Abstract
Objectives
Pharmacologic evidence suggests adequate antiplatelet activity in diabetic patients requires >100 mg aspirin daily, yet recent trials have used ≤100 mg daily. This meta-analysis explored the relationship between aspirin dose and prevention of cardiovascular events.
Data Sources
Six electronic databases were searched using database-appropriate terms for aspirin, diabetes, and comparative study from inception until February 2010.
Review Methods
Randomized controlled trials and cohort studies comparing aspirin to no antiplatelet therapy were included if they reported cardiovascular events as pre-specified outcomes, aspirin dose, and number of diabetic patients. Studies were stratified by daily aspirin dose (≤100 mg; 101–325 mg; >325 mg) and pooled risk ratios (RR) were calculated using random effects models. All-cause mortality was the primary outcome of interest. Cardiovascular-related mortality, myocardial infarction, and stroke were secondary outcomes.
Results
Data for diabetic patients were available from 21 studies (n = 17,522). Overall, 1,172 (15.4%) of 7,592 aspirin users and 1,520 (18.4%) of 8,269 controls died (p = 0.31). The pooled RRs were 0.89 (95% CI: 0.72–1.10; p = 0.27) from 13 studies using ≤100 mg (I2 = 64%); 0.89 (95% CI: 0.61–1.30; p = 0.55) from four studies using 101–325 mg (I2 = 83%); and 0.96 (95% CI: 0.85–1.08; p = 0.50) from eight studies using >325 mg (I2 = 0%). Aspirin use was associated with a significantly lower risk of mortality (RR: 0.82; 95% CI: 0.69–0.98; p = 0.03) in 13 secondary prevention studies (I2 = 27%), whereas aspirin use in seven primary prevention studies (I2 = 0%) was not (RR: 1.01; 95% CI 0.85–1.19; p = 0.94). A substantial amount of heterogeneity was observed amongst studies in all outcomes. Although inclusion of cohort studies was a major source of heterogeneity, stratification by study design did not reveal a significant dose-response relationship.
Conclusions/Interpretation
This summary of available data does not support an aspirin dose-response effect for prevention of cardiovascular events in diabetic patients. However, the systematic review identified an important gap in randomized controlled trial evidence for using 101–325 mg aspirin daily in diabetes.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-011-1757-y) contains supplementary material, which is available to authorized users.
KEY WORDS: aspirin, diabetes, mortality, myocardial infarction, stroke
BACKGROUND
Antiplatelet therapy, primarily with 75–325 mg aspirin daily, is recommended to prevent cardiovascular events in diabetes.1–3 These recommendations are based on evidence that antiplatelet therapy significantly reduces the risk of cardiovascular events without an excessive risk of adverse effects.4–9 Historically, the majority of this evidence was generated from studies enrolling patients without diabetes, but since diabetes was considered a “coronary risk equivalent”10 these conclusions were extended to diabetic patients.
Recently, 2 clinical trials examined the use of ≤100 mg aspirin daily for primary prevention of cardiovascular events in diabetic patients.11,12 Along with a diabetic subgroup analysis of the Primary Prevention Program, these studies concluded that ≤100 mg aspirin daily does not significantly lower the risk of death or a primary cardiovascular event.8,11,12 Moreover, data from observational studies suggest primary prevention with low dose aspirin may be associated with more harm than benefit.13,14 In light of such studies, the role of aspirin for preventing cardiovascular events in diabetes is being questioned.15,16 Indeed, six meta-analyses published since 2009 have not found any significant benefit for aspirin in primary prevention of cardiovascular events in diabetes.16–21
One possible explanation for the apparent lack of benefit is aspirin resistance.22 Diabetes is associated with numerous biochemical abnormalities, including elevated platelet reactivity.23,24 Indeed, diabetic patients have a lower response to aspirin compared to the general population.25–27 Although the exact mechanisms are not clear, a subgroup analysis of the Aspirin-Induced Platelet Effect (ASPECT) study demonstrated that diabetic patients exhibited a significantly lower rate of resistance when given >100 mg daily compared with a lower (and more commonly used) dose of 81 mg daily.28,29 Moreover, the Antithrombotic Trialists’ (ATT) Collaboration reported that <75 mg aspirin daily was not associated with a significantly lower risk of vascular events, while 75–1500 mg aspirin daily was.5 However, this dose-response relationship was examined in a group of high risk patients regardless of diabetes status.
The potential dose-response relationship for antiplatelet activity could have important implications for diabetes management if it is more than just a surrogate measure, especially since most diabetic patients using aspirin to prevent cardiovascular events take ≤100 mg daily.29 However, this theoretical relationship, generated from pharmacologic evidence, has not been adequately tested. To our knowledge, the Early Treatment for Diabetic Retinopathy Study (ETDRS) is the only randomized controlled trial that evaluated >100 mg aspirin daily in diabetic patients exclusively.9 This meta-analysis extends the observations of previous meta-analyses by specifically examining the effect of aspirin dose on both primary and secondary prevention of cardiovascular events in diabetic patients alone. We hypothesized that effectiveness to prevent cardiovascular events would vary according to daily aspirin dose.
METHODS
Data Sources and Searches
Randomized controlled trials, post hoc analyses of randomized controlled trial data, and cohort studies, published in any language, were eligible for inclusion if they evaluated the association between aspirin and cardiovascular outcomes.
Medline (1950–), Embase (1980-), Cochrane Library (Issue 2, 2010), Web of Science: Science Citation Index (1900–), International Pharmaceutical Abstracts (1970–), and Scopus (1960–) were searched until February 7, 2010. Database-appropriate terms for aspirin, diabetes, and comparative study were combined to identify articles. The Medline search strategy is provided in APPENDIX 1 (available online). We also hand-searched reference lists of all potentially relevant studies and review articles addressing at least two of the following topics: diabetes management, aspirin use, and cardiovascular risk reduction.
Study Selection
Two investigators independently screened the English title and abstract of all citations gathered in the literature search to identify potentially relevant studies. The peer-reviewed article for each potentially relevant study was retrieved and examined independently by two investigators to determine if it met pre-specified inclusion criteria. A study was included if it: compared aspirin to placebo or a treatment arm using neither antiplatelet nor anticoagulant therapy; reported all-cause mortality, cardiovascular-related mortality, myocardial infarction, or stroke as a pre-specified outcome; specified the aspirin dose each patient used; and reported the proportion of diabetic patients included in the study. Companion studies, such as epidemiologic follow-up studies of randomized controlled trial participants, were excluded. Discrepancies regarding study inclusion were resolved by discussion.
Assessment of Methodological Quality
One investigator evaluated methodological quality of included studies using a 27-item checklist to examine reporting quality, external validity, internal validity, and power.30 A second investigator verified accuracy of the assessment.
Data Extraction
One investigator used a standardized form to collect information on diabetic patients from each included study. A second investigator verified completeness and accuracy. Variables collected included the study design, number of diabetic patients enrolled, diabetes type (type 1 or type 2), daily aspirin dose, therapy used in the control group, history of cardiovascular disease at study enrolment (to determine if the study examined primary or secondary prevention), duration of aspirin therapy, duration of study follow-up, and number of cardiovascular events (all-cause mortality, cardiovascular-related mortality, myocardial infarction, or stroke) in each group. Data were obtained from the original article and through contact with study authors. A study was excluded at this stage if we were unable to obtain information on any cardiovascular events for diabetic patients according to our dose strata (described below).
