Abstract
Atrophic edentulous mandible fractures in geriatric patients have low incidence but present several biological and biomechanical peculiarities that produce a nonunion rate of around 20%. Surgical extraoral approaches for internal fixation of these fractures can be transcervical or by one or two submandibular incisions. Two patients sustaining multiple fractures in atrophic edentulous mandible are presented: the first patient was 72-years-old, treated by two submandibular incisions, and the second was 81-years-old, treated by transcervical approach. We discuss the advantages and drawbacks of each approach and their indications according to the Luhr et al (1996) atrophy index.
Keywords: Atrophic mandible, mandibular fracture, rigid internal fixation
Atrophic edentulous mandible fractures represent a subset of facial injuries that are sustained by older victims1,2,3,4,5,6 in whom perioperative management is different from that of younger patients and is often described as more complex.2,3,4 Their frequency is low and considered to be less than 1% of all facial fractures.7
Several techniques are described in the literature for atrophic mandible fractures fixation: miniplates,8,9 titanium mesh,6,10 and rigid plates.1,3,6,7,11 The surgical choices for approaches normally consider intraoral and extraoral approaches. Some authors support the intraoral approach,1,6,12 some extraoral,13 and others found no differences between them.10
The aim of this article is to report two cases and to compare the differences between the submandibular and transcervical approaches in geriatric patients with multiple fractured atrophic mandibles.
CASE REPORTS
Case 1
A 72-year-old man was referred to the University Hospital in June 2004 as a fall victim. After extraoral exam, mandibular X-rays showed two fractures at the left mandibular body, one in the left subcondylar region with minimal displacement and one at the right mandibular body (Figs. 1 and 2). The patient presented mouth-opening limitation, and besides the painful symptomatology during palpation, the patient reported dysphagia and paresthesia of the mental nerve bilaterally and stated that he did not wear dental prosthesis.
Figure 1.
Preoperative posteroanterior mandibular radiograph.
Figure 2.
Preoperative lateral oblique mandibular radiograph.
The patient was an insulin-dependent diabetic with medically controlled hypertension. The laboratory tests were normal except for hyperglycemia, which was far above normal. The patient remained in the hospital for 12 days, until his condition was controlled. Meanwhile, the patient was examined by a cardiologist and an anesthesiologist to determine his surgical risk and American Society of Anesthesiologists (ASA) classification; he was rated as ASA III with a surgical risk of 2.
The patient was anesthetized with nasotracheal general anesthesia. Because he didn't wear dental prostheses in the preoperative period, anatomic reduction of the fractured segments was the treatment of choice. Because the left subcondylar fracture had minimal displacement and did not cause significant mouth-opening limitation, it was not surgically treated. Two independent submandibular approaches were made.14 The fractures were reduced and stabilized with noncompression 2.4-mm reconstruction plates with bicortical screws (Figs. 3 and 4). Plane sutures were performed and compressive dressings applied. No drains were used.
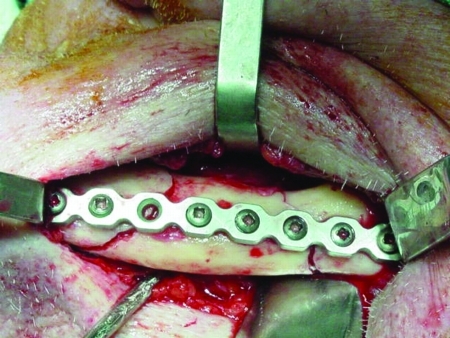
Figure 3.
Left side reduced and fixed by a 2.4-mm reconstruction plate.
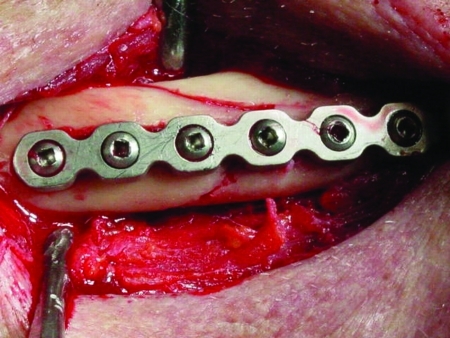
Figure 4.
