Abstract
BACKGROUND
Hospitals face increased pressure to improve their quality of care in an environment of dwindling hospital payments. It is unclear whether lower hospital margins are associated with worse quality of care or closure.
OBJECTIVE
To determine the association of hospital margins with quality of care and changes in operating status.
DESIGN, SUBJECTS, AND MAIN MEASURES
We conducted an observational cross-sectional study analyzing hospitals’ margin, quality of care (process quality, risk-adjusted readmission rates, and risk-adjusted mortality rates), and changes in operating status (rates of closure, merger and acquisition, and conversion to a critical access hospital) for 3,262 non-public U.S. hospitals with data from the Hospital Quality Alliance and Medicare Cost Reports.
KEY RESULTS
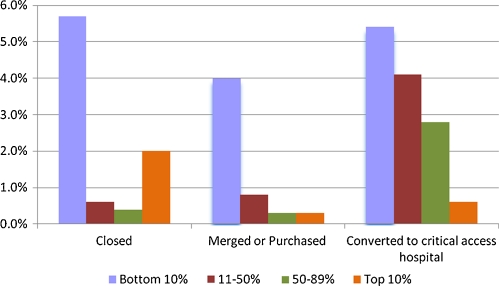
Compared to those in the bottom 10% of operating margin, those in the top 10% had higher process quality (e.g. 95.3 vs. 93.7, p = 0.002 for acute myocardial infarction [AMI]) and lower readmission rates (e.g. 19.7% vs. 22.4%, p < 0.001 for AMI). We found no association between margins and mortality rates. Hospitals in the bottom 10% were more likely than those in the top 10% to close (5.7% vs. 2.0%), merge or become acquired (4.0% vs. 0.3%), or convert to a Critical Access Hospital (5.4% vs. 0.6%). Over 15% of hospitals in the lowest decile of hospital margin changed operating status in the subsequent year.
CONCLUSIONS
Low hospital margins are associated with worse processes of care and readmission rates and with changes in operating status. We should monitor low-margin hospitals closely for declining quality of care.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-011-1815-5) contains supplementary material, which is available to authorized users.
KEY WORDS: margins, quality, closure
INTRODUCTION
These are challenging times for hospitals. Increasing competition among private sector payers has resulted in increasing fiscal pressure on hospitals.1 Medicare has slowed the increase in hospital payments and now covers only 93% of patient costs.2 At the same time, there is ever increasing interest in holding hospitals accountable for high quality care.3
For many hospitals, increasing financial pressures may result in lower margins that conflict with efforts to promote higher quality care. Funding for nursing services and important quality improvement programs may fall short. At the extreme, financial pressures might lead to closure or other changes in operating status.
In spite of the importance of this issue, surprisingly few studies have examined the association between hospital margin and quality of care, perhaps because national metrics on quality have only become available recently. Prior studies that have examined this association have either focused on patient safety or quality of care for a single condition (acute myocardial infarction).4–6 Data on margins and hospital closure are similarly lacking: we are aware of only two prior studies and they focused on patterns of care in the 1980s.7,8
In this study, we used national data on inpatient care to answer four questions. First, how does margin vary across hospitals and what hospital characteristics are associated with high and low hospital margins? Second, are hospitals’ margins consistent across time? Third, do low margin hospitals have lower quality of care? And finally, are low margin hospital more likely to subsequently change their operating status through closures, mergers or acquisition, or conversion to a Critical Access Hospital (CAH)?
METHODS
Data on Margin and Hospital Characteristics
We used data from Medicare Cost Reports to calculate hospital operating margins. We used hospital operating margin because it is the most commonly used measure of hospital financial performance,4,5 but we repeated our analyses for total margin and present these results in the Appendix (available online). Consistent with prior literature, we defined operating margin as net revenues from patient care and other operations (such as pharmacy, meal service, and parking lot receipts) minus total operating expenses divided by net revenues from patient care and other operations.9 Cost report data have been used by the Medicare Payment Advisory Committee (MedPAC) and others to calculate hospitals' margins.6,10 Nevertheless to reduce any concerns about the quality of data from the Cost Reports, we “winsorized” measures of operating margin (setting all outliers beyond the 2.5 percentile and 97.5 percentile to the values at these percentiles)11 to ensure that these outliers did not unduly affect our results. We also examined total margin defined as net income divided by total revenues.12 From an initial sample of 6,086 hospitals from the 2006 Medicare Cost Reports, we dropped 557 hospitals with incorrectly submitted cost reports, 1,148 hospitals listed in the American Hospital Association (AHA) annual survey as caring for other than medical and surgical patients, and 1,119 public hospitals, leaving a sample of 3,262 private for-profit and not-for-profit hospitals. We dropped public hospitals because they have different funding sources and a different mission than private hospitals.13
We linked Cost Report data from 2004, 2005, and 2006 to the 2007 American Hospital Association annual survey, which provides information on hospital characteristics such as U.S. census region in which they are located, ownership, teaching status, urban vs. rural location, and presence or absence of a medical intensive care unit (MICU) or coronary care unit (CCU). Finally we linked these data sets to data from the Hospitals Quality Alliance (HQA), which provides data on quality of care (see below).
