Abstract
We report a case of follicular B-cell lymphoma (FL) treated successfully using clarithromycin (CAM). A 44-year-old man who presented with lymphadenopathy was diagnosed with FL after a histological examination of his biopsy specimens. He was administered chemotherapy with R-CHOP (rituximab, cyclophosphamide, adriamycin, vincristine, and prednisolone) following which stable disease was achieved. However, the subsequent clinical course showed partial remission of FL and stable disease with tumor regrowth, each of which was treated with chemotherapeutic regimens. Since the patient was diagnosed with leukocytopenia, he could not undergo chemotherapy for the third regrowth; hence, he was administered CAM. His lymphadenopathy regressed and the levels of soluble interleukin 2-receptor decreased. This case shows that treatment using CAM may be effective in some cases of FL.
Keywords: B-cell lymphoma, Macrolide, Clarithromycin, Apoptosis, bcl-2
INTRODUCTION
Antibiotics are considered promising candidates for anticancer drugs because of their good tolerability and direct pro-apoptotic effects on tumor cells [1]. Macrolides, among the other antibiotics, have been thought to be potential antineoplastic and immunomodulatory agents [1]. As antineoplastic agents, macrolides show antilymphoproliferative effects through the down-regulation of the bcl-2 and bcl-xL proteins, both of which prevent apoptosis [2, 3]. Many cases of cancer, such as, mucosa-associated lymphoid tissue (MALT) lymphoma [1, 4], macroglobulinemia, multiple myeloma [5], relapse of Hodgkin's lymphoma [6], and follicular lymphoma [7] have been treated successfully using macrolides. We present a patient with stage IV follicular B-cell lymphoma (FL) who was treated successfully using clarithromycin (CAM).
CASE REPORT
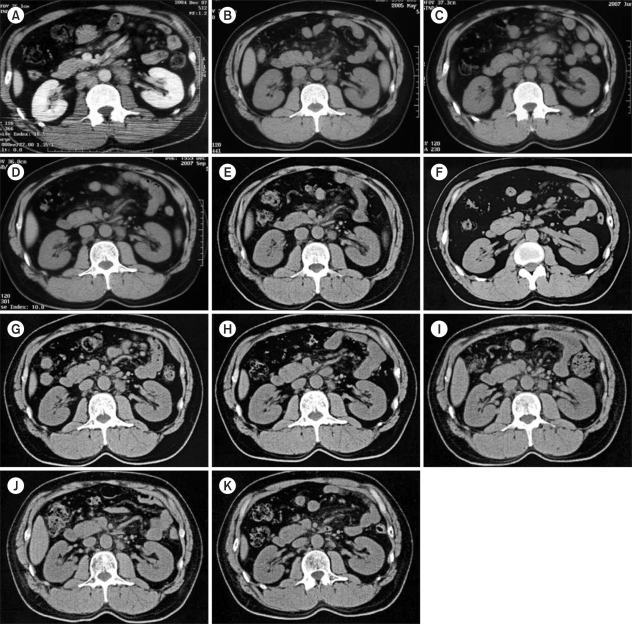
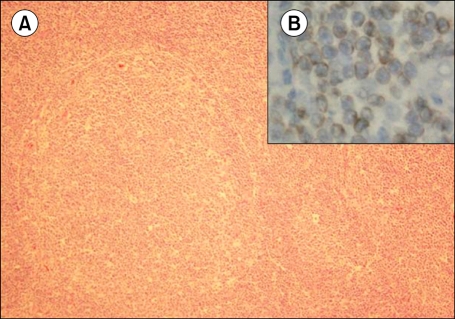
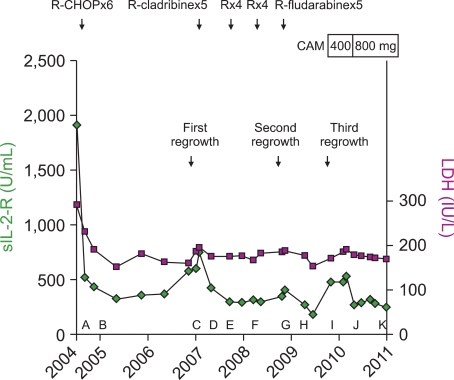
A 44-year-old man with bilateral cervical lymphadenopathy was admitted to the hospital. He had no history of fever, general fatigue, or weight loss. Physical examination showed several swollen lymph nodes in the right and left cervical, left axillary, and left inguinal regions. The patient's LDH levels and serum levels of soluble interleukin 2 receptor (sIL2-R) had increased to 293 IU/L and 1,911 U/mL, respectively. Computed tomography (CT) revealed cervical, axillary, inguinal, and para-aortic lymphadenopathy (Fig. 1A). Esophagogastroduodenoscopy (EGD) and colonoscopy (CS) showed no abnormal lesions associated with lymphoma. The biopsy specimens of the cervical lymph nodes showed well-circumscribed follicles composed of a monotonous population of predominantly small-cleaved cells that were positive for CD10 and CD20 but negative for CD5 and cyclin D1 (Fig. 2A). In the immunohistochemical study for the presence of bcl-2 protein, the small-cleaved cells stained positive (Fig. 2B). These atypical cells were detected in the bone marrow aspirates as well. Chromosome analysis of the cervical lymph node cells showed t(14;18)(q32;q21) translocation. On the basis of all these results, the patient was diagnosed with stage IV FL, and was classified as a high-risk patient since his follicular lymphoma international prognostic index (FLIPI) score was 3 points. The clinical course of the disease is shown in Fig. 3. Stable disease was achieved in the patient after 6 cycles of chemotherapy with R-CHOP (rituximab, cyclophosphamide, adriamycin, vincristine, and prednisolone), and the patient was discharged.
