Abstract
In this study, we review outcomes for 15 patients with self-inflicted submental gunshot wounds requiring free flap reconstruction. Patients presented to two tertiary care centers over a 7-year period. Mean age was 46 years (range, 16 to 76 years), 67% (n = 10) had a psychiatric history, and four were known to abuse illicit substances. Patients with oromandibular involvement required on average a total of 2.8 procedures, and those with midface (3.7) or combined defects (6) required more total procedures (p = 0.21). Donor sites included osteocutaneous radial forearm (n = 8), fibula (n = 4), fasciocutaneous radial forearm (n = 5), and anterior lateral thigh (n = 1). Median length of hospitalization was 8 days. Overall complication rate was 33% (n = 5), and included hematoma (n = 1), fistula (n = 1), and mandibular malunion (n = 2). Most patients were able to tolerate a regular or soft diet (92%), maintain oral competency (58%), and demonstrate intelligible speech (92%) at a median time to follow-up of 12 months. Despite the devastating nature of this injury, free flap reconstruction of self-inflicted submental gunshot wounds results in acceptable functional results for the majority of patients.
Keywords: Gunshot wounds, free tissue transfer, reconstruction, definitive management, self-inflicted
High energy, self-inflicted submental gunshot wounds result in considerable bone and soft tissue loss, requiring reconstruction of large portions of the upper and lower lip, anterior tongue, and mandible. Tissue necrosis, infection, and hematoma formation have traditionally complicated attempts at primary repair, resulting in the need for serial debridement and delayed bony reconstruction.1,2 Because of the extensive nature of these injuries, free tissue transfer has become the standard for definitive repair, incorporating vascularized bone and soft tissue into the wound following injury to minimize scar contracture and optimize postoperative function and cosmesis.3,4 In the present study, we assess long-term outcomes associated with free flap reconstruction of patients with self-inflicted, submental gunshot wounds and review the goals of definitive management.
METHODS
A total of 15 patients with self-inflicted complex craniofacial gunshot wounds requiring free tissue transfer presented to the Otolaryngology–Head and Neck Surgery Department at the University of Alabama at Birmingham or Oregon Health and Science University from September 2002 through June 2009. Following Institutional Review Board approval, a retrospective study of these patients was conducted.
In all cases, initial management of gunshot wounds to the face began with trauma management per advanced trauma life support protocols.5 A secure airway was established by either intubation or tracheotomy, direct pressure was applied to minimize blood loss, and a secondary survey was performed to evaluate for additional injuries. Once stabilized, radiographic evaluation was helpful in identifying fracture patterns, the presence of major vascular injury, soft tissue loss, and clearance of the cervical spine prior to surgery. An initial operation involved removal of foreign debris and devitalized tissue, closure of intracranial defects, and an attempt to salvage the globe if injured.6 Underlying fractures were stabilized via mandibulomaxillary fixation (n = 2) when required, and soft tissue closure was obtained. Where necessary, the mandible was plated with a reconstruction bar to maintain the soft tissue envelope (n = 5). All other patients were reduced anatomically without mandibulomaxillary fixation.
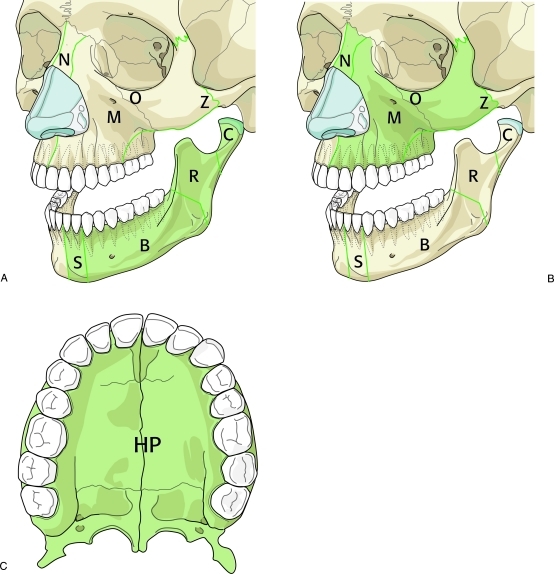
Definitive reconstruction was performed in close proximity to the initial injury, or as soon as possible after stabilization of the patient was maintained. Fractures were exposed and rigid internal fixation employed. Two of the senior authors (E.L.R. or M.K.W.) performed all free tissue transfers and bony or soft tissue reconstruction. Extent and size of the defect necessitated the type of free flap required. Defects were categorized into oromandibular, midface, or combined mandible/maxillary defects (Fig. 1). Following free flap reconstruction, patients were routinely admitted to the step-down unit for 24 hours before being transferred to the floor. Flaps were assessed for color and temperature change over the course of the first 48 hours and monitored continuously by internal Doppler until patient discharge.