Process Quality of Care
We used the September 2008 release of the HQA database, which provided data on the care of patients discharged from U.S. hospitals during 2007. For each hospital, we calculated a summary performance indicator score for acute myocardial infarction (AMI), congestive heart failure (CHF), and pneumonia. There were eight performance indicators for AMI, four performance indicators for CHF, and seven performance indicators for pneumonia. The full set of performance indicators are listed in Appendix Table 1 (available online). To create summary performance indicator scores, we used the methods recommended by the Joint Commission.14 Under this approach, the summary performance indicator score is the number of times a hospital performed the appropriate action across all measures for that condition divided by the number of opportunities the hospital had to provide appropriate care for that condition. Summary performance indicator scores were not calculated if a hospital did not have at least 30 patients for at least one of the measures for each condition.
Readmission Rates
We used 2007 Medicare Provider Analysis and Review (MedPAR) 100% files, which contain hospitalization data for all Medicare fee-for-service enrollees, and we examined hospitalizations with the primary discharge diagnoses of AMI, CHF, or pneumonia. We followed the CMS methodology for classifying “index admissions;” as a result, patients could be included in the sample more than once.15 Based on recommendations from the Joint Commission, we excluded hospitals with fewer than 25 discharges for Medicare patients for each condition.16 We calculated all-cause readmission within 30 days of discharge. Each patient’s likelihood of readmission was adjusted for patient characteristics using the Elixhauser comorbidity adjustment scheme, with adjustment for age, sex, race/ethnicity, and the presence or absence of up to 29 coexisting conditions.17
Mortality Rates
We used 2007 MedPAR 100% files to calculate 30-day mortality rates for AMI, CHF, and pneumonia. The rates were risk-adjusted for age, sex, race/ethnicity, and the presence or absence of the 29 comorbid conditions in the Elixhauser scheme.
Rates of Closure, Mergers and Acquisitions, and Conversion to Critical Access Hospital
To determine rates of closure, merger and acquisition, and conversion to a Critical Access Hospital (CAH) in relation to hospital margins, we examined hospital margins in 2004 and identified those hospitals that submitted a Cost Report in 2004 but either did not submit a Cost Report in 2006 (indicating that the hospital no longer existed by the beginning of 2006) or changed hospital provider number prior to 2006. We confirmed all instances of an apparent change in operating status by contacting administrators of these hospitals; and if we could not reach them (usually the case with closure), we contacted administrators at nearby hospitals to ascertain this information. Critical Access Hospitals are small (<26 beds), rural hospitals designated to receive cost-based reimbursement (rather than prospective payment based on patients’ diagnosis related groups) intended to improve that hospital’s financial performance and reduce the likelihood of that hospital closing.18 Prior studies have shown that hospitals that convert to a CAH have an increase in hospital margins.19
Statistical Analysis
We used a combination of chi-square tests and linear regression models to compare the structural characteristics of hospitals by operating margin (bottom 10%, 11th to 50th percentile, 51st to 89th percentile, and top 10% of operating margins). We used this categorization so we could focus on hospitals that were in financial duress and those that were financially well-off while examining the whole spectrum of financial performance.
We assessed the consistency of hospitals’ operating margins over time by calculating the correlation of a hospital’s operating margin in 2004 with its operating margin in 2005 and 2006. We made similar calculations for total margin. We also determined whether hospitals categorized in a specific operating margin quartile in 2004 were so categorized in 2005 and 2006. Finally, we examined the correlation between hospitals’ operating margin and total margin in a given year.