Fig. 1.
Computed tomography. (A) Contrast-enhanced abdominal computed tomography (CT) image showing para-aortic lymphadenopathy at the time of admission. (B) Abdominal CT image showing para-aortic lymphadenopathy after completion of 6 cycles of R-CHOP chemotherapy (rituximab, cyclophosphamide, adriamycin, vincristine, and prednisolone). (C) Abdominal CT image showing para-aortic lymphadenopathy (first regrowth). (D) Abdominal CT image showing para-aortic lymphadenopathy after completion of 5 cycles of R-cladribine therapy. (E) Abdominal CT image showing para-aortic lymphadenopathy just before the first R-monotherapy. (F) Abdominal CT image showing para-aortic lymphadenopathy 5 months after completion of 4 cycles of R-monotherapy. (G) Abdominal CT showing para-aortic lymphadenopathy (second regrowth). (H) Abdominal CT image showing para-aortic lymphadenopathy after completion of 5 cycles of R-fludarabine therapy. (I) Abdominal CT image showing para-aortic lymphadenopathy (third regrowth). (J) Abdominal CT image showing par-aortic lymphadenopathy 3 months after initiation of clarithromycin (800 mg/day) treatment. (K) Abdominal CT image showing para-aortic lymphadenopathy 9 months after initiation of clarithromycin (800 mg/day) treatment.
Fig. 2.
Histological and immunohistochemical examination of cervical lymph node biopsy specimens. (A) Histological examination showing well-circumscribed follicles consisting of a monotonous population of predominantly small-cleaved cells (Hematoxylin and eosin stain, ×100). (B) Immunohistochemical examination for bcl-2 showing positive staining in the small-cleaved cells (Immunohistochemical stain, ×400).
Fig. 3.
Clinical course. sIL2-R, soluble interleukin 2 receptor; R, rituximab; C, cyclophosphamide; H, adriamycin; O, vincristine; P, prednisolone; CAM, clarithromycin.
About 2 years later, cervical and para-aortic lymphadenopathy aggravated (Fig. 1C), and the levels of sIL2-R increased to 748 U/mL (first tumor regrowth). He was treated with 5 cycles of chemotherapy with R-cladribine followed by 4 cycles of rituximab monotherapy 2 times every 6 months. In the course of these chemotherapies, the para-aortic lymphadenopathy and sIL2-R levels improved (Fig. 1D-F). However, 5 months after these chemotherapies, the patient's condition deteriorated again, with an aggravation of the para-aortic lymphadenopathy and increase in sIL2-R levels (second tumor regrowth) (Fig. 1G). The patient was treated with 5 cycles of R-fludarabine chemotherapy, in the course of which, the para-aortic lymphadenopathy improved slightly (Fig. 1H) and sIL2-R levels decreased from 406 to 183 U/mL. About 1 year after the second regrowth, para-aortic lymphadenopathy worsened and his sIL2-R levels elevated (478 U/mL) (third tumor regrowth) (Fig. 1I). Since the patient had prolonged leukocytopenia (number of leukocytes=1,500-1,800/mm3) resulting from chemotherapy, he was administered CAM (400 mg/day), which is known to induce apoptosis in B-cell lymphoma, instead of conventional chemotherapy after obtaining informed consent. Two months after the administration of CAM, only a slight increase was observed in his IL2-R levels (478-480 U/mL). However, the levels ultimately increased to 537 U/mL, and hence, the dosage of CAM was doubled (800 mg/day). CT images obtained 3 months later showed improvement of para-aortic lymphadenopathy (Fig. 1J). The levels of sIL2-R also decreased from 537 to 268 U/mL by 6 weeks after the dosage was increased. CT images obtained 9 months after the initiation of the CAM therapy at 800 mg/day showed that the para-aortic lymphadenopathy improved further, albeit slightly (Fig. 1K), and that the sIL2-R level was constant at 200 U/mL. Mild diarrhea was noted as a side effect of the long-term use of CAM.
