Abstract
Background
Gastric secretion can provide valuable information especially when Helicobacter pylori (Hp) infection results in chronic atrophic gastritis (CAG) and intestinal metaplasia (IM) preceding adenocarcinoma (AdCa).
Aims
Looking for a potential biomarker of malignant transformation in the setting of chronic inflammation we studied the levels of prostaglandin E2 (PGE2), as well as peptide growth factors [epidermal growth factor (EGF) and transforming growth factor α (TGFα)], harbingers of injury and repair, in gastric juice aspirated at endoscopy from patients with CAG, CAG/IM, AdCa, and controls.
Methods
The PGE2, EGF and TGFα concentrations in the gastric juice were measured using radioimmunoassays (RIAs).
Results
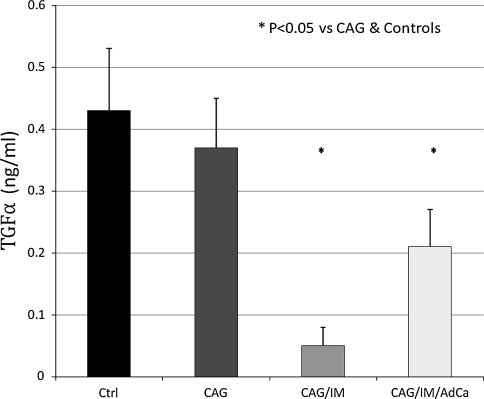
In patients with AdCa gastric juice PGE2 increased fivefold versus controls (P < 0.01) and almost threefold versus patients with CAG (P < 0.05). The EGF levels in patients with AdCa were fourfold higher versus controls (P < 0.001) and almost threefold higher versus CAG (P < 0.05). In patients with CAG/IM the EGF levels were also almost 3 times higher versus controls. The TGFα levels in patients with AdCa were half the value of controls and CAG (P < 0.05). In patients with CAG/IM the levels were as low as 1/5 of controls or CAG (P < 0.05).
Conclusions
Testing the gastric juice for PGE2, EGF, and TGFα in patients with endoscopy and biopsy proven CAG, may be helpful in follow up of patients who may potentially progress to IM and ultimately AdCa. This could be considered as an adjunct to histologic assessment especially that even the best surveillance biopsy specimen regimens are inherited with sampling errors.
Keywords: Gastritis, Intestinal metaplasia, Adenocarcinoma, Helicobacter pylori, Prostaglandins, Peptide growth factors
Introduction
The integrity of the gastrointestinal mucosa depends upon equilibrium between aggressive factors and protective mechanisms [1–3]. Among aggressive factors gastric acid and pepsins are the culprits of injury, whereas PGE2 and peptide growth factors such as EGF and TGFα are the dominant protective molecules [4–8].
Colonization of gastric mucosa with Hp profoundly changes this equilibrium mainly through generation of acute and subsequently chronic inflammation and secretion of its toxins and various enzymes [4–8].
The concentration of PGE2, EGF and TGFα in the gastric juice reflects the rate of the production by the gastric mucosa, their subsequent binding to the receptors on the luminal aspect of the surface epithelium and their proteolytic degradation by gastric acid and pepsin as well as enzymes generated by Hp [9].
The aggressive factors induced gastric mucosal injury resulting in loss of mucosal barrier can be quickly healed if adequate supply of PGE2, EGF and TGFα takes place. Therefore the measurement of PGE2, EGF and TGFα in the gastric juice could reflect their availability for restitution of injured cell epithelium and repair as well as restoration of the mucosal barrier. This is especially an important consideration given the fact that within the gastric mucosal milieu there is always a very powerful and protective endogenous barrier against the aggressive factors especially acid and pepsin [9]. We have therefore studied the concentration of PGE2, EGF and TGFα in gastric juice aspirated at the onset of surveillance endoscopy in patients colonized with Hp in the past with subsequent CAG, IM and gastric AdCa and compared the levels with those with Hp negative controls. This way we have utilized a sample of gastric juice, which would have been discarded otherwise.
