Abstract
A young, previously well primigravida presented a few hours after a short labour with sudden onset chest pain, shortness of breath and odynophagia. She had subcutaneous emphysema but did not have significant cardiorespiratory compromise. She was found to have a spontaneous pneumomediastinum, likely secondary to raised intrathoracic pressure during labour. Similar cases have been reported previously, however there are often risk factors associated such as pre-existing lung disease and illicit drug use for which this patient did not have a significant history. The patient made a speedy recovery without requiring invasive management, as is the case for most patients documented in the literature. Consideration should be given to subsequent labours for this patient to minimise excessive intrathoracic pressure, however recurrence is rarely documented. This case is useful for healthcare professionals in assessing patients with chest pain as a reminder that unusual presentations can be diagnosed through thorough history and examination.
Background
This case demonstrates an unusual cause of chest pain, shortness of breath and odynophagia in a fit young postpartum woman. The symptoms in combination with subcutaneous emphysema are worrying findings for a clinician. However, thorough history, examination, monitoring and investigation ruled out serious pathology and led to the diagnosis of spontaneous pneumomediastinum ‘Hamman’s syndrome’. This unusual diagnosis is thought to be caused by excessive intrathoracic pressures during labour causing air leakage into the mediastinal and subcutaneous tissues. Fortunately, it tends to run a benign course and resolve within days to weeks, and recurrence is thought to be low.
This report serves to remind us that thorough assessment is essential and can reveal unusual causes for common symptoms such as chest pain and shortness of breath.
Case presentation
The patient is an 18-year-old unemployed primigravida who was previously fit and well, with no significant medical history or family history. She took no medications and no illicit drugs at any time. She had smoked occasionally in social situations and very rarely drank small amounts of alcohol prior to becoming pregnant. She had an uncomplicated pregnancy. She had a spontaneous onset of labour at 39+2 weeks. Labour was short–first stage was 4 h; second stage 7 min; third stage 12 min. The only analgesia she used was gas and air. She had a first degree tear, and there was a total estimated blood loss of 250 mls.
About 8 h postdelivery, she reported chest pain and shortness of breath to the midwife looking after her. She was subsequently assessed by the on call doctor. She reported a sharp central chest pain which had come on suddenly about 1 h postdelivery, and had increased in severity since then and felt worse lying flat and on movement. Pain score varied from 3 (at rest) to 8/10 (on movement). Shortness of breath and a feeling of ‘bubbles over the chest’ were associated. She had vomited twice during the first and second stage of labour and once postdelivery. About an hour later, she had a cup of water and milk, with which she reported odynophagia. She had not had any haematemesis nor any subsequent vomiting, cough or any other systemic upset on enquiry.
On examination, she appeared comfortable at rest, but distressed on movement. Airway was patent, respiratory rate 22 and oxygen saturation from pulse oximetry 99% on air. There was diffuse subcutatneous emphysema palpable over the neck and chest, but chest was clear on auscultation with air entry throughout. Heart rate was 92 with regular rhythm, blood pressure was 116/76 and capillary refill time was less than 2 s. Heart sounds were normal. Examination was otherwise normal.
Investigations
Electrocardiogram was normal. Chest radiograph (figure 1) demonstrated evidence of pneumomediastinum and subcutaneous emphysema within the soft tissues of the neck. The lungs were clear.
Figure 1.
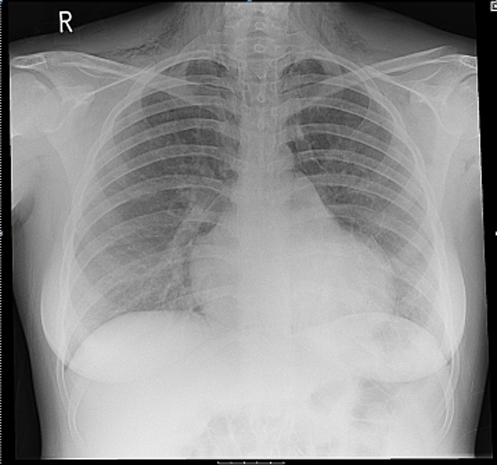
Chest radiograph demonstrating subcutaneous emphysema and pneumomediastinum.
Contrast enhanced CT (figure 2A,B) postcontrast demonstrated extensive pneumomediastinum tracking along the length of the mediastinum up into the neck with extensive subcutaneous emphysema and a small amount of gas also tracking down along the aortic and oesophageal hiatus. There were also tiny apical rims of extrapulmonary gas on both sides and pulmonary interstitial emphysema with a small amount of gas tracking along the interstitium of both lungs. Postoral contrast, contrast was present within the stomach but there was no extraluminal oral contrast in the mediastinum to suggest an oesophageal rupture.
Figure 2.

(A,B) Coronal and axial CT images more clearly demonstrating pneumomediastinum and subcutaneous emphysema.
Differential diagnosis
The diagnosis was of pneumomediastinum and subcutaneous emphysema. There was a concern that this could be due to an oesophageal tear due to vomiting during labour. Once this was ruled out, the likely aetiology was thought to be spontaneous pneumomediastinum secondary to raised intrathoracic pressure during labour.
