Abstract
Data from the WHO state that up to 85% of cases of human schistosomiasis are from Africa. The common sites of this parasitic infection are the intestine and bladder. Testicular schistosomiasis is extremely rare but the number of reported cases worldwide has doubled over the past decade. The authors report a case of testicular schistosomiasis of a Myanmar immigrant in Malaysia who presented with a 6-month history of progressively enlarging left testicular swelling. His biochemical markers and cultures were not suggestive of an ongoing infection. Hence, a testicular malignancy was strongly suspected, for which, he underwent a left orchidectomy. Our clinical suspicion was proven wrong when the histopathology of the removed left testis revealed schistosomal eggs with granulamatous tissue formation. Subsequently, the patient was treated with praziquantel.
Background
To date, there are 31 reported cases of testicular schistosomiasis (TS). But, to the best of our knowledge, this is the first reported case of TS in Malaysia and in Southeast Asia. We expect the disease burden in non-endemic areas to increase with globalisation. This case highlights the importance of considering TS as a differential diagnosis in cases of chronic unilateral testicular swelling. Failure to do so may result in unnecessary orchidectomy which may potentially disrupt male fertility. We hereby present a case report and a brief up-to-date review of TS.
Case presentation
A 29-year-old immigrant from Myanmar, with no known medical illness presented to us with a progressively enlarging left testicular swelling over a period of 6 months. With increasing size, the patient developed genital discomfort. He was not sexually active. There were no constitutional symptoms such as fever and weight loss. His bowel and urinary habits were not altered. There was no known contact with tuberculosis patients. The patient had been in Malaysia for 3 months. Back in Myanmar, he used to swim regularly in a freshwater river.
On examination, the left testis was grossly larger than the right. There was a non-tender left testicular swelling measuring 5×5×8 cm. It was firm in consistency with a nodular surface. The right testis was normal. Other systemic examination was unremarkable.
Investigations
His laboratory parameters were normal; leucocyte count of 6.1×109 cells per litre, C-reactive protein of 0.31 mmol/l and erythrocyte sedimentation rate of 26 mm/h. The tumour markers namely human chorionic gonadotrophin and αfetoprotein levels were within normal limits. Ultrasonography of the testis and scrotum revealed hypoechoeic intrascrotal cystic lesion with adjacent hyperechoeic areas (figure 1). Postoperatively, the histopathological examination (HPE) of tissue from the left testis revealed schistosomal eggs with surrounding granulamatous tissue. There was no evidence of malignancy (figure 2). For academic reasons, serology for Schistosoma was sent and the IgM turned out to be positive.
Figure 1.
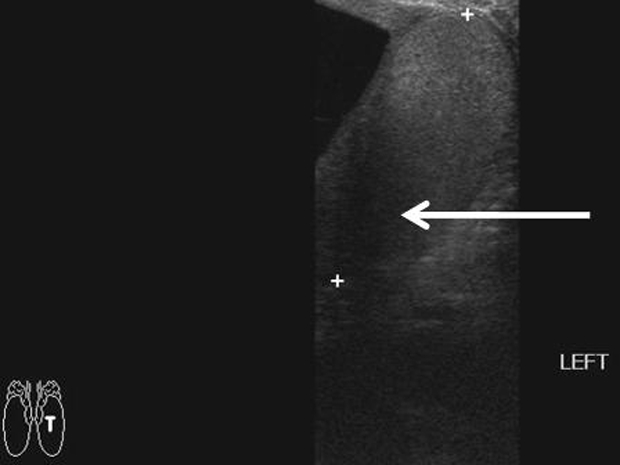
Ultrasound scan of the left testis showing hypoechoeic intrascrotal cystic lesion with adjacent hyperechoeic areas.
Figure 2.
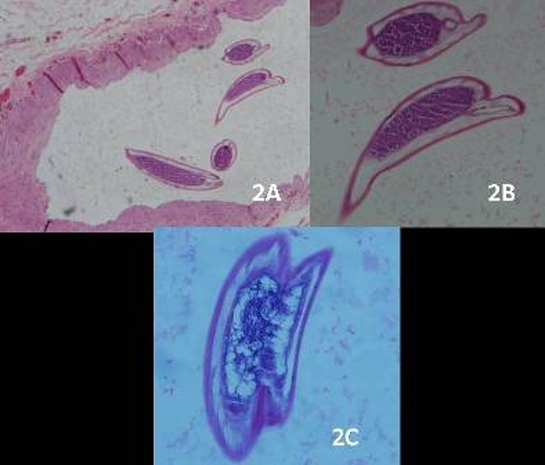
Histopathological examination of left testicular biopsy with H&E stain at various magnifications showing schistosomal eggs with surrounding granulation tissue; 4x (2A), 20x (2B) and 60x (2C).
Differential diagnosis
The differential diagnosis for a unilateral testicular swelling in a young man like this are testicular malignancies such as germ cell tumours, gonadal stromal tumours and tumour of the collecting ducts; testicular tuberculosis, testicular sarcoidosis and spermatocoele.
Treatment
The patient had a diagnostic exploratory surgery. The intraoperative morphological appearance of the left testis was highly suspicious of malignancy. There was a mass with an irregular surface and margins invading the left testis. Left orchidectomy was done and the sample was sent for HPE. Based on the HPE findings of TS, the patient was given oral praziquantel for 2 days.
