans les 10 jours. Les 12 autres (38,7 %) fistules se sont refermées dans les 7 jours après une sphinctérotomie endoscopique.
Conclusion
: Les prédicteurs d'une CBC occulte à cause d'un kyste hydatique du foie ont été identifiés. Ces facteurs pourraient permettre d'établir la probabilité d'une CBC et, par conséquent, indiquer la nécessité de procédures chirurgicales supplémentaires pour prévenir les complications d'un épanchement biliaire.
Hydatid disease, which has been recognized since the time of Hippocrates, is a parasitic infection caused by Echinococcus granulosus.1 It is endemic in Turkey,2–6 where it presents a serious health problem, but it also occurs in nonendemic regions due to travel and migration.7,8 The liver is involved in 50%–70% of cases.1,9–11 Cystobiliary communication (CBC), which is the most common complication of hepatic hydatid cyst, occurs as a result of cyst rupture into the biliary system.12–14 Communication between cyst and biliary tree is between large and small biliary channels and has an incidence of 13%–37%.15–18 There are 2 types of intrabiliary rupture: frank and occult (silent).19 In frank CBC, cyst contents, such as hydatic debris, daughter cysts and major fragments of the germinative membrane, are found in the common bile duct.4,18,20 Biliary colic, obstructive jaundice and cholangitis due to complete or partial obstruction of the common bile duct by the elements of the hydatic cyst are common.16,21,22 Diagnosis is easy, and frank communication can be managed as a surgical or endoscopic procedure.2,9,11,17,18,23
In occult or silent CBC, cyst fluid, the scolices, the small daughter cysts and minor fragments of the endocyst membranes pass into the biliary tree, where they are invisible to x-rays. Clinical findings are nonspecific at this stage.24–26 Occult CBC may be recognized at surgery but, if it remains undetected or unrepaired, postoperative biliary leakage will ensue.16,27 This may result in complications such as prolonged biliary drainage, biliary peritonitis and biliary abscess, all of which increase morbidity and time spent in hospital.10,28 Thus, it is important to diagnose and treat CBC in the preoperative and intraoperative period. We therefore studied clinical parameters associated with the risk of occult CBC in the preoperative period, by recording clinical findings in patients who developed biliary leakage after hydatid liver surgery.
Methods
The records of 222 patients treated for hepatic hydatic cyst between January 1992 and December 2002 at Çukurova University School of Medicine Department of General Surgery, Turkey, were reviewed retrospectively. According to preoperative clinical findings, imaging studies or operative findings, 22 patients (9.9%) had frank intrabiliary rupture and 3 patients had choledocholithiasis. The clinical records of 6 patients were incomplete, so these data were excluded from the study. Of the remaining 191 patients, 41 (21.5%) had postoperative biliary leakage.
In occult intrabiliary rupture or CBC, small fistulae occur between the cyst and the biliary system, allowing cyst fluid, the scolices, small daughter cysts and minor fragments of the endocyst membranes to pass into the biliary tree. This condition frequently presents with postoperative biliary leakage, in spite of the lack of CBC symptoms preoperatively. The incidence of 21.5% in our sample is consistent with the description of CBC. Presentation took the form of biliary drainage from the abdominal drain in 31 (75.6%) of the 41 patients, as biliary peritonitis in 6 (14.6%) and as biliary abscess in the cyst cavity in 4 (9.8%).
The patients' records were reviewed, and the results were recorded on a standard form. This included age, sex, the region where the patient lived, findings on physical examination, laboratory data, cyst structure according to imaging studies, cyst size and location, whether the cyst was primary or recurrent, perioperative findings, postoperative endoscopic retrograde colangiopancreatography (ERCP) findings, time to closure of the biliary fistula, and the complications, mortality and duration of postoperative hospital stay. None of patients had ERCP preoperatively. Wound dehiscence was defined as separation of the abdominal wound, involving the anterior fascial sheath and deeper layers. Biliary peritonitis was diagnosed by physical examination and imaging methods. Depending on the presence of uncontaminated or infected bile, it was described as localized (i.e., adjacent to the diaphragm, liver, transverse colon and esophagus) or diffuse in the abdominal cavity at laparotomy. Cavity infections were identified by purulent drainage from cavity drains or the clinical findings of infection (fever and leukocytosis) combined with positive culture from drainage material.
