Abstract
Chronic meningitis can be difficult to diagnose. The authors report the case of an older Caucasian lady, with no underlying immunocompromising factors, who presented with a 2 month history of confusion. Due to the non-specific symptoms on presentation, a diagnosis was only obtained after a repeat CT scan of the brain, which showed hydrocephalus. Subsequent cerebrospinal fluid analysis showed biochemical abnormalities and Cryptococcus neoformans on staining.
Background
Chronic confusion in the older may have a number of contributing factors. Chronic meningitis is a difficult diagnosis to make due to the non-specific symptoms that the patient may present with (as highlighted in the existing literature). In our experience, this case highlights this diagnostic difficulty especially due to the unusual presentation of cryptococcal disease in an otherwise apparently immunocompetent older Caucasian individual from the Greater London region. Although the literature on this form of meningitis largely relates to the HIV population, our research shows a small but growing number of reports of this particular infection in individuals with no immunocompromising predisposing factors. The national meningitis research foundation (UK) was unable to provide us with an accurate number of incidences of cryptococcal meningitis.
This case report helps to add to the limited literature that exists on this topic, thereby building our knowledge base on its’ mode of presentation and likely clinical course. We hope to promote an early diagnosis of the condition to prevent significant morbidity and mortality.
Case presentation
An older woman presented to hospital on two separate occasions with confusion. Her initial presentation was with a 1 month history of confusion and lethargy. She had a background of hypertension and hypercholesterolaemia. Her drug history consisted of aspirin, propanolol, candesartan and simvastatin and she did not smoke or consume alcohol. She was previously independent, self-caring and had no background of cognitive impairment. Examination of all systems was unremarkable and investigations revealed serum sodium of 119 with all other blood tests being normal. Candesartan was stopped. Further blood results were compatible with a picture of syndrome of inappropriate antidiuretic hormone hypersecretion (SIADH) and additional biochemical tests did not reveal any other causes of her hyponatraemia or confusion. CT head showed minor age related involutional changes. She was treated with fluid restriction and consequently demeclocycline. With the return of serum sodium to normal her cognition also improved and she was discharged 15 days after admission.
She presented again to hospital 2 months later with a 5 week history of increasing confusion (Abbreviated Mental Test Score (AMTS) 4/10, Glasgow Coma Scale (GCS) 14/15), lethargy, decreased mobility, reduced oral intake and urinary incontinence. She was still taking demeclocycline and no new drugs had been started. Examination revealed left basal crepitations and she did not have any features of meningism or any focal neurological deficit. Laboratory tests revealed raised white cell count of 21.3 (neutrophilia), urea (45.3) and creatinine (216). Other tests were normal (including complement, antineutrophil cytoplasmic antibodies, urinary Bence Jones protein, haematinics, calcium levels and thyroid function). Her chest radiograph revealed lower zone consolidation. A diagnosis of sepsis secondary to community acquired pneumonia and acute kidney injury secondary to sepsis and dehydration was made.
Despite treatment with intravenous augmentin and other supportive measures, her confusion and cognitive state continued to worsen with an AMTS of 0/10 and GCS of 9/15. She started to spike temperatures. Blood and urine cultures revealed no organisms. CT brain showed enlarged lateral ventricles, 3rd ventricle and occipital horns. A lumbar puncture revealed an opening pressure of 36 cmH20, protein 3.71, glucose 1.3 (serum glucose 8.7)) and no white cells were seen. Antibiotics were changed to tazocin and teicoplanin. Over the next 24 h, however, her condition deteriorated with worsening signs of sepsis. She developed generalised seizures and subsequently died.
After death the cerebrospinal fluid CSF culture showed Cryptococcus neoformans (on India ink staining), with cryptococcal antigen testing positive on serology indicating the patient had crytococcal meningoencephalitis (figure 1).
Figure 1.
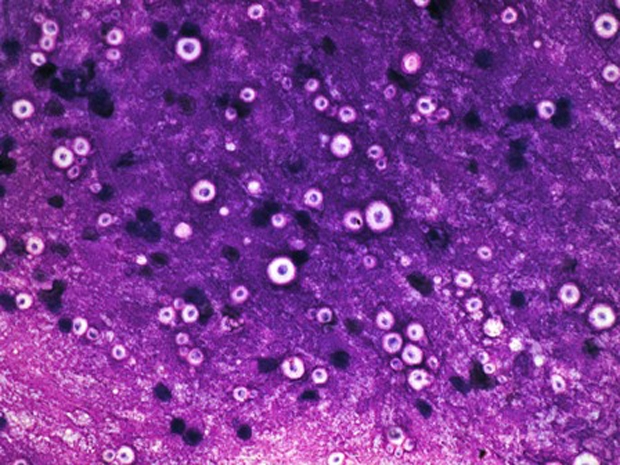
Microscopically, India ink staining identified spherical cells with a zone of clearance (‘halo’) around them representing a prominent capsule, typical of Cryptococcus neoformans. (Image courtesy of St Helier Hospital Department of Microbiology).
Investigations
Included in case presentation to portray the appropriate timeline when the investigations were carried out, due to the complexity of the case.
Differential diagnosis
(See case report).
Treatment
(See case report).
Outcome and follow-up
Patient deceased.