Figure 1.
Oromandibular and midface bony defect classification. (A) Oromandibular defects: C, condyle; R, ramus; B, body; S, symphysis. (B) Midface defects: N, nasal bones; M, maxilla; O, orbital rim; Z, zygoma; HP, hard plate.
Demographic and clinical data recorded consisted of patient age, gender, risk factors, method of injury, and anatomic subsites involved. Classification of bony and soft tissue oromandibular defects were based on the Urken7 classification system. Soft tissue defects were categorized into mucosa, tongue, and cutaneous defects. Mucosal defects included labial, buccal, soft palate, or floor of mouth defects. External cutaneous defects were divided into cheek, neck, mentum, and upper and lower lips.7
The number of surgeries and type of free flap(s) required for reconstruction, length of hospitalization, complications, and functional outcomes including speech and swallowing were noted. Adequate speech was defined as the ability of the patient to be intelligible over the telephone. Swallowing was indirectly assessed by postoperative diet, defined as regular, soft, liquid or gastrostomy tube (PEG)-dependent.
Descriptive variables are reported as means (±standard deviation) and categorical variables as percentages. Descriptive statistics were compared by general linear models for normally distributed variables or the Kruskal-Wallis test for otherwise. A p value of <0.05 was considered statistically significant. Data analysis was done using JMP Version 8.0 software (SAS Institute, Inc., Cary, NC).
RESULTS
Patients
From 2002 to 2009, 15 patients were evaluated for significant mandibular and midface defects as a result of self-inflicted gunshot wounds. Demographic and weapon-related injury data are presented in Table 1. The majority of patients were between the ages of 40 and 50, were male (66.7%), and had a history of depression or other psychiatric illness (66.7%). Four patients had a history of drug abuse. Nearly half of all patients were smokers (n = 7) and uninsured (n = 7). Follow-up ranged from 5 months to 4 years, for a median of 12 months.
Table 1.
Demographics and Mechanism of Injury
| n | % | |
|---|---|---|
| Age (y) | ||
| Mean | 46 | |
| Range | 16–76 | |
| Gender | ||
| Male | 10 | 66.7 |
| Female | 5 | 33.3 |
| Trauma-related weapon | ||
| Rifle | 5 | 33.3 |
| Shotgun | 9 | 60.0 |
| Handgun | 1 | 6.7 |
Reconstruction
A total of 18 free tissue transfers were required for reconstruction of oromandibular (n = 8), midface (n = 3), or combined (n = 4) defects. Most patients required both soft tissue and bony repair (n = 11/15; Fig. 2). Table 2 lists the various types of flaps utilized. The osteocutaneous radial forearm free flap (OCRFFF) was the flap of choice for mandibular or midface bony reconstruction (n = 8/12; Fig. 3). All radius defects were plated prophylactically. Two patients required double flap procedures. One patient required a fibula and osteocutaneous radial forearm free flap for reconstruction of the mandible and midface, respectively (Fig. 4). The other patient underwent fibula free flap reconstruction of the mandible and overlying chin complex followed by fasciocutaneous radial forearm flap (RFFF) lip reconstruction (Fig. 5). The RFFF was most commonly utilized for soft tissue coverage (n = 5/6) with the anterolateral thigh flap used as an alternative in one patient to increase bulk for a large midface defect. Midface defects included zygoma, maxilla, hard palate, inferior orbital rim, and involvement of the nasal bones (Table 3).