Fistulae with an output above 300 mL/d were described as high output. All patients underwent a full blood cell count and the following liver function tests (alkaline phosphatase [ALP], γ-glutamyl transferase [GGT], alanine aminotransferase [ALT], aspartate aminotransferase [AST] and bilirubin). The upper normal limits for liver function tests were as follows: ALP, 270 U/L; GGT, 49 U/L; total bilirubin, 20.5 μmol/L; direct bilirubin, 6.8 μmol/L; ALT, 41 U/L; and AST, 37 U/L. The upper limit of normal for leukocytes was 10.3 × 109/L, and the upper normal limit for eosinophils was 0.06 of total leukocytes. Diagnosis was by ultrasonography and computed tomography in each case and was confirmed by indirect hemagglutination titrations. No CBC or any other pathology was found by imaging studies of the biliary system. Cysts were classified radiologically as unilocular (Gharbi type I and II), multilocular (Gharbi type III) or degenerate (Gharbi type IV).29,30
Patients were selected for treatment according to their condition and the characteristics of the cyst. The indications for surgery were complicated cysts (infected, or communicating with the biliary tree, or exerting pressure on adjacent organs and structures) and uncomplicated, large, peripherally located, hydatid cysts. Small, deep parenchymal cysts, less than 4 cm in diameter and asymptomatic, and calcified cysts in patients older than 65 years were treated conservatively. The type of procedure was decided by individual surgeons. Access was gained through the right subcostal or midline incision. The cyst was isolated from the peritoneal cavity with pads soaked in scolicidal solution. All surgery was conservative, including unroofing of the cyst by partial pericystectomy and cavity management. After the unroofing, the edges of the pericystium were sutured with interlocking absorbable sutures to avoid bile leakage and bleeding. Cavity management was by external drainage, omentoplasty or capitonnage, as decided by each surgeon. Povidone-iodine was used as scolicidal agent. Dilatation of the biliary system or cystobiliary opening was not seen intraoperatively; consequently, biliary opening repair or bile duct drainage was not performed. All patients received mebendazole (50 mg/kg per day) or albendazole (10 mg/kg per day) preoperatively and postoperatively. Twelve patients with a biliary fistula that failed to close spontaneously within the first 3 postoperative weeks, or a high-output fistula, underwent ERCP and endoscopic sphincterotomy. The biliary system was found to be normal, and no debris or any component of hydatid cyst was observed on ERCP.
Possible risk factors for biliary leakage were analyzed as potential predictors of CBC. Postoperative complications, morbidity rates and the duration of postoperative hospital stay were compared between the patients with and without biliary leakage.
The results are presented as mean (and standard deviation [SD]) and number (and percent). Because tests showed that the data were distributed normally for each continuous variable, Student's t test was used to evaluate the differences between groups for measured variables and the χ2 test was used for categorical variables. Significance was set at p < 0.05 in 2-tailed tests. The cutoff values of ALP, GGT, total and direct bilirubin, ALT, AST, eosinophils, leukocytes, cyst diameter, all of which were significant factors according to the t test, were determined by receiver operating characteristic (ROC) curve. Multivariate logistic regression analyses were used to assess the factors associated with biliary leakage. Demographic and clinical variables were first subjected to bivariate analyses. Those suggesting an association whereby p < 0.10 were included in multivariate analyses. We used the stepwise forward procedure with the following variables: ALP, GGT, total bilirubin, direct bilirubin, ALT, AST, eosinophils, leukocytes, cyst diameter and cyst type.
Results
A total of 217 cysts were treated in 191 patients, 72% of whom were female. The patients' mean age was 42.7 (SD 14) years. Of 191 patients, 140 (73%) came from rural areas and 51 (27%) from urban areas. The most common symptom was abdominal pain (79.1%). One-hundred and seventy-three patients (90.6%) had 1 cyst, the remaining 18 (9.4%) had multiple cysts. One-hundred and eighty-six patients (97.3%) underwent the first cyst operation in our clinic, the remainder had undergone operation elsewhere. The cysts were located in the right hepatic lobe in 150 (79%) patients, the left lobe in 29 (15%) and in both lobes in 12 (6%) patients. The mean cyst diameter was 8.7 (SD 3.0) cm. Of 217 cysts, 98 (45.1%) were unilocular, 71 (32.7%) were multilocular and 48 (22.1%) were degenerate. Of 191 dominant cysts, 171 (89.6%) underwent external drainage, 12 (6.2%) underwent omentoplasty and 8 (4.2%) underwent capitonnage.