Discussion
Chronic meningitis is defined as a syndrome of meningeal inflammation that persists for more than 4 weeks. Patients often present with non-specific symptoms which may include headache, fever, lethargy, neck stiffness, altered cognition, ataxia and focal neurology.1 The main causes of chronic meningitis can be broadly classified as infective (tuberculous, partially treated bacterial/pyogenic, fungal, viral, protozoa, Borrelia, syphilis) or non-infective (uveo-meningitic syndromes; sarcoid, systemic lupus erythematosus, Behcet’s, other vasculitides, malignant, iatrogenic). There may, however, be a delay in making a diagnosis due to the non-specific symptoms on presentation. In about one third of patients, no cause is identified.2
C neformans accounts for most cases of fungal meningoencephalitis which usually follows a subacute or chronic course. Although more prevalent in immunocompromised hosts (HIV/AIDS, malignancy, organ transplantation, iatrogenic), in whom it is an opportunistic infection, there are now a growing number of reports worldwide of apparently immunocompetent individuals being affected.3–9 The organism has been known to reside in pigeon faeces, although the birds are not infected. Infection is thought to be acquired by inhalation of fungal spores into the lungs, the usual entry site into the body. From here it may be cleared or contained within granulomata.10 Pulmonary manifestations can be anything from asymptomatic to severe pneumonia. The organism may spread to other organs but has a tendency to involve the brain. This spread may occur after a period of quiescence, depending on host factors.11
As already mentioned, and from our experience in this case, establishing a diagnosis remains challenging and an accurate history from the patient (plus collateral sources in cases of altered cognition) would help to guide the investigative process. The mainstay of diagnosis is CSF microscopy and culture. Opening pressures at lumbar puncture are typically high (>25cmH20) and CSF analysis shows raised protein and white cell count (predominantly lymphocytes) and a low glucose (compared to serum level). Indian ink staining is positive in about 50% of non-HIV/AIDS patients (compared to about 70–90% in HIV/AIDS patients). Enzyme immunoassay can be used to detect cryptococcal antigen in CSF as well as serum (blood culture), urine and lung secretions (bronchoalveolar lavage).11 CT scan may show cerebral oedema, hydrocephalus, cryptococcomas, reveal meningeal enhancement or be normal.7 The antifungal agent amphotericin B used in combination with flucytosine forms the basis of initial treatment followed by long-term secondary prophylaxis with high dose fluconazole.
Further to our observations in this case, hyponatraemia is commonly reported in critical neurologic disease and has been reported in 7% to 32% of patients with different forms of meningitis.12 The two main mechanisms responsible are SIADH and cerebral salt washing syndrome (CSW), which can be distinguished from each other by laboratory tests (serum and urine osmolalities, and sodium balance) and determining extracellular fluid volume; typically reduced in CSW.12 Distinguishing between these two causes is important as their management differs.
In our patient, it is probable that she presented the second time with the pulmonary manifestations of cryptococcal meningoencephalitis. The CT finding of hydocephalus prompted the lumbar puncture which identified cryptococcal meningoencepalitis. This result, however, was not available until after the patient’s death.
Learning points.
-
▶
Chronic meningitis can be difficult to diagnose due to the variable and non-specific mode of presentation.
-
▶
Though more common in those that are immunocompromised, cryptococcal meningoencephalitis should always be considered as a possible cause in apparently immunocompetent individuals.
-
▶
Delay in diagnosis is associated with significant morbidity and mortality.
Footnotes
Competing interests None.
Patient consent Not obtained.
References
- 1.Ginsberg L, Kidd D. Chronic and recurrent meningitis. Pract Neurol 2008;8:348–61 [DOI] [PubMed] [Google Scholar]
- 2.Berenguer J, Moreno S, Laguna F, et al. Tuberculous meningitis in patients infected with the human immunodeficiency virus. N Engl J Med 1992;326:668–72 [DOI] [PubMed] [Google Scholar]
- 3.Chau TT, Mai NH, Phu NH, et al. A prospective descriptive study of cryptococcal meningitis in HIV uninfected patients in Vietnam - high prevalence of Cryptococcus neoformans var grubii in the absence of underlying disease. BMC Infect Dis 2010;10:199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bestard J, Siddiqi ZA. Cryptococcal meningoencephalitis in immunocompetent patients: changing trends in Canada. Neurology 2010;74:1233–5 [DOI] [PubMed] [Google Scholar]
- 5.Carniato A, Scotton PG, Miotti AM, et al. [Cryptococcus neoformans meningoencephalitis among apparently immunocompetent patients: description of two cases]. Infez Med 2009;17:41–5 [PubMed] [Google Scholar]
- 6.Guevara-Campos J, González-Guevara L, Urbéz-Cano J, et al. [Cryptococcus neoformans meningoencephalitis in immunocompetent schoolchildren]. Invest Clin 2009;50:231–9 [PubMed] [Google Scholar]
- 7.Kumari R, Raval M, Dhun A. Cryptococcal choroid plexitis: rare imaging findings of central nervous system cryptococcal infection in an immunocompetent individual. Br J Radiol 2010;83:e14–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lambertucci JR, Franco R, de Queiroz LC. Cryptococcal meningoencephalitis and pulmonary nodule in a non-HIV-infected immunocompetent patient. Rev Soc Bras Med Trop 2005;38:207–8 [DOI] [PubMed] [Google Scholar]
- 9.Mitchell DH, Sorrell TC, Allworth AM, et al. Cryptococcal disease of the CNS in immunocompetent hosts: influence of cryptococcal variety on clinical manifestations and outcome. Clin Infect Dis 1995;20:611–6 [DOI] [PubMed] [Google Scholar]
- 10.Othman N, Abdullah NA, Wahab ZA. Cryptococcal meningitis in an immunocompetent child: a case report and literature review. Southeast Asian J Trop Med Public Health 2004;35:930–4 [PubMed] [Google Scholar]
- 11.Bicanic T, Harrison TS. Cryptococcal meningitis. Br Med Bull 2004;72:99–118 [DOI] [PubMed] [Google Scholar]
- 12.Rabinstein A, Wijdicks E. Hyponatraemia in critically ill neurological patients. The Neurologist 2003;9:290–300 [DOI] [PubMed] [Google Scholar]