Outcome and follow-up
A month after discharge, the patient was found to be well during the outpatient infectious disease clinic follow-up.
Discussion
Over the years, globalisation has caused schistosomiasis to be found even in non-endemic countries. More cases are being reported in countries such as the United States and these involve mainly immigrants, travellers and expatriates.1 TS is rare and accounts for only 3.2% of total number of cases of schistosomiasis.2 We performed an extensive literature search on TS and have summarised the key points. Since the first case report in year 1967, there are 31 reported cases till today. The number of reported cases has doubled over the past decade. The vast majority of cases were among Africans. This is the first case of TS from Southeast Asia. We believe that the actual incidence may be higher as this condition is often missed and overlooked especially in non-endemic areas.
Although there are five species in the Schistosoma genus which are known to be the culprits in human schistosomiasis, only S mansoni and S haematobium have been isolated and identified in samples of patients with TS.3 The hypothesised pathophysiology is haematogenous spread of schistosomal eggs via venous communication between internal spermatic vein and mesenteric vein2 that is the rationale for treating patients with antihelmintics despite orchidectomy as in this case. The aim is to eradicate co-existing intestinal schistosomiasis.
Most patients were aged between 20–35 years. But there were two paediatric cases and a single case of a geriatric patient.4–6 The commonest presenting symptom in TS is unilateral testicular swelling. Very large lesions are often mistaken for testicular tumours as in this case. The lesion was huge enough to be described as a ‘giant fibrous pseudotumour’ in one of the reports.7 There were isolated cases of the diagnosis being made following investigation for male infertility.8 9 The most feared complication is testicular infarction with testicular atrophy leading to primary hypogonadism.6
In most case reports, the diagnosis was made postorchidectomy from the histopathological examination of the biopsied testis. Most surgeons opted for orchidectomy with testicular malignancy in mind. We assume that preoperative testicular biopsies were avoided due to the risk of tumorous seeding. Till today, there is no reliable radiological investigation to aid clinicians. Ultrasonography is not very helpful as there are no pathognomonic sonographic findings of TS. In fact, the features are difficult to distinguish from testicular malignancies.10 Fortunately, serologic testing for schistosomiasis has a high sensitivity of 95–99% and a specificity of 99%.11 The authors believe that it is worthwhile to screen for schistosomiasis in all patients with unilateral testicular swelling from endemic areas or with risk of exposure such as swimming or wading in fresh water.
TS is potentially treatable with medical therapy. The recognition of TS as a differential for testicular tumours is crucial to avoid unnecessary orchidectomies. Infertility or subfertility which is a known sequelae of orchidectomy may not be life threatening but for many is psychologically devastating.
Learning points.
-
▶
TS is on the rise in non-endemic areas with globalisation.
-
▶
Ultrasound findings does not distinguish TS from testicular malignancy.
-
▶
In the presence of risk factors, Schistosoma serology testing should be performed in individuals with unilateral testicular swelling.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Hochberg NS, Moro RN, Sheth AN, et al. High prevalence of persistent parasitic infections in foreign-born, HIV-infected persons in the United States. PLoS Negl Trop Dis 2011;5:e1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lopes RI, Leite KR, Prando D, et al. Testicular schistosomiasis caused by Schistosoma mansoni: a case report from Brazil. Braz J Infect Dis 2007;11:523–4 [DOI] [PubMed] [Google Scholar]
- 3.Salem S, Mitchell RE, El-Alim El-Dorey A, et al. Successful control of schistosomiasis and the changing epidemiology of bladder cancer in Egypt. BJU Int 2011;107:206–11 [DOI] [PubMed] [Google Scholar]
- 4.Elbadawi A, Davis RS, Cockett AT. Schistosomiasis presenting with testicular enlargement in elderly male. Urology 1978;12:87–90 [DOI] [PubMed] [Google Scholar]
- 5.Lukács T, Pajor L, Hamza L, et al. Schistosomal granulation masquerading as testicular tumour. Acta Chir Hung 1989;30:187–91 [PubMed] [Google Scholar]
- 6.Rambau PF, Chandika A, Chalya PL, et al. Scrotal swelling and testicular atrophy due to schistosomiasis in a 9-year-old boy: a case report. Case Reports in Infectious Diseases 2011;2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elem B, Patil PS, Lambert TK. Giant fibrous pseudotumor of the testicular tunics in association with Schistosoma haematobium infection. J Urol 1989;141:376–7 [DOI] [PubMed] [Google Scholar]
- 8.Kini S, Dayoub N, Raja A, et al. Schistosomiasis-induced male infertility. BMJ Case Rep 2009;2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Qahtani SM, Droupy SJ. Testicular schistosomiasis. Saudi Med J 2010;31:325–7 [PubMed] [Google Scholar]
- 10.Soans B, Abel C. Ultrasound appearance of schistosomiasis of the testis. Australas Radiol 1999;43:385–7 [DOI] [PubMed] [Google Scholar]
- 11.Tsang VC, Wilkins PP. Immunodiagnosis of schistosomiasis. Immunol Invest 1997;26:175–88 [DOI] [PubMed] [Google Scholar]