Our data represent a proof of concept that the concentrations of PGE2, EGF, or TGFα may differ at various stages of gastric mucosal pathology related to the past history of colonization with H. pylori.
Materials and Methods
Subjects
The study was approved by the Human Investigation Committee at KUMC. Informed consent was obtained from all subjects. Twenty eight consecutive patients referred for upper GI endoscopy for surveillance and with symptoms of non-ulcer dyspepsia were enrolled in the study. All patients had Hp-induced CAG or CAG/IM or CAG/IM/AdCa as confirmed by the endoscopy and gastric biopsy, although they received Hp eradication. Successful H. pylori eradication was confirmed by 14C-urea breath test.
Among recruited patients 16 were M and 12 F. Of the 28 subjects 11 had CAG (6 M & 5 F), 8 had CAG/IM (5 M & 3 F) and 9 patients had Gastric AdCa (5 M & 4 F). The mean age of the population was 55 years (range 30–65 years). There were 13 Hp negative controls with symptoms of non-ulcer dyspepsia (7 M & 6 F, mean age of 52, 28–64 range) with normal endoscopy and histology.
All subjects represent outpatient’s population within the Endoscopy Center. Patients were advised not to eat and drink after midnight. Patients were not taking non-steroidal anti-inflammatory drugs as well as antisecretory medication for at least 1 week before endoscopy. All patients were prepared for endoscopy using the same standardized procedure. None medication, including antacids, was allowed on the day of endoscopy.
The biopsy sampling and degree of gastritis was assessed according to Sydney System, 1996. Briefly, 1 specimen was obtained from the lesser and 1 from the greater curvature of the antrum, both within 2–3 cm from the pylorus; 1 sample from the lesser curvature of the corpus approximately 4 cm proximal to the angulus, 1 sample from the middle portion of the greater curvature of the corpus, about 8 cm from the cardia and 1 sample from the incisura angularis”.
Even more than 1 year after successful H. pylori eradication, in a great majority of patients at least moderate infiltration with chronic inflammatory cells was recorded and was similar in three investigated groups. Atrophy of the gastric body mucosa was defined as focal or diffuse oxyntic gland loss and/or replacement by metaplastic pyloric or intestinal glands. Atrophy of the gastric antral mucosa was defined as focal or complete replacement of antral glands with intestinal metaplastic epithelium. Presented patients with gastritis were diagnosed as moderate or severe gastritis with or without type III of intestinal metaplasia.
The age, gender and the smoker status distribution was similar in all subgroups and none of them were drinking more than 1–2 drinks per day. H. pylori eradication was implemented at least 1 year ago. Gastric cancer was found on the lesser curvature and around the angulus, measured between 2 and 5 cm and histologically represented the intestinal type of adenocarcinoma, T1 or T2, all well or moderately well differentiated.
At the time of endoscopy gastric juice present within the stomach was aspirated into a container, iced, assessed volumetrically and processed immediately.
All samples were centrifuged at 3,000 rpm (2,500g) for 30 min, conditions required to spin down cell debris such as plasma membrane sheets and nuclei (Sorvall RT 6000 Refrigerated Centrifuge, Rotor H1000, Newtown, CT). All samples were centrifuged at 4°C.
Methods
Measurement of PGE2
PGE2 in the gastric juice was measured as the methyloxime by the radioimmunoassay (RIA) using a novel iodinated label (Amersham, Arlington Heights, IL) developed by Kelly et al. [10] as described recently [11, 12]. The advantage of this method is that the imide linkage of the methyl oxime to proline results in an equal affinity of antiserum for the labeled oximated PGE2 and compound to be measured. Methyloximation also protects PGE2 from dehydration during the assay. The sample extraction step through C18 columns provides a high degree of homogeneity and it also maintains near 100% recovery of added PGE2. We achieved very good intraassay (3.4%) and interassay (5.8%) variations [11].