Data Synthesis
Data were analyzed using Review Manager (RevMan 5, Cochrane, Denmark). Pooled risk ratios (RR) and 95% confidence intervals (95% CI) were calculated using a random effects model.31 Studies were grouped according to daily aspirin dose (≤100 mg; 101–325 mg; >325 mg) to examine the effect of dose on the association between aspirin and cardiovascular outcomes. The potential benefit of higher aspirin doses preventing a cardiovascular event may be offset by an increased risk of bleeding.32,33 Therefore, all-cause mortality was chosen as the primary outcome because it provides a balanced assessment of overall safety and effectiveness for any treatment option.34 Given the likelihood of combining data from studies published in different decades and conducted in different countries, we also believed all-cause mortality would provide a homogeneous outcome measure. Although cardiovascular disease is the leading cause of death in diabetes,35,36 we felt the attribution of cause of death may vary over time and across countries. Nevertheless, cardiovascular-related mortality, myocardial infarction, and stroke were examined as secondary outcomes.
Heterogeneity amongst studies was examined using the I2 statistic. Although all included studies examined a similar question (effect of aspirin for prevention of cardiovascular events), two sources of heterogeneity were identified a priori and examined. First, we stratified the analyses according to primary (no cardiovascular disease prior to study enrolment) and secondary (documented cardiovascular disease at study enrolment) prevention. Second, we constructed separate analyses for randomized controlled trials and cohort studies.
RESULTS
Overview of Studies
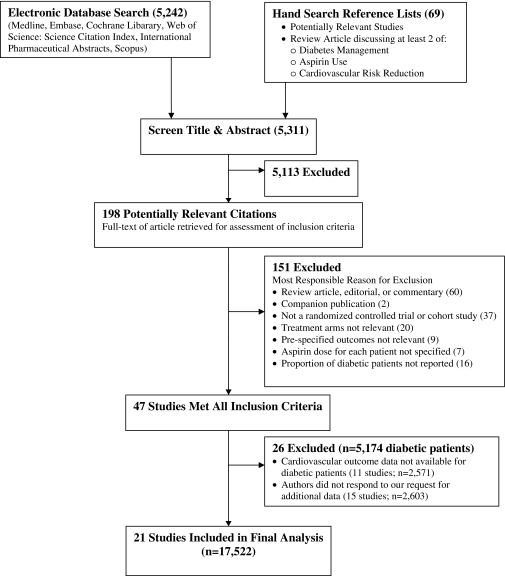
We identified 5,311 unique citations and 198 were considered potentially relevant (Fig. 1). Following independent review of the full articles, there was disagreement on the allocation of 17 (9%). After discussion, we determined that 47 studies met all inclusion criteria. However, we could not obtain any cardiovascular event data for diabetic patients from 26 studies. Data on diabetic patients were not available from 11 studies (n = 2,571) and we did not receive a response from the authors of 15 studies (n = 2,603) after two emails to both corresponding and lead authors and a registered letter sent to the corresponding author (citations available on request). Despite these subsequent exclusions, a funnel plot based on the primary outcome appeared to be symmetrical, suggesting there was minimal risk of publication bias.
Figure 1.
Citation flow diagram.
Our meta-analysis is based on 17 randomized controlled trials6–9,11,12,37–47 and four cohort studies48–51 that enrolled 17,522 diabetic patients (Table 1). The median methodological quality score was 22 (range 11 to 25), with the cohort studies having lower quality scores (median 12; range 11 to 14) compared to randomized controlled trials (median 22; range 15 to 25). Observation periods ranged from 1 to 11.6 years (median 3.8 years). Information for diabetic patients was obtained from a textbook for one study,7,52 an American Diabetes Association position statement for two studies,6,16,44 and through correspondence with authors of 15 studies.11,37–43,45–51 For each included study, we collected information on the number of diabetic patients in each treatment group and the number of cardiovascular events within each treatment group. Details of how each study identified the cardiovascular events of interest are provided in APPENDIX 2 (available online).
Table 1.
Aspirin Studies for Prevention of Cardiovascular Events Reporting Information for Diabetic Patients—Study Characteristics
| Lead Author (Study Acronym), Publication Year | Design | Follow-up (years) | Daily Aspirin Regimen | Quality Score* |
|---|---|---|---|---|
| ≤100 mg Aspirin Daily | ||||
| Diener (ESPS-2), 2009 37 | RCT | 2 | 25 mg BID | 25 |
| Ridker (WHS), 2005 38 | RCT | 10.1 (8.2–10.9) | 100 mg EOD | 24 |
| Elwin (SALT), 1991 39 | RCT | 2.7 (1.3) | 75 mg | 25 |
| Petersen (AFASAK), 1989 40 | RCT | 2 | 75 mg | 21 |
| Hansson (HOT), 1998 7 | RCT | 3.8 (3.3–4.9) | 75 mg | 22 |
| Feringa, 2009 48 | Cohort | 8.2 (5.1–10.9) | 80 mg | 12 |
| Ogawa (JPAD), 2008 11 | RCT | 4.37 (4.35–4.39) | 81 or 100 mg | 22 |
| Sacco (PPP–DM Subgroup), 2003 8 | RCT | 3.6 (2.7–4.2) | 100 mg | 21 |
| Belch (POPADAD), 2008 12 | RCT | 6.7 (4.5–8.6) | 100 mg | 24 |
| Catalano (CLIPS), 2007 41 | RCT | 1.7 ± 0.5 | 100 mg | 22 |
| Fowkes (AAA), 2010 42 | RCT | 8.2 ± 1.6 | 100 mg | 24 |
| McAlister–Low Dose, 2006 49 | Cohort | 1 | ≤100 mg | 12 |
| Cubbon–Low Dose,2008 50 | Cohort | 2 | ≤100 mg | 11 |
| Ong (FDS) Low Dose, 2010 51 | Cohort | 11.6 ± 2.9 | ≤100 mg | 14 |
| 101–325 mg Aspirin Daily | ||||
| (PHS), 1989 6 | RCT | 5.0 (3.8–6.4) | 325 mg EOD | 22 |
| Farrell (UK–TIA)–Moderate Dose, 1991 43 | RCT | 4 (1–7) | 300 mg | 22 |
| McAlister–Moderate Dose, 2006 49 | Cohort | 1 | 101–325 mg | 12 |
| Cubbon–Moderate Dose, 2008 50 | Cohort | 2 | 101–325 mg | 11 |
| Ong (FDS) Moderate Dose, 2010 51 | Cohort | 11.6 ± 2.9 | 101–325 mg | 14 |
| >325 mg Aspirin Daily | ||||
| Peto (BMD), 1988 44 | RCT | 5.5 | 500 mg | 15 |
| (ETDRS), 1992 9 | RCT | 5 (4–9) | 650 mg | 24 |
| Elwood, 1979 45 | RCT | 1 | 300 mg TID | 17 |
| (CDP Research Group), 1976 46 | RCT | 1.8 (0.8–2.3) | 324 mg TID | 19 |
| Farrell (UK–TIA)–High Dose, 1991 43 | RCT | 4 (1–7) | 600 mg BID | 22 |
| Cairns, 1985 47 | RCT | 1.5 | 325 mg QID | 20 |
| McAlister–High Dose, 2006 49 | Cohort | 1 | >325 mg | 12 |
| Cubbon–High Dose, 2008 50 | Cohort | 2 | >325 mg | 11 |
| Ong (FDS) High Dose, 2010 51 | Cohort | 11.6 ± 2.9 | >325 mg | 14 |
*Downs & Black checklist of methodological quality (maximum score = 27)30
RCT=Randomized Controlled Trial; BID = Twice Daily; EOD = Every Other Day; TID = Three Times Daily; QID = Four Times Daily
Diabetic patients comprised the entire study group for four studies,9,11,12,51 while the proportion of diabetic patients ranged from 2% to 76% (median 8.8%) in the remaining 17 (Table 2). Two studies specified that all diabetic patients had type 2 diabetes.11,51 Two studies reported enrolling patients with type 1 or type 2 diabetes;9,12 however, only one of these provided cardiovascular event data according to diabetes type.9 This limited amount of information precluded any further analyses based on diabetes type. Seven studies examined the effect of aspirin in primary prevention6,8,11,12,38,42,44 and seven studies examined the effect of aspirin in secondary prevention.37,39,43,45–47,50 In the remaining seven studies, 3% to 60% of diabetic patients had a history of myocardial infarction, stroke, or coronary heart disease at study enrolment.7,9,40,41,48,49,51 While the authors of one study provided information according to primary or secondary prevention,51 we assumed the remaining six studies reported a mix of primary and secondary cardiovascular events.7,9,40,41,48,49
Table 2.
