Abstract
Existing evidence linking residential proximity to food establishments with body mass index (BMI; weight (kg)/height (m)2) has been inconclusive. In this study, the authors assessed the relation between BMI and proximity to food establishments over a 30-year period among 3,113 subjects in the Framingham Heart Study Offspring Cohort living in 4 Massachusetts towns during 1971–2001. The authors used novel data that included repeated measures of BMI and accounted for residential mobility and the appearance and disappearance of food establishments. They calculated proximity to food establishments as the driving distance between each subject’s residence and nearby food establishments, divided into 6 categories. The authors used cross-classified linear mixed models to account for time-varying attributes of individuals and residential neighborhoods. Each 1-km increase in distance to the closest fast-food restaurant was associated with a 0.11-unit decrease in BMI (95% credible interval: −0.20, −0.04). In sex-stratified analyses, this association was present only for women. Other aspects of the food environment were either inconsistently associated or not at all associated with BMI. Contrary to much prior research, the authors did not find a consistent relation between access to fast-food restaurants and individual BMI, necessitating a reevaluation of policy discussions on the anticipated impact of the food environment on weight gain.
Keywords: body mass index, fast foods, longitudinal studies, multilevel analysis, obesity, weight gain
The rapid increase in weight in the United States over the last 30 years has been posited to be driven by changes in environmental conditions, above other factors (1–3). A key environmental factor that has received considerable attention is the role of the food environment, specifically the role of fast-food restaurants (1). The increase in away-from-home food expenditures (4), increased consumption of fast food and sugar-sweetened beverages (5), and rising portion sizes (6) are several potential mechanisms through which the food environment could contribute to higher body mass index (BMI).
Evidence regarding the association between people’s food environments and their BMIs remains inconclusive. Most prior studies have found associations between BMI and proximity to fast-food restaurants (7–14), convenience stores (10, 15), full-service restaurants (7), or supermarkets and grocery stores (10, 15–21). Other studies have found no relation between food establishments and BMI (21–24) or findings pointing in the direction opposite of what would be expected (17, 25). However, most of these studies were limited by the cross-sectional nature of the analysis, incomplete or poor ascertainment of proximity to food establishments, or both. To examine the association between proximity to food establishments and BMI, we linked data from a longitudinal cohort study to novel data regarding the food environment at each of several measurement points over a period of 30 years.
MATERIALS AND METHODS
Sample
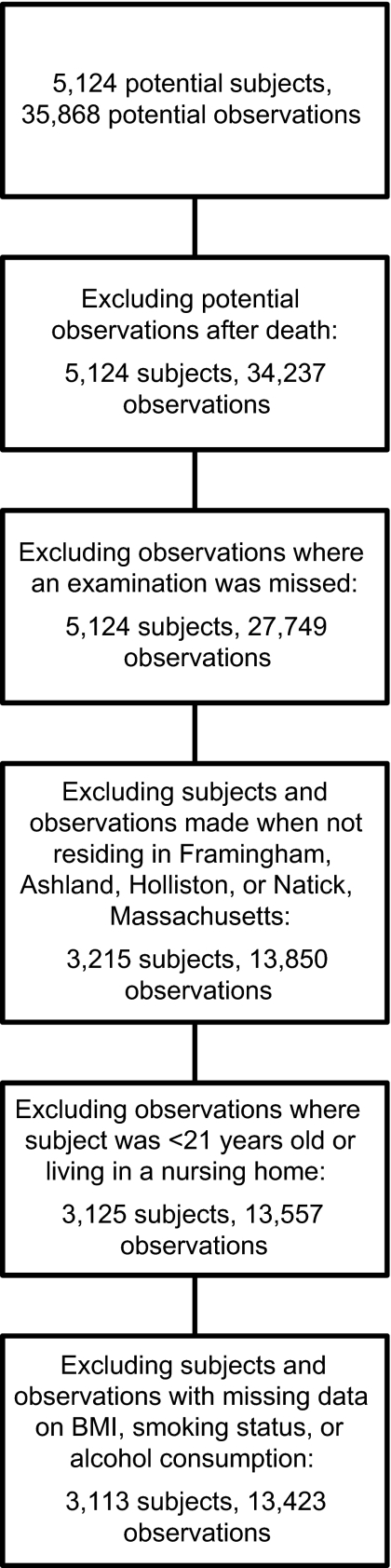
The Framingham Heart Study Offspring Cohort was created in 1971. The Offspring Cohort enrolled 5,124 subjects who were either the children of Original Cohort members or the children’s spouses (26). Subjects have been examined and surveyed repeatedly since enrollment. We used the first 7 waves of data collection (1971–2001) for this study. The prespecified objective of this study was to analyze the association of proximity to food establishments and BMI in a longitudinal fashion, which required detailed collection of historical information on food establishments. Therefore, our sample included only subjects living in a small, concentrated geographic area composed of the 4 principal towns of the Offspring Cohort: Framingham, Natick, Ashland, and Holliston, Massachusetts (which allowed us to personally visit the towns and collect the necessary data). At enrollment, 55.1% of subjects of the Offspring Cohort lived in this area; at wave 7 (1998–2001), 40.2% lived in this area. We excluded observations with missing data on BMI, smoking status, or alcohol intake and those in which a subject was under 21 years of age or living in a nursing home. These criteria resulted in a final sample of 3,113 subjects and 13,423 observations (Figure 1).