Measurement of EGF and TGFα
The pH of gastric secretion was recorded with an expandable Ion Analyzer (model AE 940; Orion, MA) and pH of gastric juice was adjusted to pH 7.4 before the measurement of EGF and TGFα. Measurements of EGF and TGFα were performed by RIA using a commercially available kit (Amersham, IL). This assay is based on the highly specific rabbit anti-human RGF and TGFα antibodies, which do not exhibit cross-reactivity with a large variety of structurally unrelated gut peptides such as gastrin, somatostatin, secretin, or pancreatic polypeptide [7, 8].
Anti-human EGF and TGF α antibodies showed an 88% cross reactivity with the mouse EGF but not rat TGFα (0% cross-reactivity). Human EGF antiserum was used at a dilution of 1:20,000. The separation between bound and unbound EGF was performed with a use of Amerlex-M second antibody. In the final calculations of EGF and TGFα concentrations, non specific binding was always considered. Human recombinant EGF (Amgen, CA) was used for a standard curve.
Statistical Analysis
All results are presented as the mean ± SEM. Statistical analysis of variance (ANOVA) was performed using Sigma-Stat (Jandel Scientific, San Rafael, CA).
Results
Gastric Juice PGE2
The levels of PGE2 (Fig. 1) in patients with CAG/IM/Ad Ca were over 2,000 pg/ml, i.e. a fivefold elevation, as compared to the controls (P < 0.01). When compared to the group with CAG the levels in patients with CAG/IM/AdCa were about threefolds higher (P < 0.05). The levels were also high in patients with CAG/IM, about threefold as compared to the controls. In patients with CAG the levels were almost twofold higher than in controls.
Fig. 1.
Gastric Juice prostaglandin E2 in controls (Ctrl), chronic atrophic gastritis (CAG), chronic atrophic gastritis/intestinal metaplasia (CAG/IM), and chronic atrophic gastritis/intestinal metaplasia/adenocarcinoma (CAG/IM/AdCa)
Gastric Juice EGF
The concentration of EGF (Fig. 2) in gastric secretion of patients with CAG/IM/AdCa was over fourfold higher than the controls (6.4 ng/ml vs. 1.6 ng/ml, P < 0.001) and threefold higher in comparison to the CAG group (P < 0.05). The levels were also elevated in CAG/IM although to a much lower concentration than those with AdCa, reaching about threefold increase as compared to the controls. The results of EGF in the samples obtained from CAG were about 1/3 higher than in controls.
Fig. 2.
Gastric juice EGF in controls (Ctrl), chronic atrophic gastritis (CAG), chronic atrophic gastritis/intestinal metaplasia (CAG/IM), and chronic atrophic gastritis/intestinal metaplasia/adenocarcinoma (CAG/IM/AdCa)
Gastric Juice TGFα
Intriguingly, the levels of TGFα (Fig. 3) in patients with CAG/IM were as low as 1/5th of the control group or patients with CAG (P < 0.05). The levels were as low as 0.07 ng/ml in this subset of patients. The concentration of TGFα in patients with CAG/IM/AdCa were half the value of controls and CAG (P < 0.05), but increased almost threefold from the lowest value recorded in patients with CAG/IM. However the TGFα levels in CAG were quite similar to values in controls.
Fig. 3.
Gastric juice TGFα in controls (Ctrl), chronic atrophic gastritis (CAG), chronic atrophic gastritis/intestinal metaplasia (CAG/IM), and chronic atrophic gastritis/intestinal metaplasia/adenocarcinoma (CAG/IM/AdCa)
Discussion
Chronic inflammation has been well implicated in the etiology of alimentary tract cancer. Key molecular players that link inflammation to carcinogenesis are prostaglandins, cytokines, nuclear factor –κB, chemokines, angiogenic growth factors and free radicals as well as gene products which contribute to multistage of carcinogenesis through activation of oncogenic products and/or inhibition of tumor suppressor genes [13]. Though inflammation includes injury, repair and resolution; all inflammatory cells may also contribute to carcinogenesis [14]. Inflammatory stimuli include chemicals, foreign bodies and infectious organisms such as Helicobacter pylori (Hp), Ebstein Barr virus among others [15].