Right side reduced and fixed by a 2.4-mm reconstruction plate.
The patient recovered well in the postoperative period, which included use of diabetic and antihypertensive medications besides the usual postoperative medication. The immediate postoperative radiograph showed proper positioning of the segments (Fig. 5), and the 2-month panoramic radiography demonstrated that reduction was maintained (Fig. 6). The subcondylar fracture was treated with physiotherapy in the postoperative period.15 The patient has 46 months of follow-up, with ~34 mm of mouth opening without functional limitation. The osseous height at the site of the fracture was determined by reassessment,6,9,12 presenting 14 mm at its lowest point and rated as class II according to Luhr et al12 classification.
Figure 5.
Segments properly positioned in the postoperative posteroanterior mandibular radiograph.
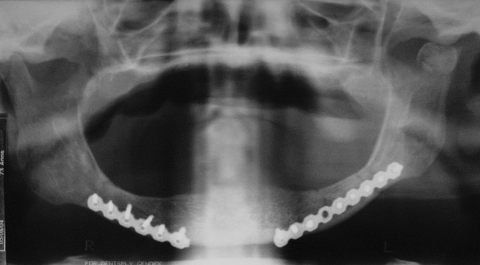
Figure 6.
Two months panoramic X-ray.
Case 2
An 81-year-old woman was referred to the University Hospital after a fall. An oral exam and mandibular X-rays (Figs. 7 and 8) revealed two fractures of the mandibular bodies, one on each side. The patient presented mouth-opening limitation and bilateral lower-lip paresthesia. According to Luhr et al12 classification, the patient presented a class III atrophic mandible and its height at the lowest point was 5 mm.
Figure 7.
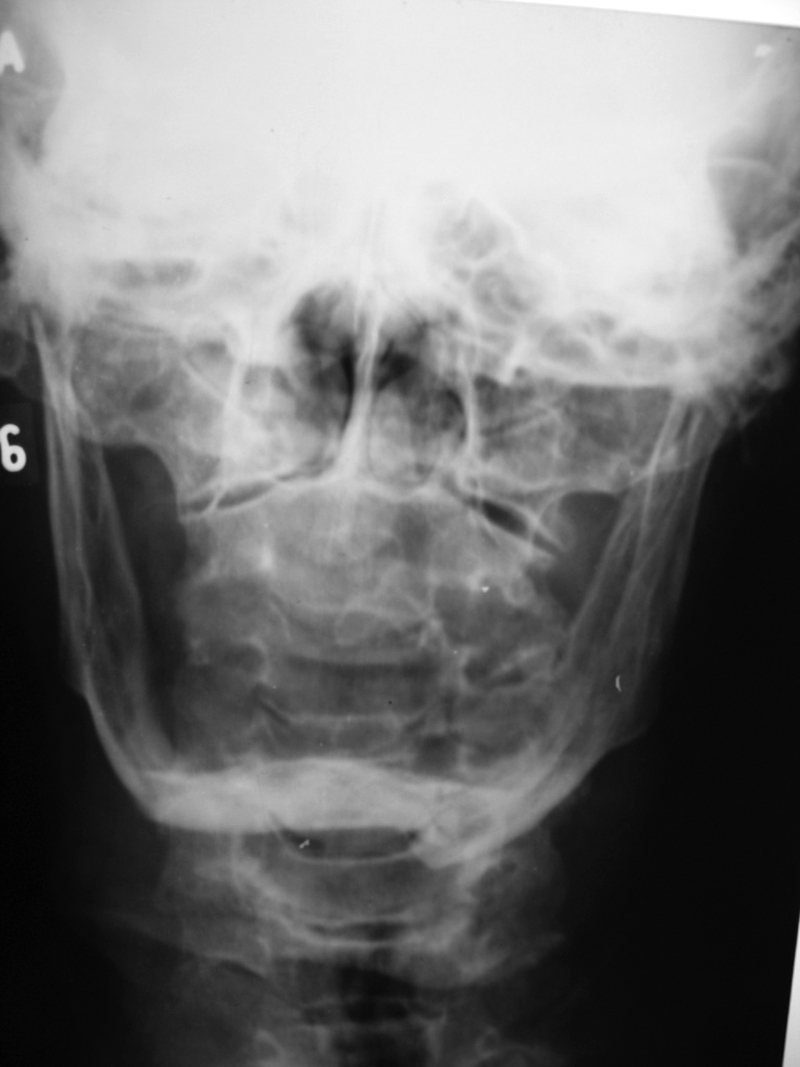
Preoperative posteroanter mandibular radiograph.
