Chemokine receptor CCR3 expression is increased by age-related stress. Activated CCR3 promotes choroidal endothelial cell migration and Rac1 activation, which may be associated with activation of VEGFR2 signaling.
Abstract
Purpose.
To explore the molecular mechanisms by which the C–C chemokine receptor type 3 (CCR3) and chemokine (C–C motif) ligand 11 (CCL11) regulate choroidal endothelial cell (CEC) migration and the interactions with the vascular endothelial growth factor (VEGF) signaling pathway.
Methods.
Human retinal sections from young and aged donor normal eyes were immunolabeled. By real-time PCR, CCR3 mRNA was measured in retinal pigmented epithelium (RPE)/choroids obtained from young and aged human donor eyes and in cultured CECs exposed to hydrogen peroxide. CCR3 ligand and CCL11- or VEGF-stimulated CEC migration was also measured in the presence of the CCR3 inhibitor or control using fluorescence microscopy. Activation of Rac1, phosphorylated Akt as a readout for phosphoinositol 3-kinase signaling, and VEGFR2 activation were measured in CECs incubated with CCL11, VEGF, or combined CCL11/VEGF.
Results.
CCR3 was expressed to a greater level in older compared with that in younger human retinas or RPE/choroids. Ligand-activated CCR3 increased CEC migration, which was inhibited by the CCR3 inhibitor. Rac1 activity, p-Akt, and p-VEGFR2 were significantly increased in CECs incubated with CCL11. The CCR3 inhibitor prevented VEGF-induced CEC migration and Rac1 activation in CECs. Rac1 activity was additively increased in CECs treated with CCL11 and VEGF compared with that in cells with CCL11 or VEGF treatment alone. Ligand-activated CCR3 caused VEGFR2 phosphorylation and coimmunoprecipitation of VEGFR2 and CCR3.
Conclusions.
Activated CCR3 promotes CEC migration and Rac1 activation and causes an association with and activation of VEGFR2. Cross-talk between CCR3 and VEGF signaling exists and may be important in choroidal neovascularization in human age-related macular degeneration.
Neovascular age-related macular degeneration (AMD) accounts for 80% of legal blindness in a rapidly growing percentage of the U.S. population, that is, those older than 60 years of age.1 Outcomes have improved with anti–vascular endothelial growth factor (VEGF) treatment,2 but visual acuity still improves in only 40% of cases, and repeated intraocular injections pose serious ocular risks, including endophthalmitis and retinal detachment.3 Also, treatment benefit is lost after repeated intravitreal injections of VEGF antibody,4 raising a concern of potential retinal toxicity or recurrent choroidal neovascularization (CNV) caused by compensatory mechanisms through altered regulation of angiogenic and inhibitory growth factors or other signaling.5–8 Thus, considering pathways besides the VEGF pathway is important in the development of therapies for neovascular AMD. The G-protein–coupled receptor (GPCR), C–C chemokine receptor 3 (CCR3), was reported to be important in neovascular AMD.9 Additional evidence supports its role in CNV.10 However, a recent study reported that CCR3 was not important in CNV development when using a CNV gelatinous protein mixture (Matrigel; BD Biosciences, Franklin Lakes, NJ) model.11 Therefore, further study regarding the potential role of CCR3 in AMD is needed.
AMD is a complex disease, influenced by environmental and genetic factors. In this study, we focused on the effects of environmental stresses associated with AMD on CCR3 expression in choroidal endothelial cells (CECs). We studied the mechanisms whereby CCR3 signaling activates CECs to migrate, a key event before the development of vision-threatening sensory retinal CNV. We obtained data from human donor eyes and used cultured human CECs and retinal pigmented epithelium (RPE). We also explored the hypothesis that CCR3 and VEGF work synergistically in triggering downstream signaling pathways. We report that the CCR3 ligand, chemokine (C–C motif) ligand 11 (CCL11), activates VEGF receptor 2 to trigger activation of the small GTPase Rac1, which we previously reported is necessary for CEC transmigration of the RPE.12–14
Methods
Cell Culture
CECs were isolated from young donor eyes obtained from the North Carolina Eye Bank as previously reported.15 Enriched condition (EC) phenotype was confirmed by labeling of EC markers (CD31, vwF, and VE-cadherin), and passages 2 through 5 were used in experiments. CECs were maintained in endothelial growth medium-2 (EGM-2; Lonza, Walkersville, MD) with 10% fetal bovine serum (FBS). ARPE-19 cells were obtained from American Type Culture Collection (Rockville, MD) and grown in Dulbecco's modified Eagle's medium/F12 (DMEM/F-12; Invitrogen, Carlsbad, CA) plus 10% FBS and penicillin–streptomycin. Cells below passage 18 were used for experiments.
