Abstract
Background
Although impaired sensory processing accompanies various clinical conditions, the question of its status as an independent disorder remains open. Our goal was to delineate the comorbidity (or lack thereof) between childhood psychopathology and sensory over-responsivity (SOR) in middle childhood using phenotypic and behavior genetic analyses.
Method
Participants (N=970) were drawn from the Wisconsin Twin Project, a population-based sample of twins and their families. Mothers completed a sensory responsivity checklist when their offspring were on average 7 years old, followed by a diagnostic interview (Diagnostic Interview Schedule for Children; DISC) within 6 – 12 months. We examined the incidence of DISC diagnoses - ADHD, Conduct Disorder, Oppositional Defiance Disorder, Agoraphobia, General Anxiety, OCD, Panic disorder, Separation Anxiety, Social Phobia, Specific Phobia, Depression, Enuresis, Trichtolloma, Tics, selective mutism, and Pica -among children with SOR, and vice-versa. Children with Autism or PDD were excluded from the present study. Additionally, we examined parent reported physical health diagnoses among non-diagnosed children and three groups of children with SOR and/or DISC diagnoses. Biometric models explored common underlying genetic and environmental influences on symptoms of SOR and psychopathology.
Results
A majority of individuals who screened positive for SOR did not qualify for a DISC diagnosis (58.2%), and vice versa (68.3%). Children who screened positive for SOR only and typical children had similar rates of physical health problems. Turning to a dimensional approach, multivariate twin models of demonstrated that modest covariation between SOR and DISC symptoms could be entirely accounted for by common underlying genetic effects.
Conclusions
Our results suggest that SOR occurs independently of recognized childhood psychiatric diagnoses but is also a relatively frequent comorbid condition with recognized diagnoses. Genetic sources of this comorbidity are implicated.
Keywords: Sensory modulation problems, psychopathology, twins, middle childhood
INTRODUCTION
Sensory experiences are one’s conduit to the physical world. However, a subset of the population experiences benign sensory stimuli as threatening, intrusive or painful. Sensory over-responsivity may include intolerance of auditory stimuli such as appliance noise, loud gymnasiums, or various humming or crackling sounds that most persons find inoffensive. Over-responsivity in the tactile domain may occur in response to stimuli such as certain fabrics, clothing tags, or viscous food textures. Aversive sensory experiences may impact one’s ability to master a range of essential developmental tasks and lead to impaired functioning (Bar-Shalita, Vatine, Seltzer & Parush, 2008; Ben-Sasson, Carter & Briggs-Gowan, 2009; Hazen, et al., 2008). Sensory challenges may also negatively impact early important relationships (Thomasgard, 200) and positive social participation during school years (Cosbey, Johnston & Dunn, 2010). For example, over-responsive children might find typical childhood play too loud and be unable to engage in age-appropriate interactions in a school lunchroom or playground. Despite the pervasive nature of sensory over-responsivity for some individuals, these painful experiences may remain largely private and may be easily misinterpreted by parents, teachers, and peers. To study sensory over-responsivity, researchers currently must rely largely on non-standardized questionnaires, observations, or clinical judgment (Royeen & Lane, 1991). Definitive epidemiological studies of sensory over-responsivity are lacking. To systematically evaluate sensory challenges as a clinical entity that persists throughout development, substantial basic research is needed.
Sensory modulation impairments, first identified by Ayers (1964), have long been recognized as a clinical phenomenon by occupational therapists. But debate continues over classifying such impairments as an independent diagnostic entity. Furthermore, problems related to sensory regulation co-occur with a variety of psychiatric and developmental disorders, particularly autism, ADHD, and Fragile X (Baranek, David & Poe, 2006; Hazen et al., 2008; Hofmann & Bitran, 2006). Thus, much of the research on sensory impairment has been conducted on clinical populations. However, not all individuals who exhibit difficulties regulating sensory input display symptoms of other disorders (Aron & Aron, 1997; Kinnealy, Oliver & Wilbarger, 1995; Reynolds & Lane, 2008). Two recent studies have examined the relationship between one common type of sensory impairment, sensory over-responsivity (SOR) and common childhood disorders in population-based samples. Goldsmith, Van Hulle, Arneson, Schrieber & Gernsbacher (2006), reported that auditory and tactile defensiveness were associated with fearful temperament and anxiety in toddlerhood but were largely distinct from other common childhood disorders. Ben-Sasson, et al.(2009) reported that children aged 7–11 years with SOR had elevated externalizing and internalizing symptoms both in early childhood and concurrently. However, no study to date has systematically investigated the overlap between SOR and symptoms related to the full spectrum of DSM disorders in a population-based sample. Common childhood disorders are influenced by both genes and environment (Lahey et al, in press) as are symptoms of SOR (Goldsmith et al. 2006). Yet no studies have explored pleiotropic influences (either genetic or environmental) on SOR and childhood disorders.
Physical health problems often co-occur with mental health problems. For example, Aarons et al. (2008) found that mental health problems significantly predicted respiratory illness among adolescents, and Lemery et al. (2007) found that physical health distinguished low and high behavior problem groups. Currently, no studies have considered the incidence of physical health problems with sensory modulation impairments.
Our objective was to investigate the distinctiveness of SOR utilizing a behavior-genetic framework in a large community-based sample of school-age twins. We employed two approaches: (1) we examined phenotypic distinctiveness between sensory over-responsivity symptoms and a wide-range of mood and behavioral disorders and specific physical health disorders (both common and rare); and (2) we explored possible common genetic or environmental etiology between symptoms of various common childhood disorders and symptoms of SOR.
METHODS
Design and Sample
Twins were identified from Wisconsin state birth records (Goldsmith, Lemery-Chalfant, Schmidt, Arneson & Schmidt, 2007); approximately 74% of all families with twins born in Wisconsin between 1997 and 2002 agreed to participate in future studies and thus were recruited to a research panel when their twins were infants/toddlers.