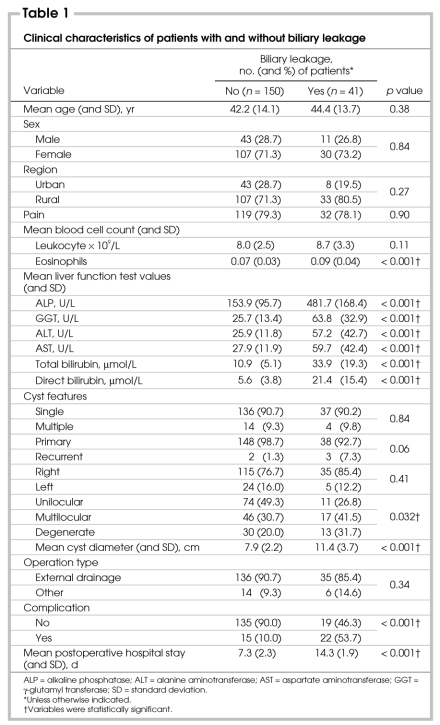
The demographic and clinical characteristics of the patients with and without biliary leakage are compared in Table 1. There were no differences in age, sex, place of residence and presence of abdominal pain between the 2 groups (p > 0.05). The frequency of biliary leakage was not affected by cysts being single or multiple (p = 0.84), primary or recurrent (p = 0.06) or in which hepatic lobe they occurred (p = 0.41).
Table 1
The biliary leakage rate was 20.5% (35/171) in patients who underwent external drainage and 30% (6/20) with other procedures. There was no relation between biliary leakage and type of operative procedure (p = 0.34). ALP, GGT, ALT, AST, total and direct bilirubin, eosinophil count and cyst diameter were all significantly higher in the biliary leakage group (p < 0.001). Multilocular or degenerate cysts increased the risk of biliary leakage (p = 0.012).
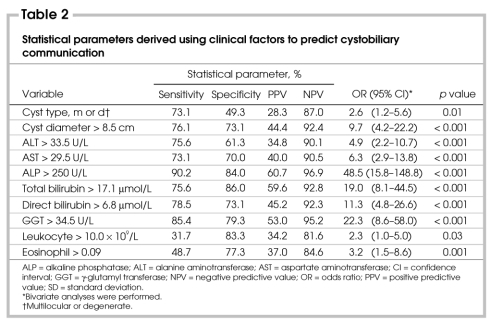
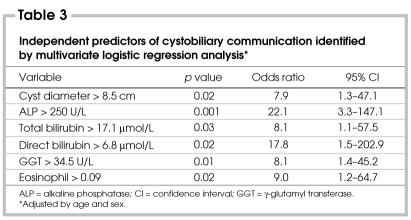
Cutoff values were 10.0 × 109/L for leukocyte count, 0.09 for eosinophil rate, 250 U/L for ALP, 34 U/L for GGT, 17.1 μmol/L for total bilirubin, 6.8 μmol/L for direct bilirubin, 33.5 U/L for ALT, 29.5 U/L for AST and 8.5 cm for cyst size. Table 2 shows the results of bivariate analyses for risk factors for occult CBC presenting as biliary leakage after hydatid liver surgery. Bivariate analysis showed that elevated findings on liver function tests preoperatively, eosinophilia, leukocytosis, larger cysts, and multilocular or degenerate cysts were significant clinical factors that increased the risk of occult CBC. The most significant clinical factor, in terms of increasing the risk of biliary leakage, was an ALP level greater than 250 U/L (positive predictive value 60.7). An ALP level greater than 250 U/L, a GGT level greater than 34.5 U/L, total bilirubin greater than 17.1 μmol/L, a direct bilirubin level above 6.8 μmol/L, eosinophils greater than 0.09 and cyst diameter greater than 8.5 cm were independent clinical predictors of occult CBC in multivariate logistic regression analysis (Table 3). The most significant clinical predictor was a raised preoperative ALP level (odds ratio 22.1).