Figure 2.
Combined anterior mandible and overlying soft tissue destruction (A, B). The patient underwent rigid internal fixation of a Le Fort level II fracture and osteocutaneous radial forearm free flap reconstruction of the mandible (C, D). Patient 3 months postoperatively (E).
Table 2.
Free Flaps Required for Reconstruction
| Bone-containing free flaps | |
| OCRFFF | 8 |
| Fibula | 4 |
| Soft tissue free flaps | |
| RFFF | 5 |
| ALT | 1 |
Figure 3.
Computed tomography scan with 3-D bone reconstruction demonstrating anterior mandibular avulsion with bony destruction and involvement of the anterior maxillary complex and orbit (A). The patient underwent primary repair with placement of a mandibular reconstruction bar (B) and soft tissue closure (C) prior to definitive mandibular reconstruction (D) with radial forearm free tissue transfer (E).
Figure 4.
Status post-gunshot wound involving the anterior mandible, maxilla, and nasal bones requiring both osteocutaneous radial forearm and fibular free flap reconstruction (A). The patient developed cutaneous loss of her fibula flap requiring radial forearm free tissue transfer for soft tissue loss (B). A paramedian forehead flap was utilized for nasal reconstruction (C). Patient 1 year postoperatively (D).
Figure 5.
Extensive anterior mandible, maxillary, and soft tissue destruction following a self-inflicted gunshot wound (A, B). Patient status post–open reduction and internal fixation of naso-orbital-ethmoidal and zygomaticomaxillary complex fractures with fibula free flap reconstruction of the mandible and fasciocutaneous radial forearm lower and upper lip reconstruction (C,D).
Table 3.
Classification of Oromandibular and Midface Defects
| Patient | Weapon | Subsite | Defect | Flap | |||||
|---|---|---|---|---|---|---|---|---|---|
| Bone | Soft Tissue | ||||||||
| 1 | Handgun | Midface | Z | CCH | OCRFFF | ||||
| 2 | Shotgun | Midface | M, OIR | — | OCRFFF | ||||
| 3 | Shotgun | Oromandibular | — | — | RFFF | ||||
| 4 | Shotgun | Oromandibular | BSB | — | OCRFFF | ||||
| 5 | Shotgun | Oromandibular | BSH | CCH, TM | Fibula | ||||
| 6 | Shotgun | Oromandibular | SH | CCH | RFFF | ||||
| 7 | Rifle | Combined | SB, M | OCRFFF | |||||
| 8 | Rifle | Combined | BSB, M, HP, N | FOM, CUL | Fibula, OCRFFF | ||||
| 9 | Rifle | Oromandibular | BSB | FOM | Fibula | ||||
| 10 | Rifle | Oromandibular | — | FOM, TM, CCH | RFFF | ||||
| 11 | Rifle | Midface | HP | CCH, CUL | ALT | ||||
| 12 | Shotgun | Oromandibular | BSH | CM | OCRFFF | ||||
| 13 | Shotgun | Combined | BSH, M, HP, OIR | FOM | OCRFFF | ||||
| 14 | Shotgun | Oromandibular | S | CM, CLL | OCRFFF | ||||
| 15 | Shotgun | Combined | BSB, M, HP | CM, CUL, CLL | Fibula, RFFF | ||||
Z, zygoma; M, maxilla; OIR, inferior orbital rim; HP, hard palate; N, nasal bones; S, symphysis; B, body; SH, hemisymphysis; CCH, cheek; FOM, floor of mouth; CUL, upper lip; TM, tongue; CM, mentum; OCRFF, osteocutaneous radial forearm free flap; RFFF, radial forearm free flap; ALT, anterolateral thigh.
Patients with isolated oromandibular involvement required fewer total procedures on average (2.8 ± 1.33) when compared with patients with midface (3.7 ± 1.53) or combined defects (6 ± 4.24; p = 0.21). Median time from initial injury to time of definitive reconstruction was 2 months (range 0.5 to 29 months). One patient had undergone primary closure with obturator placement for her hard palate defect; she presented to the head and neck service over a year after her injury (29 months) for definitive reconstruction. Time from reconstruction to a second procedure was 3.3 months on average (range 0.5 to 10 months). Additional procedures included scar revision, flap debulking, removal of infected hardware, and fistula closure. One patient with a combined mandible/maxillary defect required extensive nasal reconstruction necessitating a total of nine operations including a paramedian forehead flap for the nasal tip and Karapandzic flap for lip reconstruction.