Aspirin Studies for Prevention of Cardiovascular Events Reporting Information for Diabetic Patients—Patient Characteristics
| Lead Author (Study Acronym), Publication Year | Data Source* | Diabetic Patients n (%)† | Diabetes Type | Cardiovascular History | Prevention Type | Outcomes Reported for Diabetic Patients | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Prior MI | Prior Stroke or TIA | Prior CHD | All-Cause Mortality | CV-Related Mortality | MI | Stroke | |||||
| ≤100 mg Aspirin Daily | |||||||||||
| Diener (ESPS-2), 2009 37 | Authors | 479 (15%) | NR | NR | 100% | NR | Secondary | X | X | ||
| Ridker (WHS), 2005 38 | Authors | 1027 (3%) | NR | 0% | 0% | 0% | Primary | X | X | ||
| Elwin (SALT), 1991 39 | Authors | 180 (13%) | NR | 14.4% | 100% | 23.9% | Secondary | X | X | X | X |
| Petersen (AFASAK), 1989 40 | Authors | 59 (9%) | NR | 7.4%‡ | 5.7%‡ | NR | Mixed | X | X | X | |
| Hansson (HOT), 1998 7 | Textbook 52 | 1501 (8%) | NR | 2.5% | 2.5% | 11.1% | Mixed | X | X | X | X |
| Feringa, 2009 48 | Authors | 161 (10%) | NR | 55.0% | 60.0% | 25.0% | Mixed | X | X | X | X |
| Ogawa (JPAD), 2008 11 | Authors | 2539 (100%) | 2 | 0% | 0% | 0% | Primary | X | X | X | X |
| Sacco (PPP-DM Subgroup), 2003 8 | Article | 1031 (22%) | NR | 0% | 0% | 0% | Primary | X | X | X | X |
| Belch (POPADAD), 2008 12 | Article | 1276 (100%) | 1 & 2 | 0% | 0% | 0% | Primary§ | X | X | X | X |
| Catalano (CLIPS), 2007 41 | Authors | 277 (76%) | NR | 3%‡ | 4%‡ | NR | Mixed§ | X | X | X | X |
| Fowkes (AAA), 2010 42 | Authors | 88 (3%) | NR | 0% | 0% | 0% | Primary§ | X | X | X | X |
| McAlister-Low Dose, 2006 49 | Authors | 695 (10%) | NR | 36%‡ | 13%‡ | NR | Mixed | X | |||
| Cubbon-Low Dose,2008 50 | Authors | 273 (11%) | NR | NR | NR | 100% | Secondary | X | |||
| Ong (FDS) Low Dose, 2010 51 | Authors | 405 (100%) | 2 | 3% | 0% | 31% | Mixed | X | X | X | X |
| 101-325 mg Aspirin Daily | |||||||||||
| (PHS), 1989 6 | ADA Statement 16 | 533 (2%) | NR | 0% | 0% | 0% | Primary | X | X | ||
| Farrell (UK-TIA)-Moderate Dose, 1991 43 | Authors | 45 (2%) | NR | 14% | 100% | NR | Secondary | X | X | X | X |
| McAlister-Moderate Dose, 2006 49 | Authors | 1381 (19%) | NR | 36%‡ | 13%‡ | NR | Mixed | X | |||
| Cubbon-Moderate Dose, 2008 50 | Authors | 105 (4%) | NR | NR | NR | 100% | Secondary | X | |||
| Ong (FDS) Moderate Dose, 2010 51 | Authors | 547 (100%) | 2 | 4% | 0% | 41% | Mixed | X | X | X | X |
| >325 mg Aspirin Daily | |||||||||||
| Peto (BMD), 1988 44 | ADA Statement 16 | 101 (2%) | NR | 0% | 0% | 0% | Primary | X | |||
| (ETDRS), 1992 9 | Article | 3711 (100%) | 1 & 2 | 5.5% | 1.5% | 7.7% | Mixed | X | X | X | X |
| Elwood, 1979 45 | Authors | 66 (4%) | NR | 100% | NR | NR | Secondary | X | X | X | X |
| (CDP Research Group), 1976 46 | Authors | 85 (6%) | NR | 100% | 11.9%‡ | NR | Secondary | X | |||
| Farrell (UK-TIA)-High Dose, 1991 43 | Authors | 45 (2%) | NR | 10% | 100% | NR | Secondary | X | X | X | X |
| Cairns, 1985 47 | Authors | 44 (16%) | NR | 40.0%‡ | 2.0%‡ | NR | Secondary║ | X | X | X | X |
| McAlister-High Dose, 2006 49 | Authors | 491 (7%) | NR | 36%‡ | 13%‡ | NR | Mixed | X | |||
| Cubbon-High Dose, 2008 50 | Authors | 39 (2%) | NR | NR | NR | 100% | Secondary | X | |||
| Ong (FDS) High Dose, 2010 51 | Authors | 338 (100%) | 2 | 1% | 0% | 21% | Mixed | X | X | X | X |
*Data source for outcomes in diabetic patients (Authors = authors provided supplemental data not included in original article; Textbook = data obtained from a textbook52; Article = data obtained from original article; ADA Statement = data obtained from the American Diabetes Association position statement on aspirin use for primary prevention in diabetes16)
†Number of diabetic patients and proportion of entire study sample
‡Presence of cardiovascular disease at baseline for entire study sample
§All patients had peripheral arterial disease at baseline
║All patients had unstable angina
MI = Myocardial Infarction; TIA = Transient Ischemic Attack; CHD = Coronary Heart Disease; NR = Not Reported
Three cohort studies and one randomized controlled trial examined the effect of two or more aspirin doses relative to a control group on cardiovascular events.43,49–51 To avoid double-counting events in the control group, and therefore minimize a unit of analysis error, we divided the number of patients and events in the control group by the number of aspirin dose groups and entered each pair-wise comparison separately.53 Stratification according to daily aspirin dose produced 14 studies (n = 9,991) using ≤100 mg daily, five studies (n = 2,611) using 101–325 mg daily, and nine studies (n = 4,920) using >325 mg daily relative to a control group using placebo or no antiplatelet or anticoagulant therapy (Table 2).