CEC Migration Assay
CCL11 and VEGF (R&D Systems, Minneapolis, MN) were reconstituted in 0.1% BSA and then mixed with gelatinous protein mixture extract (Matrigel; BD Biosciences) diluted 1:1 with serum-free endothelial basal media (EBM-2; Lonza). Controls were PBS in 0.1% BSA mixed in gelatinous protein mixture extract. A small molecule CCR3 inhibitor that specifically prevents ligand binding to CCR3 with an IC50 of 28 nM (US 2010/0273795 A1; a gift of Axikin Pharmaceuticals, San Diego, CA) was dissolved in dimethyl sulfoxide and used at concentrations from 1 to 1000 nM. EBM-2 (500 μL) was added to each well of a 24-well plate followed by a 6.5-mm-diameter insert (8-μm pores; Transwell; Corning, Inc., Corning, NY). Human CECs in EBM-2 were prestained with cell-labeling solution (Vybrant DiO; Invitrogen, Carlsbad, CA) for 30 minutes at 37°C and seeded into the inserts at 50,000 cells per 200 μL of serum-free EBM-2 media. The plates were allowed to incubate for 24 hours at 37°C, 5% CO2. The migrated cells were imaged with a culture microscope and microscope digital camera (Olympus CK40 and Olympus DP71, respectively; both Olympus America, Inc., Center Valley, PA).
Rac-1 Activity Assay
Human CECs were cultured in EGM-2 containing 10% FBS. Before starting the assay, cells were serum starved with basal medium EBM2 (Lonza) for at least 2 hours. Cells were stimulated for designated times with CCL11 (10 ng/mL) or/and VEGF (20 ng/mL) and PBS was used as control. Equal amounts of lysates (500 μg) were incubated for 30 minutes at 4°C, with rotation with glutathione S-transferase–p21-activated kinase 1 p21 binding domain agarose beads (Millipore, Temecula, CA) to pull down active guanosine triphosphate (GTP)–bound Rac-1. The samples were subsequently analyzed for bound Rac-1 by Western blot analysis using an anti–Rac-1 antibody (BD Transduction Laboratories, San Jose, CA).
Phospho-Akt and Phospho-STAT3 Assays
Human primary CECs were grown in 6-well plates. After starving in serum-free EBM-2, cells were incubated with CCL11 (10 ng/mL), VEGF (20 ng/mL), or both for 30 minutes. Cells were lysed in radioimmunoprecipitation assay (RIPA) buffer to probe phospho-Akt and total AKT using antibodies for p-Akt and Akt1 or for phospho-STAT3 and total STAT3 (Cell Signaling Technology, Danvers, MA).
Phospho-VEGFR2 by Immunoprecipitation
Human CECs were seeded into 6-well plates. After 2 hours of starving in serum-free EBM-2, cells were treated with CCL11 (10 ng/mL) for 0, 15, 30, or 60 minutes. Cells were harvested in RIPA buffer and cell lysates were probed by immunoprecipitation and Western blot analysis to detect phospho-VEGFR2 using antibodies to VEGFR2 (Santa Cruz Biotechnology, Santa Cruz, CA) and phospho-tyrosine (BD Transduction Laboratories). As a positive control, phospho-VEGFR2 was determined in cells after a 15-minute incubation with VEGF (20 ng/mL).
Immunolabeling with CCR3
Human retinal paraffin sections of eyes from a 91-year-old male donor, obtained through the Georgia Eye Bank, were deparaffinized and an antigen-retrieval step was performed with antigen-retrieval solution (Dako North America, Inc., Carpinteria, CA) before immunostaining. Human retinal cryosections from an eye of a 25-year-old male donor was obtained from the Utah Lions Eye Bank. For immunolabeling in CECs, human CECs grown on uncoated coverslips were fixed with 4% paraformaldehyde for 20 minutes, then rinsed in PBS. Cells and retinal sections were incubated in 2% normal goat serum in PBS/0.5% Triton X-100 for 1 hour, to block nonspecific binding of the primary antibody. Sections were incubated with rabbit anti-CCR3 (1:50 dilution; Santa Cruz Biotechnology) overnight at 4°C. After three washes in PBS, sections were incubated for 1 hour with a 1:500 dilution of dye-conjugated goat anti-rabbit secondary antibody (Alexa Fluor 488; Invitrogen, Carlsbad, CA) for CCR3. The sections were rinsed in PBS, stained with the nuclear dye 4′,6′-diamidino-2-phenindole, and mounted in a water-soluble, nonfluorescing compound (Fluoromount-G; SouthernBiotech, Birmingham, AL). Images were captured with an inverted microscope (Olympus 1X81, Tokyo, Japan) and digitally stored for analysis.
RNA Isolation and Real-Time PCR
Cells were removed from culture medium and washed with cold PBS. Total RNA was extracted by use of a single-step RNA isolation reagent (Tri-Reagent; Sigma-Aldrich, St. Louis, MO). RNA was quantified by use of a microvolume instrument (NanoDrop; Thermo Fisher Scientific, Inc., Waltham, MA). cDNA was generated using a commercial kit (High-Capacity cDNA Archive Kit; Applied Biosystems, Foster City, CA). RT-PCR was performed on a gene-sequence detector instrument (ABI Prism 7500; Applied Biosystems) using probes (TaqMan probes; Applied Biosystems) to human CCR3 and β-actin genes and primers to CCL11, CCL24, and CCL26 (SYBR Green qPCR Master Mix; Clontech, Mountain View, CA). Expression levels for all genes were normalized to the mean value of internal control human β-actin. Sequences for the primers (SYBR Green) were as follows: human CCL11: Forward 5′-AGAAGAAGTGGGTGCAGGATTCCA-3′, Reverse 5′-TTAGGCAACACTCAGGCTCTGGTT-3′; human CCL24: Forward 5′-AGAAGAAGTGGGTGCAGGATTCCA-3′, Reverse 5′-TTAGGCAACACTCAGGCTCTGGTT-3′; human CCL26: Forward 5′-AGAAGAAGTGGGTGCAGGATTCCA-3′, Reverse 5′-TTAGGCAACACTCAGGCTCTGGTT-3′.