Figure 8.

Preoperative lateral oblique mandibular radiograph.
Medical evaluation found no significant systemic illness, and the anesthesiologist labeled the patient as ASA class II. The patient was anesthetized with nasotracheal general anesthesia. A transcervical approach was performed to expose the fractured segments (Fig. 9). Simplification of the fractures was made with temporary stabilization (Fig. 10), with application of simple hardware allowing correct adaptation of a single 2.4-mm reconstruction plate fixed by bicortical screws (Fig. 11). After removal of the hardware used for simplification, layered suture closure was performed and compressive dressing applied. No drains were used.
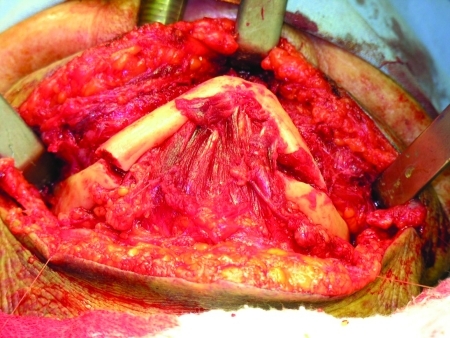
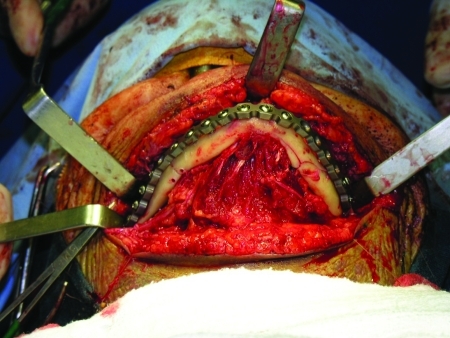
Figure 9.
Surgical exposure of the body fractures.
Figure 10.
Fractures simplification.
Figure 11.
Fractures reduced and fixed by a single 2.4-mm reconstruction plate.
The patient recovered well in the postoperative period, using regular postsurgical medication. The immediate postoperative radiograph showed proper segment alignment (Fig. 12). In the follow-up, the patient had no complaints, except of the impossibility to extend her neck (owing to the cervical scar contraction) and the bilateral lower-lip paresthesia. After proper physiotherapy, the patient was able to restore her normal neck function, but the lower-lip paresthesia was still noticeable 29 months after the operation.
Figure 12.
Postoperative posteroanterior mandibular radiograph.