Table 2
Table 3
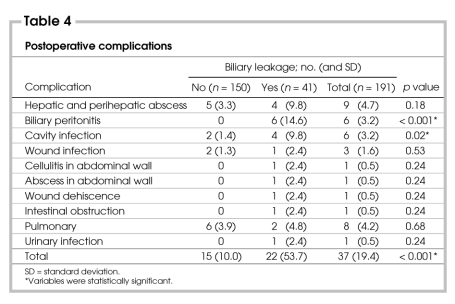
There was no mortality during our study. Postoperative complication rates were much higher in the patients with biliary leakage than those without (53.7% v. 10%, p < 0.001 [Table 4]). Biliary peritonitis developed in 6 patients, of whom 5 had localized peritonitis. One patient had generalized peritonitis and underwent omentoplasty plus T-tube drainage on the first postoperative day. The opening of the biliary channel could not be located, although the leakage was from the cyst cavity. Of the 5 patients with localized biliary peritonitis, 3 underwent reoperation on the third postoperative day and 2 on the fourth. Bile was found in perihepatic regions and cystic cavities, but no active biliary drainage was observed from the cyst cavity, and drainage was carried out in all 5 patients. Of 4 patients with biliary abscess (in the biliary leakage group), 3 were drained percutaneously and 1 surgically. Of 5 hepatic and perihepatic abscesses that developed in the patients without biliary leakage, 3 were drained percutaneously and 2 were treated surgically following unsuccessful percutaneous intervention. Cavity infection developed in 6 patients in the 2 groups. The patients were discharged abscess free following antibiotic and supportive therapy. The abdominal drain caused cellulitis and abscess in the abdominal wall of the patients with biliary leakage. It was treated by antibiotics and surgical drainage under local anesthesia. All other complications were treated medically.
Table 4
Biliary fistulae closed spontaneously within 10 days in 19 (61.3%) of the 31 patients, whereas those that took longer or had high-output fistulae closed within 7 days of endoscopic sphincterotomy in the other 12 (38.7%) patients. Mean closure time for all fistulae was 12.7 (SD 3.7) days. The mean postoperative hospital stay was 8.8 (SD 3.6) days and was significantly greater in patients with biliary leakage than those without (14.3 [SD 1.9] d v. 7.3 [SD 2.3] d, p < 0.001).
Discussion
Although communication between biliary system and cyst occurs in 80%–90% of patients with hepatic hydatid cyst, the incidence of clinical CBC is only 13%–37%.8,15–17,24,26 The criteria for CBC are visualization of a cystobiliary opening during operation or demonstration of communication by ERCP in patients with hydatid jaundice or biliary leakage after hydatid liver surgery.15 We studied occult intrabiliary rupture, which presents with biliary leakage, if the cystobiliary opening cannot be detected and repaired at operation.16,27 The incidence of frank intrabiliary rupture ranges between 5% and 17%.2,9,16 Although its mortality and morbidity are high, there are no significant problems with the management of CBC.17,18,31 However, occult CBC, which constitutes 10%–37% of cases, is difficult to diagnose, because the symptoms and preoperative radiological findings are unremarkable.32 In our study, 63 (28.4%) of the 222 patients had CBC, of which cases 41 (18.5%) were occult. Twenty-two patients with frank CBC (9.9%) were excluded from this study.
Intracystic pressure is 30–80 cm H2O, but normal biliary system pressure is 15–20 cm H2O.24,26,33 Flow is therefore toward the biliary system, and bile may not be present in the cavity despite occult CBC.34
In 1 prospective study of analyzed cavity contents, 45 cystobiliary fistulae were found. Six patients had hydatid jaundice in the preoperative period that was confirmed by ERCP. CBC was confirmed in 25 (64.1%) of the remaining 39 patients who had postoperative biliary leakage.15 Once the cyst has been drained, leakage follows because the pressure gradient is reversed, and bile flows into the residual cavity rather than through the papilla of Vater.12 That most of occult CBC cases appear as biliary leakage also supports this view.16,25,31 CBC is the most common complication of hepatic hydatid cyst, occurring in 14%–25% of cases of postoperative biliary leakage.15 The incidence of biliary leakage in our study was 21.5%. Biliary fistula develops when the postoperative leak is able to drain; if it cannot, biliary peritonitis and biliary abscess develop.10 Occult CBC significantly increases the complication rate.27 In our study, the complication rate was 10% in patients without biliary leakage, and 53.7% in those with leakage, which is consistent with the findings of other studies.10,27,31 In our patients, these complications necessitated additional surgical, percutaneous and endoscopic interventions and intensive care. Postoperative biliary leakage significantly increases postoperative hospital stay;15 here, the normal 7 days' stay was increased to 14 days, consistent with the study reported by Atli and colleagues.35 In the study by Kayaalp and colleagues,28 the stay in hospital was increased from 6 days to 17 days.