To examine the association between a hospital’s operating margin and its quality of care, we created a set of regression models using the quality metric of interest (e.g. process quality) as the outcome and operating margin as the continuous main predictor, adjusting for hospital characteristics we posited, a priori, might be potential confounders, including size, profit status, location (urban versus rural), teaching status (member of the Council of Teaching Hospitals or not), the presence of a MICU, the presence of a CCU, the percentage of patients who had Medicare insurance, the percentage of patients with Medicaid insurance, and region of the county. In sensitivity analyses, we further adjusted for nurse-census ratio, which was calculated by dividing the number of full-time nurses by 1,000 patient days. We used quality metrics from 2007 and operating margins from 2006 because we hypothesized that a hospital’s financial situation in a given year would affect its quality of care in the following year.
Finally, we calculated rates of closure, merger or acquisition, or conversion to a CAH by the above categorization of operating margin (and total margin, again in the Appendix [available online]). All analyses were conducted using STATA 10.0 and used robust standard errors to adjust for heterogeneity.
RESULTS
Operating margins in 2006 ranged from −23.7% to +25.0%, with a median of 2.1% and an interquartile range of −2.7% to +7.1%. There were substantial statistically significant differences in the characteristics of hospitals by margin, although the patterns were not always monotonic (Table 1). Compared to other hospitals, those with low margins were less likely to be in the West, more likely to be small or teaching, less likely to be urban, and less likely to have a CCU or MICU. Hospitals with low margins also had higher proportions of Medicare and black patients.
Table 1.
Hospital Characteristics by Operating Margin in 2006
| Operating Margina | Total sample | Bottom 10% | 11–50% | 51%–89% | Top 10% | p-value |
|---|---|---|---|---|---|---|
| 2.1 (−23.7 to 25.0) | −15.5 (−23.7 to −9.0) | −1.3 (−8.9 to 2.1) | 5.9 (2.1 to 14.3) | 19.5 (14.3 to 25.0) | ||
| Total Margina | 4.3 (−17.3 to 24.3) | −9.5 (−17.3 to 17.7) | 1.0 (−17.3 to 24.3) | 7.4 (−17.3 to 24.3) | 17.8 (−17.3 to 24.3) | |
| Region | ||||||
| Northeast | 16% | 14% | 24% | 13% | 3.4% | p < 0.001 |
| Midwest | 30% | 23% | 29% | 34% | 25% | |
| South | 36% | 48% | 32% | 34% | 50% | |
| West | 17% | 14% | 15% | 19% | 21% | |
| Size | ||||||
| Small | 41% | 54% | 41% | 38% | 43% | p < 0.001 |
| Medium | 48% | 38% | 49% | 49% | 49% | |
| Large | 11% | 7.7% | 10% | 13% | 8.3% | |
| Profit Status | ||||||
| For-profit | 21% | 34% | 14% | 16% | 54% | p < 0.001 |
| Private non-profit | 79% | 66% | 86% | 84% | 46% | |
| Urban | 81% | 75% | 79% | 82% | 91% | p < 0.001 |
| Teaching | 6.0% | 7.1% | 5.2% | 7.1% | 3.4% | p = 0.61 |
| CCU | 35% | 21% | 34% | 40% | 32% | p < 0.001 |
| MICU | 70% | 52% | 69% | 75% | 69% | p < 0.001 |
| Percent Medicare | 48% | 50% | 50% | 47% | 45% | p < 0.001 |
| Percent Medicaid | 16% | 16% | 16% | 16% | 16% | p = 0.65 |
| Nurse ratio | 7.0 | 6.9 | 6.5 | 7.2 | 7.9 | p < 0.001 |
| Proportion of black patients | 7.7% | 13% | 7.9% | 6.4% | 7.0% | p < 0.001 |
a Median listed along with the range in parentheses
Source of Information: 2006 Medicare Cost Reports, 2007 MedPAR data, and 2007 annual survey of the American Hospital Association
Notes: CCU is cardiac care unit. MICU is medical intensive care unit. Percent Medicare and percent Medicaid refer to the percentage of patients with each type of insurance, respectively. Nurse–staffing ratio is per 1,000 patient days. P-values refer to the statistical significance of chi-squared tests or simple linear regressions, as appropriate, for hospital characteristics across the categories of operating margin. The number of hospitals in the sample was 3,262
Consistency of Margin Over Time
Hospitals’ operating margins were moderately stable over time. The year-to-year correlations for a hospital’s operating margin were 0.63 between 2004 and 2006, 0.75 between 2004 and 2005, and 0.74 between 2005 and 2006. Similarly, the year-to-year correlations for a hospital’s total margin were 0.59 between 2004 and 2006, 0.70 between 2004 and 2005, and 0.72 between 2005 and 2006. When we categorized hospitals into quartiles of operating margin, hospital rankings were fairly stable: 66% of hospitals in the bottom quartile in 2004 were still in the bottom quartile in 2005, and 90% were still in the lower half of operating margin (Table 2). The correlation of operating margin and total margin in 2006 was 0.81.