Main Analyses
The primary outcome analysis was based on 1,172 (15.4%) deaths in 7,592 aspirin users and 1,520 (18.4%) deaths in 8,269 controls (APPENDIX 3A, available online). The pooled RR from these 25 studies (I2 = 57%), was 0.93 (95% CI: 0.81-1.07; p = 0.31). Stratification according to daily aspirin dose revealed small, non-significant differences in the pooled RRs (Table 3). Although the pooled RR for each dose group suggested a lower risk of mortality with aspirin use, there was substantial heterogeneity amongst studies and none of the associations were statistically significant.
Table 3.
Main and Stratified Analyses of the Effect of Aspirin Dose on Cardiovascular Outcomes
| Group | Main Analyses | Primary Prevention Only | Secondary Prevention Only | Cohort Study Only | RCT Only | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | RR (95% CI) | I2 | n | RR (95% CI) | I2 | n | RR (95% CI) | I2 | n | RR (95% CI) | I2 | n | RR (95% CI) | I2 | |
| All-Cause Mortality | |||||||||||||||
| ≤100 mg | 13 | 0.89 (0.72–1.10) | 64% | 5 | 0.94 (0.77–1.14) | 0% | 4 | 0.80 (0.58–1.11) | 64% | 4 | 0.71 (0.42–1.19) | 89% | 9 | 0.96 (0.82–1.12) | 0% |
| 101–325 mg | 4 | 0.89 (0.61–1.30) | 83% | 1 | 1.29 (0.90–1.84) | NA | 3 | 0.74 (0.52–1.03) | 39% | 3 | 0.89 (0.59–1.35) | 88% | 1 | 0.83 (0.27–2.51) | NA |
| >325 mg | 8 | 0.96 (0.85–1.08) | 0% | 1 | 0.78 (0.07–8.66) | NA | 6 | 1.11 (0.76–1.60) | 0% | 3 | 1.32 (0.86–2.04) | 0% | 5 | 0.93 (0.82–1.06) | 0% |
| All Studies | 25 | 0.93 (0.81–1.07) | 57% | 7 | 1.01 (0.85–1.19) | 0% | 13 | 0.82 (0.69–0.98) | 27% | 10 | 0.88 (0.67–1.14) | 81% | 15 | 0.94 (0.85–1.04) | 0% |
| Cardiovascular Mortality | |||||||||||||||
| ≤100 mg | 9 | 0.81 (0.52–1.25) | 65% | 5 | 0.74 (0.36–1.52) | 49% | 2 | 0.93 (0.61–1.43) | 0% | 2 | 0.62 (0.10–4.02) | 93% | 7 | 0.92 (0.64–1.32) | 25% |
| 101–325 mg | 2 | 1.52 (1.13–2.06) | 0% | 1 | 1.22 (0.65–2.29) | NA | 2 | 0.98 (0.67–1.43) | 0% | 1 | 1.52 (1.11–2.07) | NA | 1 | 1.66 (0.38–7.27) | NA |
| >325 mg | 5 | 0.89 (0.77–1.04) | 0% | 1 | 1.69 (0.15–18.96) | NA | 4 | 0.98 (0.57–1.68) | 0% | 1 | 1.77 (0.35–8.92) | NA | 4 | 0.89 (0.76–1.04) | 0% |
| All Studies | 16 | 0.98 (0.76–1.25) | 54% | 7 | 0.98 (0.63–1.53) | 26% | 8 | 0.96 (0.75–1.24) | 0% | 4 | 1.01 (0.50–2.05) | 82% | 12 | 0.91 (0.80–1.04) | 0% |
| Myocardial Infarction | |||||||||||||||
| ≤100 mg | 10 | 0.77 (0.53–1.11) | 68% | 6 | 1.12 (0.81–1.56) | 47% | 2 | 0.45 (0.22–0.92) | 0% | 2 | 0.94 (0.30–3.00) | 91% | 8 | 0.72 (0.48–1.08) | 58% |
| 101–325 mg | 3 | 0.98 (0.31–3.12) | 88% | 2 | 0.88 (0.20–3.87) | 94% | 2 | 1.28 (0.41–3.98) | 0% | 1 | 1.81 (1.36–2.41) | NA | 2 | 0.61 (0.19–1.95) | 53% |
| >325 mg | 5 | 0.85 (0.73–0.99) | 0% | 1 | 1.77 (0.35–8.89) | NA | 3 | 0.78 (0.41–1.49) | 0% | 1 | 1.76 (0.35–8.83) | NA | 4 | 0.85 (0.73–0.99) | 0% |
| All Studies | 18 | 0.84 (0.65–1.09) | 71% | 9 | 1.06 (0.75–1.51) | 70% | 7 | 0.68 (0.44–1.06) | 0% | 4 | 1.26 (0.70–2.27) | 80% | 14 | 0.76 (0.59–0.97) | 47% |
| Stroke | |||||||||||||||
| ≤100 mg | 12 | 0.81 (0.68–0.97) | 0% | 6 | 0.81 (0.55–1.19) | 49% | 2 | 0.83 (0.60–1.15) | 0% | 2 | 1.50 (0.83–2.73) | 0% | 10 | 0.76 (0.63–0.92) | 0% |
| 101–325 mg | 3 | 1.57 (1.08–2.30) | 0% | 2 | 1.52 (1.01–2.27) | 0% | 1 | 1.84 (0.59–5.73) | NA | 1 | 1.56 (0.97–2.50) | NA | 2 | 1.60 (0.85–3.03) | 0% |
| >325 mg | 6 | 1.20 (0.91–1.59) | 0% | 2 | 1.30 (0.24–7.05) | 0% | 3 | 1.51 (0.55–4.14) | 0% | 1 | 1.18 (0.09–16.05) | NA | 5 | 1.20 (0.91–1.59) | 0% |
| All Studies | 21 | 0.98 (0.82–1.16) | 20% | 10 | 0.98 (0.71–1.35) | 46% | 6 | 0.92 (0.69–1.24) | 0% | 4 | 1.53 (1.06–2.21) | 0% | 17 | 0.90 (0.76–1.07) | 9% |
RCT = Randomized Controlled Trial; n = Number of studies contributing data; NA = Not Appropriate; RR = Pooled Risk Ratio;
95% CI = 95% Confidence Interval
Cardiovascular mortality was reported in 447 (7.7%) of 5,798 aspirin users and 599 (9.3%) of 6,456 controls (APPENDIX 3B, available online). The pooled RR, based on data from 16 studies (I2 = 54%), was 0.98 (95% CI: 0.76–1.25; p = 0.86). Stratification by daily aspirin dose did not reveal a significant dose–response relationship (Table 3).