Hp has been linked epidemiologically to gastric and duodenal ulcers, gastric cancer and gastric mucosa-associated lymphoid tissue (MALT) lymphoma [16–18]. Hp induced CAG is a prerequisite for the formation of preneoplastic and malignant lesions, both in humans and in rodent models of Hp-induced disease [19, 20]. The transformation from normal mucosa to gastric cancer occurs via a sequence of precursor lesions starting with CAG, IM and dysplasia [21].
Inflammation and carcinogenesis share a common molecular mediator, the cyclooxygenase (COX) enzymes COX-1 and COX-2 which generate their major product PGE2, exerting its effects by binding to the ubiquitously expressed the E prostanoid receptors 1–4 [22, 23].
COX-2–dependent pathways play a role in carcinogenesis, especially in the gastrointestinal tract [24, 25]. The long-term low-level intake of nonsteroidal anti-inflammatory drugs inhibiting COX activity reduces the risk of gastric and colorectal cancer [26–28]. Tumor-derived PGE2 is believed to promote cancer progression by stimulating cell motility/invasion, angiogenesis and by preventing tumor cell apoptosis [29] through potentiation and induction of target genes by activation of the EGF receptor pathway [30]. PGE2 through its strong immunosuppressive effects, may allow tumors to evade immune surveillance [31].
It is a known fact that COX-1 and COX-2 are widely expressed in gastric cancers resulting in elevated PGE2 levels which up regulates VEGF expression and this effect is mediated by the EGFR activation [32–36]. This enhances the cancer cell invasion and angiogenesis via TLR2 and TLR9, which can be attenuated by the specific COX-2 inhibitor NS398 or celecoxib [37].
Our study clearly substantiates the above concepts of a link between prostaglandin E2 and carcinogenesis. The levels of PGE2 were significantly higher in CAG/IM/AdCa and the levels showed a proportional increase in CAG and CAG/IM. This confirms the findings that PGE2 in the gastric mucosa and plasma is increased in all patients with gastric cancer, especially with metastasis and it correlates well with age, stage, histological pattern of tumor, its differentiation and infiltration [38, 39].
The gastrointestinal tract possesses the remarkable ability to withstand injury resulting in cell migration (restitution), followed by an increase in proliferation and remodeling with at least 30 different peptides being involved in stimulating the repair process. In general peptides can be compartmentalized into: (1) mucosal integrity peptides which are predominantly involved in maintaining mucosal morphology e.g., TGFα (2) luminal surveillance peptides which stimulate proliferation and repair at sites of injury e.g., EGF and (3) rapid response repair peptides whose production is rapidly regulated at sites of injury [40].
EGF, a potent stimulant of proliferation, migration and gut repair is most effective when it can bind to its receptor predominantly located on the basolateral membrane which is easily accessible at the site of injury [41–44]. TGFα is a potent stimulant of proliferation and differentiation acting via the EGF receptor too (EGF-R or c-erb2) [40].
EGF family growth factors including TGFα have been proposed as integrative cytoprotective factors against gastric injury [37, 45], through stimulation of cell proliferation, migration, inhibition gastric acid secretion and increasing the release of mucus [46–48], which is greatly affected by sialoadenectomy in experimental animals [49, 50].
Gastric cancer patients show an increased expression of EGF and TGFα but their gastric acid secretion is markedly reduced possibly due to atrophy of oxyntic mucosa. Overexpression of growth factors in gastric mucosa as well as reduced gastric acid secretion due to gastric mucosal atrophy may be implicated in the pathogenesis of gastric cancer [51].
In our study there is a significant increase in the EGF levels which in concordance with the declining levels of TGFα would benefit to detect those transforming from CAG to CAG/IM and eventually to gastric carcinoma. Very high levels of EGF were found in patients with AdCa, almost a fivefold increase in the concentration compared to the two to threefold rise in CAG and CAG/IM.
Our analysis of gastric juice samples also shows the significant reduction in the TGFα level, which confirms the potential cytoprotective value of this growth factor against development of gastric neoplasm in the setting of CAG/IM. Significant reduction in the levels of TGFα in CAG/IM tissue may facilitate its transformation into gastric cancer. This important aspect during the analysis of the gastric juice should be borne in mind in patients with CAG and with very low levels of TGFα, who could be progressing towards IM vis-à-vis AdCa.