Seven year-old twins (M=85.4 months, SD=7.3) were screened for child psychopathology via telephone interview with the primary caregiver (>95% mothers) using the behavior problems portion of the Health and Behavior Questionnaire (HBQ; Armstrong & Goldstein, 2003). Sensory symptoms were measured with the Sensory Over-Responsivity Inventory (SensOR; Schoen, Miller & Green). Complete screening measures were available for 2,361 children. HBQ scores were used to modestly “enrich” a follow-sample for high symptoms; a group of low symptom comparison participants and unselected cotwins of children identified as at-risk or control were also included in the follow-up study conducted 6–12 months after initial screening (Goldsmith et al., 2007). Of the children who were screened, 888 did not qualify for the follow-up study. Of the 1,473 who were initially selected for follow-up, 357 declined to participate or (more commonly) aged out of the target range, and 42 children who exhibited signs of autism or PDD were invited to participate in a separate twin study, leaving 1,074 follow-up participants. Some mothers were unable to complete the DISC interview portion of the follow-up study (N=104), resulting in a final sample of 970 children for whom both SOR screening measures and DISC interviews were available. Parents completed a consent form prior to each phase of the study in accordance with University of Wisconsin Institutional Review Board.
Most twins in this sample were between the ages of 7–8 yrs (M=90.4 months, SD=8.5) during the follow-up study. The sample was 49.2% female and contained approximately equal numbers of monozygotic (MZ; 36%), same-sex dizygotic (DZ; 31%), and opposite sex dizygotic twin pairs (33%). The majority of the sample was Caucasian (83%), with 4% Hispanic, 4% African-American and 6% Other. Mothers had an average of 15.3 years of education; fathers had an education of 14.6 years on average. Median income was between $60,000 and $70,000 with 80% of the sample reporting an annual income of $35,000 or more.
Zygosity was classified using a combination of parental report (Zygosity Questionnaire for Young Twins; Goldsmith, 1991), observer ratings, birth records, and genotyping. The zygosity questionnaire alone yields over 95% agreement with zygosity determined via genotyping (Forget-Dubois et al., 2003; Price et al., 2000). If the zygosity questionnaire and observer ratings did not result in a clear assignment of zygosity, we examined hospital pathology reports on the placenta(e) or genotyped 15 highly polymorphic alleles. Seventeen pairs (3.4%) for whom zygosity could not be unambiguously determined were excluded from genetic analyses.
Assessments
Probable diagnoses were obtained by interviewing primary caregivers in their homes using the Diagnostic Interview Schedule for Children (DISC, Version IV; Fisher, Lucas & Shaffer, 1997), a computer assisted, structured psychiatric interview that yields both diagnoses and symptom counts based on DSM-IV criteria. DISC modules included ADHD, Conduct Disorder, Oppositional Defiance Disorder, Agoraphobia, General Anxiety, OCD, Panic disorder, Separation Anxiety, Social Phobia, Specific Phobia, Depression, Enuresis, Trichtolloma, Tics, selective mutism, and Pica.
Symptoms of over-responsivity were obtained using the SensOR (Schoen et al. 2008), which taps both auditory symptoms (e.g., the sound of the toilet flushing bothers my child) and tactile symptoms (e.g., finger paint on my child’s hands bothers him/her). The SensOR is the only scale designed specifically to differentiate SOR from typical responsivity and is highly correlated with comparable scales from the Dunn’s Short Sensory Profile (Schoen et al. 2008).
Thirty items relate to tactile over-responsivity and include reactions to contact with substances or surfaces, grooming activities, and contact with people. Twenty-two items relate to auditory over-responsivity and include reactions to mildly irritating noises (e.g., vacuum cleaner or siren), background noises, and loud places (e.g., concerts or cafeterias). Mothers indicated whether the child was “bothered” by each experience (0=no, 1=yes). Separate auditory (Cronbach’s α =.82) and tactile (Cronbach’s α =.83) scores were created by summing across the relevant items. No specific items had an extreme influence on either scale. Finally, auditory and tactile summary scores were moderately correlated (r = .47).
The Physical Health section of the HBQ (Armstrong & Goldstein, 2003), was administered during the follow-up study and used to assess frequency of 16 chronic health conditions, ranging from relatively common (asthma) to rare (cystic fibrosis), as well as problems related to speech, language, hearing and vision. For each twin, the mother was provided a list of medical conditions and asked to indicate whether her child had ever had the condition. Health conditions were scored as never (0) or ever (1) occurring during the child’s lifetime.
Parental history of psychopathology was assessed via the Composite International Diagnostic Interview (CIDI; Robins, 1988). The CIDI generates a lifetime diagnosis based on ICD-10 and DSM-III-R definitions and criteria. Most mothers (N=458) and two-thirds of fathers (N=299) completed the CIDI. Parents were administered sections related to depression, phobias, anxiety, alcohol abuse, and alcohol dependence.
Data Analytic Approach
Our main research question regarding the comorbidity of SOR and behavior problems is purely descriptive. We used logistic models (SAS 9.1) to test whether the child physical health or parental mental health problems occurred with greater frequency among children (or families) with DISC diagnoses and/or who screened positive for SOR compared with typical children (or families), as described in the Results section. Child physical health problems and parental mental health were coded as present or absent.
We fit bivariate correlated factors(Loehlin, 1996) and multivariate psychometric twin models (McArdle & Goldsmith, 1990) to explore the genetic and environmental correlations between symptoms of behavior problems and SOR. Both of these models are extensions of the traditional twin model that is used in quantitative behavioral genetic studies. These models use information from the observed twin variances/covariances to partition the overall observed variance/covariance into latent additive genetic (A), common (or shared) environmental (C), and nonshared environmental (E) influences (Neale & Cardon, 1992). The proportion of variation associated with genetic differences is called the heritability. Shared environment effects reflect between-family environmental factors that make individuals in a family similar to one another and are expected to affect members of a twin pair to the same degree, regardless of zygosity. Nonshared environmental effects are unique to each individual and include measurement error. Due to the skewed distribution of both SOR and DISC symptoms, all variables were log-transformed prior to genetic analysis.