A myocardial infarction occurred in 547 (8.3%) of 6,605 aspirin users and 720 (10.0%) of 7,210 controls (APPENDIX 3C, available online). The pooled RR, based on data from 18 studies (I2 = 71%), was 0.84 (95% CI: 0.65–1.09; p = 0.20). When stratified by daily aspirin dose (Table 3), there was substantial heterogeneity amongst 10 studies using ≤100 mg (I2 = 68%) and 3 studies using 101–325 mg (I2 = 88%). However, there was no significant heterogeneity amongst the 5 studies using >325 mg daily (I2 = 0%) and there was a significantly lower risk of myocardial infarction (RR: 0.85; 95% CI: 0.73–0.99; p = 0.04) associated with aspirin use.
A stroke occurred in 344 (5.0%) of 6,902 aspirin users and 418 (5.6%) of 7,420 controls (APPENDIX 3D, available online). The pooled RR, based on data from 21 studies (I2 = 20%) was 0.98 (95% CI: 0.82–1.16; p = 0.80). When stratified according to daily aspirin dose (Table 3), there was no significant heterogeneity (I2 = 0%) in all three dose groups. Use of ≤100 mg daily was associated with a significantly lower risk of stroke (RR: 0.81; 95% CI: 0.68–0.97; p = 0.02).
Stratified Analyses
With the substantial amount of heterogeneity observed amongst studies, we had sufficient information to examine two potential sources in detail (Table 3). The first approach was to stratify studies according to prevention strategy. When data from seven primary prevention studies were combined (I2 = 0%), the pooled RR was 1.01 (95% CI: 0.85–1.19; p = 0.94). However, when data from 13 secondary prevention studies were pooled (I2 = 27%), there was a significantly lower risk of all-cause mortality (RR: 0.82; 95% CI: 0.69–0.98; p = 0.03). Although this lower risk seemed to be associated with ≤325 mg aspirin daily (RR: 0.77; 95% CI: 0.63–0.95; p = 0.02), there was still substantial heterogeneity amongst these seven studies (I2 = 48%).
The second approach was to stratify according to study design, which identified that a major source of heterogeneity was inclusion of cohort studies. When data from randomized controlled trials alone were examined (Table 3), there was no significant heterogeneity (I2 = 0%) for most analyses. However, we also identified that there are only 2 randomized controlled trials—the Physicians’ Health Study (PHS) and the United Kingdom Transient Ischaemic Attack (UK–TIA) aspirin trial—examining 101–325 mg aspirin daily in 578 diabetic patients.6,43 Moreover, the UK–TIA is the only randomized controlled trial to report all-cause mortality rates in 29 diabetic patients using 101–325 mg aspirin daily.43 In contrast, stroke rates were reported in all 17 randomized controlled trials. Although there was no significant difference in stroke risk when these data were combined (RR: 0.90; 95% CI: 0.76–1.07; p = 0.23; I2 = 9%), there was a significantly lower risk (RR: 0.76; 95% CI: 0.63–0.92; p < 0.01) associated with ≤100 mg aspirin daily when data from 10 randomized controlled trials using were combined (I2 = 0%).
Other potential sources of heterogeneity include duration of follow-up, methodological quality, proportion of diabetics in the study sample, age, gender, diabetes type, prevalence of comorbidities, and management of other cardiovascular risk factors. With the limited amount of available data, we conducted post hoc analyses stratifying studies based on duration of follow-up, methodological quality, and proportion of diabetics in the study sample. These were consistent with the pre-specified subgroup analyses (data available on request).
DISCUSSION
This meta-analysis examined the effect of dose on the association between aspirin and cardiovascular outcomes using data from 21 studies with 17,522 diabetic patients. Overall, we found that aspirin use was not associated with a statistically significant difference in mortality risk and stratification by daily aspirin dose revealed only small differences in the pooled risk ratios. We did observe two significant associations within different dose strata for other cardiovascular outcomes. First, daily doses >325 mg were associated with a 15% (95% CI: 1% to 27%; p = 0.04) lower risk of myocardial infarction. Second, daily doses ≤100 mg were associated with a 19% (95% CI: 3% to 32%; p = 0.02) lower risk of stroke. However, in both analyses, there was a substantial amount of heterogeneity amongst studies and there was no apparent dose-response relationship.
When examining sources of heterogeneity, we observed an 18% (95% CI: 2% to 31%; p = 0.03) lower risk of all-cause mortality in the 13 studies enrolling diabetic patients with a history of cardiovascular disease. Although the lower mortality risk seemed to be associated with ≤325 mg aspirin daily, there was still a substantial amount of heterogeneity amongst studies. Stratification by study design identified that inclusion of cohort studies was a major source of heterogeneity. Restriction to randomized controlled trials also identified that only 578 diabetic patients have been included in studies using 101–325 mg aspirin daily.
Although the totality of available evidence neither confirms nor refutes our dose-response hypothesis for aspirin and prevention of cardiovascular events in diabetes, this meta-analysis contributes novel information. Our literature search and contact with original study authors provides the most comprehensive collection of data examining the effect of aspirin for primary and secondary prevention of cardiovascular events in diabetes. Our systematic literature review also found an important evidence gap whereby very few studies examined the effect of 101–325 mg aspirin daily in diabetic patients.
Previous Literature
Our results are consistent with observations from previous meta-analyses assessing aspirin use for primary prevention of cardiovascular events in people with diabetes16,17,19–21 and other high-risk patient populations.18 These meta-analyses used various combinations of data from nine randomized controlled trials to examine the effect of 50–650 mg daily aspirin on primary prevention of cardiovascular events.6–9,11,12,38,44,52,54 Despite differences in study inclusion, all six meta-analyses reported similar pooled risk ratios for cardiovascular outcomes (Table 4).16–19 We excluded the ETDRS and Hypertension Optimal Treatment (HOT) studies from our stratified analyses examining aspirin use in primary prevention because 8% and 11% of patients reported a history of cardiovascular disease at enrolment, respectively.7,9 Therefore, we could not be certain if these studies were reporting primary or secondary cardiovascular events. We also included data from the Aspirin for Asymptomatic Athersclerosis (AAA) Trial, which was published after the search strategies were completed in other meta-analyses.42 Even with a different mix of studies, however, we observed similar associations for all-cause mortality, cardiovascular-related mortality, and stroke (Table 4).
Table 4.