From our analysis of gastric juice samples we conclude that a step wise increase in the PGE2 starting from normal and going through phases of CAG, CAG/IM and ultimately to CAG/IM/AdCa provides a good evidence that testing its content in samples aspirated during surveillance endoscopy could be of value in their predictive potential before and during the development of AdCa. This however requires further investigation. In a similar way simultaneously measuring the concentration of growth factors such as EGF and TGFα will provide us clue as to the underlying disease progression. As noted above in our discussion EGF levels closely parallel the PGE2 levels showing a step wise increase from controls through stages of CAG, CAG/IM and CAG/IM/AdCa. However the levels of TGFα are conversely reduced as the condition progresses from CAG through CAG/IM and CAG/IM/AdCa thereby concurring with several studies done earlier on its protective values [44, 45].
Although in our study subjects the Hp was eradicated prior to the screening endoscopy, it takes several years for most of the patients with CAG to significantly improve the gastric morphology despite eradication. Therefore although our patients had Hp negative CAG, CAG/IM and CAG/IM/AdCa the gastric juice analysis of PGE2, EGF and TGFα still reflect the ongoing chronic inflammatory changes within the gastric mucosa. Hence to eliminate the potential detrimental impact of Hp colonization and subsequent development of chronic inflammation leading to no return to the original normal morphology but rather going on to CAG, CAG/IM and the dreaded complication of gastric AdCa it is highly advisable to treat young people at an early age especially in countries with high endemicity of Hp. This is the only way to prevent the potential chronic complications associated with Hp the most notable being the gastric AdCa.
In conclusion, testing the gastric juice for EGF, TGFα and PGE2 in patients with endoscopy and biopsy proven CAG, due to Hp may be helpful in follow up of these patients who may potentially progress to IM and ultimately to AdCa. This could be considered as an adjunct to histologic assessment especially given the fact that even the best biopsy specimen regimens during surveillance are inherited with significant sampling errors.
Conflict of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Goldberg HI, Dodds WJ, Gee S, et al. Role of acid and pepsin in acute experimental esophagitis. Gastroenterology. 1969;56:223–230. [PubMed] [Google Scholar]
- 2.Richter JE. The symptom index: correlation of acid reflux with symptoms. In: Richter JE, editor. Ambulatory esophageal pH monitoring. New York: Igaku-Shoin; 1991. pp. 93–100. [Google Scholar]
- 3.Slomiany BL, Sarosiek J, Slomiany A. Gastric mucus and the mucosal barrier. Dig Dis. 1987;5:125–145. doi: 10.1159/000171168. [DOI] [PubMed] [Google Scholar]
- 4.Sarosiek J, Feng T, McCallum RW. The interrelationship between salivary epidermal growth factor and the functional integrity of the esophageal mucosal barrier in the rat. Am J Med Sci. 1991;302:359–363. doi: 10.1097/00000441-199112000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Sarosiek J, Bilski J, Murty VLN, et al. Role of salivary epidermal growth factor in the maintenance of physicochemical characteristics of oral and gastric mucus coat. Biochem Biophys Res Commun. 1988;152:1421–1427. doi: 10.1016/S0006-291X(88)80444-3. [DOI] [PubMed] [Google Scholar]