DISCUSSION
Various factors may contribute to the weakening of the mandible in this age group,2 including biological and biomechanical factors.7 Biologically, there is a reduced vascularity or decreased blood flow in the elderly.2,7,16 Also, loss of the teeth, which in many older patients occurs at an early age, leads to subsequent loss of bone mass.2,3,9,17 Bradley16 hypothesized that the subperiosteal plexus is probably the major supply to the mandible, and the elevation of the periosteum during the surgery may seriously impair the vascular supply to the bone, resulting in nonunion of fractures treated by open reduction and direct osseous fixation. Concerning the systemic biological problems related to this patient population, systemic diseases associated with advancing age, osteoporosis, and change in bone quality should be included.7,16
Biomechanical considerations include the loss of the buttressing effects associated with diminished bone height of the atrophic edentulous mandible, as well as the stability associated with the specific form of fixation.5,7,12,18 Because of the unfavorable conditions produced by the reduced cross-sectional and smaller contact areas of the fractured ends, as well as the usually dense and sclerotic bone that is poorly vascularized, prolonged fracture healing can be expected.4,6,8,9,12,16,18,19
Older patients with these types of fractures will generally have significant health problems that may not support general anesthesia or a long procedure.2,3,20 Advanced age (i.e., older than 85 years) is considered a risk factor for patients with severe multiorgan dysfunction.21 However, chronologic age should not be considered a contraindication to skillfully administered anesthetic and invasive surgery.2,22
The relative amount of displacement of the fractured segments is obviously a determining factor to conservative or surgical treatment.2 Invasive surgical treatment management of the atrophic mandible body fracture should be considered when closed techniques have a high likelihood of malunion/nonunion or resulting in continued oral functional impairment for the patient.5 The current literature suggests that more invasively treated fractures have a greater likelihood of complications and increased general morbidity. Unfortunately, it is impossible to ascertain how patients who were treated more invasively would have done if left untreated to a dysfunctional endpoint.5
Though immediate treatment is not necessary in isolated edentulous mandibular fractures,5 delaying the management of an edentulous mandible fracture for several weeks may be a very prudent alternative for compromised patients. Identifying comorbid conditions and optimizing the trauma victim's cardiorespiratory and general systemic health are critical initiatives to reduce morbidity and mortality in the high-risk patient.5 In agreement with the literature, it was necessary to postpone the surgical intervention for 12 days in the first case, until the patient was stable and could be operated.
The term edentulous made comparing the results of different treatment modalities difficult.9 Luhr et al12 defined that a mandible with a height at the fracture site of 20 mm or less is atrophic and proposed a comprehensive classification (Table 1).
Table 1.
Atrophic Mandible Classification
| Class | Height (mm) |
|---|---|
| I. Moderate atrophy | 16–20 |
| II. Significant atrophy | 11–15 |
| III. Extreme atrophy | < 10 |
Adapted from Luhr et al.12
The transcervical incision provides maximum exposure of the mandible with one incision instead of multiple extraoral and intraoral incisions for bilateral mandibular procedures.13 The transcervical access provides complete and uninterrupted visualization of the mandible as a whole. Plating and grafting can be accomplished without any exposure limitations; recipient vessels are easily exposed for microsurgical anastomosis; injury to the facial nerve is less likely compared with the limited isolated extraoral approaches; and the mental nerve is not jeopardized. Postoperatively, wound healing is good due to the robust blood supply to the skin and platysma.13 The skin incision between hyoid bone and thyroid cartilage falls in the upper neck crease, well away from a tracheotomy site, and typically heals without any venous congestion. Cosmetically, the scar is acceptable, especially when the incision is hidden in neck creases.13
The transcervical approach also facilitates reconstruction plate fixation in the mandibular lower border in cases where it is not possible to fix the plate in the lateral border due to insufficient height in extremely atrophic mandibles (class III from Luhr et al7). Moreover, in these class III cases, longer plates should bridge to the areas that have sufficient bone height, normally the symphysis and angle/ramus regions,20,23 restoring the appropriate mandibular contour, even if the fracture area has no screws nearby due to insufficient height. The most common site of fractures in edentulous mandible is the mandibular body.3,9,13
The drawbacks of the transcervical approach are transient motor disturbances; temporary or permanent sensory loss; soft tissue infection; hematoma; scarring; fistula formation; orocervical fistula; and seroma formation.13 Another disadvantage is the necessity of major periosteal detachment, which significantly compromises the blood supply of the atrophic mandible, especially when rigid plates are used to fix the fracture.8,20
The submandibular approach14 has lower morbidity, is quicker to perform, provides easier adaptation of rigid fixation plates, and requires fewer sutures. Limited vision, multiple skin incisions, and more visible skin scars as compared with the transcervical approach are among its disadvantages.