Table 2.
Stability Over Time of Operating Margin Between 2004 and 2006a
| 2005 | 2006 | |||||||
|---|---|---|---|---|---|---|---|---|
| 2004 | Q1 Low Margin | Q2 | Q3 | Q4 High Margin | Q1 Low Margin | Q2 | Q3 | Q4 High Margin |
| Q1 Low Margin | 66% | 21% | 7.2% | 3.8% | 54% | 21% | 11% | 5.2% |
| Q2 | 24% | 51% | 21% | 4.9% | 26% | 46% | 26% | 9.8% |
| Q3 | 6.3% | 24% | 54% | 17% | 13% | 25% | 48% | 25% |
| Q4 High Margin | 4.0% | 5.3% | 17% | 75% | 6.4% | 8.7% | 15% | 60% |
aStability refers to hospitals that remained in the same quartile of operating margin or moved to an adjacent quartile over time
Source of Information: 2004, 2005, and 2006 Medicare Cost Reports
Notes: The sample of non-public hospitals caring for medical and surgical patients that submitted Medicare Cost Reports in both 2004 and 2005 was 3,279. The sample of non-public hospitals caring for medical and surgical patients that submitted Medicare Cost Reports in both 2004 and 2006 was 2,780
Operating Margin and Quality of Care
We found a consistent, although small, relationship between operating margin and process quality of care (Table 3). For example, those hospitals in the bottom 10% of operating margin had a CHF HQA summary score of 82.3, while those in the top 10% had a summary score of 87.0 (p = 0.006). Similarly, those in the bottom 10% of operating margin had a pneumonia HQA summary score of 88.5, while those in the top 10% had a summary score of 92.0 (p < 0.001).
Table 3.
The Association of Operating Margin and Performance on Process Indicators, Risk-Adjusted Readmissions, and Risk Adjusted Mortality Rates
| Bottom 10% (Low Margins) | 11–50% | 51%–89% | Top 10% (High Margins) | p-value | |
|---|---|---|---|---|---|
| Process Indicators of Quality (%) | |||||
| AMI HQA summary score (N = 1,718) | 93.7 | 94.7 | 95.2 | 95.3 | p = 0.002 |
| CHF HQA summary score (N = 2,602) | 82.3 | 85.4 | 86.3 | 87.0 | p < 0.001 |
| Pneumonia HQA summary score (N = 2,767) | 88.5 | 90.2 | 91.0 | 92.0 | p < 0.001 |
| Risk-adjusted 30-day readmission rates (%) | |||||
| AMI readmission rate (N = 1,818) | 22.4 | 22.1 | 21.0 | 19.7 | p < 0.001 |
| CHF readmission rate (N = 2,674) | 27.5 | 26.3 | 25.4 | 24.5 | p < 0.001 |
| Pneumonia readmission rate (N = 2,865) | 22.4 | 20.1 | 19.6 | 18.8 | p < 0.001 |
| Risk-adjusted 30-day mortality rates (%) | |||||
| AMI mortality rate (N = 3,023) | 17.3 | 17.5 | 17.9 | 16.0 | p = 0.88 |
| CHF mortality rate (N = 3,167) | 10.3 | 10.8 | 11.4 | 10.4 | p = 0.09 |
| Pneumonia mortality rate (N = 3,183) | 11.2 | 11.6 | 11.4 | 10.7 | p = 0.84 |
Source of Information: 2006 Medicare Cost Reports, 2007 MedPAR data, and 2007 annual survey of the American Hospital Association
Notes: Models adjusted for hospital size, profit and ownership status, location (urban or rural), teaching status (member of COTH versus not), the presence or absence of a medical intensive care unit or cardiac care unit, the percentage of patients who had Medicare, the percentage of patients who had Medicaid, and region in the country (Northeast, Midwest, South, West). P-values refer to the statistical significance of the coefficient on operating margin. Summary performance indicator scores for HQA measures were not calculated if a hospital did not have at least 30 patients for at least one of the measures for each condition. Readmission rates were not calculated if a hospital had fewer than 25 discharges for Medicare patients for each condition
We also found a consistent relationship between operating margin and readmission rates (Table 3). For example, those in the bottom 10% of operating margin had an 30-day AMI readmission rate of 22.4%, while those in the top 10% of operating margin had a 30-day AMI readmission rate of 19.7% (p = 0.001). Similarly, those in the bottom 10% of operating margin had a 30-day CHF readmission rate of 27.5% while those in the top 10% had a 30-day CHF readmission rate of 24.5% (p < 0.001).