- 6.Sarosiek J, McCallum RW. The evolving appreciation of the role of esophageal mucosal protection in the pathophysiology of gastroesophageal reflux disease. J Pract Gastroenterol. 1994;18:20J–20Q. [Google Scholar]
- 7.Rourk RM, Namiot Z, Sarosiek J, et al. Diminished content of esophageal epidermal growth factor in patients with reflux esophagitis. Am J Gastroenterol. 1994;89:1177–1184. [PubMed] [Google Scholar]
- 8.Rourk RM, Namiot Z, Sarosiek J, et al. Impairment of salivary epidermal growth factor secretory response to esophageal mechanical and chemical stimulation in patients with reflux esophagitis. Am J Gastroenterol. 1994;89:237–244. [PubMed] [Google Scholar]
- 9.Sarosiek J, Jensen TJ, Maton PN, et al. Gastric salivary epidermal growth factor in patients with Zollinger-Ellison syndrome: its protective potential. Am J Gastroenterol. 2000;95:1158–1165. doi: 10.1111/j.1572-0241.2000.02003.x. [DOI] [PubMed] [Google Scholar]
- 10.Kelly RW, Graham BJM, O’Sullivan MJ. Measurement of PGE2 as the methyl oximate by the radioimmunoassay using a novel iodinated label. Prostagland Leukotrienes Essential Fatty Acids. 1989;89:588–594. doi: 10.1016/0952-3278(89)90084-7. [DOI] [PubMed] [Google Scholar]
- 11.Sarosiek J, Yu Z, Namiot Z, et al. Impact of acid and pepsin on human esophageal prostaglandins. Am J Gastroenterol. 1994;89:588–594. [PubMed] [Google Scholar]
- 12.Marcinkiewicz M, Sarosiek J, Edmunds MC, et al. Monophasic luminal release of prostaglandin E2 in patients with reflux esophagitis under the impact of acid and acid/pepsin solutions: its potential pathogenetic significance. J Clin Gastroenterol. 1995;21:268–274. doi: 10.1097/00004836-199512000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Kim YJ, Chung JW, Lee SJ, et al. Progression from chronic atrophic gastritis to gastric cancer; tangle, toggle, tackle with Korea red ginseng. J Clin Biochem Nutr. 2010;46:195–204. doi: 10.3164/jcbn.10-03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oshima H, Tazawa H, Sylla BS, Sawa T. Prevention of human cancer by modulation of chronic inflammatory process. Mutat Res. 2005;591:110–122. doi: 10.1016/j.mrfmmm.2005.03.030. [DOI] [PubMed] [Google Scholar]
- 15.Coussens L, Werb Z. Inflammation and cancer. Nature. 2002;420:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parsonnet J, Friedman GD, Vandersteen DP, et al. Helicobacter pylori infection and the risk of gastric carcinoma. N Engl J Med. 1991;325:1127–1131. doi: 10.1056/NEJM199110173251603. [DOI] [PubMed] [Google Scholar]
- 17.Parsonnet J, Isaacson PG. Bacterial infection and MALT lymphoma. N Engl J Med. 2004;350:213–215. doi: 10.1056/NEJMp038200. [DOI] [PubMed] [Google Scholar]
- 18.Danesh J. Helicobacter pylori infection and gastric cancer: systematic review of the epidemiological studies. Aliment Pharmacol Ther. 1999;13:851–856. doi: 10.1046/j.1365-2036.1999.00546.x. [DOI] [PubMed] [Google Scholar]
- 19.Fox JG, Sheppard BJ, Dangler CA, et al. Germ-line p53-targeted disruption inhibits Helicobacter-induced premalignant lesions and invasive gastric carcinoma through down-regulation of Th1 proinflammatory responses. Cancer Res. 2002;62:696–702. [PubMed] [Google Scholar]
- 20.Rieder G, Merchant JL, Haas R. Helicobacter pylori cag-type IV secretion system facilitates corpus colonization to induce precancerous conditions in Mongolian gerbils. Gastroenterology. 2005;128:1229–1242. doi: 10.1053/j.gastro.2005.02.064. [DOI] [PubMed] [Google Scholar]