Statistical Analyses
Significant differences between groups were determined by ANOVA with post-hoc protected t-tests, as indicated for specific experiments in the figure legends. All experiments had an n = 3 to n = 6. Cell migration experiments and Rac1 activity assays were repeated three times. A minimum value of P < 0.05 was considered statistically significant.
Results
CCR3 Expression in Human Retina and RPE/Choroids from Young and Aged Donors
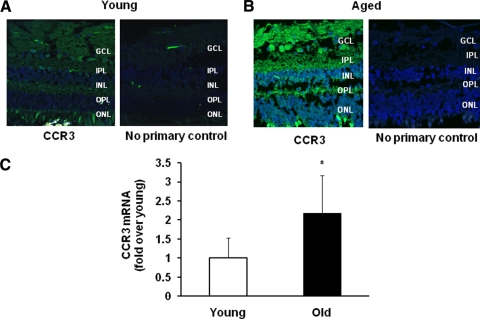
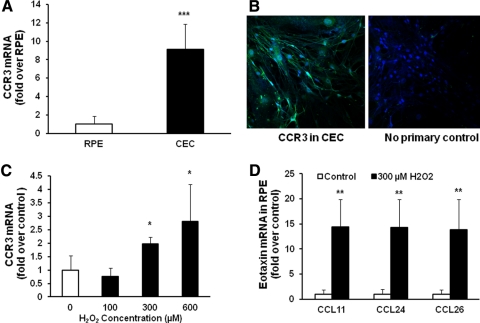
Age is the leading factor associated with increased risk of AMD.16 We previously reported that all VEGF splice variants were significantly increased in RPE from eyes of donors older than 70 years of age compared with donors between 20 and 40 years of age.14 Because we found that CCR3 was important in human neovascular AMD,9 we predicted that eyes from donors of increased age would show greater expression of CCR3 than that of eyes from younger donors. Figures 1A and 1B showed that immunolabeling with CCR3 appeared qualitatively greater in the retina from a 91-year-old donor's eye compared with (Fig. 1B) that from a 25-year-old donor's (Fig. 1A). We then measured CCR3 mRNA in RPE/choroids from young and old donor eyes (n = 3 from each) by quantitative real-time PCR. CCR3 mRNA was significantly increased in RPE/choroids from aged versus young donors (Fig. 1C). We next determined the expression level of CCR3 in cultured CECs and RPE cells. We found that CCR3 mRNA was highly expressed in CECs, with a nearly 10-fold increase compared with RPE (Fig. 2A). This finding was supported by positive CCR3 labeling in cultured CECs (Fig. 2B), whereas there was no CCR3 label in cultured RPE (data not shown).
Figure 1.
CCR3 expression in human retinal sections and RPE/choroids. Representative immunostaining of CCR3 in human retinal sections from 25-year-old (A) and 91-year-old (B) donors using anti-CCR3 antibody (magnification, ×40). (C) The expression of CCR3 mRNA was measured by real-time PCR in RPE/choroid from aged and young donors. *P < 0.05 vs. young (n = 3 individual donor eyes for each group).
Figure 2.
CCR3 expression in CECs and RPE cells increased by AMD-related stresses. CCR3 expression in CECs and RPE cells (A, C) and its ligands in RPE cells (D) were measured by real-time PCR. (A) Cultured human CECs and RPE cells. ***P < 0.001 vs. RPE (n = 6). (B) CCR3 immunostaining in cultured CECs. (C) Human CECs were exposed to H2O2 at different doses (100, 300, and 600 μM) for 6 hours. *P < 0.05 vs. 0 μM H2O2 (n = 6). (D) Human ARPE-19 cells were incubated with 300 μM H2O2 for 6 hours. **P < 0.01 vs. control (n = 6).