We fit two multivariate psychometric models to the data. In model 1, a latent externalizing phenotype was indexed by symptom counts for CD, ODD, and ADHD. This latent phenotype, representing the common variation that is shared across DISC disorders, was decomposed into variation due to latent genetic, shared environment, and non-shared environmental influences. Note that non-shared environmental factors that influence this underlying disposition are unbiased by measurement error, which by definition are specific to each observed variable. Variation in a second latent phenotype, indexed by auditory and tactile SOR symptoms, was also decomposed into underlying genetic and environmental influences. The remaining variation that is unique to each DISC disorder or SOR domain is decomposed into trait-specific latent A, C, and E factors. Model 2 replaced the externalizing latent phenotype with an internalizing latent phenotype indexed by depression, social phobia, specific phobia, general anxiety, separation anxiety, and OCD, but was otherwise identical. Covariation between the externalizing or internalizing latent phenotype and SOR latent phenotypes was accounted for by correlations between the A, C, and E factors that influence each latent phenotype; trait-specific factors were assumed to be uncorrelated.
RESULTS
Frequency of DISC Diagnoses and Screening Positive for SOR
We start by examining the phenotypic distinctiveness between sensory over-responsivity and mood and behavioral disorders. For this community sample (enriched slightly for elevated symptoms, as explained above), 390/970 participants (40.2%; 207 girls) qualified for at least one of the 16 DISC diagnoses. Children with Pervasive Developmental Disorder were excluded because they had been recruited for another study. Some diagnoses were rare (e.g., selective mutism and trichotillomania, each with N = 2 cases, 0.21%); some were moderate in frequency (tics, N =33, 3.4%), and others were more common (ADHD, N =78, 8.0%). Compared to children without a DISC diagnosis, those who qualified for at least one DISC diagnosis had parents with fewer years of education (M = 15.4 vs. M = 15.1 for mothers; M=14.1 vs. 14.9, for fathers). No gender or age differences distinguished children who qualified for at least one DISC diagnosis from those who did not. Of the 390 children who received at least one DISC diagnosis, 194 (20%) had specific phobia as one of their diagnoses. While not minimizing the potential seriousness or predictive value of a specific phobia diagnosis, we note the relative ease of qualifying for a specific phobia diagnosis on the DISC. Thus, analyses were conducted with and without specific phobia.
Mean auditory and tactile SOR scores were M=1.1 (SD = 2.2) and M=2.9 (SD=3.5), respectively. Based on consultation with the instrument’s author, we used a threshold of 6 or more symptoms to qualify as at-risk for tactile SOR and 4 or more symptoms to qualify as at-risk for the auditory SOR. Children above the threshold on either domain were classified as screening positive for SOR. Of the 970 children in this sample, 201 (20.7%; 95 girls) screened positive for SOR. Of course, some of these children would not have qualified for an actual diagnosis of Sensory Processing Disorder if they had been evaluated clinically. There were no differences in parental education, gender, or age between children who screened positive for SOR and those who did not.
Overlap and distinctiveness of positive screens for SOR and DISC diagnoses
Of the 201 children who screened positive for SOR, how many also fell into the group of 390 with a DISC diagnosis? The answer is N = 115 (44% girls); that is, 29.5% of the DISC-diagnosed children screened positive for tactile or auditory symptoms. Examining the broad domains of externalizing and internalizing, 58 children comorbid for SOR had an externalizing diagnosis (26% girls) and 81 had an internalizing diagnosis (49% girls). Only 35 of these young children met criteria for an internalizing diagnosis other than specific phobia. Therefore, we repeated this analysis excluding the specific phobias. In this case, we ask, of the 201 children who screened positive for SOR, how many also fell into the reduced group of 265 with at least one DISC diagnosis other than specific phobia? The answer is N = 84 (32% girls), that is, 31.7% of children with a DISC diagnosis other than specific phobia screened positive for tactile or auditory symptoms.
Shifting to the main question of these analyses—the distinctiveness of SOR—85/201 children (42.2%) who screened positive for SOR did not qualify for a DISC diagnosis. When we excluded specific phobia, the number of children who screened positive for SOR but had no DISC diagnosis number rose from 85 to 117 (58.2%).
SOR and DISC Symptom Counts
Children at-risk for SOR who do not qualify for a DISC diagnosis could potentially be prodromal for a DSM condition; if this were true, then the case just made for the distinctiveness of SOR would need to be qualified. To investigate this possibility, we examined mean differences in DISC symptom counts among the subset of children who did not qualify for a DISC diagnosis (N=579; see Table 1). We excluded trichotillomania, tics, selective mutism, and pica due to infrequent endorsement. Children who screened positive for SOR had higher mean symptom counts than children who were not positive on SOR on six of the remaining 11 DISC disorders: Specific Phobia, depression, Panic Disorder, Generalized Anxiety, OCD, and ADHD. Conversely, among children who did not screen positive for SOR, children who qualified for at least one DISC diagnosis nevertheless endorsed more symptoms of SOR than children who did not qualify for a DISC diagnosis (auditory: M = 0.58 vs. 0.36, Wald test χ2(1)=2.9, p=.004; tactile: M = 2.4 vs. 1.8, Wald test χ2(1))=2.1, p=.03). We conducted similar analyses using a slightly more stringent cut-off (requiring ≥ 8 tactile symptoms rather than 6, but continuing to use ≥ 4 auditory symptoms as the threshold), which lowers the rate of false positives. In general, results were very similar to those already reported. For instance, of the 390 children with a DISC diagnosis, 77 (19.7%) continued to screen positive for SOR, and 67 out of 144 children who still screened positive for SOR did not receive a DISC diagnosis (46.5%).