- 21.Correa P. Helicobacter pylori and gastric carcinogenesis. Am J Surg Pathol. 1995;19:S37–S43. doi: 10.1097/00000478-199501000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Simmons DL, Botting RM, Hla T. Cyclooxygenase isozymes: the biology of prostaglandin synthesis and inhibition. Pharmacol Rev. 2004;56:387–437. doi: 10.1124/pr.56.3.3. [DOI] [PubMed] [Google Scholar]
- 23.Narumiya S, Sugimoto Y, Ushikubi F. Prostanoid receptors: structures, properties, and functions. Physiol Rev. 1999;79:1193–1226. doi: 10.1152/physrev.1999.79.4.1193. [DOI] [PubMed] [Google Scholar]
- 24.Potter JD, Ulrich CM. COX-2 and gastric cancer: more on inflammation and neoplasia. Gastroenterology. 2006;130:2198–2200. doi: 10.1053/j.gastro.2006.04.037. [DOI] [PubMed] [Google Scholar]
- 25.Liu F, Pan K, Zhang X, et al. Genetic variants in cyclooxygenase-2: expression and risk of gastric cancer and its precursors in a Chinese population. Gastroenterology. 2006;130:1975–1984. doi: 10.1053/j.gastro.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 26.Ulrich CM, Bigler J, Potter JD. Non-steroidal anti-inflammatory drugs for cancer prevention: promise, perils and pharmacogenetics. Nat Rev Cancer. 2006;6:130–140. doi: 10.1038/nrc1801. [DOI] [PubMed] [Google Scholar]
- 27.Kune GA, Kune S, Watson LF. Colorectal cancer risk, chronic illnesses, operations, and medications: case control results from the Melbourne Colorectal Cancer Study. Cancer Res. 1988;48:4399–4404. [PubMed] [Google Scholar]
- 28.Wang WH, Huang JQ, Zheng GF, et al. Non-steroidal anti-inflammatory drug use and the risk of gastric cancer: a systematic review and meta-analysis. J Natl Cancer Inst. 2003;95:1784–1791. doi: 10.1093/jnci/djg106. [DOI] [PubMed] [Google Scholar]
- 29.Wang D, DuBois RN. Inflammatory mediators and nuclear receptor signaling in colorectal cancer. Cell Cycle. 2007;6:682–685. doi: 10.4161/cc.6.6.4030. [DOI] [PubMed] [Google Scholar]
- 30.Cha YI, Dubois RN. NSAIDs and cancer prevention: targets downstream of COX-2. Annu Rev Med. 2007;58:239–252. doi: 10.1146/annurev.med.57.121304.131253. [DOI] [PubMed] [Google Scholar]
- 31.Pockaj BA, Basu GD, Pathangey LB, et al. Reduced T-cell and dendritic cell function is related to cyclooxygenase-2 overexpression and prostaglandin E2 secretion in patients with breast cancer. Ann Surg Oncol. 2004;11:328–339. doi: 10.1245/ASO.2004.05.027. [DOI] [PubMed] [Google Scholar]
- 32.Jang TJ. Expression of proteins related to prostaglandin E2 biosynthesis is increased in human gastric cancer, during gastric carcinogenesis. Virchow’s Arch. 2004;445:564–571. doi: 10.1007/s00428-004-1104-3. [DOI] [PubMed] [Google Scholar]
- 33.Rigas B, Goldman IS, Levine L. Altered eicosanoid levels in human colon cancer. J Lab Clin Med. 1993;122:518–523. [PubMed] [Google Scholar]
- 34.Bennett A, Civier A, Hensby CN, Melhuish PB, Stamford IF. Measurement of arachinodate and its metabolites extracted from human normal and malignant gastrointestinal tissues. Gut. 1987;28:315–318. doi: 10.1136/gut.28.3.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McLemore TL, Hubbard WC, Litterst CL, et al. Profiles of prostaglandin biosynthesis in normal lung and tumor tissue from lung cancer patients. Cancer Res. 1998;58:3140–3147. [PubMed] [Google Scholar]
- 36.Ding Y-B, Shi R-H, Tong J-D, et al. PGE2 up-regulates vascular endothelial growth factor expression in MKN28 Gastric cancer cells via epidermal growth factor receptor signalling system. Exp Oncol. 2005;27:108–113. [PubMed] [Google Scholar]