CCR3 Expression Increased in Cultured CECs by AMD-Related Stresses
Evidence supports both exogenous and endogenous reactive oxidative species (ROS) as factors involved in pathologic steps in AMD.12,17–20 We therefore determined the effect of H2O2 on CCR3 expression level in CECs. We previously reported that 600 μM H2O2 caused a significant and selective upregulation of the VEGF189 splice variant in RPE.14 However, in CECs, there was no change in the expression levels of VEGF splice variants, VEGF121, VEGF165, and VEGF189.14 To determine the effect of H2O2 on CCR3 expression in CECs, a dose–response experiment was performed with H2O2 at 100, 300, or 600 μM concentrations. After incubation for 24 hours, CCR3 expression in CECs was found to be increased 4-fold from control at the 300 μM concentration (Fig. 2C). In cultured RPE, H2O2 exposure also caused a significant increase in CCR3 mRNA compared with control, although the expression levels remained 10-fold less than that of CCR3 (data not shown). When RPE were exposed to 300 μM H2O2, there was a significant 15-fold increase in expression of all three CCR3 ligands (CCl11, CCl24, and CCl26; Fig. 2D), whereas CEC expression of all three ligands was unchanged from control after exposure to 300 μM H2O2 (data not shown). Therefore, age and oxidative stress appeared to upregulate CCR3 in both CECs and RPE, and induce increased CCR3 ligand production only in RPE cells.
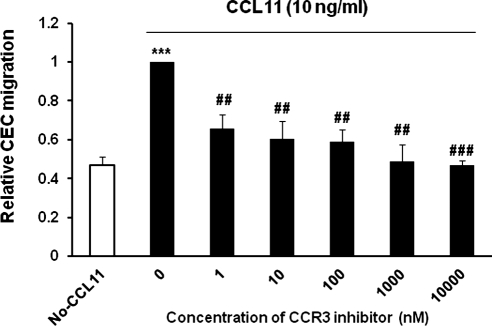
CEC Migration Is Increased by CCR3 Ligand
We were then interested in the effects of CCR3 signaling on CEC migration. We measured CEC migration after stimulation with the CCR3 ligand, CCL11. We found that at a dose of 10 ng/mL, CCL11 induced migration of CECs with a twofold increase over control. This ligand-induced CEC migration was significantly inhibited by a CCR3 inhibitor in a dose-dependent manner, consistent with previous findings9 (Fig. 3).
Figure 3.
CCR3 ligand CCl11 promotes CEC migration. The number of migrated CECs toward gelatinous protein mixture extract (Matrigel; BD Biosciences) mixed with 10 ng/mL CCL11 or control was measured after incubation with control or CCR3 inhibitor at different doses (1 nM, 10 nM, 100 nM, 1 μM, and 10 μM) for 24 hours. Migrated CECs toward gelatinous protein mixture extract without CCL11 were used as a control (No-CCL11). Overall one-way ANOVA P < 0.0001; post-hoc Newman-Keuls multiple comparison testing: ***P < 0.001 vs. No-CCL11, ##P < 0.01, ###P < 0.001 vs. CCL11 alone (n = 9).
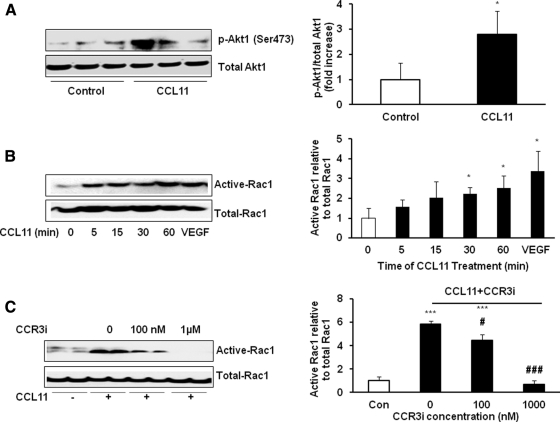
Effect of CCR3 on EC Signaling Pathways
Several signaling pathways can lead to CEC migration. The Janus kinase/signaling transducer and activator of transcription pathway can mediate EC and other cell migration through phosphorylation of STAT3.21 We reported that soluble VEGF activated phosphoinositol 3-kinase (PI 3-kinase) signaling and VEGF receptor 2 (VEGFR2), and both were important in CEC transmigration of the RPE13,15 by mediating the activation of the small GTPase, Rac1, in CECs.12–14 As shown in Figure 4A, after stimulation with CCL11 (10 ng/mL) for 30 minutes, we found a significant activation of PI 3-kinase determined by increased p-Akt. However, when VEGF was used to stimulate p-Akt, we did not find activation at the same time points as CCL11 stimulated p-Akt, nor did we find p-STAT3 increased at the time points tested in CECs after stimulation with CCL11 or VEGF (data not shown). We next measured Rac1 activity in CECs incubated with CCL11 for different times. At a dose of 10 ng/mL, CCL11 significantly induced Rac1 activity at 30 minutes and the effect was sustained through 60 minutes (Fig. 4B). This was similar to the time course of VEGF-stimulated Rac1 activation we previously observed in CECs.12 We then determined whether CCL11-induced Rac1 activation was mediated through the CCR3 receptor. CECs were pretreated with the small molecule CCR3 inhibitor for 30 minutes before stimulation with CCL11 and assayed for Rac1 activity. Rac1 activation induced by CCL11 was significantly inhibited by the CCR3 inhibitor at 100 nM and, at the 1 μM dose, the CCR3 inhibitor totally blocked CCL11-stimulated Rac1 activation (Fig. 4C).
Figure 4.