Figure 1.
Selection of subjects and observations for an analysis of proximity to food establishments and body mass index (BMI), Framingham Heart Study Offspring Cohort, 1971–2001. A total of 5,124 subjects were enrolled in the Framingham Heart Study Offspring Cohort from 1971 to 1975, and subjects have been examined and surveyed repeatedly. The current study included completed observations made when subjects were living in Framingham, Natick, Ashland, and Holliston, Massachusetts, from 1971 to 2001. The final sample included 13,423 observations from 3,113 subjects.
Outcome and exposure variable
Time-varying individual BMI was the outcome variable, calculated from measured height and weight (weight (kg)/height (m)2). The primary exposure variables were 1) the driving distance between each subject’s residential address and the nearest restaurant or food store, divided into specific categories of establishments, and 2) the mean driving distance to the 5 closest restaurants or food stores, again divided by category at each wave. We calculated distances using ArcGIS, version 9.3 (Esri, Redlands, California). Measuring actual driving distances to food establishments is a more realistic method of determining exposure to establishments than the more commonly used neighborhood density measures. Actual driving distance captures how far it is for a subject to drive to a given establishment rather than simply measuring how many food establishments are located nearby.
We defined the restaurant and food store categories according to the definitions of the North American Industry Classification System, the system used by US federal agencies. Our restaurant categories were fast-food restaurants, full-service restaurants, and bakeries/coffee shops. Our food store categories were chain supermarkets, grocery stores, and convenience stores.
We compiled food establishment names, addresses, category, and years of operation from several sources: files of open and closed food establishments maintained by local boards of health, which inspect food establishments in Massachusetts; historical Framingham-area telephone book yellow pages for selected years from each wave; a targeted search of historical Framingham-area telephone book white pages; and a commercial database compiled by Dun & Bradstreet (Short Hills, New Jersey) for selected years from each wave (16). We collected and geocoded all data for the 4-town primary geographic area, as well as for the 10 additional towns that surround the primary geographic area and could be a source of food establishment exposure for subjects living near the borders of these towns. (Maps of food establishments are available as Web Figures 1 and 2 (http://aje.oxfordjournals.org/).) We validated the final database of food establishments through site visits to presently open establishments and by review of local boards of health and Framingham Heart Study staff. (Further details on the search strategy and food establishment classification are available in Web Methods Note 1.)
Covariates
Individual-level covariates included time-varying attributes (marital status, smoking status, and alcohol consumption) and time-invariant attributes (age at enrollment, sex, and education). Residential addresses for subjects were collected in each wave and subsequently geocoded using ArcGIS. US Census tracts served as our definition of a neighborhood (27, 28). Each address was assigned to one of 24 census tracts contained within the 4-town geographic area at each wave to allow for linkage to neighborhood-level covariates. Because the boundaries of census tracts changed over time, we took the tract boundaries of Census 2000 as fixed across time and geocoded subjects within these boundaries.