- 37.Nakajima T, Konda Y, Izumi Y, et al. Gastrin stimulates the growth of gastric pit cell precursors by inducing its own receptors. Am J Physiol Gastrointest Liver Physiol. 2002;282:G359–G366. doi: 10.1152/ajpgi.00117.2001. [DOI] [PubMed] [Google Scholar]
- 38.Fu QL, Yang MF, Li ZJ, Jiang YY, Song SB, Song TH, Wang HX. Prostaglandin E (PGE), gastric carcinoma. Zhonghua Zhong Liu Za Zhi. 1986;8:345–348. [PubMed] [Google Scholar]
- 39.Kushlinkskiĭ NE, Klimenkov AA, Abdraimov SB, Rommenberg VI, Liakina LT. Prostaglandins E in malignant stomach neoplasms. Vopr Onkol. 1994;40:171–176. [PubMed] [Google Scholar]
- 40.Playford RJ, Wright NA, Marchbank T. Endogenous peptides and peptide therapy in gut defense and repair. Drug News Perspect. 2000;13:330. [PubMed] [Google Scholar]
- 41.Wright NA, Pike C, Elia G. Induction of a novel epidermal growth factor-secreting cell lineage by mucosal ulceration in human gastrointestinal stem cells. Nature. 1990;343:82–85. doi: 10.1038/343082a0. [DOI] [PubMed] [Google Scholar]
- 42.Playford PJ, Harby A, Gschmeissner S, Peiffer LP, McGarrity T, Wright NA. The epidermal growth factor receptor (EGF-R) is present on the basolateral, but not the apical surface of the enterocytes in the human gastrointestinal tract. Gut. 1996;38:303–305. doi: 10.1136/gut.38.3.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sarosiek J, Feng T, McCallum RW. The interrelationship between salivary epidermal growth factor and the functional integrity of the esophageal mucosal barrier in the rat. Am J Med Sci. 1991;302:359–363. doi: 10.1097/00000441-199112000-00007. [DOI] [PubMed] [Google Scholar]
- 44.Playford RJ, Wright NA. Why is EGF present in the gut lumen? Gut. 1996;38:303–305. doi: 10.1136/gut.38.3.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Barnard JA, Beauchamp RD, Russell WE, Dubois RN, Coffey RJ. Epidermal growth factor-related peptides and their relevance to gastrointestinal pathophysiology. Gastroenterology. 1995;108:564–580. doi: 10.1016/0016-5085(95)90087-X. [DOI] [PubMed] [Google Scholar]
- 46.Ciacci C, Lind SE, Podolsky DK. Transforming growth factor beta regulation of migration in wounded rat intestinal epithelial monolayers. Gastroenterology. 1993;105:93–101. doi: 10.1016/0016-5085(93)90014-4. [DOI] [PubMed] [Google Scholar]
- 47.Konturek JW, Bielanski W, Konturek SJ, Bogdal J, Olesky J. Distribution and release of epidermal growth factor in man. Gut. 1989;30:1194–1200. doi: 10.1136/gut.30.9.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Konturek SJ, Brzozowski T, Majka J, Dembinski A, Slomiany A, Slomiany BL. Transforming growth factor alpha and epidermal growth factor in protection and healing of gastric mucosal injury. Scand J Gastroenterol. 1992;27:649–655. doi: 10.3109/00365529209000134. [DOI] [PubMed] [Google Scholar]
- 49.Skov Olsen P, Poulsen SS, Therkelsen K, Nex E. Effect of sialoadenectomy and synthetic human urogastrone on healing of chronic duodenal ulcers in rats. Gut. 1986;27:1443–1449. doi: 10.1136/gut.27.12.1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Konturek SJ, Dembinski A, Warzecha Z, Brzozowski T, Gregory H. Role of epidermal growth factor in healing of chronic gastroduodenal ulcers in rats. Gastroenterology. 1988;94:1300–1307. doi: 10.1016/0016-5085(88)90667-1. [DOI] [PubMed] [Google Scholar]
- 51.Konturek PC, Bielanski W, Konturek SJ, Hahn EG. Gastric mucosal expression and luminal release of growth factors in gastric carcinoma and duodenal ulcer patients before and after eradication of helicobacter pylori. J Physiol Pharmacol. 1997;48:375–382. [PubMed] [Google Scholar]