Abstract
Spinal dural arterio-venous fistula (DAVF) is rare and usually involves the thoracic segments. The classical presentation is a slowly progressive ataxia. Clinical presentation of intracranial DAVF depends on the site of the DAVF, as well as the vessels involved. Patients may present with pulsatile tinnitus, occipital bruit, headache, dementia, visual impairment as well as neurological deterioration distant from the DAVF as a result of venous hypertension and cortical haemorrhage. The authors present a rare case of progressive myelopathy secondary to an intracranial DAVF.
Background
It is worthwhile to think of possible remote, intracranial cause of cervical cord ‘tumour’ manifesting as myelopathy when no intrinsic spinal cause is found.
Case presentation
A 64-year-old female presented with a 3-month history of bilateral lower limb weakness and a 2-week history of unsteady gait. Examination revealed mild ataxia with evidence of myelopathic signs in the lower limbs. Power was preserved at 4/5. Upper limb and cranial nerve examination was normal. No sensory level was noted.
Investigations
MRI of the cervical spine showed extensive diffuse cervical cord swelling, as well as flow voids (figure 1). Spinal angiography confirmed dilated spinal perimedullary veins (figure 2) suggestive of arterio-venous malformation (AVM) but no obvious spinal vascular malformation was demonstrated. Cerebral angiography revealed an intracranial dural arterio-venous fistula (DAVF) causing the cervical venous engorgement and cord oedema (figure 3).
Figure 1.

MRI cervical spine showing cord swelling with vascular flow voids.
Figure 2.
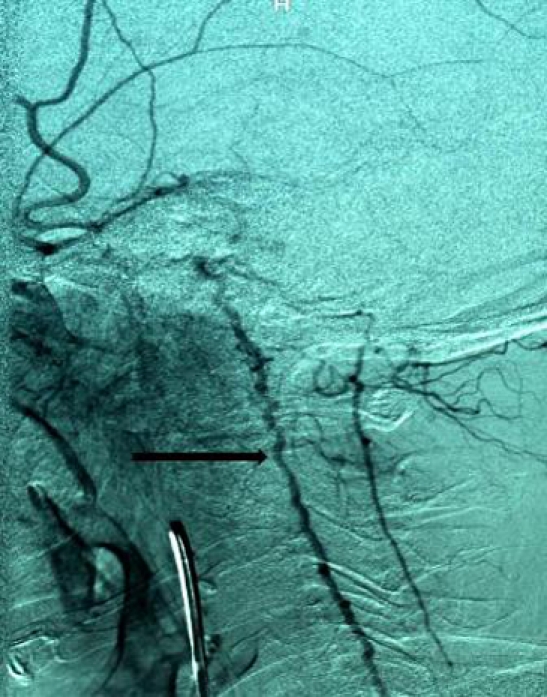
Spinal angiogram showing dilated perimedullary veins.
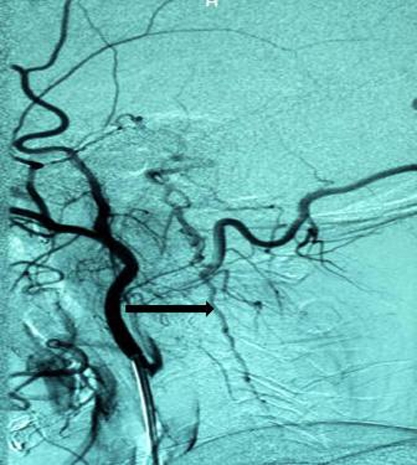
Figure 3.

Cerebral angiogram showing dural arterio-venous fistula as shown by the arrow.
Treatment
Trans-arterial embolisation of the fistula was carried out successfully.
Outcome and follow-up
Trans-arterial embolisation of the fistula was carried out successfully. Post embolisation angiography confirmed significant reduction of the fistula as well as improvement in the dilatation of cervical cord veins (figures 4 and 5).
Figure 4.

MRI cervical spine showing decreased cord swelling post embolisation of dural arterio-venous fistula.
Figure 5.
Spinal angiogram showing decreased dilatation of the cervical perimedullary veins post embolisation of dural arterio-venous fistula (compare figures 2 and 5).
Discussion
AVFs are rare variety of vascular malformations characterised by single or multiple dilated arterioles that connect directly to a vein without a nidus, unlike the AVM which has interposed tangle of abnormal vessels. DAVFs account for 10–15% of all intracranial AVMs.1 61–66% occurs in females, and patients are usually in the 5th decade of life.
DAVFs are probably acquired since reported cases present about middle age or beyond.2 The possible pathogenesis involves collateral revascularisation following thrombosis of a dural venous sinus.3 They are contained within the leaflets of the dura mater, and are usually adjacent to dural venous sinuses. The transverse sinus is most commonly involved with slightly left preponderance. The severity of adverse effects is related to the degree of venous hypertension and retrograde flow in the venous sinus and cortical veins as depicted in the classification by Borden and Cognard. The reported case is classified as Borden type III and Cognard type V.
Borden classification2
-
▶
Type I: Dural arterial supply drains antegrade into a dural venous sinus or meningeal vein. Usually benign clinical behaviour.
-
▶
Type II: Dural arterial supply drains into venous sinus. High pressure in sinus results in both antegrade and retrograde drainage via subarachnoid veins. May present with haemorrhage.
-
▶
Type III: Dural arterial supply drains retrograde into subarachnoid veins. This causes venous hypertension with risk of haemorrhage (table 1).
Table 1.
Cognard classification4
| Type I | Normal antegrade flow into dural sinus |
| Type IIa | Drainage into a sinus with retrograde flow within sinus |
| Type IIb | Drainage into a sinus with retrograde flow to cortical veins |
| Type III | Direct drainage into a cortical vein without venous ectasia |
| Type IV | Direct drainage into a cortical vein with ectasia >5 mm and 3x larger than the diameter of the draining vein |
| Type V | Direct drainage into spinal perimedullary veins |
The aim of treatment is to interrupt or eliminate communication between the draining vein and the fistula and resolve venous congestion. Early treatment has proven to be beneficial as patients tend to improve neurologically. The first line of treatment is endovascular obliteration of the fistula. If embolisation fails, surgical interruption of the DAVF can be attempted if the site is amenable to surgical access. Stereotactic radio-surgery is also another option. This usually resolves the venous congestion of the cord occasioned by arterialisation of the anterior and posterior spinal medullary veins.
Learning points.
-
▶
DAVF is a documented cause of spinal cord ‘tumour’ leading to neurological deterioration as initially reported in our case.
-
▶
If spinal angiography is negative in a case of suspected DAVF, cerebral angiography is indicated to rule out intracranial DAVF connected to the spinal perimedullary venous system.
-
▶
Early interruption of DAVF permits recovery.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Newton TH, Cronqvist S. Involvement of dural arteries in intracranial arteriovenous malformations. Radiology 1969;93:1071–8 [DOI] [PubMed] [Google Scholar]
- 2.Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg 1995;82:166–79 [DOI] [PubMed] [Google Scholar]
- 3.Kwon BJ, Han MH, Kang HS, et al. MR imaging findings of intracranial dural arteriovenous fistulas: relations with venous drainage patterns. AJNR Am J Neuroradiol 2005;26:2500–7 [PMC free article] [PubMed] [Google Scholar]
- 4.Cognard C, Gobin YP, Pierot L, et al. Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology 1995;194:671–80 [DOI] [PubMed] [Google Scholar]