The choice of the osteosynthesis is based on the type of fracture and the condition of the surrounding tissues.19 Rigid fixation allows free movement of the mandible, normal speech, and immediate resumption of a soft solid diet, providing greater comfort for the patient.12 This seems to be the most important factor in the fracture healing, particularly in fractures of the edentulous atrophic mandible.3,11,12 In contrast to dentate mandibles, tension, neutral, and compression zones are situated closely together due to the reduced height of the bone,11 making it more prone to complications.4,9,12 Consequently, the plates must carry a full function load (“load-bearing”) in the healing period and counteract the masticatory forces.23,24 If miniplates are intended to be functional, they should be positioned in the tension border of the mandible to counteract the muscle pull exerted by the suprahyoid muscles.18 This could compromise the patient's function in the postoperative period due to trauma promoted by the prosthesis or solid food over the thin mucosa overlying the plates.25
The locking plate/screw systems is probably the best device to fix fractured atrophic mandibles nowadays, as it shares the functional load with the bone, provides greater stability, does not require perfect adaptation, and decreases inflammatory complications from loosening hardware.18,24
Finally, fracture stability, immediate function, and control of systemic deficits will result in the lowest morbidity in the management of edentulous mandible fractures,22 with long-term maxillomandibular fixation unacceptable nowadays, especially in systemically compromised patients.1,12
CONCLUSION
The importance of the preoperative evaluation of the patient (i.e., ASA; surgical risk) and the correct choice of the fixation material are paramount for a postoperative period without complication. Class III multiple fractured atrophic mandibles are probably an indication for transcervical approach, as they require longer rigid plates for fixation, which would protect fragile areas. In cases where atrophic mandible was labeled as class I or II, the isolated submandibular approaches present good results, if the fractures are sufficiently distant from each other.
References
- Eyrich G K, Gratz K W, Sailer H F. Surgical treatment of fractures of the edentulous mandible. J Oral Maxillofac Surg. 1997;55:1087–1088. doi: 10.1016/s0278-2391(97)90284-6. [DOI] [PubMed] [Google Scholar]
- Barber H D. Conservative management of the fractured atrophic edentulous mandible. J Oral Maxillofac Surg. 2001;59:789–791. doi: 10.1053/joms.2001.24734. [DOI] [PubMed] [Google Scholar]
- Bruce R A, Ellis E., III The second Chalmers J. Lyons Academy study of fractures of the edentulous mandible. J Oral Maxillofac Surg. 1993;51:904–911. doi: 10.1016/s0278-2391(10)80113-2. [DOI] [PubMed] [Google Scholar]
- Bruce R A, Strachan D S. Fractures of the edentulous mandible: the Chalmer J. Lyons Academy study. J Oral Surg. 1976;34:973–979. [PubMed] [Google Scholar]
- Marciani R D. Invasive management of the fractured atrophic edentulous mandible. J Oral Maxillofac Surg. 2001;59:792–795. doi: 10.1053/joms.2001.24736. [DOI] [PubMed] [Google Scholar]
- Wittwer G, Adeyemo W L, Turhani D, Ploder O. Treatment of atrophic mandibular fractures based on the degree of atrophy—experience with different plating systems: a retrospective study. J Oral Maxillofac Surg. 2006;64:230–234. doi: 10.1016/j.joms.2005.10.025. [DOI] [PubMed] [Google Scholar]
- Madsen M J, Haug R H. A biomechanical comparison of 2 techniques for reconstructing atrophic edentulous mandible fractures. J Oral Maxillofac Surg. 2006;64:457–465. doi: 10.1016/j.joms.2005.11.018. [DOI] [PubMed] [Google Scholar]