CCL11 stimulates PI 3-kinase and Rac1 activation via CCR3. Rac1 activation was measured by pull-down assays in CECs. (A) p-Akt-1 and total Akt-1 were measured in CECs incubated with CCL11 (10 ng/mL) for 30 minutes as a readout for PI 3-kinase activity. *P < 0.05 vs. control (n = 3, representative experiment). (B) CECs were incubated with 10 ng/mL CCL11 for 0, 5, 15, 30, and 60 minutes or treated with 20 ng/mL VEGF for 60 minutes as a positive control. *P < 0.05 vs. 0 min of CCL11 treatment (n = 6). (C) CECs were pretreated with CCR3 inhibitor at two doses (100 nM and 1 μM) for 30 minutes, and then cells were exposed to 10 ng/mL CCL11 for 60 minutes. Overall one-way ANOVA P < 0.0001; post-hoc Newman-Keuls multiple comparison testing: ***P < 0.001 vs. control; #P < 0.05 and ###P < 0.001 vs. CCL11 alone (n = 6).
Cross-talk between CCR3 and VEGF Signaling
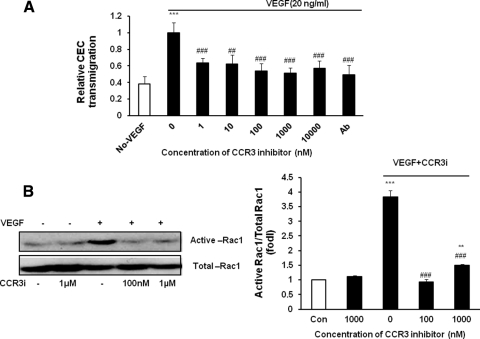
Results in Figure 4 indicate that ligand-activated CCR3 induced CEC migration through PI 3-kinase/Rac1 signaling. Our previous studies also showed that VEGF activated PI 3-kinase and Rac1 to cause CEC transmigration of the RPE.13,15 We then determined whether there was cross-talk between the CCR3 and VEGF signaling pathways to mediate CEC activation. CEC migration toward VEGF165 was measured in the presence of different concentrations of the CCR3 inhibitor. We found that the CCR3 inhibitor caused a dose-dependent decrease in VEGF-induced CEC migration that was significant at all doses measured (Fig. 5A). We then determined whether the CCR3 inhibitor was able to prevent VEGF-induced Rac1 activation. CECs were pretreated with the CCR3 inhibitor for 30 minutes and exposed to VEGF or control for 1 hour. Rac1 was measured in cells lysates using pull-down assays. VEGF-induced Rac1 activation was significantly inhibited by the CCR3 inhibitor (Fig. 5B).
Figure 5.
CCR3 inhibitor blocks VEGF-induced CEC migration and Rac1 activation. (A) Migrated CECs toward gelatinous protein mixture extract (Matrigel; BD Biosciences) mixed with 20 ng/mL VEGF or control were measured after cells were incubated with control or CCR3 inhibitor at different doses (1 nM, 10 nM, 100 nM, 1 μM, and 10 μM) for 24 hours. Migrated CECs toward gelatinous protein mixture extract without VEGF were used as a negative control and neutralizing VEGF antibody as positive controls. Overall one-way ANOVA P < 0.0001; post-hoc Newman-Keuls multiple comparison testing: ***P < 0.001 vs. Non-VEGF, ##P < 0.01 vs. VEGF alone. #P < 0.05, ###P < 0.001 vs. CCL11 alone (n = 6). (B) Rac1 activity was measured by pulldown assay in CECs pretreated with CCR3 inhibitor for 30 minutes and then exposed to 20 ng/mL VEGF or control for 1 hour. Overall one-way ANOVA P < 0.0001; post-hoc Newman-Keuls multiple comparison testing: ***P < 0.001 and **P < 0.01 vs. control; ###P < 0.001 vs. VEGF (n = 6).
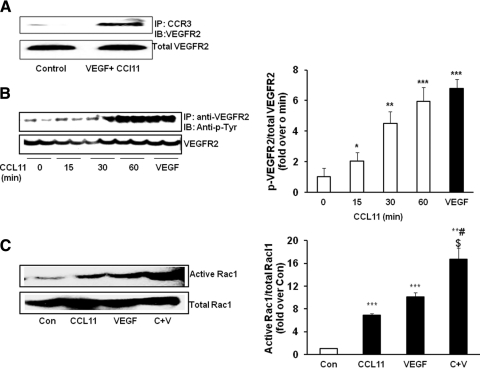
One mechanism whereby cross-talk between signaling pathways can occur is through colocalization of receptors. We performed coimmunoprecipitation assays for VEGFR2 and CCR3 in CECs incubated with CCL11 (10 ng/mL) and VEGF (20 ng/mL) for 30 minutes. We found that CCR3 bound to VEGFR2 in response to combined CCL11 and VEGF treatment (Fig. 6A). When CECs were stimulated with CCL11 alone, p-VEGFR2 was significantly increased compared with control at 15 minutes, with a maximum at 60 minutes, which was similar to the effect obtained by VEGF stimulation alone (Fig. 6B). This finding provided evidence that CCL11-induced stimulation of CCR3 can also induce the phosphorylation of VEGFR2. We then determined if the interaction between CCR3 and VEGFR2 affected downstream Rac1 activation. After a 1-hour stimulation with VEGF, CCL11, or both ligands together, we found CCL11 and VEGF each caused a significant increase in Rac1 activation, and exposure to both ligands led to an additive increase in Rac1 activity (Fig. 6C).