No significant difference was found between patients with and without biliary leakage in terms of age, sex, place of residence (rural or urban) and symptoms. The nature of the cysts, whether primary or recurrent, single or multiple, and their location (right lobe, left lobe or both), did not affect the risk of biliary leakage. These findings are consistent with those of other studies of CBC.28,35
Hepatectomy and pericystectomy are radical operations for hydatid liver cyst. Radical surgery carries a perioperative risk, but postoperative biliary leakage and recurrence are rare.36–38 The fistula is repaired in healthy tissue. Formal hepatectomy should only be performed by experienced surgeons, in specialized centres.31 Conservative surgery, which is preferred in endemic regions, carries a high incidence of postoperative biliary leakage and local recurrence.10,38 The main aims of conservative surgery are inactivation of viable elements of the parasite, evacuation of the cyst cavity and management of the residual cavity.2,6,10,30 All the patients in our study were treated conservatively. As reported by others,28,39 there were no differences in the incidence of biliary leakage between several types of conservative surgical treatment.
ALP concentrations greater than 250 U/L, a total bilirubin level above 17.1 μmol/L, direct bilirubin above 6.8 μmol/L, GGT greater than 34.5 U/L, eosinophils greater than 0.09 and cyst size greater than 8.5 cm in the preoperative period were independent predictors of occult CBC presenting as biliary leakage; ALP was the most important. A high intracystic pressure causing intermittent passage of cyst fluid, scolices and minor fragments into the biliary system can cause elevated ALP, GGT and bilirubin.24,26,35 Some studies report that these indices are more prominent in frank intrabiliary rupture than in the occult type.8,17,18,22 Elevated ALP and direct bilirubin were risk factors for occult CBC, as reported by Atli and colleagues.35 High ALP and GGT levels were risk factors for CBC according to Kayaalp and colleagues,28 who suggested that percutaneous treatment should be avoided in patients with increased ALP and GGT, because CBC contraindicates percutaneous treatment.40
Absorption of hydatid antigen following cyst rupture into biliary channels or the peritoneum may increase the eosinophil count. Eosinophilia has been reported in 29%–100% of patients with intrabiliary rupture.41–44 An eosinophil count exceeding 0.09, namely, significantly greater than in patients without biliary leakage, is an independent risk factor for CBC in our study. Humayun and colleagues42 found more than 10% eosinophilia in the presence of CBC.
Mean cyst diameter was significantly greater at 11.4 cm in patients with biliary leakage compared with 7.9 cm in those without. Cyst size above 8.5 cm was an independent predictor of occult CBC. Atli and colleagues35 found that cyst diameters of 14.5 cm or more independently predicted occult intrabiliary rupture, although Kayaalp and colleagues28 found that 65% of cysts that caused biliary leakage were less than 10 cm, and Bedirli and colleagues17 found a mean cyst diameter of 9 cm in 41 patients with intrabiliary rupture. The mean cyst size of 9.9 cm reported by Atli and colleagues in patients without biliary rupture exceeds that in other studies, but our sizes are consistent with those of others. We found occult CBC, represented by biliary leakage, to be more common with multilocular and degenerate cysts, as have others.17,28,35
How can the risk of biliary leakage from occult CBC be evaluated preoperatively, and what should be done intraoperatively? The independent clinical predictors, determined by multivariate analysis, should be investigated preoperatively. Because the contents and other components of the cyst are drained into the biliary system, preoperative ERCP may demonstrate both biliary dilatation and communication with the cyst in patients with frank intrabiliary rupture. But occult CBC cannot be demonstrated preoperatively by ERCP because of the high intracystic pressure and small communication.24 Consequently, cystobiliary openings may be found following surgery in patients with occult CBC in the presence of independent clinical predictors. After partial cystectomy and cyst evacuation, cyst contents and signs of communication with the biliary system should be carefully sought. Özmen and Coskun34 describe an easy and reliable technique, using a telescope, for finding the communication opening via direct visualization during conservative surgery for hydatid liver cysts in situations in which visualization of the cavity is difficult. Communication between the cyst and biliary tree was found and sutured in 6 of 18 patients, and no postoperative biliary leakage developed.
