Abstract
Objective
Individuals with serious mental illness (SMI: e.g., schizophrenia, bipolar disorder) experience disparities in mortality relative tothe general population, mainly because of medical conditions (i.e., cardiometabolic disease).We assessed whether VA patients with SMI and receiving care from VA mental health facilities with colocated medical care were more likely to receive cardiometabolic risk assessments in accordance with clinical practice guidelines than patients from non-colocated facilities.
Methods
Patients with SMI identified prescribed second-generation antipsychotic medications in fiscal year (FY) 2007receiving care from VA mental health facilities completing the VA Mental Health Program Surveywere included. VA administrative data were ascertained to assess receipt of the following tests every 6 months in FY 2007: BMI, blood pressure, lipid profile, and fasting glucose.
Results
Out of 40,600 patients with SMI prescribed second-generation antipsychotics, 29% received all cardiometabolic tests (lipid, glucose, BMI and blood pressure). While 79% and 76% received blood pressure and BMI assessments, respectively, only 37% received a lipid test. Patients from colocated sites were more likely to receive all cardiometabolic tests (OR=1.26, 95% CI: 1.18–1.35, p<0.001).
Conclusions
Colocated general medical providers in mental health clinicsare more likely to provide cardiometabolic assessments for patients with SMI prescribed second-generation antipsychotics.
Keywords: Mental disorders, quality of care, cardiovascular disease, integrated care
INTRODUCTION
Individuals with serious mental illness (SMI) have shortened life expectancies relative to the general population[1–2]. Observed disparities in mortality are chiefly attributable to a disproportionate burden of medical conditions, notably cardiovascular disease among patients with SMI [3–5]. Patients with SMI also experience elevated rates of cardiometabolic factors, including high cholesterol, obesity, andpoor glycemic control [6].
Second-generation antipsychotics(SGAs) have been associated with increased cardiometabolic risk factorsincluding elevated glucose and weight gain[4]. In response, the American Diabetes and American Psychiatric Associations published guidelines for the appropriate screening of cardiometabolic risk factors, including BMI, lipids, blood pressure, and fasting glucose assessment[7]. However,patients with SMI are less likely to be assessed for cardiometabolic risk factors than those without SMI[6,8].These gaps in quality have been attributed to fragmentation of physical and mental health services[9–10].
Colocation of primary services in the mental health setting may reduce barriers tomedical care among those with SMI, including appropriate cardiometabolic monitoring [11]. Prior randomized controlled trials of integrated care models primarily focused on colocating medical providers in mental health clinics, and were associated with improved access to care for patients with SMI[12–13]. However, the extent to which colocated general medical services (i.e., medical care providers embedded in mental health clinics) in usual practice improve rates of cardiometabolic screening has not been demonstrated. The purpose of this study is to determine the association between colocation of medical and psychiatric services and receipt of cardiometabolic screeningin a nationwide sample of Veterans with SMI.
METHODS
This cross-sectional study included VA patients who were diagnosed with SMI, prescribed an SGA in fiscal year (FY) 2007, and received care from VA facilities with complete data from the 2006 VA Mental Health Program Survey[14–16], anational survey of mental health program directors (N=107, 81% response rate) on organization and integration of care of VHA mental health programs [14]. The National Psychosis Registry (NPR) includes VA administrative data on utilization, diagnosis, pharmacy, lab, and vital signson all VA patients diagnosed with SMI, including schizophrenia or schizoaffective disorder (ICD-9 codes 295.0–295.4; 295.6–295.9), bipolar disorder (296.0–296.1; 296.4–296.8), or other psychotic disorders (297.x, 298.x). This study was reviewed and approved by local Institutional Review Boards.
All patients diagnosed with SMI identified from the NPR who were prescribed SGAs in fiscal year (FY) 2007, including olanzapine, aripiprazole, clozapine, quetiapine, risperidone, or ziprasidone were included in this study. A mental health program was considered to have colocated general medical care if medical services were reported to be located within the mental health clinic by survey respondents. We assessed the percentage receiving the following tests at least twice in FY 2007 (reflecting minimum necessary standards of care) [7]: BMI, blood pressure, lipid profile, and fasting glucose among patients based on NPR data.
Bivariate analyses were used to assess the association between colocation statusand receipt of all four cardiometabolic tests and receipt of each testat least twice in FY2007. Multivariable logistic regression analyses using generalized estimating equations to account for facility-patient clustering were used to determine the independent association between colocation and cardiometabolic test receipt, adjusting forfacility physician-staff ratio, number of unique patients at facility,academic affiliation (defined as medical resident training), andpatient age, sex, race, marital status, service connection, Charlson comorbidity score, anxiety or PTSD diagnosis, substance usediagnosis, and number of primary care visits in FY 2007.