Table 1.
Mean DISC symptom counts for among the subset of children who do not qualify for a DISC diagnosis by SOR status.
| SOR negative N=86 | SOR positive N-494 | Wald test (χ2(1)) | |
|---|---|---|---|
| Internalizing | |||
|
|
|||
| Depression | 1.20 | 1.92 | 2.6** |
|
|
|||
| Social Phobia | 0.78 | 0.97 | n.s. |
| Specific Phobia | 0.63 | 1.09 | 3.6** |
| Panic | 0.03 | 0.10 | 2.6** |
| General Anx | 1.02 | 1.84 | 4.6** |
| Separation Anx | 0.98 | 2.00 | 4.6** |
| Agoraphobia | 0.02 | 0.05 | n.s. |
| OCD | 0.08 | 0.20 | 2.5* |
| Externalizing | |||
| ADHD | 2.73 | 4.20 | 2.5* |
| ODD | 4.63 | 5.20 | n.s. |
| CD | 0.63 | 1.11 | n.s. |
p<.05,
p<.01
SOR, DISC Diagnosis and Physical Health
For these analyses, children were divided into those who did not screen positive for SOR or qualify for a DISC diagnosis (“typical” group, N=494) and three non-typical profiles: those who screened positive for SOR but did not qualify for a DISC diagnosis (SOR only, N=86), those who received a DISC diagnosis but did not screen positive for SOR (DISC only, N=275), and finally those who screened positive for SOR and received a DISC diagnosis (comborbid, N=115). Physical health data were missing for 51 children. Table 2 presents the number of children in each group who were reported by mothers to have ever experienced a specific physical health problem. Children who screened positive for SOR and qualified for a DISC diagnosis consistently had higher rates of health problems compared with the other groups. For instance, the odds of having allergies were 2.1 times higher for comorbid children than typical children. Children who screened positive only for SOR tended to have similar rates of medical disorders as children in the typical group. However, children who screened positive for SOR regardless of DISC diagnosis were more likely have hearing problems than children who did not screen positive for SOR.
Table 2.
Frequency of mother reported health problems for children with typical and non-typical profiles.
| “Typical” (N=494) | SOR only (N = 86) | DISC only (N=275) | Comorbid (N=115) | Wald test (χ2(3)) | |
|---|---|---|---|---|---|
| arthritis | 0 | 0 | 0 | 0 | NA |
| asthma | 67 (14.5%) | 8 (9.7%) | 33 (12.6%) | 25a (23.4%) | n.s. |
| other lung disease | 7 (1.5%) | 1 (1.2%) | 7 (2.7%) | 3 (2.8%) | n.s |
| birth defect | 3 (0.9%) | 2 (2.4%) | 4 (1.5%) | 2 (1.9%) | n.s |
| blood disease | 3 (0.6%) | 0 | 5 (1.9%) | 1 (0.9%) | NA |
| bowel disease | 13 (2.8%) | 4 (4.9%) | 12 (4.6%) | 13a (12.1%) | 13.8** |
| chronic heart problem | 4 (0.9%) | 0 | 3 (1.2%) | 0 | NA |
| cystic fibrosis | 0 | 0 | 0 | 0 | NA |
| diabetes | 0 | 0 | 2 (0.8%) | 1 (0.9%) | NA |
| HIV | 0 | 0 | 0 | 0 | NA |
| Luekemia or cancer | 1 (.2%) | 0 | 0 | 0 | NA |
| Kidney disease | 0 | 0 | 0 | 1 (0.9%) | NA |
| cerebral palsey | 5 (1.1%) | 1 (1.2%) | 2 (0.8%) | 3 (2.8%) | n.s. |
| persistent ear infections | 82 (17.6%) | 18 (21.9%) | 60 (23.0%) | 32a (29.9%) | n.s. |
| persistent urinary infection | 8 (1.7%) | 2 (2.4%) | 7 (2.7%) | 4 (3.7%) | n.s. |
| allergies requiring intervention | 40 (8.5%) | 9 (11.0%) | 42a (16.1%) | 19a (17.8%) | 10.9* |
| Other health problems | 78 (15.8%) | 19 (22.0%) | 61a (22.2%) | 27a (23.4%) | 7.5* |
| Learning Disorders | 39 (8.4%) | 12 (15.0%) | 40a (15.4%) | 20a (18.7%) | 12.7** |
| Speech problems | 100(21.4%) | 22 (26.8%) | 68 (26.1%) | 31 (29.3%) | n.s |
| Hearing problems | 10 (2.2%) | 7a (8.7%) | 14a (5.4%) | 10a (9.6%) | 14.0** |
| Vision problems | 63 (13.6%) | 7 (8.8%) | 37 (14.3%) | 20 (18.9%) | n.s |
p<.05,
p<.01
Odds of mother endorsing health problem are significantly higher compared to typical group.
SOR, DISC Diagnosis and Parental Psychopathology
We interviewed parents to determine lifetime diagnoses. Roughly half of parents qualified for at least one CIDI lifetime diagnosis (50.4% of mothers and 47.5% of fathers). Alcohol abuse was the most common diagnosis (24% of mothers and 41% of fathers) followed by depression (23% of mothers and 11% of fathers). To avoid counting parents twice, families rather than individual children were divided into groups analogous to those described above: families in which neither twin screened positive for SOR or received a DISC diagnosis (N=137); families in which at least one child screened positive for SOR but neither child received a DISC diagnosis (N=41); families in which neither child screened positive for SOR but at least one child received a DISC diagnosis (N=158); and families in which at least one child was comorbid for SOR and psychopathology (N=81). There were no differences among the four groups in odds of paternal psychopathology with exception of alcohol dependency (see Table 3). Mothers in all non-typical families had greater odds of reporting alcohol abuse and depression. Mothers of children who qualified for at least one DISC diagnosis, regardless of SOR status, also had greater odds of qualifying for a diagnosis of anxiety and specific phobia (see Table 3).