We included several US Census-measured neighborhood-level covariates in the models: percentage of residents in the census tract living in poverty, median household income in the census tract, and percentages of census tract residents who were black and Hispanic. We used US Census data from 1970, 1980, 1990, and 2000 to assign these covariates to census tracts, and we used data from the commercial vendor GeoLytics (East Brunswick, New Jersey) to adjust all census data to the 2000 census tract boundaries. We assigned census data to subjects by wave according to the date of their study examination. If the examination occurred between the beginning of the decade and the midpoint of the decade, assignment was made to census data from the beginning of the decade. We included 1 measure of neighborhood walkability in our models: the number of intersections per mile. Using ArcGIS, we calculated the number of street intersections per square mile (per 1.6 km2) for each block group for each subject at each wave.
Analysis
Because some persons moved frequently, no clear nested hierarchy between all observations, individuals, and neighborhoods existed. To account for these repeated measures with changing neighborhood membership over time, we used a cross-classified, multilevel model for the analysis. Observation occasion served as level 1, and individual and neighborhood were separate cross-classified levels for level 2 (Web Figure 3), with a random intercept that was allowed to vary across all combinations of individual and neighborhood. We included a random slope for time indexed by individual subject to ensure that individual weight trajectories were accommodated in the models, and we also included a fixed effect for time. (Further details on the modeling are available in Web Methods Note 2.)
We examined the association between food establishment distance measures for each establishment category and BMI in separate models, with and without adjustment for the individual and neighborhood-level covariates. Neighborhood-level, US Census covariates did not change results appreciably, were not significant in any models, and were excluded from the final analyses. Because interaction terms between the food establishment distance measures and sex were significant in most models, we conducted additional sex-stratified analyses. We analyzed models with BMI as a measure that was contemporaneous to the exposure and covariates. Beta coefficient parameters represent the difference in BMI units (kg/m2) for every 1-km (0.6-mile) increment in the distance to the closest food establishment of each type or the mean distance to the 5 closest food establishments of each type. This 1-km distance is approximately equivalent to 1 standard deviation of the driving distances to establishments across all subjects.
We conducted sensitivity analyses to examine the robustness of the relation between BMI and distance to food establishments. First, we examined the relation between distance and lagged BMI, capturing the relation between distance at each wave and BMI at the following wave. The associated parameter estimates represent the BMI difference for every 1-km incremental difference in the distance to food establishments at the prior wave. Second, to isolate the independent association of each restaurant and food store category with BMI, we created a set of summary variables to capture the relative closeness of food establishment categories to which a subject was exposed at each wave. These measures represent the degree to which a person is closer to one type of food establishment compared with the other types (details are available in Web Methods Note 3). We calculated these relative closeness measures because inclusion of measures of the distance to all types of food establishments in the same model was affected by collinearity, due to high correlations between distances for food establishment categories (Web Tables 1 and 2).
Models were analyzed using Markov chain Monte Carlo methods in MLWin, version 2.12 (Centre for Multilevel Modelling, University of Bristol, Bristol, United Kingdom), to generate multiple iterative samples from the joint posterior distribution of the parameters, from which parameter estimates could be constructed (29). We report parameter estimates from models with 95% credible intervals that reflect the posterior distribution of actual population parameter estimates. Significant findings are defined as those predictors with estimated parameters whose 2-sided 95% credible intervals did not include 0. We generated descriptive results using SAS statistical software, version 9.1 (SAS Institute Inc., Cary, North Carolina). The institutional review board of Harvard Medical School approved this study.
RESULTS
The mean number of observations per subject was 4.31. In terms of residential mobility, 42.9% of subjects never moved throughout the course of their follow-up, and 26.1% moved twice or more. Mean BMI for women increased from 24.2 at wave 1 to 28.0 by wave 7; for men, it increased from 26.7 at wave 1 to 28.9 by wave 7 (Table 1, Web Tables 3–6). For women, the mean driving distance from the residential address to the closest fast-food restaurant decreased from 1,325 m (standard deviation (SD), 934) at wave 1 to 1,140 m (SD, 774) at wave 7. The mean driving distance to the nearest chain supermarket decreased from 4,223 m (SD, 2,405) at wave 1 to 2,599 m (SD, 1,565) at wave 7 (Web Tables 3–6). The values for men were similar.
Table 1.
