Abstract
The authors report a case of a young male with median arcuate ligament syndrome (MALS). An abnormally low insertion of the median arcuate ligament fibres caused extrinsic compression and stenosis of the coeliac trunk. However, partial dissection of ligament fibres by laparoscopic surgery did not relieve abdominal angina. Multidetector CT confirmed that MALS did not differ from the preoperative scan. The arcuate ligament compressed the coeliac trunk on expiration, thereby eliciting occlusion of the coeliac trunk. Inspiration induced decompression of the ligament with partial release of occlusion of the coeliac trunk. This leads to hypo-perfusion of intestinal organs and abdominal angina. Considering the severe impairment of quality of life, open surgery for decompression of the coeliac trunk with vascular reconstruction is a reasonable option.
Background
Median arcuate ligament syndrome (MALS) is an unusual condition caused by abnormally low insertion of the median arcuate ligament fibres, resulting in compression and luminal narrowing of the coeliac trunk. These fibres connect the right and left crura of the diaphragm and define the anterior margin of the aortic hiatus. The coeliac trunk supplies blood to digestive splanchnic organs through left gastric, common hepatic and splenic arteries. Supply to the intestines includes the coeliac trunk , superior mesenteric artery (SMA) and inferior mesenteric artery (IMA). The coeliac trunk is an essential source of blood because the interconnections with the SMA and IMA are not adequate to sustain sufficient perfusion to splanchnic organs. MALS has been described as a rare disorder. A prevalence of 1.7% has been reported in a series of 3449 young patients.1 A PubMed search carried out to identify articles from 2008 to June 2011 detected only 33 articles. We used the keywords ‘median arcuate ligament syndrome’, ‘coeliac artery compression syndrome’ and ‘Dunbar’s syndrome’ in this search.
Case presentation
In March 2011, a 25-year-old male presented to us with asthenia, postprandial discomfort, episodes of diarrhoea, weight loss as well as abdominal pain upon physical effort. Gastrointestinal investigations were inconclusive. Examination revealed a bruit on the midepigastrium and a body mass index of 16 kg/m2. In November 2008, the patient underwent unsuccessful laparoscopic surgery for MALS with partial dissection of ligament fibres.
Investigations
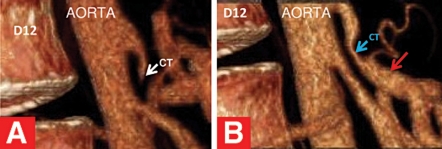
In April 2011, multidetector CT (MDCT) confirmed that MALS did not differ from the preoperative scan. The arcuate ligament compressed the coeliac trunk on expiration, thereby eliciting occlusion of the coeliac trunk (figure 1A). Inspiration induced decompression of the ligament with partial release of occlusion of the coeliac trunk (figure 1B). Poststenotic dilation was observed (figure1B). The gastroduodenal artery and splenic artery (figure 2) were conspicuously dilated in response to the increased blood flow diverted from pathways with the SMA. This haemodynamic response led to intestinal hypo-perfusion by a ‘SMA steal’ mechanism.
Figure 1.
MDCT sagittal three-dimensional volume-rendered images. (A) Occlusion of the coeliac trunk with a ‘hook-like’ appearance on expiration (white arrow). (B) Release of occlusion of the coeliac trunk during inspiration (blue arrow); poststenosis dilation (red arrow).
Figure 2.

MDCT coronal three-dimensional volume-rendered images. Dilated gastroduodenal artery (red arrow) and splenic artery (green arrow). The gastroduodenal artery is a subdivision of the common hepatic artery and a branch of the coeliac trunk. The splenic artery is a branch of the coeliac trunk (yellow arrow). The calibre of these arteries appears to be increased by more than two-thirds when compared with that of normal patients.
Differential diagnosis
Chronic intestinal ischaemia is most likely caused by atherosclerosis and less frequently by external compression, fibromuscular dysplasia and vasculitis.2 Symptomatic coeliac trunk-dynamic stenosis is an uncommon, potentially underdiagnosed condition of hypo-perfusion of the digestive splanchnic organs .This vascular disorder may involve diverse revascularisation strategies . The use of MDCT during respiration phases is an established method for the diagnosis of MALS.
Treatment
Guidelines for MALS treatment are not available. Therapy remains equivocal.
Outcome and follow-up
During the last few years, this vascular disorder deeply affected the patient’s social life. He reduced his number of heavy physical activities, gave up sporting activities and intentionally limited his daily intake of food.
Discussion
Under resting conditions, visceral multiple connections through the SMA and IMA fulfil intestinal metabolic needs. However, if metabolic demands exceed the supply of blood, intestinal ischaemia occurs with abdominal discomfort, diarrhoea, food avoidance, weight loss or abdominal angina. Laparoscopic surgery has a potential for vascular injury and adjunctive interventions.3 Angioplasty or stenting under CT guidance are inadequate if undertaken without release of the extrinsic compression.4 Poststenotic dilation and collateral dilated vessels have the potential to evolve into aneurysms with risk of rupture and sudden death.5 Taking into consideration the impairment of quality of life and previous unsuccessful laparoscopic surgery, the evaluation of open surgery for decompression of the coeliac trunk with vascular reconstruction is a reasonable option.6 In a young patient, the triad of midabdominal bruit, weight loss and undiagnosed gastrointestinal symptoms might suggest MALS. In such cases, the use of a widely available technique such as colour Doppler sonography is the method of choice for initial imaging of this vascular disorder.
Learning points.
-
▶
MALS is a rare (but often underdiagnosed) vascular disorder.
-
▶
CT undertaken during respiration phases is an established method for the diagnosis of MALS.
-
▶
Angioplasty or stenting are inadequate if undertaken without release of the extrinsic compression.
-
▶
Colour Doppler sonography is the method of choice for initial imaging in young patients.
Acknowledgments
The authors acknowledge Dr Angelo Gorini for his valid technical help.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Scholbach T. Celiac artery compression syndrome in children, adolescents, and young adults: clinical and color duplex sonographic features in a series of 59 cases. J Ultrasound Med 2006;25:299–305 [DOI] [PubMed] [Google Scholar]
- 2.Zeller T, Macharzina R. Management of chronic atherosclerotic mesenteric ischemia. VASA 2011;40:99–107 [DOI] [PubMed] [Google Scholar]
- 3.Roseborough GS. Laparoscopic management of celiac artery compression syndrome. J Vasc Surg 2009;50:124–33 [DOI] [PubMed] [Google Scholar]
- 4.Delis KT, Gloviczki P, Altuwaijri M, et al. Median arcuate ligament syndrome: open celiac artery reconstruction and ligament division after endovascular failure. J Vasc Surg 2007;46:799–802 [DOI] [PubMed] [Google Scholar]
- 5.Sugiyama K, Takehara Y. Analysis of five cases of splanchnic artery aneurysm associated with coeliac artery stenosis due to compression by the median arcuate ligament. Clin Radiol 2007;62:688–93 [DOI] [PubMed] [Google Scholar]
- 6.Grotemeyer D, Duran M, Iskandar F, et al. Median arcuate ligament syndrome: vascular surgical therapy and follow-up of 18 patients. Langenbecks Arch Surg 2009;394:1085–92 [DOI] [PubMed] [Google Scholar]