Table 3.
Frequency of CIDI diagnosis among parents in families with typical and non-typical profiles.
| “Typical” | SOR only | DISC only | Comorbid | Wald test (χ2(3)) | |
|---|---|---|---|---|---|
| Mothers | (N = 137) | (N = 41) | (N = 158) | (N = 81) | |
| Alchohol Dependency | 5 (3.7) | 5 (12.2) | 17 (10.8) | 7 (8.6) | n.s. |
| Alchohol Abuse | 21 (15.3) | 12 (29.2) | 44a (27.8) | 20a (24.5) | 8.5* |
| Depression | 15 (10.9) | 15a (36.6) | 46a (29.1) | 25a (29.6) | 23.8** |
| Specific Phobia | 14 (10.2) | 3 (7.9) | 17 (10.8) | 24a (29.6) | 21.2** |
| Anxiety | 14(11.3) | 8 (19.5) | 28a (21.2) | 14a (20.0) | 9.3* |
| Fathers | (N = 94) | (N =29) | (N = 106) | (N = 44) | |
| Alchohol Dependency | 3 (3.2) | 1 (3.5) | 14a (13.2) | 6a (13.6) | 9.4* |
| Alchohol Abuse | 33 (35.0) | 12 (41.4) | 47 (31.1) | 17 (38.6) | n.s. |
| Depression | 12 (12.8) | 4 (13.8) | 10 (9.4) | 3 (6.8) | n.s. |
| Specific Phobia | 6 (6.4) | 2 (6.9) | 5 (4.7) | 3 (6.8) | n.s. |
| Anxiety | 9 (9.6) | 2 (6.9) | 6 (5.7) | 7 (15.9) | n.s. |
p<.05,
p<.01
Odds of qualifying for a diagnosis significantly higher compared to typical group.
Shared Etiology of SOR and DISC Symptoms
We turn now to our second approach. Here we explore the relationship between mean SOR and DISC symptoms using behavior genetic methods. Intraclass cross-twin MZ and DZ correlations for each trait as well as with within-twin, cross-trait (i.e. phenotypic) correlations and the cross-twin, cross-trait correlations are shown in Table 4. Recall, the extent to which MZ twins are more highly correlated across two different traits than DZ twins indicates the extent to which those two traits are influenced by a common set of latent genetic influences. The pattern of intraclass correlations for each variable indicated significant genetic influences on all symptoms. However, the cross-twin, cross-trait correlations were generally low (all <.26) and similar across zygosity with the exception of tactile SOR and mean symptoms of CD and ADHD.
Table 4.
Correlations between mean DISC symptom counts and mean SOR symptom counts, within and across twins.
| Intraclass (Cross-twin) Correlation | Phenotypic (Cross-trait) Correlation | Cross-twin, Cross-trait Correlation | ||||||
|---|---|---|---|---|---|---|---|---|
| Tactile | Auditory | Tactile | Auditory | |||||
| Symptom domains | MZ | DZ | MZ | DZ | MZ | DZ | ||
| Depression | 0.51 | 0.34 | 0.18 | 0.18 | 0.15 | 0.11 | 0.12 | 0.15 |
| Social Phobia | 0.39 | 0.09 | 0.16 | 0.11 | 0.20 | 0.11 | 0.11 | 0.16 |
| Specific Phobia | 0.65 | 0.33 | 0.19 | 0.25 | 0.14 | 0.15 | 0.22 | 0.15 |
| General Anxiety | 0.43 | 0.24 | 0.21 | 0.21 | 0.10 | 0.18 | 0.14 | 0.17 |
| Separation Anxiety | 0.52 | 0.34 | 0.21 | 0.19 | 0.11 | 0.16 | 0.15 | 0.19 |
| Conduct Disorder | 0.82 | 0.53 | 0.19 | 0.14 | 0.25 | 0.10a | 0.16 | 0.11 |
| Attention Deficit Hyperactivity | 0.72 | 0.21 | 0.17 | 0.16 | 0.26 | 0.15a | 0.14 | 0.20 |
| Oppositional Defiant | 0.78 | 0.49 | 0.15 | 0.13 | 0.15 | 0.13 | 0.15 | 0.11 |
| Tactile | 0.74 | 0.42 | ||||||
| Auditory | 0.69 | 0.34 | ||||||
Note: p<.05 for all correlations.
MZ twin correlation significantly larger than DZ twin correlation
We first fit a series of bivariate correlated factors models (McArdle & Goldsmith, 1990), pairing each DISC symptom domain with symptoms of either tactile or auditory SOR (excluding agoraphobia, panic disorder, obsessive compulsive disorder, trichotillomania, tics, selective mutism, and Pica due to infrequent endorsement), resulting in 16 separate models. In these models, the observed variation in each manifest variable was decomposed into underlying latent A, C, and E factors, and the covariation between traits was accounted for by correlations between corresponding latent A, C, and E factors. A full description of results are available upon request. Heritability estimates for DISC symptoms were in the moderate range (.39–.65) and somewhat higher for SOR (.65–.70) with the remaining variation accounted for primarily by unique environmental influences. Genetic correlations (rA) ranged from .13 to .41. For both auditory and tactile SOR, genetic correlations were stronger with internalizing symptoms than with externalizing symptoms (average rA = .32 vs. .20). These correlations reflect the extent to which genes influencing DISC symptoms also influence SOR symptoms. Environmental and shared environmental correlations were non-significant. In other words, while the overall covariation between SOR and DISC symptoms is modest, it is almost exclusively due to genetic pleiotropy, according to a standard intrepretation of this approach.