Characteristics of the Study Sample, Framingham Heart Study Offspring Cohort, 1971–2001
| Characteristic | Women (n = 7,043a) |
Men (n = 6,380) |
||||
| Across Waves | Wave 1 | Wave 7 | Across Waves | Wave 1 | Wave 7 | |
| Mean body mass indexb | 26.0 | 24.2 | 28.0 | 27.6 | 26.7 | 28.9 |
| Mean age, years | 50.8 | 37.9 | 63.1 | 50.9 | 38.9 | 62.9 |
| Education, % | ||||||
| High school or less | 53.6 | 48.2 | 53.2 | 47.2 | 42.2 | 46.0 |
| More than high school | 42.2 | 39.3 | 43.4 | 48.8 | 44.6 | 52.1 |
| Missing data | 4.2 | 12.6 | 3.4 | 4.0 | 13.2 | 1.9 |
| % married | 75.2 | 84.7 | 64.4 | 83.4 | 84.2 | 81.7 |
| % current smokers | 30.8 | 47.2 | 16.4 | 31.4 | 47.4 | 15.4 |
| Alcohol consumption (drinks/day), % | ||||||
| 0 | 35.5 | 17.5 | 45.6 | 22.5 | 9.8 | 31.6 |
| 1–2 | 59.4 | 76.2 | 50.8 | 53.7 | 61.4 | 50.8 |
| >2 | 5.2 | 6.3 | 3.6 | 23.9 | 28.8 | 17.6 |
Number of observations across all waves.
Weight (kg)/height (m)2.
In adjusted models comprising all subjects, close residential proximity to the nearest fast-food restaurant was associated with higher BMI (Table 2). Each 1-km increase (approximately a 1-SD increase) in driving distance to the closest fast-food restaurant was associated with a 0.11-unit decrease in BMI. In sex-stratified analyses, this effect was present only for women, such that each 1-km increase in driving distance to the closest fast-food restaurant was associated with a 0.19-unit decrease in BMI. In adjusted models with BMI lagged by 1 wave, the relation between close proximity to the nearest fast-food restaurant and BMI remained, both in the pooled analysis and in the sex-stratified analysis of women. For every 1-km increase in driving distance to the closest fast-food restaurant, BMI in the subsequent wave decreased by 0.10 units in the pooled analysis and 0.17 units for women (data are shown in Web Tables 7–9). Controlling for the relative closeness of all establishments produced similar results (Web Tables 7–9).
Table 2.
Multilevel, Cross-Classified, Multivariable Regression Parameter Estimates for the Adjusted Change in Body Mass Indexa for Every 1-km Increase in Distance to Food Establishments, Framingham Heart Study Offspring Cohort, 1971–2001b
| Variable | Totalc |
Womend |
Mend |
|||
| βe (n = 13,423f) | 95% CrI | β (n = 7,043) | 95% CrI | β (n = 6,380) | 95% CrI | |
| Distance to closest food establishment | ||||||
| Closest fast-food restaurant | −0.11g | −0.20, −0.04 | −0.19g | −0.32, −0.06 | −0.05 | −0.14, 0.05 |
| Closest full-service restaurant | 0.02 | −0.07, 0.11 | 0.08 | −0.06, 0.21 | −0.05 | −0.14, 0.05 |
| Closest bakery/coffee shop | −0.02 | −0.08, 0.04 | −0.04 | −0.12, 0.05 | −0.01 | −0.07, 0.05 |
| Closest convenience store | 0.02 | −0.06, 0.09 | 0.00 | −0.12, 0.12 | 0.00 | −0.08, 0.08 |
| Closest grocery store | −0.06g | −0.10, −0.01 | −0.07 | −0.15, 0.001 | −0.04 | −0.08, 0.01 |
| Closest chain supermarket | −0.02 | −0.06, 0.01 | −0.03 | −0.08, 0.02 | 0.01 | −0.03, 0.05 |
| Mean distance to closest 5 food establishments | ||||||
| Closest 5 fast-food restaurants | −0.03 | −0.10, 0.05 | −0.05 | −0.16, 0.07 | 0.00 | −0.08, 0.08 |
| Closest 5 full-service restaurants | −0.04 | −0.13, 0.06 | −0.01 | −0.16, 0.14 | −0.04 | −0.15, 0.05 |
| Closest 5 bakeries/coffee shops | −0.03 | −0.08, 0.03 | −0.02 | −0.10, 0.06 | −0.01 | −0.07, 0.05 |
| Closest 5 convenience stores | 0.01 | −0.06, 0.08 | −0.03 | −0.12, 0.09 | 0.03 | −0.05, 0.10 |
| Closest 5 grocery stores | −0.08g | −0.15, −0.03 | −0.11g | −0.21, −0.01 | −0.06 | −0.12, 0.01 |
| Closest 5 chain supermarkets | −0.01 | −0.06, 0.02 | 0.00 | −0.06, 0.06 | 0.00 | −0.04, 0.04 |
Abbreviation: CrI, credible interval.