If the opening of the biliary channel into the cyst cavity cannot be located, the cyst should be filled with saline and air injected from the cystic duct. Alternatively, methylene blue can be injected into the gallbladder or common bile duct; bubbles or methylene blue will reveal the opening.26 Jabbour and colleagues45 reported that decompression of the biliary system through the cystic duct prevents bile leakage from occult communications and, therefore, decreases the risk of infectious complications. After complete unroofing of the cyst, the CBC was identified via air injected from the cystic duct. These communications were then sutured, and cavity management was performed by omentoplasty. In 1 of the 6 patients, a Roux-en-Y hepaticojejunostomy was performed because of distal common bile duct stricture. In 4 patients, cystic duct drainage was performed for biliary decompression. In the other patient without prophylactic drainage, a persistent bile leak developed postoperatively.
These procedures usually require cholecystectomy and could cause confusion later, if it fails to identify the opening. Another method is to pack the cyst with gauze soaked in hypertonic saline and wait for bile stains to appear. We use povidone-iodine as a scolicidal agent; it colours the cyst cavity, making it difficult to identify CBC if bile does not appear immediately, and thus some biliary leakage from occult CBC was seen postoperatively in our study too. Another risk of giving the scolicidal agent after aspirating the cyst is that of caustic sclerosing cholangitis.26
If occult CBC is found, the opening in the biliary system should be sutured with absorbable material, with or without cystic duct drainage. If no biliary opening is found, cystic duct drainage may be performed if preoperative factors predict the presence of CBC. Cavity management can then be performed by omentoplasty or external drainage, preferably with suction drainage. External biliary fistula is the most common postoperative complication of hydatid liver surgery in endemic regions.46 The frequency ranges from 6% to 28%;1–3 it was 16.2% in our study. Although most external biliary fistulae close spontaneously, they persist in 4%–27.5% of cases.25 Nineteen (61.3%) of 31 external biliary fistulae closed spontaneously in our study. Endoscopic sphincterotomy is indicated in biliary fistula of more than 3 weeks' duration or with output exceeding 300 mL/d.10,29 Saritas and colleagues13 treated 45 patients, Dolay and colleagues25 treated 33 patients, and Tekant and colleagues47 treated 9 patients successfully with endoscopic procedures. Fistula closure time after endoscopic treatment was reported to be 17 days, 10 days and 7 days, respectively. In this study, 12 cases of delayed closure or of high-output fistulae closed within 7 days of endoscopic sphincterotomy. The policy of sphincterotomy for high-output fistulae increased the use of endoscopic methods in our study.
Conclusion
We found that occult CBC presenting as biliary leakage following hydatid liver surgery can be predicted by levels of ALP, GGT, total and direct bilirubin, eosinophils and cyst diameter. Multilocular or degenerate cysts were found to be important predictors of CBC. Postoperative biliary leakage was associated with increased morbidity and a prolonged stay in hospital. Additional procedures performed in the intraoperative period help prevent complications due to biliary leakage by allowing determination of CBC. We suggest that when postoperative biliary fistula develops despite all preventive measures, it should first be treated by conservative methods, and with endoscopic procedures if it persists.
Competing interests: None declared.
Correspondence to: Prof. Orhan Demircan, Çukurova University, School of Medicine, Department of General Surgery, Balcali Hastanesi, 01330 Balcali, Adana, Turkey; fax 90 322 338 64 32; odemircan@cu.edu.tr
References
- 1.Sayek I, Yalin R, Sanac Y. Surgical treatment of hydatid disease of the liver. Arch Surg 1980;115:847-50. [DOI] [PubMed]