- Choi B H, Huh J Y, Suh C H, Kim K N. An in vitro evaluation of miniplate fixation techniques for fractures of the atrophic edentulous mandible. Int J Oral Maxillofac Surg. 2005;34:174–177. doi: 10.1016/j.ijom.2003.10.024. [DOI] [PubMed] [Google Scholar]
- Mugino H, Takagi S, Oya R, Nakamura S, Ikemura K. Miniplate osteosynthesis of fractures of the edentulous mandible. Clin Oral Investig. 2005;9:266–270. doi: 10.1007/s00784-005-0012-5. [DOI] [PubMed] [Google Scholar]
- Schug T, Rodemer H, Neupert W, Dumbach J. Treatment of complex mandibular fractures using titanium mesh. J Craniomaxillofac Surg. 2000;28:235–237. doi: 10.1054/jcms.2000.0146. [DOI] [PubMed] [Google Scholar]
- Luhr H G. On the stable osteosynthesis in mandibular fractures. Dtsch Zahnarztl Z. 1968;23:754. [PubMed] [Google Scholar]
- Luhr H G, Reidick T, Merten H A. Results of treatment of fractures of the atrophic edentulous mandible by compression plating: a retrospective evaluation of 84 consecutive cases. J Oral Maxillofac Surg. 1996;54:250–254. doi: 10.1016/s0278-2391(96)90733-8. [DOI] [PubMed] [Google Scholar]
- Landa L E, Tartan B F, Acartuk A, Skouteris C A, Gordon C, Sotereanos G C. The transcervical incision for use in oral and maxillofacial surgical procedures. J Oral Maxillofac Surg. 2003;61:343–346. doi: 10.1053/joms.2003.50035. [DOI] [PubMed] [Google Scholar]
- Risdon F. Ankylosis of the temporomaxillary joint. J Am Dent Assoc. 1934;21:1933–1937. [Google Scholar]
- Ellis E., III Condylar process fractures of the mandible. Facial Plast Surg. 2000;16:193–205. doi: 10.1055/s-2000-12579. [DOI] [PubMed] [Google Scholar]
- Bradley J C. A radiological investigation into the age changes of the inferior dental artery. Br J Oral Surg. 1975;13:82–90. doi: 10.1016/0007-117x(75)90027-x. [DOI] [PubMed] [Google Scholar]
- Ellis E, III, Moos K F, el-Attar A. Ten years of mandibular fractures: an analysis of 2,137 cases. Oral Surg Oral Med Oral Pathol. 1985;59:120–129. doi: 10.1016/0030-4220(85)90002-7. [DOI] [PubMed] [Google Scholar]
- Sikes J W, Jr, Smith B R, Mukherjee D P. An in vitro study of the effect of bony buttressing on fixation strength of a fractured atrophic edentulous mandible model. J Oral Maxillofac Surg. 2000;58:56–61. doi: 10.1016/s0278-2391(00)80017-8. [DOI] [PubMed] [Google Scholar]
- Eyrich G K, Grätz K W, Sailer H F. Surgical treatment of fractures of the edentulous mandible. J Oral Maxillofac Surg. 1997;55:1081–1087. doi: 10.1016/s0278-2391(97)90284-6. [DOI] [PubMed] [Google Scholar]
- Buchbinder D. Treatment of fractures of the edentulous mandible, 1943 to 1993: a review of the literature. J Oral Maxillofac Surg. 1993;51:1174–1180. doi: 10.1016/s0278-2391(10)80285-x. [DOI] [PubMed] [Google Scholar]
- Muravchick S. Anesthesia of the elderly. In: Miller R D, editor. Anesthesia. 5th ed. Vol. 2. Philadelphia: Churchill-Livingstone; 1999. pp. 2140–2156. [Google Scholar]
- Luhr H G, Reidick T, Merten H A. Results of treatment of fractures of the atrophic edentulous mandible by compression plating: a retrospective evaluation of 84 consecutive cases. J Oral Maxillofac Surg. 1996;54:254–255. doi: 10.1016/s0278-2391(96)90733-8. [DOI] [PubMed] [Google Scholar]
- Schilli W, Stoll P, Bähr W, Prein J. Mandibular fractures. In: Prein J, editor. Manual of Internal Fixation in the Cranio-Facial Skeleton. Berlin: Springer-Verlag; 1998. pp. 57–93. [Google Scholar]
- Ellis E. Selection of internal fixation devices for mandibular fracture: how much fixation is enough? Semin Plast Surg. 2002;16:229. [Google Scholar]
- Dingman R O, Natvig P. Mandibular fractures. In: Dingman R O, editor. Surgery of Facial Fractures. Philadelphia: Saunders; 1964. pp. 185–206. [Google Scholar]