DISCUSSION
A newly proposed prognostic index for FL-FLIPI-classifies the prognosis of FL into 3 groups [8]. On the basis of the FLIPI score, our patient was classified as being a high-risk patient. Since the patient had no organ dysfunction, cytopenia, or bulky disease, watchful waiting could have been an option, but the patient chose to undergo chemotherapy. The risk of histological transformation is higher in patients who have advanced-stage disease and have been determined to be at high-risk on the basis of the FLIPI score at diagnosis [9]; hence, we decided to continue the treatment.
Macrolides are thought to be potential antineoplastic and immunomodulatory agents [1]. CAM, a macrolide antibiotic, is known to induce apoptosis in B-cell lymphoma cells [10]. After the third tumor regrowth, the patient was administered CAM instead of conventional chemotherapy. CAM when administered at a dosage of 400 mg/day, appeared to be slightly effective, since it arrested the rapid elevation of sIL2-R levels. However, when administered at a dosage of 800 mg/day, CAM appeared to be very effective because it rapidly decreased the levels of sIL2-R and improved the lymphadenopathy. Thus, CAM at a dose of 800 mg/day can be concluded to have antilymphoproliferative effects.
Macrolides, such as CAM and rapamycin, have antiproliferative activities against a variety of B-cell proliferative diseases [1, 2, 4-6]. Ishimatsu et al. [4] reported 2 cases of pulmonary MALT lymphoma successfully treated with low-dose, long-term CAM therapy (200 mg/day); they speculated that the macrolide induces apoptosis in lymphocytes via the down-regulation of bcl-xL protein expression. Similarly, Hayun et al. [2] reported that rapamycin and curcumin induces apoptosis in resting cells in B-cell chronic lymphocytic leukemia (B-CLL); they found that rapamycin decreases the levels of the anti-apoptotic protein bcl-2 and increases the levels of the pro-apoptotic protein Bax. These results show a clear transition from an anti-apoptotic to a pro-apoptotic signal in the tumor cells.
In our case, chromosome analysis identified t(14;18)(q32;q21) translocation-a frequent chromosomal aberration in FL, involving the immunoglobulin heavy chain (IgH) gene on chromosome 14q32 and the bcl-2 gene on chromosome 18q12. This translocation results in up-regulation of bcl-2 protein expression in most cases of FL [11]. The bcl-2 protein inhibits apoptosis, thus leading to immortality of the cells. Similarly, the bcl-xL gene, which exerts an anti-apoptotic effect on lymphocytes, is over-expressed in FL patients [12].
The lymphoma cells from our patient stained positive for bcl-2 in the immunohistochemical examination. Therefore, the mechanism by which macrolides inhibit lymphoproliferative disorders may be through their effects on bcl-2 and probably bcl-xL.
Although MALT lymphoma could be controlled with only 200 mg/day of CAM, a dose of 800 mg/day was required to control FL in our patient. This suggests that lymphoproliferative activity in FL is higher than that in MALT lymphoma.
Yaguchi et al. [7] also reported partial regression of duodenal lesions in intestinal FL after antibiotic treatment. According to their report, the patient was treated with lansoprazole (30 mg twice daily), CAM (400 mg twice daily), and amoxicillin (750 mg twice daily) for 7 days, although the tests for Helicobacter pylori were negative. EGD performed after 3 months confirmed the regression of duodenal lesions. Because antibiotic treatment induced regression, they speculated that antigenic stimuli from a source other than H. pylori might play a role in the pathogenesis of this lymphoma.