Pooled Risk Ratios for Primary Prevention with Aspirin in People with Diabetes from Other Systematic Reviews
| Lead Author, Publication Year | All Cause Mortality | Cardiovascular Mortality | Myocardial Infarction | Stroke | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | RR (95% CI) | I2 | n | RR (95% CI) | I2 | n | RR (95% CI) | I2 | n | RR (95% CI) | I2 | |
| De Berardis, 2009 17 | 4 | 0.93 (0.82–1.05) | 0% | 4 | 0.94 (0.72–1.23) | 57% | 6 | 0.86 (0.61–1.21) | 62% | 5 | 0.83 (0.72–1.23) | 53% |
| ATT Collaboration, 2009 18 | NR | NR | 6 | 0.88 (0.67–1.15)* | NR | NR | 0.81 (0.51–1.30)† | NR | ||||
| Zhang, 2010 19 | 5 | 0.95 (0.85–1.06) | 0% | 5 | 0.95 (0.71–1.27) | 41% | 7 | 0.85 (0.65–1.11) | 55% | 6 | 0.83 (0.63–1.10) | 44% |
| Pignone, 2010 16 | NR | NR | 9 | 0.91 (0.79–1.05)‡ | 8% | 9 | 0.85 (0.66–1.11) | 36% | ||||
| Younis, 2010 20 | 3 | 0.96 (0.78–1.18) | NR | NR | 6 | 0.95 (0.76–1.18) | NR | 3 | 0.75 (0.55–1.02) | NR | ||
| Stavrakis, 2011 21 | 4 | 0.99 (0.82–1.20) | 0% | 4 | 0.99 (0.62–1.60) | 39% | 3 | 0.83 (0.40–1.72) | 64% | 3 | 0.70 (0.44–1.11) | 29% |
| Simpson | 7 | 1.01 (0.85–1.19) | 0% | 7 | 0.98 (0.63–1.53) | 26% | 9 | 1.06 (0.75–1.51) | 70% | 10 | 0.98 (0.71–1.35) | 46% |
*Reported as “Serious Vascular Events”
†Reported as “Ischemic Stroke”
‡Combined “Major Coronary Event (coronary heart disease death + nonfatal myocardial infarction + sudden death)” reported in three studies with “Coronary heart disease death + nonfatal myocardial infarction” reported in one study and “Fatal + non-fatal myocardial infarction” reported in five studies
n=Number of studies contributing data; ATT = Antithrombotic Trialists’; NR = Not Reported; RR = Pooled Risk Ratio; 95% CI = 95% Confidence Interval
Our meta-analysis also extends the current understanding of aspirin use in people with diabetes garnered from previous ATT Collaboration meta-analyses.4,5,18 The 1994 meta-analysis examined the effects of antiplatelet therapy in diabetic patients by pooling data from 27 studies (n = 4,502) with patient-level information and found a 17% (95% CI: 6% to 27%) lower risk of vascular events compared to no therapy.4 The 2002 meta-analysis pooled data for 4,961 diabetic patients from nine studies and found that antiplatelet therapy was associated with a non-significant 7% (p = 0.35) lower risk of a vascular event.5 It is important to note, however, that both meta-analyses included regimens with aspirin, dipyridamole, picotamide, sulfinpyrazone, and ticlopidine in their definition of antiplatelet therapy.4,5 The 2002 meta-analysis also examined the effect of aspirin dose on risk of vascular events by combining data for 59,395 high risk patients from 65 studies.5 The risk of a vascular event was 19% (SD 3%) lower for patients taking 500–1500 mg daily, 26% (SD 3%) lower for patients taking 160–325 mg daily, and 32% (SD 6%) lower for patients taking 75–150 mg daily when compared to no therapy. The lowest dose group, <75 mg daily, was not associated with a significantly lower risk of vascular events compared to no therapy. It is important to note, however, that the effect of different aspirin doses was examined in all high risk patients, regardless of diabetes status. In our meta-analysis, we focused on aspirin monotherapy and used data from similar as well as more recent studies to explore the effect of dose on the association between aspirin use cardiovascular outcomes in diabetic patients alone.
Limitations
The major limitation of our meta-analysis, shared by others, is the paucity of available data on aspirin use in diabetes.17,19 Of particular relevance to our meta-analysis, we found only one study that randomly allocated patients to different aspirin doses.43 To maximize inclusion of potentially relevant articles, our pre-specified search strategy used six well-recognized, comprehensive electronic databases and database-appropriate terms designed to capture a wide range of comparative studies evaluating aspirin use in diabetes. Although we identified 47 studies meeting our inclusion criteria and successfully contacted authors of many of these studies, cardiovascular event data were available for 17,522 diabetic patients in 21 studies. This represents 77% of an estimated 22,697 diabetic patients enrolled in 47 studies meeting the inclusion criteria for our meta-analysis. The limited amount of data, especially from studies examining >100 mg daily, restricted our ability to contrast the effect of aspirin across different daily dosage groups and between primary and secondary prevention of cardiovascular disease.
A second limitation was the variation in study design and patient characteristics across included studies. These variations likely contributed to the heterogeneity observed in many of our analyses. We assumed a priori that study design, prevention strategy, and diabetes type would be potential sources of heterogeneity to investigate. Ideally, an individual-level meta-analysis would help minimize confounding from study design and patient characteristics.55 However, we were unable to conduct this type of analysis with the limited amount of available data and therefore our results must be interpreted with caution.
A third limitation is the short duration of follow-up in many of the studies included in this meta-analysis. With 8 of 21 studies following diabetic patients for ≤2 years, there may not have been enough events to reliably test our dose-response hypothesis.37,40,41,45–47,49,50
Last, our meta-analysis only examined the effectiveness of aspirin dose to prevent cardiovascular events. Although an examination of the risk of adverse events such as hemorrhagic stroke or gastrointestinal bleeding was beyond the scope of our study, this has been examined by others.32,33 Pooling the rates of bleeding events reported in 3133 and 5032 randomized controlled trials showed that the rate of major bleeding events was similar for <100 mg compared to 100–325 mg aspirin daily; however, the rate of any bleeding events was significantly lower for <100 mg compared to 100–325 mg aspirin daily.
CONCLUSIONS
Results of this meta-analysis neither confirm nor refute our hypothesis that the effect of aspirin to prevent cardiovascular events in diabetes varies according to daily dose. This hypothesis, generated from pharmacologic evidence of a dose-response relationship between aspirin and antiplatelet activity in diabetic patients,28 remains unanswered in a clinical setting. Although two on-going clinical trials—the Aspirin and Simvastatin Combination for Cardiovascular Events Prevention Trial in Diabetes (ACCEPT-D; International Standard Randomized Controlled Trial Number ISRCTN48110081), and A Study of Cardiovascular Events in Diabetes (ASCEND; ISRCTN60635500)—may help answer some questions regarding the role of aspirin in diabetes, both trials are using 100 mg of aspirin daily. We identified that very few diabetic patients have been included in randomized controlled trials examining 101–325 mg aspirin daily. Given that diabetes guideline recommendations include aspirin doses above 100 mg,1–3 we advocate the completion of clinical trials examining doses in this range. Currently there is very limited clinical evidence available to guide aspirin dose selection for prevention of cardiovascular events in diabetes.
Electronic Supplementary Materialsquery
Below is the link to the electronic supplementary material.
Acknowledgments
Contributors We are very grateful for the additional information provided by original study authors.We thank Angela Adams, Dr. Tomasz Hruczkowski, Dr. Raimar Löbenberg, Dr. Franco Pasutto, and Soleil Surette for their assistance during the article screening phase of our meta-analysis.We also thank Dr. Sumit Majumdar for providing comments on a draft of this manuscript.
Funding Sources Dr. Simpson is supported as a New Investigator by the Canadian Institutes of Health Research (CIHR). Mr. Gamble holds a Canada Graduate Scholarship from CIHR and a full-time Health Research Studentship from the Alberta Heritage Foundation for Medical Research (AHFMR).
Prior Presentations An abstract of this study was presented at the American Diabetes Association Scientific Sessions in June 2010.
Conflict of Interest Disclosure None disclosed.
Contributor Information
Scot H. Simpson, Phone: +1-780-4927538, FAX: +1-780-4921217, Email: ssimpson@pharmacy.ualberta.ca.
John-Michael Gamble, Email: jm.gamble@ualberta.ca.