- 2.Akinoglu A, Bilgin I, Erkoçak EU. Surgical management of hydatid disease of the liver. Can J Surg 1985;28:171-4. [PubMed]
- 3.Demirci S, Eraslan S, Anadol E. Comparison of different surgical techniques in the management of hydatid cysts of the liver. World J Surg 1989;13:88-90. [DOI] [PubMed]
- 4.Ulualp KM, Aydemir I, Senturk H, et al. Management of intrabiliary rupture of hydatid cyst of the liver. World J Surg 1995; 19:720-4. [DOI] [PubMed]
- 5.Balik AA, Basoglu M, Çelebi F, et al. Surgical treatment of hydatid disease of the liver. Review of 304 cases. Arch Surg 1999; 134:166-9. [DOI] [PubMed]
- 6.Erdem E, Nessar M, Sungurtekin U, et al. The management of hydatid cyst: review of 94 cases. J Hepatobiliary Pancreat Surg 1998; 5:179-83. [DOI] [PubMed]
- 7.Pitt HA, Korzelius J, Tompkins RK. Management of hepatic echinococcosis in Southern California. Am J Surg 1986; 152: 110-5. [DOI] [PubMed]
- 8.Langer JC, Rose DB, Keystone JS, et al. Diagnosis and management of hydatid disease of the liver. Ann Surg 1984; 199: 412-7. [DOI] [PMC free article] [PubMed]
- 9.Akkiz H, Akinoglu A, Çolakoglu S, et al. Endoscopic management of biliary hydatid disease. Can J Surg 1996;39:287-92. [PMC free article] [PubMed]
- 10.Skroubis G, Vagianos C, Polydorou A, et al. Significance of bile leaks complicating conservative surgery for liver hydatidosis. World J Surg 2002;26:704-8. [DOI] [PubMed]
- 11.Al Karawi MA, Yasawy MI, El Shiekh Mohamed AR. Endoscopic management of biliary hydatid disease: report on six cases. Endoscopy 1991; 23:278-81. [DOI] [PubMed]
- 12.Vignote ML, Mino G, de la Mata M, et al. Endoscopic sphincterotomy in hepatic hydatid disease open to the biliary tree. Br J Surg 1990;77:30-1. [DOI] [PubMed]
- 13.Saritas U, Parlak E, Akoglu M, et al. Effectiveness of endoscopic treatment modalities in complicated hepatic hydatid disease after surgical intervention. Endoscopy 2001;33:858-63. [DOI] [PubMed]
- 14.Koksal N, Muftuoglu T, Gunerhan Y, et al. Management of intrabiliary ruptured hydatid disease of the liver. Hepatogastroenterology 2001;48:1094-6. [PubMed]
- 15.Kayaalp C, Bostanci B, Yol S, et al. Distribution of hydatid cysts into the liver with reference to cystobiliary communications and cavity-related complications. Am J Surg 2003;185:175-9. [DOI] [PubMed]
- 16.Alper A, Ariogul O, Emre A, et al. Choledochoduodenostomy for intrabiliary rupture of hydatid cysts of liver. Br J Surg 1987; 74:243-5. [DOI] [PubMed]
- 17.Bedirli A, Sakrak O, Sozuer EM, et al. Surgical management of spontaneous intrabiliary rupture of hydatid liver cysts. Surg Today 2002;32:594-7. [DOI] [PubMed]
- 18.Kornaros SE, Aboul-Nour T. Frank intrabiliary rupture of hydatid hepatic cyst: diagnosis and treatment. J Am Coll Surg 1996; 183:466-70. [PubMed]
- 19.Hankins JR. Management of complicated hydatid cysts. Ann Surg 1963;158:1020-34. [DOI] [PMC free article] [PubMed]
- 20.Marti-Bonmati L, Menor F, Ballesta A. Hydatid cyst of the liver: rupture into the biliary tree. AJR Am J Roentgenol 1988; 150:1051-3. [DOI] [PubMed]
- 21.Ovnat A, Peiser J, Avinoah E, et al. Acute cholangitis caused by ruptured hydatid cyst. Surgery 1984;95:497-500. [PubMed]
- 22.Lygidakis NJ. Diagnosis and treatment of intrabiliary rupture of hydatid cyst of the liver. Arch Surg 1983;118:1186-9. [DOI] [PubMed]
- 23.Giouleme O, Nikolaidis N, Zezos P, et al. Treatment of complications of hepatic hydatid disease by ERCP. Gastrointest Endosc 2001;54:508-10. [DOI] [PubMed]
- 24.Ozaslan E, Bayraktar Y. Endoscopic therapy in the management of hepatobiliary hydatid disease. J Clin Gastroenterol 2002; 35:160-74. [DOI] [PubMed]
- 25.Dolay K, Akçakaya A, Soybir G, et al. Endoscopic sphincterotomy in the management of postoperative biliary fistula. A complication of hepatic hydatid disease. Surg Endosc 2002;16:985-8. [DOI] [PubMed]
- 26.Milicevic H. Hydatid disease. In: Blumgart L, Fong Y, editors. Surgery of the liver and biliary tract. 2nd ed. Philadelphia: WB Saunders Company; 2000. p. 1167-204.