RESULTS
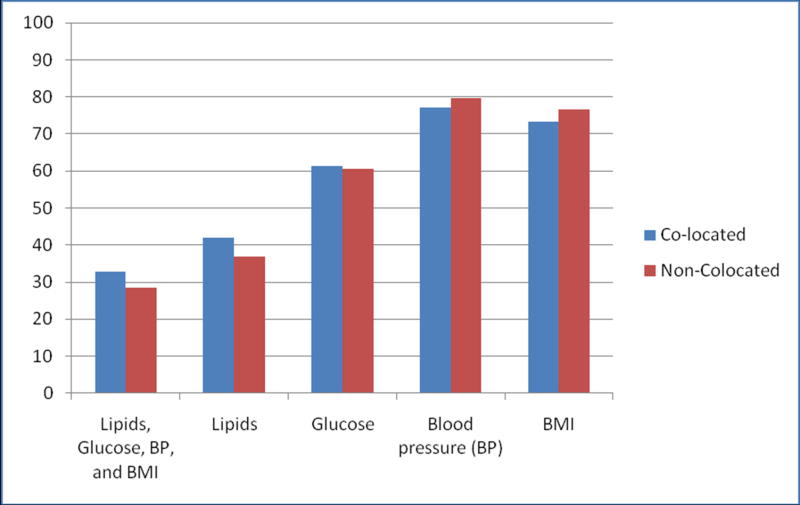
Overall, out of 122,162 VA patients with SMI in FY 2007, 105,100 (85%) received care from the 107 VA medical centerswith complete mental health program survey information, and of those, 40,600 (38%) were prescribed SGAs. Of the 40,600, the mean age was 55 (SD=11.6), 91% were male, and 26% African-American. The 40,600 included in the analyses did not differ in patient characteristics from those not prescribed second-generation antipsychotics or from the total SMI patient population in FY 2007 (e.g., respective mean ageswere 55–57 years, 9% were women, and 21–27% were African-American).Twenty-nine percent received all recommended cardiometabolic tests (lipid, glucose, BMI and blood pressure) at least twice in FY 2007. While 79% and 76% received blood pressure and BMI assessments, respectively, only 37% received a lipid test. Patients from colocated sites were more likely to receive all four cardiometabolic tests (Figure 1, P<.001).
Figure 1.
Percentage of Patients with Serious Mental Illness Receiving Cardiometabolic Monitoring Twice a Year in Fiscal Year 2007 by Colocation of General Medical Services in VA Mental Health Programs (N=40,600)*
*Differences in the combined measures (lipids, glucose, blood pressure, and weight), lipids, blood pressure, and weight are all statistically significant at P<.001
After adjusting for patient and organizational factors, patients from colocated sites were more likely to receive all cardiometabolic tests (OR=1.26, 95% CI: 1.18–1.35, P<.001)than those not from colocated sites. This difference appears to be primarily attributed to observed gaps in monitoring of lipids between colocated and non-colocated sites. In particular, patients from colocated sites were more likely to receive lipid testing (OR=1.26, 95% CI: 1.16–1.38, P<.001), but less likely to receive glucose (OR=.70, 95% CI: .79–.95, P<.01), BMI (OR=.74, 95% CI: . 69–.81, P<.001), or blood pressure monitoring (OR=.76, 95% CI: .69–.95, P<.001) after adjusting for patient and facility factors.
DISCUSSION
About one-third of VA patients with SMI who were prescribed SGAs received all four recommended cardiometabolic monitoring tests twice a year. Gaps in monitoring were especially evident for lab tests. Patients receiving care from colocated mental and general medical clinics were more likely to receive all four recommended cardiometabolic tests.
In light of the cardiometabolic risk factors associated with SGAs, the Substance Abuse and Mental Health Services Administration and the Department of Veterans Affairs (VA) have called for programs to improve integrated medical care for persons with SMI[9]. Receipt of cardiometabolic tests among our study population exceeded estimates found in non-VA settings [10], as the majority of VA patients are receiving regular BMI and blood pressure checks, both of which are important indicators of cardiometabolic risk.Our results suggest that patients from colocated general medical programs were 26% more likely to receive cardiometabolic risk monitoring compared to non-colocated sites. Nonetheless, less than halfreceived recommended lipid and glucose monitoring lab tests. Perhaps these patients faced barriers to obtaining blood draws whichare often done in a separate laboratory. Even in colocated settings, providers may lack the resources to assist patients in following through with lab tests.
Several limitations warrant consideration. First, we were unable to differentiate fasting versus non-fasting labs.When controlling for number of primary care visits, we were unable to differentiate visits made within the colocated clinic from those made to an external VA primary care clinic. Other unmeasured facility factors beyond colocation, such as coordination of specific services or provider communication between mental health and primary care may have influenced the results. Finally, findings from this study may not generalize to non-VA providers or patients.
Colocation of medical and mental health care may likely be associated with effective screening and treatment of cardiometabolic disorders and represents a potentially important step toward reducing the increased mortality experienced by persons with SMI[15]. The challenge will be to develop flexible systems, either concrete [11–13] or virtual[16], by which the principles of collocation can be implemented.