Weight (kg)/height (m)2.
Results were adjusted for age, time (as both a categorical fixed effect and a linear random effect), education, and time-varying marital status, smoking status, alcohol consumption, and number of intersections per square mile (per 1.6 km2).
Adjusted for sex, in addition to the other covariates.
Sex-stratified analyses were conducted because the interaction between sex and distance to food establishments was significant in most models.
Change in body mass index units (kg/m2).
Number of observations across all waves.
Two-sided 95% credible interval does not contain 0.
Close residential proximity to grocery stores was associated with higher BMI in pooled adjusted analyses and for women (Table 2). For every 1-km increase in driving distance to the closest grocery store, BMI decreased by 0.06 units in the pooled analysis. For every 1-km increase in the mean driving distance to the 5 closest of these stores, BMI decreased by 0.08 units in the pooled analysis and by 0.11 units for women in the sex-stratified analysis. In adjusted models with BMI lagged by 1 wave, no significant association between BMI and distance to grocery stores remained (Web Tables 7–9). In models controlling for the relative closeness of all establishments, a significant association between BMI and mean distance to the 5 closest grocery stores was present in the pooled analysis only (Web Tables 7–9). When examining all remaining types of establishments, we noted no significant associations between food establishment proximity and BMI (Web Tables 7–9).
Among other covariates, predictors of higher BMI for both men and women included time, older age, being married, not smoking, and consuming more than 2 alcoholic drinks per day. A high school education or less and consumption of 1–2 alcoholic drinks daily also were associated with higher BMI for women. These results were consistent in models controlling only for covariates and models controlling for the relative closeness of each food establishment category (Web Tables 10 and 11).
DISCUSSION
In a longitudinal cohort study, we performed a comprehensive assessment of the association between the commercial food environment and individual BMI over a period of 30 years. Contrary to much prior research, we did not find a consistent relation between access to fast-food restaurants and individual BMI. For every 1-km increase in driving distance to the closest fast-food restaurant, BMI decreased by 0.11 units in the overall sample and 0.19 units among women. On the basis of these results, a woman of average height in the Framingham Heart Study Offspring Cohort (63.6 inches or 161.5 cm) would weigh 0.50 kg less for every 1-km increase in driving distance to the nearest fast-food restaurant (or 50 g less for every 100-m increase in driving distance). This small association between distance to fast-food restaurants and BMI for women only is concordant with prior research that has found sex differences in the associations between neighborhood characteristics and BMI (30–33). Such sex differences could arise because women are more aware of their residential neighborhood environments than men (34, 35).
Prior research on the association of weight status with proximity to food establishments has been inconclusive. These prior studies had several limitations that we attempted to surmount in the present study. Most studies have been limited by the use of cross-sectional analyses. Only 4 of the 19 studies we discovered on this topic had any longitudinal component for the outcome (9, 21, 24, 36). Only 2 of these had time-varying exposure data on proximity to food establishments (9, 21). Among the studies that incorporated longitudinal data on both the outcome and exposure, investigators used only 1 source of data on food establishments, which is likely to have limited the number of establishments found, and the researchers measured the proximity to food establishments through crude measures (i.e., number of food establishments per land area or per number of residents) which failed to capture the exact distance between individual residences and food establishments. For example, using birth certificates for over 1.5 million pregnant women who had 2 or more children in Texas, Michigan, and New Jersey from 1989 to 2003, Currie et al. (9) found that the presence of contemporaneous chain fast-food restaurants within 0.5 miles (0.8 km) of the residential address was associated with an increased risk of gestational weight gain (mean increased weight gain of 49 g). In our study, we addressed each of these limitations by including longitudinal data on both BMI and exposure to food establishments, using multiple sources of data on food establishments, and precisely measuring the distances between residential addresses and food establishments in each wave of data collection, accounting for both residential moves by subjects and the opening and closing of establishments across time.