Laurie Mereu, Email: laurie.mereu@ualberta.ca.
Thane Chambers, Email: thane.chambers@ualberta.ca.
References
- 1.Canadian Diabetes Association Clinical Practice Guidelines Expert Committee Vascular protection in people with diabetes. Can J Diabetes. 2008;32(suppl 1):S102–S106. [Google Scholar]
- 2.Buse JB, Ginsberg HN, Bakris GL, et al. Primary prevention of cardiovascular diseases in people with diabetes mellitus: a scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care. 2007;30(1):162–172. doi: 10.2337/dc07-9917. [DOI] [PubMed] [Google Scholar]
- 3.Ryden L, Standl E, Bartnik M, et al. Guidelines on diabetes, pre-diabetes, and cardiovascular diseases: executive summary. The Task Force on Diabetes and Cardiovascular Diseases of the European Society of Cardiology (ESC) and of the European Association for the Study of Diabetes (EASD) Eur Heart J. 2007;28(1):88–136. doi: 10.1093/eurheartj/ehm124. [DOI] [PubMed] [Google Scholar]
- 4.Collaborative overview of randomised trials of antiplatelet therapy--I: Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. Antiplatelet Trialists' Collaboration. BMJ 1994;308(6921):81–106. [PMC free article] [PubMed]
- 5.Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002;324(7329):71–86. [DOI] [PMC free article] [PubMed]
- 6.Final report on the aspirin component of the ongoing Physicians' Health Study. Steering Committee of the Physicians' Health Study Research Group. N Engl J Med 1989;321(3):129–135. [DOI] [PubMed]
- 7.Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet. 1998;351(9118):1755–1762. doi: 10.1016/S0140-6736(98)04311-6. [DOI] [PubMed] [Google Scholar]
- 8.Sacco M, Pellegrini F, Roncaglioni MC, Avanzini F, Tognoni G, Nicolucci A. Primary Prevention of Cardiovascular Events With Low-Dose Aspirin and Vitamin E in Type 2 Diabetic Patients: Results of the Primary Prevention Project (PPP) trial. Diabetes Care. 2003;26(12):3264–3272. doi: 10.2337/diacare.26.12.3264. [DOI] [PubMed] [Google Scholar]
- 9.Aspirin effects on mortality and morbidity in patients with diabetes mellitus. Early Treatment Diabetic Retinopathy Study report 14. ETDRS Investigators. JAMA 1992;268(10):1292–1300. [DOI] [PubMed]
- 10.Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001;285(19):2486–2497. [DOI] [PubMed]
- 11.Ogawa H, Nakayama M, Morimoto T, et al. Low-dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: a randomized controlled trial. JAMA. 2008;300(18):2134–2141. doi: 10.1001/jama.2008.623. [DOI] [PubMed] [Google Scholar]
- 12.Belch J, MacCuish A, Campbell I, et al. The prevention of progression of arterial disease and diabetes (POPADAD) trial: factorial randomised placebo controlled trial of aspirin and antioxidants in patients with diabetes and asymptomatic peripheral arterial disease. BMJ. 2008;337:a1840. doi: 10.1136/bmj.a1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Welin L, Wilhelmsen L, Bjornberg A, Oden A. Aspirin increases mortality in diabetic patients without cardiovascular disease: a Swedish record linkage study. Pharmacoepidemiol Drug Saf. 2009;18(12):1143–1149. doi: 10.1002/pds.1828. [DOI] [PubMed] [Google Scholar]
- 14.Leung WY, So WY, Stewart D, et al. Lack of benefits for prevention of cardiovascular disease with aspirin therapy in type 2 diabetic patients–a longitudinal observational study. Cardiovascular Diabetology. 2009;8:57. doi: 10.1186/1475-2840-8-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Colwell JA. Does aspirin use reduce cardiovascular risk in diabetes? Nat Rev Endocrinol. 2009;5(4):188–190. doi: 10.1038/nrendo.2009.44. [DOI] [PubMed] [Google Scholar]
- 16.Pignone M, Alberts MJ, Colwell JA, et al. Aspirin for primary prevention of cardiovascular events in people with diabetes. Diabetes Care. 2010;33(6):1395–1402. doi: 10.2337/dc10-0555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berardis G, Sacco M, Strippoli GF, et al. Aspirin for primary prevention of cardiovascular events in people with diabetes: meta-analysis of randomised controlled trials. BMJ. 2009;339:b4531. doi: 10.1136/bmj.b4531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baigent C, Blackwell L, Collins R, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet. 2009;373(9678):1849–1860. doi: 10.1016/S0140-6736(09)60503-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang C, Sun A, Zhang P, et al. Aspirin for primary prevention of cardiovascular events in patients with diabetes: A meta-analysis. Diabetes Res Clin Pract. 2010;87(2):211–218. doi: 10.1016/j.diabres.2009.09.029. [DOI] [PubMed] [Google Scholar]
- 20.Younis N, Williams S, Ammori B, Soran H. Role of aspirin in the primary prevention of cardiovascular disease in diabetes mellitus: a meta-analysis. Expert Opin Pharmacother. 2010;11(9):1459–1466. doi: 10.1517/14656561003792538. [DOI] [PubMed] [Google Scholar]
- 21.Stavrakis S, Stoner JA, Azar M, Wayangankar S, Thadani U. Low-dose aspirin for primary prevention of cardiovascular events in patients with diabetes: a meta-analysis. Am J Med Sci. 2011;341(1):1–9. doi: 10.1097/MAJ.0b013e3181f1fba8. [DOI] [PubMed] [Google Scholar]
- 22.Krasopoulos G, Brister SJ, Beattie WS, Buchanan MR. Aspirin "resistance" and risk of cardiovascular morbidity: systematic review and meta-analysis. BMJ. 2008;336(7637):195–198. doi: 10.1136/bmj.39430.529549.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tantry US, Mahla E, Gurbel PA. Aspirin resistance. Prog Cardiovasc Dis. 2009;52(2):141–152. doi: 10.1016/j.pcad.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 24.Ajjan R, Storey RF, Grant PJ. Aspirin resistance and diabetes mellitus. Diabetologia. 2008;51(3):385–390. doi: 10.1007/s00125-007-0898-3. [DOI] [PubMed] [Google Scholar]
- 25.Hovens MM, Snoep JD, Eikenboom JC, Bom JG, Mertens BJ, Huisman MV. Prevalence of persistent platelet reactivity despite use of aspirin: a systematic review. Am Heart J. 2007;153(2):175–181. doi: 10.1016/j.ahj.2006.10.040. [DOI] [PubMed] [Google Scholar]
- 26.Mehta SS, Silver RJ, Aaronson A, Abrahamson M, Goldfine AB. Comparison of aspirin resistance in type 1 versus type 2 diabetes mellitus. Am J Cardiol. 2006;97(4):567–570. doi: 10.1016/j.amjcard.2005.09.093. [DOI] [PubMed] [Google Scholar]
- 27.Fateh-Moghadam S, Plockinger U, Cabeza N, et al. Prevalence of aspirin resistance in patients with type 2 diabetes. Acta Diabetol. 2005;42(2):99–103. doi: 10.1007/s00592-005-0186-y. [DOI] [PubMed] [Google Scholar]