We found a small and inconsistent relationship between operating margin and mortality rates (Table 3). Hospitals with low operating margins had 30-day mortality rates that were comparable to those hospitals with high operating margins.
When we further adjusted for nurse-census ratio, our results remained essentially unchanged (data not shown). The coefficients for the analysis of quality of care are in the appendix, Table 2 (available online).
Operating Margin and Change in Operating Status
We found a consistent relationship between low operating margin in 2004 and rates of closure, merger and acquisition, and conversion to a Critical Access Hospital in 2005 (Fig. 1). Those in the bottom 10% of operating margin were substantially more likely than those in the top 10% to close (5.7% vs. 2.0%, p = 0.01), merge or become acquired (4.0% vs. 0.3%, p < 0.001), or convert to a CAH (5.4% vs. 0.6%, p < 0.001). Similarly, when comparing those in the bottom 10% of operating margin to the rest of the hospitals as a whole, those in the bottom 10% were more likely to close (5.7% vs. 0.6%, p < 0.001), merge or become acquired (4.0% vs. 0.5%, p < 0.001), or convert to a CAH (5.4% vs. 3.1%, p = 0.03). Overall, over 15% of hospitals in the lowest decile of hospital margins changed operating status in the subsequent year.
Figure 1.
The Association of Operating Margin in 2004 and Rates of Closure, Merger/Acquisition, or Conversion to a Critical Access Hospital in 2005. Source of Information: Authors’ analysis of Medicare Cost Reports. Notes: The sample of non-public hospitals caring for medical and surgical patients that submitted Medicare Cost Reports in 2004 was 3,514.
Total Margin, Quality of Care and Change in Operating Status
We examined the association between hospitals’ total margin and quality of care and change in operating status and generally found similar relations as we did for operating margin (Appendix, Table 3 and Figure 1 [available online]), although there were minor differences for the relation between total margin and process quality for CHF and for conversion to a CAH.
DISCUSSION
Our study has three key findings. First, operating margins varied substantially across hospitals, although they were relatively stable from year to year. Second, lower margins are associated with lower quality of care as measured by process metrics and risk-adjusted readmission rates. Third, we found that hospitals with low margins were much more likely to close, merge, become acquired, or convert to a Critical Access Hospital.
The familiar maxim “no margin, no mission” would suggest that our findings may be causal. For example, fiscally-strapped hospitals hire fewer nurses and may not be able to afford substantial investment in quality improvement efforts. Hospitals with low margins more often are located in rural areas and serve more Medicare patients and black patients—segments of the population that may have greater service needs and be at increased risk of lower quality care.20–22 Therefore, shortfalls in services and in investments in quality improvement due to low margins may have a particularly acute impact on hospital quality performance. On the other hand, our results may not be completely causal; factors such as ineffective management may result in both poor financial performance and poor quality of care and thus be partially responsible for the associations that we observed. It is also theoretically possible that the causal relationship could occur in reverse; that is, low quality care may lead to lower margins as those patients with better-paying insurance leave. However, prior studies have not shown that publicly reporting quality of care has much impact on patients' choice of hospital.3,23 Poor quality of care may also lead to lower margins through delayed recovery and uncompensated complications of care. In addition, we find that margins are associated with process quality and readmission rates, but not with mortality rates. It may be that hospitals with higher margins are better able to invest in efforts to improve process quality or transitional care that leads to lower readmission rates, but that reducing mortality rates is more difficult.