Figure 6.
Ligand-activated CCR3 coimmunoprecipitates with and activates VEGFR2 and leads to synergistic activation of Rac1. (A) Coimmunoprecipitation of CCR3 and VEGFR2 was performed in CECs incubated with VEGF (20 ng/mL) and CCL1 (10 ng/mL) for 1 hour using antibodies to CCR3 and blotting for VEGFR2 (n = 3). (B) Phospho-VEGFR2 was detected by immunoprecipitation with antibodies against VEGFR2 and a blot for phospho-tyrosine in CECs treated with CCL11 (10 ng/mL) for 0, 15, 30, and 60 minutes; phosphorylation of VEGFR2 in CECs exposed to VEGF (20 ng/mL) for 15 minutes was a positive control. Overall one-way ANOVA P < 0.0001; post-hoc Newman-Keuls multiple comparison testing: *P < 0.05, **P < 0.01, and ***P < 0.001 vs. 0 minutes of CCL11 treatment (n = 3). (C) Rac1 activity in CECs was measured in response to the stimulation of CCL11 (10 ng/mL) and VEGF (20 ng/mL). Rac1 activity in cells with either CCL11 or VEGF treatment alone was used as a control. Overall one-way ANOVA P < 0.0001; post-hoc Newman-Keuls multiple comparison testing: **P < 0.01 and ***P < 0.001 vs. control; #P < 0.05 vs. CCL11 alone; $P < 0.05 vs. VEGF alone (n = 3).
Discussion
In this study, we found that the chemokine receptor CCR3 was significantly expressed in CECs in conditions associated with increased risk of AMD, that is, older age and oxidative stress. We also found that the mRNA for ligands of CCR3 (CCL11, CCL24, and CCL26) were expressed in RPE and were increased in response to H2O2 challenge. CCR3 labeling was greater in aged human retinas compared with younger donor eyes such as reported in specimens of human neovascular AMD.9 However, Li et al.11 reported that CCR3 was not involved in CNV caused when gelatinous protein mixture extract (Matrigel; BD Biosciences) was injected through the sclera into the subretinal space to cause choroidal neovascularization. There may be several reasons for this. CCR3 may be expressed under certain conditions: increased age or oxidative stress, both known factors associated with advanced AMD. We found supporting evidence of this in our cell culture studies. Previously we found that laser to induce CNV in mouse retinas caused increased generation of ROS through activated NADPH oxidase.12 In this report, we found that ROS increased CCR3 expression in CECs and CCR3 ligand expression in RPE. It is not clear whether retinal ROS generation is affected in the in vivo gelatinous protein mixture extract (Matrigel; BD Biosciences) CNV assay.
In this study, we explored potential mechanisms whereby CCR3 signaling would lead to neovascular AMD, focusing on CEC activation and migration. In agreement with our earlier report,9 the CCR3 ligand, CCL11, mediated CEC migration and the activation of Rac1, and this was inhibited by a specific CCR3 inhibitor that blocked binding of the ligand to the receptor. We had previously reported that Rac1 is essential to CEC transmigration of the RPE.12–14 Rac1 is a small GTPase of the Rho family that is activated by guanine nucleotide exchange factors. In the GTP-bound activated state, Rac1 can modulate cell behavior by binding to effector proteins. It is returned to the inactive state by GTPase-activating proteins (GAPs) that promote hydrolysis of bound GTP to guanosine diphosphate (GDP).22 Rac122,23 has a number of cell functions, many related to regulation of the actin cytoskeleton, such as control over cell motility and migration.24–26 Rac1 is also a subunit of nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, which generates ROS that can then act as a second messenger, as in angiogenesis.27 We found that VEGF activated Rac1 and mediated NADPH oxidase-generated ROS in CECs and in CNV after laser injury.12 From the data in this report, Rac1 also appear to be activated downstream of CCL11-stimulated CCR3 signaling.
We found PI 3-kinase was activated in CECs stimulated with CCL11. We had previously reported that PI 3-kinase was involved in soluble VEGF-mediated CEC transmigration as an upstream regulator for Rac1.13 However, unlike VEGF and CCL11, which had an additive effect in activating Rac1, we did not find a synergistic effect between VEGF and p-Akt.