In our patient, no abnormal lesions associated with lymphoma were observed after performing EGD and CS at the time of admission. Additionally, the results of the anti-H. pylori immunoglobulin (Ig) antibody test was negative. We therefore concluded that, our patient's condition was not associated with H. pylori infection. The effectiveness of CAM treatment indicates that CAM may have antilymphoproliferative activity, and not just antibiotic activity.
More extensive research is required to substantiate our findings and determine the optimal dose, estimate the response rate, and assess the effectiveness of our CAM regimen alone or in combination with other agents.
ACKNOWLEDGEMENTS
We would like to thank Dr. Akira Suzuki from KKR Sapporo Medical Center for his interpretation of pathological results.
References
- 1.Govi S, Dognini GP, Licata G, et al. Six-month oral clarithromycin regimen is safe and active in extranodal marginal zone B-cell lymphomas: final results of a single-centre phase II trial. Br J Haematol. 2010;150:226–229. doi: 10.1111/j.1365-2141.2010.08179.x. [DOI] [PubMed] [Google Scholar]
- 2.Hayun R, Okun E, Berrebi A, et al. Rapamycin and curcumin induce apoptosis in primary resting B chronic lymphocytic leukemia cells. Leuk Lymphoma. 2009;50:625–632. doi: 10.1080/10428190902789181. [DOI] [PubMed] [Google Scholar]
- 3.Mizunoe S, Kadota J, Tokimatsu I, Kishi K, Nagai H, Nasu M. Clarithromycin and azithromycin induce apoptosis of activated lymphocytes via down-regulation of Bcl-xL. Int Immunopharmacol. 2004;4:1201–1207. doi: 10.1016/j.intimp.2004.05.011. [DOI] [PubMed] [Google Scholar]
- 4.Ishimatsu Y, Mukae H, Matsumoto K, et al. Two cases with pulmonary mucosa-associated lymphoid tissue lymphoma successfully treated with clarithromycin. Chest. 2010;138:730–733. doi: 10.1378/chest.09-2358. [DOI] [PubMed] [Google Scholar]
- 5.Niesvizky R, Jayabalan DS, Christos PJ, et al. BiRD (Biaxin [clarithromycin]/Revlimid [lenalidomide]/dexamethasone) combination therapy results in high complete- and overall-response rates in treatment-naive symptomatic multiple myeloma. Blood. 2008;111:1101–1109. doi: 10.1182/blood-2007-05-090258. [DOI] [PubMed] [Google Scholar]
- 6.Sauter C, Blum S. Regression of lung lesions in Hodgkin's disease by antibiotics: case report and hypothesis on the etiology of Hodgkin's disease. Am J Clin Oncol. 2003;26:92–94. doi: 10.1097/00000421-200302000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Yaguchi T, Imaeda H, Kizaki M, et al. Partial regression of duodenal lesions of intestinal follicular lymphoma after antibiotic treatment. Dig Endosc. 2010;22:316–318. doi: 10.1111/j.1443-1661.2010.01011.x. [DOI] [PubMed] [Google Scholar]
- 8.Solal-Céligny P, Roy P, Colombat P, et al. Follicular lymphoma international prognostic index. Blood. 2004;104:1258–1265. doi: 10.1182/blood-2003-12-4434. [DOI] [PubMed] [Google Scholar]
- 9.Montoto S, Davies AJ, Matthews J, et al. Risk and clinical implications of transformation of follicular lymphoma to diffuse large B-cell lymphoma. J Clin Oncol. 2007;25:2426–2433. doi: 10.1200/JCO.2006.09.3260. [DOI] [PubMed] [Google Scholar]
- 10.Ohara T, Morishita T, Suzuki H, Masaoka T, Ishii H, Hibi T. Antibiotics directly induce apoptosis in B cell lymphoma cells derived from BALB/c mice. Anticancer Res. 2004;24:3723–3730. [PubMed] [Google Scholar]
- 11.Bosga-Bouwer AG, van Imhoff GW, Boonstra R, et al. Follicular lymphoma grade 3B includes 3 cytogenetically defined subgroups with primary t(14;18), 3q27, or other translocations: t(14;18) and 3q27 are mutually exclusive. Blood. 2003;101:1149–1154. doi: 10.1182/blood.V101.3.1149. [DOI] [PubMed] [Google Scholar]
- 12.Zhao WL, Daneshpouy ME, Mounier N, et al. Prognostic significance of bcl-xL gene expression and apoptotic cell counts in follicular lymphoma. Blood. 2004;103:695–697. doi: 10.1182/blood-2003-06-1901. [DOI] [PubMed] [Google Scholar]