Given the realities of the marketplace, it makes sense that hospitals with substantially negative margins are more likely to close or enter into new ownership relationships through merger and acquisition. The magnitude of these changes in operating status is notable at the extremes; we found that over 15% of the hospitals in the lowest decile of margin changed operating status in the subsequent year. At the same time, it seems surprising that the majority of hospitals with very low and negative margins are able to continue on. Our findings are consistent with observations by Duffy and Friedman using data from the early 1980s. They speculated that many of the negative margin hospitals might have sponsors such as local government, universities, or multi-hospital systems that provide non-operating transfers, income from grants, loan forgiveness, or other omissions from typical accounting reports.8 However, these sources of revenue would be captured in our measure of total margin.
There have been few prior studies of the relationship between hospital margins and quality of care. Both Encinosa and Bernard4 and Bazzoli et al.5 studied the effect of hospital margin on patient safety, but they reached contrary results. Encinosa and Bernard examined hospitals in Florida and found an association between lower margin and more frequent patient safety events, while Bazzoli et al studied hospitals in eleven states and found no impact. Volpp et al.6 used a sample of approximately 200 hospitals to examine the effect of the Balanced Budget Act of 1997 on quality of care for AMI and found that hospital margins became smaller over time but there was no change in process quality or mortality. Our study is the first to use a national sample of hospitals and a broad array of quality metrics. Our results on closure are consistent with findings from the 1980s by Williams et al.7 and Duffy and Friedman.8 We used more recent data and examined merger and acquisition and conversion to a Critical Access Hospital in addition to closure.
Our study has several limitations. The data on hospital costs come from the Medicare Cost Reports. While they are widely used by groups such as MedPAC, these reports are not uniformly audited, so their accuracy may be limited. We could only identify an association between margin and quality and cannot be sure of causality. Readmission and mortality rates are based on Medicare patients only; however, the elderly make up nearly half of all hospitalized medical and surgical patients. Our process quality measures were limited to three conditions, the magnitude of the differences we found was relatively small, and improvements in one dimension of quality (i.e. process quality) may not translate to other dimensions (i.e. mortality). Our data were cross sectional and we did not directly test the hypothesis that changes in margin lead to changes in quality. Finally, we had limited ability to adjust for case mix using claims.
In summary, we found large variations in operating margins, a closely watched marker of financial health, across U.S. hospitals. Low margin hospitals provide lower quality of care and were much more likely to subsequently close, merge, become acquired, or convert to a Critical Access Hospital. These observations argue for continuing efforts to monitor hospital margin closely. As legislators increasingly push to reduce the costs of the U.S. health care system by lowering hospital reimbursement rates, they need to ensure that these efforts do not adversely impact quality of care and access.
Acknowledgments
We would like to acknowledge George H. Pink for his help with calculating the hospital margins.
Funding None disclosed.
Conflicts of Interest None disclosed.
Online Appendix
Below is the link to the electronic supplementary material.
Hospital Quality Alliance Performance Measures for Acute Myocardial Infarction, Congestive Heart Failure, and Pneumonia in 2007 (DOC 31 kb)
The Association of Operating Margin and Performance on Process Indicators, Risk Adjusted Readmissions, and Risk Adjusted Mortality Rates: Coefficients on Operating Margin (DOC 34 kb)
The Association of Total Margin and Quality Performance Measured by Process Indicators, Risk Adjusted 30-day Readmissions, and Risk Adjusted 30-day Mortality (DOC 21.0 kb)
The Association of Total Margin and Rates of Closure, Merger/Acquisition, or Conversion to a Critical Access Hospital in 2005 (DOC 52 kb)
References
- 1.A data book: Healthcare spending and the Medicare program. Washington: MedPAC; 2005. [Google Scholar]
- 2.Medicare Payment Advisory Commission (MedPAC). Report to the Congress: Medicare payment policy. Available at: http://www.medpac.gov/documents/Mar10_EntireReport.pdf. Accessed July 20, 2011.