CCR3, as a GPCR, historically has been studied for its role in eosinophil chemotaxis and, more recently, in angiogenesis.9,28 In this report, we studied the interaction between VEGF and CCR3 signaling pathways in mediating CEC migration toward the chemokine CCL11. There are several reasons to study potential cross-talk between VEGF and CCR3 signaling. VEGF and CCR3 signaling are both important in human neovascular AMD.2,9 We previously found that RPE-produced VEGF triggered VEGFR2 signaling and active Rac1 in CECs that caused CEC transmigration of the RPE.14,15 We showed that CCL11-stimulated CCR3 signaling also stimulates Rac1 activation and CEC chemotactic migration. In this study, we now report several lines of evidence that cross-talk exists between the CCR3 and VEGF signaling pathways. First, we found a physical interaction between CCR3 and VEGFR2 through coimmunoprecipitation of CCR3 and VEGFR2 in response to stimulation with ligands CCL11 and VEGF. Chemokines and their receptors usually function in complex networks involving homo- and heterodimerization with other chemokine receptors or receptor tyrosine kinases (RTKs),29 and our coimmunoprecipitation results suggest this as a possibility between VEGFR2 and CCR3. We also found that CCL11 treatment activated VEGFR2, recognized as increased phosphorylation of VEGFR2. GPCRs can interact with other receptors through transactivation of receptors, including RTKs,29 such as VEGFR2. The data in our report suggest that CCL11 may be able to act on VEGFR2 via CCR3. Our data also showed a synergistic effect of the interaction between activated CCR3 and VEGFR2 on downstream activation of Rac1, which is important in CEC transmigration of the RPE.12–14
In summary, we have shown that increased age and stresses associated with AMD, such as oxidative stress, lead to increased expression of CCR3 in CECs and its ligands in RPE. CCR3 by itself is able to mediate CEC migration, and it can also modulate VEGFR2 signaling and exacerbate Rac1 activation. The cross-talk of CCR3 with VEGF signaling suggests that inhibition of CCR3 may be an additional method to prevent or treat vision-threatening neovascular AMD. However, in sections from aged human eyes, we found CCR3 labeling occurred in other retinal neurons. This could indicate that inhibiting CCR3 may be detrimental to retinal survival. Rac1-mediated NADPH oxidase activation can generate ROS and cytokines, which have been reported to also cause retinal neuronal damage.30 Therefore, inhibition of CCR3-induced Rac1 activation may alternatively promote neuronal survival. In future studies, we will look at other mechanisms of cross-talk and also potential downstream signaling through pathways, such as ERK (extracellular signal-regulated kinase),31 found activated by CCR3 signaling in other diseases.
Acknowledgments
The authors thank Kevin Bacon, PhD (Axikin Pharmaceuticals), for the CCR3 inhibitor used in this study and for funding part of this research and Shami Kanekar, PhD, for her help with labeling sections of human retina.
Footnotes
Supported in part by National Eye Institute Grants R01 EY015130 (MEH) and EY017011 (MEH).
Disclosure: H. Wang, Axikin Pharmaceuticals (F); E.S. Wittchen, Axikin Pharmaceuticals (F); Y. Jiang, None; B. Ambati, None; H.E. Grossniklaus, None; M.E. Hartnett, Axikin Pharmaceuticals (F)
References
- 1. Gehrs KM, Anderson DH, Johnson LV, Hageman GS. Age-related macular degeneration—emerging pathogenetic and therapeutic concepts. Ann Med. 2006;38:450–471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. The CATT Research Group Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N Engl J Med. 2011;364:1897–1908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Day S, Acquah K, Mruthyunjaya P, Grossman DS, Lee PP, Sloan FA. Ocular complications after anti-vascular endothelial growth factor therapy in Medicare patients with age-related macular degeneration. Am J Ophthalmol. 2011;152:266–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Eghøj MS, Sørensen TL. Tachyphylaxis during treatment of exudative age-related macular degeneration with ranibizumab. Br J Ophthalmol. In press [DOI] [PubMed] [Google Scholar]
- 5. Dias JR, Rodrigues EB, Maia M, Magalhães O, Jr, Penha FM, Farah ME. Cytokines in neovascular age-related macular degeneration: fundamentals of targeted combination therapy. Br J Ophthalmol. In press [DOI] [PubMed] [Google Scholar]
- 6. Bhutto IA, Kim SY, McLeod DS, et al. Localization of collagen XVIII and the endostatin portion of collagen XVIII in aged human control eyes and eyes with age-related macular degeneration. Invest Ophthalmol Vis Sci. 2004;45:1544–1552 [DOI] [PubMed] [Google Scholar]
- 7. Hageman GS, Anderson DH, Johnson LV, et al. A common haplotype in the complement regulatory gene factor H (HF1/CFH) predisposes individuals to age-related macular degeneration. Proc Natl Acad Sci USA. 2005;102:7227–7232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lamoreaux WJ, Fitzgerald MEC, Reiner A, Hasty KA, Charles ST. Vascular endothelial growth factor increases release of gelatinase A and decreases release of tissue inhibitor of metalloproteinases by microvascular endothelial cells in vitro. Microvasc Res. 1998;55:29–42 [DOI] [PubMed] [Google Scholar]