The study findings should be considered with the following caveats. First, we undertook a comprehensive approach to the identification of food establishments across time and combined multiple resources from a discrete geographic area. However, no ideal historical record of food establishments exists. We could have missed some establishments or misclassified their type. If any misclassification occurred in neighborhoods where subjects experienced greater weight gain, the results could be biased. We also could not measure workplace proximity to food establishments, a possible source of unmeasured confounding between BMI and residential proximity to food establishments. Second, because of the extensive effort to identify historical food establishments, the geographic area of the study included only the 4 major towns of the Offspring Cohort. We were not able to follow subjects if they moved out of this area. This limits the generalizability of the study, as does the lack of racial diversity in the Offspring Cohort. However, this limitation in generalizability also strengthens the plausibility of the association’s being causal by removing confounding by design. Because all of the subjects were living in the Framingham area, neighborhoods were more similar than those of diffuse areas, and neighborhoods primarily differed with regard to the exposure rather than other, unobserved factors. The lack of racial diversity is an unavoidable limitation of all research done within the Framingham Heart Study for the past 50 years. Third, the restricted geographic area of our subjects and the ascertainment of food establishment locations limited the range of distances over which subjects could be exposed to food establishments. We cannot extrapolate our associations beyond this limited range. Fourth, we presently lack data on actual food consumption and physical activity in each wave with which to determine whether consumption of specific types of foods or exercise was associated with weight gain in this population and whether these factors might have mediated the relation between close proximity to fast-food restaurants and weight gain; this will be the subject of future research. However, with a weak, inconsistent association found between proximity to fast-food restaurants and BMI, it is doubtful that any mediation of this association, which might result from the inclusion of additional variables, would change the interpretation of our results. Fifth, income data were only available for 1 wave, and there was a high percentage of missing data. As a result, education was the only measure of individual socioeconomic status in this study. The weak association between close proximity to fast-food restaurants and BMI could be accounted for by unobserved income; however, research has demonstrated a high correlation between education and income (37).
In summary, in a large cohort followed over a period of 30 years, after accounting for residential mobility and the appearance and disappearance of food establishments, we did not find a consistent relation between access to fast-food restaurants and a person’s BMI. This will necessitate a reevaluation of policy discussions on the anticipated impact of the food environment on weight gain. This study shows that the food environment’s contribution to reducing or controlling the obesity epidemic may be limited.
Supplementary Material
Acknowledgments
Author affiliations: Department of Population Medicine, Harvard Pilgrim Health Care Institute, Harvard Medical School, Boston, Massachusetts (Jason P. Block); Department of Health Care Policy, Harvard Medical School, Boston, Massachusetts (Nicholas A. Christakis, A. James O’Malley); and Department of Society, Human Development and Health, Harvard School of Public Health, Boston, Massachusetts (S. V. Subramanian).
This work was supported by the National Institute of Aging (grant P01 AG031093; Nicholas A. Christakis, Principal Investigator) and by contract N01-HC-25195 from the National Heart, Lung, and Blood Institute (NHLBI), awarded to the Framingham Heart Study investigators. Dr. Jason P. Block received support from the NHLBI (grant P30 HL101312-01; Dr. Matthew W. Gillman, Principal Investigator) and was supported by the Robert Wood Johnson Health and Society Scholars Program at the Harvard School of Public Health. Dr. S. V. Subramanian was supported by an NHLBI Career Development Award (K25 HL081275) and the Robert Wood Johnson Investigator Award in Health Policy Research.
The authors thank Rebecca Joyce, Laurie Meneades, and Karen Mutalik for the expert assistance required to build the data set.
Results from this study were presented at the Annual Meeting of the Society of General Internal Medicine in April 2010 and the Annual Meeting of the HMO Research Network in March 2011.
Conflict of interest: none declared.