Treatment
Treatment was intially supportive. Continuous non-invasive monitoring was done, but supplemental oxygen therapy was not required. She was kept nil by mouth and given broad-spectrum intravenous antibiotics until contrast CT was performed to rule out oesophageal rupture. She later had oral analgesia for pain but had declined any parenteral analgesia.
Outcome and follow-up
The patient was transferred to a tertiary referral centre where she was treated conservatively for 3 days. On further review of the CT, they felt it was likely that the aetiology was that of a very small ruptured bulla or alveoli secondary to raise intrathoracic pressure during labour. She was discharged with follow-up 2 weeks later, at which time she was well. She was advised to have obstetric review in future pregnancies for discussion around labour to minimise significant rise in intrathoracic pressure.
Discussion
A spontaneous pneumomediastinum (SP) occurs when free air enters into the mediastinum that has not been proceeded by trauma or a medical procedure. SP can be encountered in a variety of clinical settings, however published data on the topic are limited; in the region of 200 cases, which have been previously published.
The signs and symptoms of SP are typically of sudden onset and include shortness of breath, chest pain or neck pain and subcutaneous emphysema.1–6 Chest pain is the predominant symptom in the majority of cases.7 8
There are associated risk factors including vomiting, coughing and inhalational drug abuse.1 Several structural lung diseases including bronchiectasis, asthma, emphysema and intersitial lung disease can predispose to the development of SP.1 One study of 42 patients found cocaine consumption to be the most important predisposing factor.8 However, it may occur in isolation of risk factors as was the case with our patient.
SP is typically associated with a benign clinical course. The most common complication is the development of a concomitant pneumothorax; previous studies have found a frequency ranging from 6% to 32%.1 7 The risk of developing this is higher in patients with co-existing lung disease. Other complications include a tension penumomediastinum which occurs when air enters the mediastinum via a 1-way valve leading to increased pressure, this can impair venous return and cardiac function, and as such can be life threatening.9
SP is usually diagnosed with chest x-ray and/or CT. Chest x-ray has been shown to be a sensitive means to diagnosis SP, previous studies have found between 91% and 95% cases to be diagnosed by chest x-ray alone.3 7 In addition to picking up the SP too small to be seen on chest x-ray, CT also has the advantage of showing other evidence of underlying or associated disease, as such should be the mainstay investigation. It is also suggested that further diagnostic tests including oesophogastroduodenoscopy and bronchoscopy offer little further information in patients with SP.2 4–6
SP is managed conservatively, with supportive oxygen and analgesia as required. The rate of recurrence is unknown but thought to be low. Despite this and the usually benign course that the syndrome takes, it is thought to be sensible to monitor women in subsequent labours due to the rare but possibly serious consequences.
Learning points.
-
▶
Thorough assessment is vital. Even when faced with an unfamiliar scenario, by using basic principles and an understanding of physiology it is possible to work out the diagnosis.
-
▶
It is important to rule out serious causes for this constellation of symptoms such as an oesophageal tear in this case, and other more common causes of chest pain and shortness of breath.
-
▶
Spontaneous pneumomediastinum more often occurs in those with pre-existing lung disease, smoking or drug use and prolonged labour, however it can occur in absence of these risk factors.
-
▶
The syndrome tends to run a benign course, however when complications do occur they are potentially life threatening and therefore careful monitoring is advised.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Newcomb AE, Clarke CP. Spontaneous pneumomediastinum: a benign curiosity or a significant problem? Chest 2005;128:3298–302 [DOI] [PubMed] [Google Scholar]
- 2.Macia I, Moya J, Ramos R, et al. Spontaneous pneumomediastinum: 41 cases. Eur J Cardiothorac Surg 2007;31:1110–4 [DOI] [PubMed] [Google Scholar]
- 3.Kaneki T, Kubo K, Kawashima A, et al. Spontaneous pneumomediastinum in 33 patients: yield of chest computed tomography for the diagnosis of the mild type. Respiration 2000;67:408–11 [DOI] [PubMed] [Google Scholar]
- 4.Koullias GJ, Korkolis DP, Wang XJ, et al. Current assessment and management of spontaneous pneumomediastinum: experience in 24 adult patients. Eur J Cardiothorac Surg 2004;25:852–5 [DOI] [PubMed] [Google Scholar]
- 5.Takada K, Matsumoto S, Hiramatsu T, et al. Management of spontaneous pneumomediastinum based on clinical experience of 25 cases. Respir Med 2008;102:1329–34 [DOI] [PubMed] [Google Scholar]
- 6.Abolnik I, Lossos IS, Breuer R. Spontaneous pneumomediastinum. A report of 25 cases. Chest 1991;100:93–5 [DOI] [PubMed] [Google Scholar]
- 7.Iyer VN, Joshi AY, Ryu JH. Spontaneous pneumomediastinum: analysis of 62 consecutive adult patients. Mayo Clin Proc 2009;84:417–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perna V, Vila E, Guelbenzu J, et al. Pneumomediastinum: is this really a benign entity? When it can be considered as spontaneous? Our experience in 47 adult patients. Eur J Cardiothorac Surg 2010;37:573–5 [DOI] [PubMed] [Google Scholar]
- 9.Gabor SE, Renner H, Maier A, et al. Tension pneumomediastinum after severe vomiting in a 21-year-old female. Eur J Cardiothorac Surg 2005;28:502–3 [DOI] [PubMed] [Google Scholar]