Acknowledgments
This work was supported by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service and the National Institute of Mental Health. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs. The authors report no conflicts of interest- financial or non-financial- in relation to this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lopez AD, Murray CC. The global burden of disease, 1990-2020. Vol. 4. National Medicine; 1998. pp. 1241–1243. [DOI] [PubMed] [Google Scholar]
- 2.Kilbourne AM, Ignacio RV, Kim HM, et al. Datapoints: are VA patients with serious mental illness dying younger? Psychiatric Services. 2009;60:589. doi: 10.1176/ps.2009.60.5.589. [DOI] [PubMed] [Google Scholar]
- 3.Daumit GL, Pratt LA, Crum RM, Powe NR, Ford DE. Characteristics of primary care visits for individuals with severe mental illness in a national sample. Gen Hosp Psychiatry. 2002;24:391–5. doi: 10.1016/s0163-8343(02)00213-x. [DOI] [PubMed] [Google Scholar]
- 4.Newcomer JW. Medical risk in patients with bipolar disorder and schizophrenia. J Clin Psychiatry. 2006;67:e16. [PubMed] [Google Scholar]
- 5.Carney CP, Jones L, Woolson RF. Medical comorbidity in women and men with schizophrenia: a population-based controlled study. J Gen Intern Med. 2006;21:1133–7. doi: 10.1111/j.1525-1497.2006.00563.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Correll CU, Druss BG, Lombardo I, O'Gorman C, Harnett JP, Sanders KN, et al. Findings of a U.S. national cardiometabolic screening program among 10,084 psychiatric outpatients. Psychiatr Serv. 61:892–8. doi: 10.1176/ps.2010.61.9.892. [DOI] [PubMed] [Google Scholar]
- 7.American Diabetes Association; American Psychiatric Association; American Association of Clinical Endocrinologists; North American Association for the Study of Obesity. Consensus development conference on antipsychotic drugs and obesity and diabetes. Diabetes Care. 2004;27:596–601. doi: 10.2337/diacare.27.2.596. [DOI] [PubMed] [Google Scholar]
- 8.Kilbourne AM, Welsh D, McCarthy JF, Post EP, Blow FC. Quality of care for cardiovascular disease-related conditions in patients with and without mental disorders. J Gen Intern Med. 2008;23:1628–33. doi: 10.1007/s11606-008-0720-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Druss BG, Bornemann TH. Improving health and health care for persons with serious mental illness: the window for US federal policy change. JAMA. 2010;303:1972–1973. doi: 10.1001/jama.2010.615. [DOI] [PubMed] [Google Scholar]
- 10.Moeller KE, Rigler SK, Mayorga A, Nazir N, Shireman TI. Quality of monitoring for metabolic effects associated with second generation antipsychotics in patients with schizophrenia on public insurance. Schizophr Res. 2011;126:117–2. doi: 10.1016/j.schres.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 11.Horvitz-Lennon M, Kilbourne AM, Pincus HA. From silos to bridges: meeting the general health care needs of adults with severe mental illnesses. Health Aff. 2006;25:659–69. doi: 10.1377/hlthaff.25.3.659. [DOI] [PubMed] [Google Scholar]
- 12.Druss BG, Rohrbaugh RM, Levinson CM, et al. Integrated medical care for patients with serious psychiatric illness: a randomized trial. Arch Gen Psychiatr. 2001;58:861–868. doi: 10.1001/archpsyc.58.9.861. [DOI] [PubMed] [Google Scholar]
- 13.McGuire J, Gelberg L, Blue-Howells J, et al. Access to primary care for homeless veterans with serious mental illness or substance abuse: a follow-up evaluation of co-located primary care and homeless social services. Administration and Policy in Mental Health. 2009;36:255–264. doi: 10.1007/s10488-009-0210-6. [DOI] [PubMed] [Google Scholar]
- 14.Kilbourne AM, Greenwald DE, Hermann RC, et al. Financial incentives and accountability for integrated medical care in Department of Veterans Affairs mental health programs. Psychiatrice Services. 2009;61:38–44. doi: 10.1176/ps.2010.61.1.38. [DOI] [PubMed] [Google Scholar]
- 15.Smith TE, Sederer LI. A new kind of homelessness for individuals with serious mental illness? The need for a "mental health home". Psychiatric Services. 2009;60:528–533. doi: 10.1176/ps.2009.60.4.528. [DOI] [PubMed] [Google Scholar]
- 16.Simon GE, Katon WJ, VonKorff M, Unützer J, Lin EH, Walker EA, Bush T, Rutter C, Ludman E. Cost-effectiveness of a collaborative care program for primary care patients with persistent depression. Am J Psychiatry. 2001;158:1638–44. doi: 10.1176/appi.ajp.158.10.1638. [DOI] [PubMed] [Google Scholar]