- 9. Takeda A, Baffi J, Kleinman M, et al. CCR3 is a therapeutic and diagnostic non-inflammatory target for neovascular age-related macular degeneration. Nature. 2009;460:225–230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ahmad I, Balasubramanian S, Del Debbio CB, et al. Regulation of ocular angiogenesis by Notch signaling: implications in neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci. 2011;52:2868–2878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Li Y, Huang D, Xia X, Wang Z, Luo L, Wen R. CCR3 and choroidal neovascularization. PLoS ONE. 2011;6:e17106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Monaghan-Benson E, Hartmann J, Vendrov AE, et al. The role of vascular endothelial growth factor-induced activation of NADPH oxidase in choroidal endothelial cells and choroidal neovascularization. Am J Pathol. 2010;177:2091–2102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Peterson LJ, Wittchen ES, Geisen P, Burridge K, Hartnett ME. Heterotypic RPE-choroidal endothelial cell contact increases choroidal endothelial cell transmigration via PI 3-kinase and Rac1. Exp Eye Res. 2007;84:737–744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wang H, Geisen P, Wittchen ES, et al. The role of RPE cell-associated VEGF189 in choroidal endothelial cell transmigration across the RPE. Invest Ophthalmol Vis Sci. 2011;52:570–578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Geisen P, McColm JR, Hartnett ME. Choroidal endothelial cells transmigrate across the retinal pigment epithelium but do not proliferate in response to soluble vascular endothelial growth factor. Exp Eye Res. 2006;82:608–619 [DOI] [PubMed] [Google Scholar]
- 16. Smith W, Assink J, Klein R, et al. Risk factors for age-related macular degeneration: pooled findings from three continents. Ophthalmology. 2001;108:697–704 [DOI] [PubMed] [Google Scholar]
- 17. Espinosa-Heidmann DG, Suner IJ, Catanuto P, Hernandez EP, Marin-Castano ME, Cousins SW. Cigarette smoke–related oxidants and the development of sub-RPE deposits in an experimental animal model of dry AMD. Invest Ophthalmol Vis Sci. 2006;47:729–737 [DOI] [PubMed] [Google Scholar]
- 18. Crabb JW, Miyagi M, Gu X, et al. Drusen proteome analysis: an approach to the etiology of age-related macular degeneration. Proc Natl Acad Sci USA. 2002;99:14682–14687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Eye Disease Case-Control Study Group Antioxidant status and neovascular age-related macular degeneration. Arch Ophthalmol. 1993;111:104–109 [DOI] [PubMed] [Google Scholar]
- 20. Age-Related Eye Disease Study Research Group (AREDS) A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS Report No. 8. Arch Ophthalmol. 2001;119:1417–1436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Teng TS, Lin B, Manser E, Ng DCH, Cao X. Stat3 promotes directional cell migration by regulating Rac1 activity via its activator + PIX. J Cell Sci. 2009;122:4150–4159 [DOI] [PubMed] [Google Scholar]
- 22. Burridge K, Wennerberg K. Rho and Rac take center stage. Cell. 2004;116:167–179 [DOI] [PubMed] [Google Scholar]
- 23. Soga N, Namba N, McAllister S, et al. Rho family GTPases regulate VEGF-stimulated endothelial cell motility. Exp Cell Res. 2001;269:73–87 [DOI] [PubMed] [Google Scholar]
- 24. Ridley AJ, Schwartz MA, Burridge K, et al. Cell migration: integrating signals from front to back. Science. 2003;302:1704–1709 [DOI] [PubMed] [Google Scholar]
- 25. Fukata M, Nakagawa M, Kaibuchi K. Roles of Rho-family GTPases in cell polarisation and directional migration. Curr Opin Cell Biol. 2003;15:590–597 [DOI] [PubMed] [Google Scholar]
- 26. Itoh RE, Kurokawa K, Ohba Y, Yoshizaki H, Mochizuki N, Matsuda M. Activation of Rac and Cdc42 video imaged by fluorescent resonance energy transfer-based single-molecule probes in the membrane of living cells. Mol Cell Biol. 2002;22:6582–6591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ushio-Fukai M, Alexander RW. Reactive oxygen species as mediators of angiogenesis signaling. Role of NAD(P)H oxidase. Mol Cell Biochem. 2004;264:85–97 [DOI] [PubMed] [Google Scholar]
- 28. Salcedo R, Young HA, Ponce ML, et al. Eotaxin (CCL11) induces in vivo angiogenic responses by human CCR3+ endothelial cells. J Immunol. 2001;166:7571–7578 [DOI] [PubMed] [Google Scholar]
- 29. Robitaille G, Christin MS, Clément I, Senécal JL, Raymond Y. Nuclear autoantigen CENP-B transactivation of the epidermal growth factor receptor via chemokine receptor 3 in vascular smooth muscle cells. Arthritis Rheum. 2009;60:2805–2816 [DOI] [PubMed] [Google Scholar]
- 30. Barth BM, Stewart-Smeets S, Kuhn TB. Proinflammatory cytokines provoke oxidative damage to actin in neuronal cells mediated by Rac1 and NADPH oxidase. Mol Cell Neurosci. 2009;41:274–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Miyagaki T, Sugaya M, Murakami T, et al. CCL11–CCR3 interactions promote survival of anaplastic large cell lymphoma cells via ERK1/2 activation. Cancer Res. 2011;71:2056–2065 [DOI] [PubMed] [Google Scholar]