Postoperative Outcomes
Following free flap reconstruction, average hospital stay was 8 days (range 5 to 17 days). Patients with high-energy (use of a rifle) self-inflicted gunshot wounds required on average more procedures (5.8 ± 2.22, p = 0.08) and a longer hospital stay (14.3 days ± 5.51) when compared with shotgun or handgun injuries, although this was not statistically significant (p = 0.23; Table 4). The overall complication rate was 33.3% and included postoperative hematoma (n = 1), fistula formation and infection (n = 1), and mandibular malunion (n = 2). There were no flap failures; however, one partial flap failure occurred (n = 1) with partial cutaneous loss, necessitating fasciocutaneous radial forearm free tissue transfer. Another patient developed an arterial clot at the anastomotic site and underwent successful revision.
Table 4.
Number of Procedures and Length of Hospital Stay by Mechanism of Injury
| Rifle | Shotgun | Handgun | p Value | |
|---|---|---|---|---|
| Mean No. of procedures | 5.8 | 2.0 | 4.0 | 0.08 |
| Length of hospital stay (d) | 14.3 | 7.9 | 4.9 | 0.23 |
Acceptable functional results were obtained in the majority of patients. Most required PEG tube placement (n = 10/15, 66.7%); 40% retained PEG tubes for a median of 24 weeks (range, 17 to 104 weeks). Return to oral intake was 14 weeks on average. All but one patient resumed a regular or soft diet (91.7%), nearly 60% were able to maintain oral competency, and all but one demonstrated intelligible speech over the telephone (91.7%). One patient remained PEG-dependent due to persistent aspiration (8.3%). Two patients received dental implants, and one patient was being evaluated for dental reconstruction. A total of 12 patients required tracheotomies and 3 (25.0%) remained tracheostomy tube-dependent at median follow-up of 12 months.
DISCUSSION
Self-inflicted submental gunshot wounds present a significant challenge for the facial reconstructive surgeon. Although initial care for these patients still centers on the basics of trauma management and resuscitation, there has been a shift from delayed bony repair and serial debridement to early definitive management.2,3,8,9,10 Median time from initial injury to definitive reconstruction was 2 months for this patient population. Most presented with extensive oromandibular or midface defects, necessitating simultaneous bony and soft tissue free flap reconstruction.6
The type and extent of injury dictated the type of free tissue transfer required in the majority of cases. The Urken7 classification system was utilized to categorize oromandibular defects and predict functional outcomes. We defined both bony and soft tissue midface defects in a similar fashion to that proposed by Urken et al.7 Mandibular and maxillary defects were primarily managed with osteocutaneous radial forearm free flaps, which have become more popular than fibula or iliac crest flaps for bony reconstruction. Improved aesthetic and functional outcomes have been demonstrated with use of the radial forearm free flap in maxillary11,12 and mandibular13 reconstruction, although its use in mandibular reconstruction has been met with controversy. Limitations to its use include thinness of the bony stock and donor site morbidity (fracture of the radius).12,14 With prophylactic plating of the radius and modification of osteotomies, radius fractures have nearly been eliminated.13,15,16
The osteocutaneous radial forearm free flap has been used to bridge anterior oromandibular defects following tumor resection.13,17 This is the first large study to evaluate use of the OCRFFF in trauma patients. The thin pliable nature of the flap makes it ideal for limited anterior mandibular defects or when reconstruction is required for combined mandible and overlying soft tissue lower lip defects (Fig. 5). The fibular free flap has also been utilized for bony and soft tissue oromandibular reconstruction. In contrast to the radial forearm free flap, the fibula has a higher incidence of partial flap failure as was demonstrated by one patient in our series who developed cutaneous loss and required additional soft tissue coverage.18
The thin, pliable nature of the radial forearm flap has made it the preferred choice for reconstruction of intraoral defects.19 The majority of patients in this series underwent radial forearm free flap reconstruction for soft tissue defects. One patient required additional bulk for a large midface defect and underwent anterolateral thigh free tissue transfer. The flap provides a generous skin paddle with underlying vascularized fat, maintaining long-term flap volume and acceptable results in midface reconstruction.20
Wound-healing complications approach 39% for gunshot wounds that traverse the oral cavity,9 and an infection rate of 100% has been reported for close-range shotgun injuries.21 Complications including postoperative hematoma, infection, and fistula formation occurred in 33% of patients in our series. One patient developed partial flap loss requiring additional soft tissue coverage. Mandibular malunion occurred in two patients who underwent subsequent plating for reinforcement.