Glossary
Abbreviations
- BMI
body mass index
- SD
standard deviation
References
- 1.Hill JO, Peters JC. Environmental contributions to the obesity epidemic. Science. 1998;280(5368):1371–1374. doi: 10.1126/science.280.5368.1371. [DOI] [PubMed] [Google Scholar]
- 2.Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med. 2006;62(7):1650–1671. doi: 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- 3.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 4.Lin B, Frazão E, Guthrie J. Away-From-Home Foods Increasingly Important to Quality of American Diet. (Agriculture Information Bulletin no. 749) Washington, DC: Agricultural Research Service, US Department of Agriculture; 1999. [Google Scholar]
- 5.Nielsen SJ, Popkin BM. Changes in beverage intake between 1977 and 2001. Am J Prev Med. 2004;27(3):205–210. doi: 10.1016/j.amepre.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Nielsen SJ, Popkin BM. Patterns and trends in food portion sizes, 1977–1998. JAMA. 2003;289(4):450–453. doi: 10.1001/jama.289.4.450. [DOI] [PubMed] [Google Scholar]
- 7.Mehta NK, Chang VW. Weight status and restaurant availability: a multilevel analysis. Am J Prev Med. 2008;34(2):127–133. doi: 10.1016/j.amepre.2007.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chou SY, Grossman M, Saffer H. An economic analysis of adult obesity: results from the Behavioral Risk Factor Surveillance System. J Health Econ. 2004;23(3):565–587. doi: 10.1016/j.jhealeco.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 9.Currie J, DellaVigna S, Moretti E, et al. The Effect of Fast Food Restaurants on Obesity. (NBER Working Paper 14721) Cambridge, MA: National Bureau of Economic Research; 2009. [Google Scholar]
- 10.Spence JC, Cutumisu N, Edwards J, et al. Relation between local food environments and obesity among adults. BMC Public Health. 2009;9:192. doi: 10.1186/1471-2458-9-192. (doi:10.1186/1471-2458-9-192) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Inagami S, Cohen DA, Brown AF, et al. Body mass index, neighborhood fast food and restaurant concentration, and car ownership. J Urban Health. 2009;86(5):683–695. doi: 10.1007/s11524-009-9379-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li F, Harmer P, Cardinal BJ, et al. Built environment and 1-year change in weight and waist circumference in middle-aged and older adults: Portland Neighborhood Environment and Health Study. Am J Epidemiol. 2009;169(4):401–408. doi: 10.1093/aje/kwn398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oreskovic NM, Kuhlthau KA, Romm D, et al. Built environment and weight disparities among children in high- and low-income towns. Acad Pediatr. 2009;9(5):315–321. doi: 10.1016/j.acap.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 14.Maddock J. The relationship between obesity and the prevalence of fast food restaurants: state-level analysis. Am J Health Promot. 2004;19(2):137–143. doi: 10.4278/0890-1171-19.2.137. [DOI] [PubMed] [Google Scholar]
- 15.Morland K, Diez Roux AV, Wing S. Supermarkets, other food stores, and obesity: the Atherosclerosis Risk in Communities Study. Am J Prev Med. 2006;30(4):333–339. doi: 10.1016/j.amepre.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 16.Mujahid MS, Diez Roux AV, Shen M, et al. Relation between neighborhood environments and obesity in the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2008;167(11):1349–1357. doi: 10.1093/aje/kwn047. [DOI] [PubMed] [Google Scholar]
- 17.Zick CD, Smith KR, Fan JX, et al. Running to the store? The relationship between neighborhood environments and the risk of obesity. Soc Sci Med. 2009;69(10):1493–1500. doi: 10.1016/j.socscimed.2009.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lopez RP. Neighborhood risk factors for obesity. Obesity (Silver Spring) 2007;15(8):2111–2119. doi: 10.1038/oby.2007.251. [DOI] [PubMed] [Google Scholar]
- 19.Rundle A, Neckerman KM, Freeman L, et al. Neighborhood food environment and walkability predict obesity in New York City. Environ Health Perspect. 2009;117(3):442–447. doi: 10.1289/ehp.11590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu GC, Wilson JS, Qi R, et al. Green neighborhoods, food retail and childhood overweight: differences by population density. Am J Health Promot. 2007;21(suppl 4):317–325. doi: 10.4278/0890-1171-21.4s.317. [DOI] [PubMed] [Google Scholar]