- 27.Magistrelli P, Masetti R, Coppola R, et al. Surgical treatment of hydatid disease of the liver. A 20-year experience. Arch Surg 1991; 126:518-23. [DOI] [PubMed]
- 28.Kayaalp C, Bzeizi K, Demirbag AE, et al. Biliary complications after hydatid liver surgery. Incidence and risk factors. J Gastrointest Surg 2002;6:706-12. [DOI] [PubMed]
- 29.Gharbi HA, Hassine W, Brauner MW, et al. Ultrasound examination of the hydatic liver. Radiology 1981;139:459-63. [DOI] [PubMed]
- 30.Kayaalp C. Evacuation of hydatid liver cysts using laparoscopic trocar. World J Surg 2002;26:1324-7. [DOI] [PubMed]
- 31.Zaouche A, Haouet K, Jounini M, et al. Management of liver hydatid cysts with a large biliocystic fistula: multicenter retrospective study. World J Surg 2001;25:28-9. [DOI] [PubMed]
- 32.Becker K, Frieling T, Saleh A, et al. Resolution of hydatid liver cyst by spontaneous rupture into the biliary tract. J Hepatol 1997; 26:1408-12. [DOI] [PubMed]
- 33.Yalin R, Aktan AÖ, Yegen C, et al. Significance of intracystic pressure in abdominal hydatid disease. Br J Surg 1992;79:1182-3. [DOI] [PubMed]
- 34.Özmen M, Coskun F. New technique for finding the ruptured bile duct into the liver cyst: scope in the cave technique. Surg Laparosc Endosc Percutan Tech 2002; 12:187-9. [DOI] [PubMed]
- 35.Atli M, Kama NA, Yuksek YN, et al. Intrabiliary rupture of a hepatic hydatid cyst. associated clinical factors and proper management. Arch Surg 2001;136:1249-55. [DOI] [PubMed]
- 36.Giordano G, Angrisano A, Palazzo P, et al. Surgical treatment of hydatid cyst of the liver: pericystectomy or resection. Personal experience. Int J Surg Sci 1999; 6: 113-7.
- 37.Moreno Gonzalez E, Rico Selas P, Martinez B, et al. Results of surgical treatment of hepatic hydatidosis: current therapeutic modifications. World J Surg 1991;15:254-63. [DOI] [PubMed]
- 38.Kayaalp C, Sengul N, Akoglu M. Importance of cyst content in hydatid liver surgery. Arch Surg 2002;137:159-63. [DOI] [PubMed]
- 39.Dziri C, Paquet JC, Hay JM, et al. Omentoplasty in the prevention of deep abdominal complications after surgery for hydatid disease of the liver. A multicenter, prospective, randomized trial. J Am Coll Surg 1999; 188:281-9. [DOI] [PubMed]
- 40.Bret PM, Fond A, Bretagnolle M, et al. Percutaneous aspiration and drainage of hydatid cysts in the liver. Radiology 1988; 168:617-20. [DOI] [PubMed]
- 41.Van Steenbergen W, Fevery J, Broeckaert L, et al. Hepatic echinococcosis ruptured into the biliary tract. Clinical, radiological, and therapeutic features during five episodes of spontaneous biliary rupture in three patients with hepatic hydatosis. J Hepatol 1987;4:133-9. [DOI] [PubMed]
- 42.Humayun MS, Rady AM, Soliman GM. Obstructive jaundice secondary to intra-biliary rupture of hepatic hydatid cyst. Int Surg 1989;74:4-6. [PubMed]
- 43.Kattan YB. Intrabiliary rupture of hydatid cyst of the liver. Br J Surg 1975;62:885-90. [DOI] [PubMed]
- 44.Stavorovsky M, Wientroub S, Iellin A, et al. Rupture of a hydatid cyst of liver into the biliary tract. Int Surg 1977;62:603-8. [PubMed]
- 45.Jabbour N, Shirazi SK, Genyk Y, et al. Surgical management of complicated hydatid disease of the liver. Am Surg 2002; 68: 984-8. [PubMed]
- 46.Dadoukis J, Prousalidis J, Botsios D, et al. External biliary fistula. HPB Surg 1998; 10: 375-7. [DOI] [PMC free article] [PubMed]
- 47.Tekant Y, Bilge O, Acarli K, et al. Endoscopic sphincterotomy in the treatment of postoperative biliary fistulas of hepatic hydatid disease. Surg Endosc 1996;10:909-11. [DOI] [PubMed]