On average, patients who presented with midface or combined defects required more surgical procedures. Although adequate function can be obtained at the time of initial reconstruction, additional procedures are often required to optimize function and aesthetics. In a study by Futran et al,6 patients with midface defects that involved the orbit or nasal components also required more subsequent operations. One patient from our series with a combined mandible/maxillary defect and nasal involvement required a total of nine procedures to obtain an aesthetically pleasing nasal structure. Upper- and lower-lip reconstruction can also be a challenge to achieve oral competence and acceptable aesthetic results.
All but one patient resumed a regular or soft diet, and nearly half were able to maintain oral competency at a median follow-up of 12 months. One patient with a defect involving the mandible and lateral tongue remained PEG-dependent with tethering at the site of injury and poor tongue movement following corrective procedures. All but one patient demonstrated intelligible speech over the telephone, and three remained tracheostomy tube-dependent. These results are consistent with those obtained in a similar multi-institutional study where all but one patient was able to resume a soft diet and demonstrate intelligible speech.6 In the present study, we evaluated outcomes in patients with the most complex and common injury: submental self-inflicted gunshot wounds. Although this review represents a small series of patients, it further defines the use of free flap reconstruction in severe ballistic facial trauma and provides long-term outcomes for this unique subset of patients.
CONCLUSION
Early and definitive free flap reconstruction has become the standard of care for complex craniofacial gunshot wounds with improved aesthetic and functional results obtained in the majority of patients. In the present study, we demonstrate acceptable outcomes for patients with extensive midface, oromandibular, or combined bony and soft tissue defects following free tissue transfer.
References
- Thorne C H. Gunshot wounds to the face. Current concepts. Clin Plast Surg. 1992;19:233–244. [PubMed] [Google Scholar]
- Clark N, Birely B, Manson P N, et al. High-energy ballistic and avulsive facial injuries: classification, patterns, and an algorithm for primary reconstruction. Plast Reconstr Surg. 1996;98:583–601. doi: 10.1097/00006534-199609001-00001. [DOI] [PubMed] [Google Scholar]
- Gruss J S, Antonyshyn O, Phillips J H. Early definitive bone and soft-tissue reconstruction of major gunshot wounds of the face. Plast Reconstr Surg. 1991;87:436–450. doi: 10.1097/00006534-199103000-00008. [DOI] [PubMed] [Google Scholar]
- Vitkus K, Vitkus M. Microsurgical reconstruction of shotgun-blast wounds to the face. J Reconstr Microsurg. 1990;6:279–286. doi: 10.1055/s-2007-1006831. [DOI] [PubMed] [Google Scholar]
- Demetriades D, Chahwan S, Gomez H, Falabella A, Velmahos G, Yamashita D. Initial evaluation and management of gunshot wounds to the face. J Trauma. 1998;45:39–41. doi: 10.1097/00005373-199807000-00007. [DOI] [PubMed] [Google Scholar]
- Futran N D, Farwell D G, Smith R B, Johnson P E, Funk G F. Definitive management of severe facial trauma utilizing free tissue transfer. Otolaryngol Head Neck Surg. 2005;132:75–85. doi: 10.1016/j.otohns.2004.08.013. [DOI] [PubMed] [Google Scholar]