- 21.Powell LM, Bao Y. Food prices, access to food outlets and child weight. Econ Hum Biol. 2009;7(1):64–72. doi: 10.1016/j.ehb.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 22.Jeffery RW, Baxter J, McGuire M, et al. Are fast food restaurants an environmental risk factor for obesity? Int J Behav Nutr Phys Act. 2006;3:2. doi: 10.1186/1479-5868-3-2. (doi:10.1186/1479-5868-3-2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burdette HL, Whitaker RC. Neighborhood playgrounds, fast food restaurants, and crime: relationships to overweight in low-income preschool children. Prev Med. 2004;38(1):57–63. doi: 10.1016/j.ypmed.2003.09.029. [DOI] [PubMed] [Google Scholar]
- 24.Sturm R, Datar A. Body mass index in elementary school children, metropolitan area food prices and food outlet density. Public Health. 2005;119(12):1059–1068. doi: 10.1016/j.puhe.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 25.Wang MC, Kim S, Gonzalez AA, et al. Socioeconomic and food-related physical characteristics of the neighbourhood environment are associated with body mass index. J Epidemiol Community Health. 2007;61(6):491–498. doi: 10.1136/jech.2006.051680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Feinleib M, Kannel WB, Garrison RJ, et al. The Framingham Offspring Study. Design and preliminary data. Prev Med. 1975;4(4):518–525. doi: 10.1016/0091-7435(75)90037-7. [DOI] [PubMed] [Google Scholar]
- 27.Krieger N, Chen JT, Waterman PD, et al. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures—the Public Health Disparities Geocoding Project. Am J Public Health. 2003;93(10):1655–1671. doi: 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krieger N, Chen JT, Waterman PD, et al. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the Public Health Disparities Geocoding Project. Am J Epidemiol. 2002;156(5):471–482. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- 29.Rasbash J, Steele F, Browne WJ, et al. A User’s Guide to MLWin: Version 2.10. Bristol, United Kingdom: Centre for Multilevel Modelling, University of Bristol; 2009. [Google Scholar]
- 30.Morenoff J, Diez Roux AV, Oyspuk T, et al. Residential Environments and Obesity: What Can We Learn About Policy Interventions From Observational Studies? Ann Arbor, MI: National Poverty Center, Gerald R Ford School of Public Policy, University of Michigan; 2006. [Google Scholar]
- 31.Matheson FI, White HL, Moineddin R, et al. Neighbourhood chronic stress and gender inequalities in hypertension among Canadian adults: a multilevel analysis. J Epidemiol Community Health. 2010;64(8):705–713. doi: 10.1136/jech.2008.083303. [DOI] [PubMed] [Google Scholar]
- 32.Chang VW, Christakis NA. Income inequality and weight status in US metropolitan areas. Soc Sci Med. 2005;61(1):83–96. doi: 10.1016/j.socscimed.2004.11.036. [DOI] [PubMed] [Google Scholar]
- 33.Stafford M, Cummins S, Macintyre S, et al. Gender differences in the associations between health and neighbourhood environment. Soc Sci Med. 2005;60(8):1681–1692. doi: 10.1016/j.socscimed.2004.08.028. [DOI] [PubMed] [Google Scholar]
- 34.Campbell KE, Lee BA. Gender differences in urban neighboring. Sociol Q. 2005;31(4):495–512. [Google Scholar]
- 35.Campbell KE, Lee BA. Sources of personal neighbor networks: social, integration, need or time? Soc Forces. 1992;70(4):1077–1110. [Google Scholar]
- 36.Li F, Harmer P, Cardinal BJ, et al. Obesity and the built environment: does the density of neighborhood fast-food outlets matter? Am J Health Promot. 2009;23(3):203–209. doi: 10.4278/ajhp.071214133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Day JC, Newburger EC. The Big Payoff: Educational Attainment and Synthetic Estimates of Work-Life Earnings. (Current Population Reports, P23-210) Washington, DC: Economics and Statistics Administration, Bureau of the Census, US Department of Commerce; 2002. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.