Previous research suggests that DISC categories are indistinct, and multiple disorders may index an underlying predisposition towards externalizing or internalizing behavior problems (Lahey et al. 2008). Factor analyses confirmed that the externalizing (CD, ODD, and ADHD) symptom counts along with depression symptoms loaded on a single factor (loadings>.67), whereas the anxiety related disorders (general anxiety, separation anxiety, social phobia and specific phobia) loaded on a second factor (loadings>.55). Together these factors accounted for 48% of the total variance. Similarly, auditory and tactile symptoms were moderately correlated (r = .47) and might reflect a general tendency toward intense responses to sensation (Miller, Anzalone, Lane, Cermak & Osten, 2008). Thus, we attempted to explore common influences on these more general underlying dispositions.
Standardized parameter estimates for Models 1 and 2 are shown in Figure 1. In Model 1, the latent externalizing phenotypes accounted for 63–68% of the variation in each DISC disorder, and the latent SOR phenotype accounted for 57–69% of the variance in tactile and auditory SOR. The model fit the data reasonably well with RMSEA = .030 and CFI = .975. An RMSEA < .05 indicates a close approximate fit (Browne & Cudeck, 1993) and CFI > .95 indicates a good fit (Hu & Bentler, 1999). Additive genetic factors accounted for nearly all variation in the latent externalizing and SOR phenotypes, with a small contribution from non-shared environment, but no shared environmental influences. In contrast, variance specific to each disorder was more evenly split between genetic and non-shared environmental influences. There was a significant genetic correlation between the additive genetic influences on the latent externalizing phenotype and the additive genetic influences on the latent SOR phenotype (ra = .34). In Model 2, the latent phenotypes accounted for 45–70% of the variance in DISC disorder and 62–63% of variance in tactile and auditory SOR. Model 2 also fit the data well (RMSEA = .031, CFI = .948). The genetic correlation between additive genetic influences on latent internalizing and SOR phenotypes was ra = .58, a value that was substantially higher than the genetic correlation of .34 from Model 1. In both models, the correlation between non-shared environmental factors could be dropped without a significant loss in fit (Model 1: Δχ2 = .01, 1 df, p=.92; Model 2: Δχ2 = 3.1, 1 df, p=.07) All shared environmental influences were non-significant with the exception of shared environmental contributions to trait-specific variation in CD and ODD.
Figure 1.
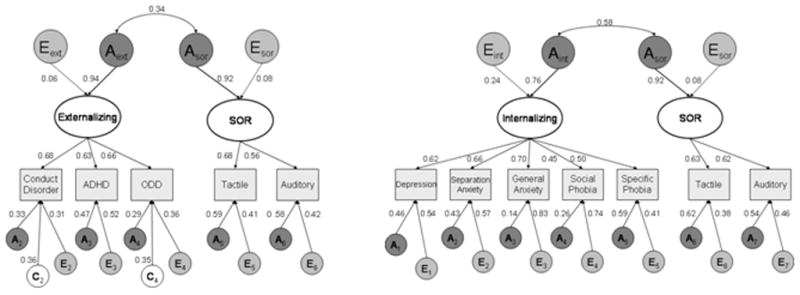
Psychometric model of genetic and environmental influences on latent Externalizing (left panel) or Internalizing (right panel) behavior and Sensory Over-Responsivity indexed by mother-reported DISC and SOR symptoms, respectively.
Note: A = additive genetic influences, C = shared environmental influences, and E = non-shared environmental influences.
DISCUSSION
These data show that a substantial portion of children who screen positive for SOR do not have a DISC diagnosis. However, screening for low base rate phenotypes inevitably leads to false positives (Cohen, 1994) and thus the possibility arises that those who screen positive for SOR with no DISC diagnosis are actually false positives for SOR. Thus, bearing in mind that questions of overlap and distinctiveness crucially depend on base rates, we must ask three questions in interpreting this evidence for partial non-overlap: (1) Would the children who screen positive for SOR but who did not have a DISC diagnosis actually receive an SOR diagnosis if they were to be evaluated clinically by an expert in SOR? A direct answer to this question would require follow-up of children spread across a state and an indirect answer could rely on sensitivity/specificity data from another sample. Given that neither of these options was feasible in this study, we can appeal to deeper analyses of the existing data. For instance, 48 of the 201 children who screened positive for SOR were above threshold on both the tactile and auditory scales. These “doubly positive” children would seem likely to be true positives (i.e., they would likely qualify for an SOR diagnosis if evaluated). Nineteen of these children had a DISC diagnosis other than specific phobia, 13 had a specific phobia diagnosis, and 24 did not have any DISC diagnosis. Thus, this line of evidence supports the notion of “true” partial non-overlap. However, other thresholds on the sensory screener could obviously lead to different results regarding issues of overlap. We explored this by raising the threshold for screening positive (which reduces false positives). Doing so did not attenuate the evidence for partial distinctiveness of SOR. (2) Do the children who screen positive for SOR and do not have a DISC diagnosis qualify for a PDD diagnosis? As mentioned above, children who were known to have a PDD diagnosis were recruited for a study of autism and excluded from the follow-up. Thus, very few children with PDD (presumably those with later diagnoses) would have been in the sample of 970. Thus, the known co-occurrence of sensory symptoms with PDD (Rogers & Oznoff, 2005) could not have accounted for the non-overlap. (3) Do the children who screen positive for SOR and do not have a DISC diagnosis qualify for some other medical diagnosis? As noted before, children who screen positive for SOR only have the same rates of medical problems than typically developing children.