- Urken M L, Weinberg H, Vickery C, Buchbinder D, Lawson W, Biller H F. Oromandibular reconstruction using microvascular composite free flaps. Report of 71 cases and a new classification scheme for bony, soft-tissue, and neurologic defects. Arch Otolaryngol Head Neck Surg. 1991;117:733–744. doi: 10.1001/archotol.1991.01870190045010. [DOI] [PubMed] [Google Scholar]
- Chen A Y, Stewart M G, Raup G. Penetrating injuries of the face. Otolaryngol Head Neck Surg. 1996;115:464–470. doi: 10.1177/019459989611500519. [DOI] [PubMed] [Google Scholar]
- Kihtir T, Ivatury R R, Simon R J, Nassoura Z, Leban S. Early management of civilian gunshot wounds to the face. J Trauma. 1993;35:569–575. discussion 575–577. doi: 10.1097/00005373-199310000-00012. [DOI] [PubMed] [Google Scholar]
- Greenberg A M. Management of facial fractures. N Y State Dent J. 1998;64:42–47. [PubMed] [Google Scholar]
- Santamaria E, Cordeiro P G. Reconstruction of maxillectomy and midfacial defects with free tissue transfer. J Surg Oncol. 2006;94:522–531. doi: 10.1002/jso.20490. [DOI] [PubMed] [Google Scholar]
- Bardsley A F, Soutar D S, Elliot D, Batchelor A G. Reducing morbidity in the radial forearm flap donor site. Plast Reconstr Surg. 1990;86:287–292. discussion 293–294. [PubMed] [Google Scholar]
- Villaret D B, Futran N A. The indications and outcomes in the use of osteocutaneous radial forearm free flap. Head Neck. 2003;25:475–481. doi: 10.1002/hed.10212. [DOI] [PubMed] [Google Scholar]
- Vaughan E D. The radial forearm free flap in orofacial reconstruction. Personal experience in 120 consecutive cases. J Craniomaxillofac Surg. 1990;18:2–7. doi: 10.1016/s1010-5182(05)80596-7. [DOI] [PubMed] [Google Scholar]
- Thoma A, Khadaroo R, Grigenas O, et al. Oromandibular reconstruction with the radial-forearm osteocutaneous flap: experience with 60 consecutive cases. Plast Reconstr Surg. 1999;104:368–378. discussion 379–380. doi: 10.1097/00006534-199908000-00007. [DOI] [PubMed] [Google Scholar]
- Edmonds J L, Bowers K W, Toby E B, Jayaraman G, Girod D A. Torsional strength of the radius after osteofasciocutaneous free flap harvest with and without primary bone plating. Otolaryngol Head Neck Surg. 2000;123:400–408. doi: 10.1067/mhn.2000.109474. [DOI] [PubMed] [Google Scholar]
- Kim J H, Rosenthal E L, Ellis T, Wax M K. Radial forearm osteocutaneous free flap in maxillofacial and oromandibular reconstructions. Laryngoscope. 2005;115:1697–1701. doi: 10.1097/01.mlg.0000174952.98927.9f. [DOI] [PubMed] [Google Scholar]
- Hildago D A, Shenaq S M, Larson D L. Mandibular reconstruction in the pediatric patient. Head Neck. 1996;18:359–365. doi: 10.1002/1097-0347(199607/08)18:4<359::aid-hed2880180402>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Eckardt A, Meyer A, Laas U, Hausamen J E. Reconstruction of defects in the head and neck with free flaps: 20 years experience. Br J Oral Maxillofac Surg. 2007;45:11–15. doi: 10.1016/j.bjoms.2005.12.012. [DOI] [PubMed] [Google Scholar]
- Amin A, Rifaat M, Civantos F, Weed D, Abu-Sedira M, Bassiouny M. Free anterolateral thigh flap for reconstruction of major craniofacial defects. J Reconstr Microsurg. 2006;22:97–104. doi: 10.1055/s-2006-932503. [DOI] [PubMed] [Google Scholar]
- Suominen E, Tukiainen E. Close-range shotgun and rifle injuries to the face. Clin Plast Surg. 2001;28:323–337. [PubMed] [Google Scholar]