- 28.Dichiara J, Bliden KP, Tantry US, et al. The effect of aspirin dosing on platelet function in diabetic and nondiabetic patients: an analysis from the aspirin-induced platelet effect (ASPECT) study. Diabetes. 2007;56(12):3014–3019. doi: 10.2337/db07-0707. [DOI] [PubMed] [Google Scholar]
- 29.Law EH, Simpson SH. Aspirin use rates in diabetes: a systematic review and cross-sectional study. Can J Diabetes. 2010;34(3):211–217. [Google Scholar]
- 30.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 32.Serebruany VL, Malinin AI, Eisert RM, Sane DC. Risk of bleeding complications with antiplatelet agents: meta-analysis of 338,191 patients enrolled in 50 randomized controlled trials. Am J Hematol. 2004;75(1):40–47. doi: 10.1002/ajh.10451. [DOI] [PubMed] [Google Scholar]
- 33.Serebruany VL, Steinhubl SR, Berger PB, et al. Analysis of risk of bleeding complications after different doses of aspirin in 192,036 patients enrolled in 31 randomized controlled trials. Am J Cardiol. 2005;95(10):1218–1222. doi: 10.1016/j.amjcard.2005.01.049. [DOI] [PubMed] [Google Scholar]
- 34.Ray WA. Observational studies of drugs and mortality. N Engl J Med. 2005;353(22):2319–2321. doi: 10.1056/NEJMp058267. [DOI] [PubMed] [Google Scholar]
- 35.Morrish NJ, Wang SL, Stevens LK, Fuller JH, Keen H. Mortality and causes of death in the WHO Multinational Study of Vascular Disease in Diabetes. Diabetologia. 2001;44(Suppl 2):S14–S21. doi: 10.1007/PL00002934. [DOI] [PubMed] [Google Scholar]
- 36.Jansson SP, Andersson DK, Svardsudd K. Mortality trends in subjects with and without diabetes during 33 years of follow-up. Diabetes Care. 2010;33(3):551–556. doi: 10.2337/dc09-0680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Diener HC, Cunha L, Forbes C, Sivenius J, Smets P, Lowenthal A. European Stroke Prevention Study. 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci. 1996;143(1–2):1–13. doi: 10.1016/S0022-510X(96)00308-5. [DOI] [PubMed] [Google Scholar]
- 38.Ridker PM, Cook NR, Lee IM, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352(13):1293–1304. doi: 10.1056/NEJMoa050613. [DOI] [PubMed] [Google Scholar]
- 39.Swedish Aspirin Low-Dose Trial (SALT) of 75 mg aspirin as secondary prophylaxis after cerebrovascular ischaemic events. The SALT Collaborative Group. Lancet 1991;338(8779):1345–1349. [PubMed]
- 40.Petersen P, Boysen G, Godtfredsen J, Andersen ED, Andersen B. Placebo-controlled, randomised trial of warfarin and aspirin for prevention of thromboembolic complications in chronic atrial fibrillation. The Copenhagen AFASAK study. Lancet. 1989;1(8631):175–179. doi: 10.1016/S0140-6736(89)91200-2. [DOI] [PubMed] [Google Scholar]
- 41.Catalano M, Born G, Peto R. Prevention of serious vascular events by aspirin amongst patients with peripheral arterial disease: randomized, double-blind trial. J Intern Med. 2007;261(3):276–284. doi: 10.1111/j.1365-2796.2006.01763.x. [DOI] [PubMed] [Google Scholar]
- 42.Fowkes FG, Price JF, Stewart MC, et al. Aspirin for prevention of cardiovascular events in a general population screened for a low ankle brachial index: a randomized controlled trial. JAMA. 2010;303(9):841–848. doi: 10.1001/jama.2010.221. [DOI] [PubMed] [Google Scholar]
- 43.Farrell B, Godwin J, Richards S, Warlow C. The United Kingdom transient ischaemic attack (UK-TIA) aspirin trial: final results. J Neurol Neurosurg Psychiatry. 1991;54(12):1044–1054. doi: 10.1136/jnnp.54.12.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Peto R, Gray R, Collins R, et al. Randomised trial of prophylactic daily aspirin in British male doctors. Br Med J (Clin Res Ed) 1988;296(6618):313–316. doi: 10.1136/bmj.296.6618.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Elwood PC, Sweetnam PM. Aspirin and secondary mortality after myocardial infarction. Lancet. 1979;2(8156–8157):1313–1315. doi: 10.1016/S0140-6736(79)92808-3. [DOI] [PubMed] [Google Scholar]
- 46.Aspirin in coronary heart disease The Coronary Drug Project Research Group. J Chronic Dis. 1976;29(10):625–642. doi: 10.1016/0021-9681(76)90020-5. [DOI] [PubMed] [Google Scholar]
- 47.Cairns JA, Gent M, Singer J, et al. Aspirin, sulfinpyrazone, or both in unstable angina. Results of a Canadian multicenter trial. N Engl J Med. 1985;313(22):1369–1375. doi: 10.1056/NEJM198511283132201. [DOI] [PubMed] [Google Scholar]
- 48.Feringa HH, Bax JJ, Karagiannis SE, et al. Elderly patients undergoing major vascular surgery: risk factors and medication associated with risk reduction. Arch Gerontol Geriatr. 2009;48(1):116–120. doi: 10.1016/j.archger.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 49.McAlister FA, Ghali WA, Gong Y, Fang J, Armstrong PW, Tu JV. Aspirin use and outcomes in a community-based cohort of 7352 patients discharged after first hospitalization for heart failure. Circulation. 2006;113(22):2572–2578. doi: 10.1161/CIRCULATIONAHA.105.602136. [DOI] [PubMed] [Google Scholar]
- 50.Cubbon RM, Gale CP, Rajwani A, et al. Aspirin and mortality in patients with diabetes sustaining acute coronary syndrome. Diabetes Care. 2008;31(2):363–365. doi: 10.2337/dc07-1745. [DOI] [PubMed] [Google Scholar]
- 51.Ong G, Davis TM, Davis WA. Aspirin is associated with reduced cardiovascular and all-cause mortality in type 2 diabetes in a primary prevention setting: the Fremantle Diabetes study. Diabetes Care. 2010;33(2):317–321. doi: 10.2337/dc09-1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zanchetti A. Aspirin and Antiplatelet Drugs in the Prevention of Cardiovascular Complications of Diabetes. In: Morgensen CE, editor. Pharmacotherapy of diabetes: new developments. New York: Springer; 2007. pp. 211–218. [Google Scholar]
- 53.Cochrane Handbook for Systematic Reviews of Interventions. 5.0.2 [updated September 2009] ed. The Cochrane Collaboration; 2008.
- 54.Thrombosis prevention trial: randomised trial of low-intensity oral anticoagulation with warfarin and low-dose aspirin in the primary prevention of ischaemic heart disease in men at increased risk. The Medical Research Council's General Practice Research Framework. Lancet 1998;351(9098):233–241. [PubMed]
- 55.Lambert PC, Sutton AJ, Abrams KR, Jones DR. A comparison of summary patient-level covariates in meta-regression with individual patient data meta-analysis. J Clin Epidemiol. 2002;55(1):86–94. doi: 10.1016/S0895-4356(01)00414-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Below is the link to the electronic supplementary material.