- 3.Hibbard JH, Stockard J, Tusler M. Hospital performance reports: impact on quality, market share, and reputation. Health Aff (Millwood) 2005;24:1150–1160. doi: 10.1377/hlthaff.24.4.1150. [DOI] [PubMed] [Google Scholar]
- 4.Encinosa WE, Bernard DM. Hospital finances and patient safety outcomes. Inquiry. 2005;42:60–72. doi: 10.5034/inquiryjrnl_42.1.60. [DOI] [PubMed] [Google Scholar]
- 5.Bazzoli GJ, Chen HF, Zhao M, et al. Hospital financial condition and the quality of patient care. Health Econ. 2008;17:977–995. doi: 10.1002/hec.1311. [DOI] [PubMed] [Google Scholar]
- 6.Volpp KG, Konetzka RT, Zhu J, et al. Effect of cuts in Medicare reimbursement on process and outcome of care for acute myocardial infarction patients. Circulation. 2005;112:2268–2275. doi: 10.1161/CIRCULATIONAHA.105.534164. [DOI] [PubMed] [Google Scholar]
- 7.Williams D, Hadley J, Pettengill J. Profits, community role, and hospital closure: an urban and rural analysis. Med Care. 1992;30:174–187. doi: 10.1097/00005650-199202000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Duffy SQ, Friedman B. Hospitals with chronic financial losses: what came next? Health Aff (Millwood) 1993;12:151–163. doi: 10.1377/hlthaff.12.2.151. [DOI] [PubMed] [Google Scholar]
- 9.Pink GH, Howard A, Holmes GM, et al. Differences in measurement of operating margin. Available at: http://flexmonitoring.org/documents/BriefingPaper17_OperatingMargin.pdf. Accessed July 20, 2011.
- 10.Hackbarth GM. Report to the Congress: Medicare payment policy. Available at: http://www.medpac.gov/documents/Mar09_March%20report%20testimony_WM%20FINAL.pdf. Accessed July 20, 2011.
- 11.Angrist JD, Krueger AB. Empirical strategies in labor economics. In: Card D, Ashenfelter O, eds. Handbook of labor economics: Elsevier Science; 2000.
- 12.Pink GH, Holmes GM, D'Alpe C, et al. Financial indicators for Critical Access Hospitals. Available at: http://www.flexmonitoring.org/documents/BriefingPaper7_FinancialIndicators.pdf. Accessed July 20, 2011. [DOI] [PubMed]
- 13.Anderson RJ, Boumbulian PJ, Pickens SS. The role of U.S. public hospitals in urban health. Acad Med. 2004;79:1162–1168. doi: 10.1097/00001888-200412000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Kahn CN, 3rd, Ault T, Isenstein H, et al. Snapshot of hospital quality reporting and pay-for-performance under Medicare. Health Aff (Millwood) 2006;25:148–162. doi: 10.1377/hlthaff.25.1.148. [DOI] [PubMed] [Google Scholar]
- 15.Bernheim SM, Lin Z, Bhat KR, et al. 2010 measures maintenance technical report: Acute myocardial infarction, heart failure, and pneumonia 30-Day risk-standardized readmission measures. Available at: http://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1219069855841. Accessed July 20, 2011.
- 16.The Joint Commission. Population and sampling specifications. Available at: http://manual.jointcommission.org/releases/TJC2010A/SamplingChapterTJC.html. Accessed July 20, 2011.
- 17.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Rural Assistance Center. CAH frequently asked questions. Available at: http://www.raconline.org/info_guides/hospitals/cahfaq.php#whatis. Accessed July 20, 2011.
- 19.Schoenman JA, Sutton JP. Impact of CAH conversion on hospital finances and mix of inpatient services. Available at: http://www.norc.org/NR/rdonlyres/A91D9471-49FD-4881-994F-51DACEBC7577/0/ImpactofCAHConversion_FinalReport_NORC.pdf. Accessed July 20, 2011.
- 20.Sheikh K, Bullock C. Urban-rural differences in the quality of care for Medicare patients with acute myocardial infarction. Arch Intern Med. 2001;161:737–743. doi: 10.1001/archinte.161.5.737. [DOI] [PubMed] [Google Scholar]
- 21.Baldwin LM, MacLehose RF, Hart LG, et al. Quality of care for acute myocardial infarction in rural and urban US hospitals. J Rural Health. 2004;20:99–108. doi: 10.1111/j.1748-0361.2004.tb00015.x. [DOI] [PubMed] [Google Scholar]
- 22.Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington: National Academy Press; 2003. [PubMed] [Google Scholar]
- 23.Jha AK, Epstein AM. The predictive accuracy of the New York State coronary artery bypass surgery report-card system. Health Aff (Millwood) 2006;25:844–855. doi: 10.1377/hlthaff.25.3.844. [DOI] [PubMed] [Google Scholar]