Interestingly, mothers of children who screened positive for SOR or a DISC disorder (and especially both) are more likely to report a history of mental illness. This finding suggests that mothers might pass on genes related to SOR and psychopathology symptoms or that mothers with a history of mental illness might be biased towards endorsing SOR symptoms or be more sensitive to such issues in their offspring. We examined possible shared etiology between symptoms of externalizing or internalizing behavior problems and symptoms of SOR in children. The latent externalizing (or internalizing) and SOR phenotypes accounted for a majority of variation in individual DISC disorders and SOR domains respectively. Genetic factors strongly influenced the latent phenotypes, however, non-shared environmental factors accounted for a substantial portion of the trait specific variation. Although all covariance between the latent externalizing or internalizing factors and SOR phenotypes could be attributed to genetic influences, the covariance was modest in magnitude (34% and 58% respectively). Greater covariance between SOR and internalizing than externalizing symptoms is perhaps unsuprising in the light of previous studies showing children (typical and atypical) who display elevated symptoms of SOR also tend to be at elevated risk for anxiety (Goldsmith et al. 2006; Green & Ben-Sasson, 2010).
Limitations and Conclusion
The most critical limitation of the study is what generally characterizes research regarding sensory modulation problems: we relied on survey methods rather than obtaining a formal diagnosis of SOR. However, the senSOR Inventory has been shown to discriminate between typically developing individuals and a group of children identified as exhibiting SOR in a clinical evaluation (Schoen et al., 2008). As always, caution must be exercised when applying results obtained on twin populations to singleton births. In addition, data on SOR prevalence and correlates among non-Caucasian populations is sparse, making it difficult to determine whether these findings apply to other ethnicities.
CONCLUSIONS
The data support the idea that a subset of children with symptoms of putative Sensory Processing Disorder does not qualify for other diagnoses. As we have emphasized, various qualifications apply to this tentative support. Another observation is that sensory symptoms are commonly reported across the full range of childhood diagnoses studied, and it is conceivable that the sensory symptoms might be primary rather than secondary in some of these cases.
Key Points.
Sensory modulation problems, especially sensory over-responsivity, are known to co-occur with a variety of childhood disorders such Fragile X and ADHD.
Some research suggests sensory modulation problems also exist independently of other disorders.
We found that SOR occurred independently of common childhood psychiatric diagnoses in nearly half of all children who screened positive for SOR in a population-based sample.
SOR is also a relatively frequent comorbid condition with recognized diagnoses, and genetic factors are likely a main contributor to this comorbidity.
Acknowledgments
This work was supported by research grants from the National Institute of Mental Health (R01 MH59785 and R37 MH50560 to Goldsmith), the Wisconsin Center for Affective Science (P50 MH069315), the Wallace Research Foundation. Infrastructure support was provided by the Waisman Center via a core grant from the National Institute of Child Health and Human Development (P30 HD03352).
Abbreviations
- SOR
Sensory Over-responsivity
- SenSOR
Sensory Over-responsivity Inventory
- DISC
Diagnostic Interview Schedule for Chidlren
- HBQ
Health and Behavior Questionnaire
- CIDI
Composite International Diagnostic Interview
References
- Aarons GA, Monn AR, Leslie LK, Garland AF, Ludo L, Hough R, Brown SA. Association between mental and physical heatlh problems in high-risk adolescents: a longitudinal study. Journal of Adolescent Health. 2008;43:260–267. doi: 10.1016/j.jadohealth.2008.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong JM, Goldstein LH. MacArthur Foundation Research Network on Psychopathology and Development. Pittsburgh: University of Pittsburgh; 2003. The MacArthur Working Group on Outcome Assessment: Manual for the MacArthur Health and Behavior Questionnaire (HBQ 1.0) [Google Scholar]
- Aron EN, Aron A. Sensory processing sensitivity and its relation to introversion and emotionality. Journal of Personality & Social Psychology. 1997;73:354–368. doi: 10.1037//0022-3514.73.2.345. [DOI] [PubMed] [Google Scholar]
- Ayers AJ. Patterns of perceptual-motor dysfunction in children: a factor analytic approach. Perceptual Motor Skills. 1964;20:335–368. doi: 10.2466/pms.1965.20.2.335. [DOI] [PubMed] [Google Scholar]
- Baranek GT, David FJ, Poe MD. Sensory experience questionnaire: Discriminating sensory features in young children with autism, developmental delays, and typical development. Journal of Child Psychology & Psychiatry. 2006;47:591–601. doi: 10.1111/j.1469-7610.2005.01546.x. [DOI] [PubMed] [Google Scholar]
- Bar-Shalita T, Vatine JJ, Seltzer Z, Parush S. Sensory modulation disorder: a risk factor for participation in daily life activities. Developmental Medical Child Neurology. 2008;50:932–937. doi: 10.1111/j.1469-8749.2008.03095.x. [DOI] [PubMed] [Google Scholar]
- Ben-Sasson A, Carter AS, Briggs-Gowan MJ. Sensory over-responsivity in elementary school: Prevalence and social-emotional correlates. Journal of Abnormal Psychology. 2009;37:705–716. doi: 10.1007/s10802-008-9295-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne M, Cudeck R. Alternative ways of assessing model fit. Sociological Methods Research. 1993;21:230–258. [Google Scholar]
- Cohen J. The Earth is round (p<.05) American Psychologist. 1994;49:997–1003. [Google Scholar]
- Cosbey J, Johnston SS, Dunn ML. Sensory processing disorders and social participation. American Journal of Occupational Therapy. 2010;64:462–473. doi: 10.5014/ajot.2010.09076. [DOI] [PubMed] [Google Scholar]
- Fisher PW, Lucas C, Shaffer D. Diagnostic interview schedule for children, Version IV (DISC IV): Test-retest reliability in a clinical sample. Paper presented at: 44th Annual Meeting of the American Academy of Child and Adolescent Psychiatry; 1997; Toronto. 1997. [Google Scholar]
- Forget-Dubois N, Pérusse D, Turecki G, Girard A, Billette JM, Rouleau G. Diagnosing zygosity in infant twins: Physical similarity, genotyping, and chorionicity. Twin Research in Human Genetics. 2003;6:479–485. doi: 10.1375/136905203322686464. [DOI] [PubMed] [Google Scholar]
- Green SA, Ben-Sasson A. Anxiety Disorders and Sensory Over-Responsivity in Children with Autism Spectrum Disorders: Is There a Causal Relationship? Journal of Autism and Developmental Disorders. 2010;40:1495–1504. doi: 10.1007/s10803-010-1007-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsmith HH. A zygosity questionnaire for young twins: A research note. Behavior Genetics. 1991;21:257–269. doi: 10.1007/BF01065819. [DOI] [PubMed] [Google Scholar]
- Goldsmith HH, Lemery-Chalfant K, Schmidt NL, Arneson CL, Schmidt CK. Longitudinal analyses of affect, temperament, and childhood psychopathology. Twin Research in Human Genetics. 2007;10:118–126. doi: 10.1375/twin.10.1.118. [DOI] [PubMed] [Google Scholar]
- Goldsmith HH, Van Hulle CA, Arneson CL, Schrieber JE, Gernsbacher MA. A population-based twin study of parentally reported tactile and auditory defensiveness in young children. Journal of Abnormal Child Psychology. 2006;34:393–407. doi: 10.1007/s10802-006-9024-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazen EP, Reichert EL, Piacentini JC, Miguel EC, do Rosario MC, Pauls D, Geller DA. Case series: Sensory intolerance as a primary symptom of pediatric OCD. Annals of Clinical Psychiatry. 2008;20:199–203. doi: 10.1080/10401230802437365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Bitran S. Sensory processing sensitivity in social anxiety disorder: Relationship to harm avoidance and diagnostic subtypes. Journal of Anxiety Disorders. 2007;21:944–954. doi: 10.1016/j.janxdis.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, Bentler P. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Kinnealey M, Oliver B, Wilbarger PA. Phenomenological study of sensory defensiveness in adults. American Journal of Occupational Therapy. 1995;49:444–51. doi: 10.5014/ajot.49.5.444. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Rathouz PJ, Van Hulle CA, Urbano RC, Krueger RF, Applegate B, Garriock HA, Chapman DA, Waldman ID. Testing structural models of the DSM-IV symptoms of common forms of child and adolescent psychopathology. Journal of Abnormal Child Psychology. 2008;36:187–206. doi: 10.1007/s10802-007-9169-5. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Van Hulle CA, Singh AL, Waldman ID, Rathouz PJ. Higher-order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Archives of General Psychiatry. doi: 10.1001/archgenpsychiatry.2010.192. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemery-Chalfant K, Schreiber JE, Schmidt NL, Van Hulle CA, Essex MJ, Goldsmith HH. Assessing internalizing, externalizing, and attention problem in young children: Validation of the MacArthur HBQ. Journal of the American Academy of Chid & Adolescent Psychiatry. 2007;46:1315–1323. doi: 10.1097/chi.0b013e3180f616c6. [DOI] [PubMed] [Google Scholar]
- Loehlin JC. The Cholesky approach: a cautionary note. Behavior Genetics. 1996;26:65–69. [Google Scholar]
- McArdle JJ, Goldsmith HH. Alternative common factor models for multivariate biometric analyses. Behavior Genetics. 1990;20:569–608. doi: 10.1007/BF01065873. [DOI] [PubMed] [Google Scholar]
- Miller L, Anzalone M, Lane S, Cermak SA, Osten E. Concept evolution in sensory integration. A proposed noslogogy for diagnosis. American Journal of Occupational Therapy. 2007;61:135–140. doi: 10.5014/ajot.61.2.135. [DOI] [PubMed] [Google Scholar]
- Neale MC, Cardon L. Methodology for genetic studies of twins and families. Boston: Kluwer; 1992. [Google Scholar]
- Price TS, Freeman B, Craig I, Petrill SA, Ebersole L, Plomin R. Infant zygosity can be assigned by parental report questionnaire. Twin Research in Human Genetics. 2003;3:129–133. doi: 10.1375/136905200320565391. [DOI] [PubMed] [Google Scholar]
- Reynolds S, Lane SJ. Diagnostic Validity of Sensory Over-Responsivity: A Review of the Literature and Case Reports. Journal of Autism & Developmental Disorders. 2008;38:516–529. doi: 10.1007/s10803-007-0418-9. [DOI] [PubMed] [Google Scholar]
- Robins LN. The composite international diagnostic interview – an epidemiologic instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Archives of General Psychiatry. 1988;45:1069–1077. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- Rogers SJ, Oznoff S. What do we know about sensory dysfunction in autism? A critical review of the empirical evidence. Journal of Child Psychology & Psychiatry. 2005;46:1255–1268. doi: 10.1111/j.1469-7610.2005.01431.x. [DOI] [PubMed] [Google Scholar]
- Royeen CB, Lane SJ. Tactile processing and sensory defensiveness. In: Fisher A, Murry E, Bundy A, editors. Sensory Integration: Theory and practice. Philadelphia, PA: FA Davis Company; 1991. pp. 108–133. [Google Scholar]
- Schoen SA, Miller LJ, Green KE. Pilot study of the sensory over-responsivity scales: assessment and inventory. American Journal of Occupational Therapy. 62:393. doi: 10.5014/ajot.62.4.393. [DOI] [PubMed] [Google Scholar]
- Thomasgard M. Working with challenging young children: relations between child temperament, response to novelty and sensory processing. Clinical Pediatrics. 2003;42:197–204. doi: 10.1177/000992280304200302. [DOI] [PubMed] [Google Scholar]


