Abstract
Study Objectives:
Reduced time in bed relative to biological sleep need is common. The impact of habitual short sleep on auditory attention has not been studied to date. In the current study, we utilized novelty oddball tasks to evaluate the effect of habitual short sleep on brain function underlying attention control processes measured by the mismatch negativity (MMN, index of pre-attentive stage), P3a (attention-dependent), and P3b (memory-dependent) event related brain potentials (ERPs). An extended time in bed in a separate study was used to evaluate the possible reversal of the impairments of these processes in habitual short sleepers.
Methods:
Ten self-defined short sleepers (total sleep time [TST] ≤ 6h) and 9 normal-sleeping subjects with TST 7-8 h, participated. ERPs were recorded via a 64-channel EEG system. Two test conditions: “ignore” and “attend” were implemented. The ERPs were analyzed and compared between groups on the 2 task conditions and frontal/central/parietal electrodes by 3-factor ANOVA. Sleep diary data were compared between groups by t-test. Sleep was recorded by the Zeo sleep monitoring system for a week in both habitual and extended sleep conditions at home.
Results:
The main findings of the present study show that short sleeping individuals had deficiency in activity of the MMN and P3a brain responses over frontal areas compared to normal-sleeping subjects. The P3b amplitude was increased over frontal areas and decreased over parietal with respect to the control group. Extension of time in bed for one week increased TST (from 5.7 h to 7.4 h), and concomitantly MMN amplitude increased from −0.1μV up to −1.25 μV over frontal areas.
Conclusions:
Reduced time in bed is associated with deficiency of the neuronal process associated with change detection, which may recover after one week of sleep extension, whereas attention-dependent neural processes do not normalize after this period of time in habitually short sleeping individuals and may require longer recovery periods.
Citation:
Gumenyuk V; Roth T; Korzyukov O; Jefferson C; Bowyer S; Drake CL. Habitual short sleep impacts frontal switch mechanism in attention to novelty. SLEEP 2011;34(12):1659-1670.
Keywords: Short sleep, ERPs, attention, memory, sleep extension
INTRODUCTION
The importance of adequate sleep duration is often overlooked, especially in countries with busy 24/7 schedules. In a meta-analysis by Knutson et al.,1 the trend of shorter sleep periods among individuals in the USA for the time period of 1975-2006 was documented. Short sleepers were defined as those reporting < 6 h of sleep in their sleep diary. They found an increase in the number of short sleepers from 7.6% in 1975 to 9.3% in 2006 among full-time workers. Another meta-analysis on 1,382,999 participants from 8 different countries (USA, Japan, UK, Spain, Sweden, Finland, Israel, and Taiwan) showed that both short and long duration of sleep are associated with increased mortality risk.5
Studies have shown that restricting sleep to ≤ 6 h in healthy individuals can produce a significant decline in vigilance reaction time, increase objective daytime sleepiness to pathological levels, and produce impairments in memory.6–8 However, it is unclear whether impairments of neuronal processing of auditory information are present in individuals who regularly restrict habitual time in bed (TIB) to ≤ 6 hours.
It is also unknown if deficiency in neuronal processing can be reversed following sleep extension. Sleep extension in college students has been shown to improve daytime alertness vigilance and mood.9 Roehrs and colleagues10 showed that habitually sleepy individuals (multiple sleep latency test [MSLT] < 6 min) did improve their sleepiness after 6 consecutive nights of extended TIB (10 h) to near fully alert levels (MSLT = 10 min).
In a recent sleep restriction-extension study,11 the authors showed that one week of sleep extension (TIB 10 h) improved resilience during subsequent sleep restriction and facilitated task related performance during recovery in normal subjects. A 2-week sleep extension study showed full recovery of alertness after 2 weeks.12 These data suggest that increasing time in bed in habitual short sleepers may also provide benefits for specific aspects of cognitive function. However, it remains unknown if extending time in bed to levels typical of the general population would have benefits on cognitive processing.
Neurocognitive changes associated with sleep loss have been studied in both clinic and research subjects. Among methods used for this assessment are event-related brain potentials (ERPs). ERPs are one of the most informative and dynamic methods of monitoring the information stream in the brain. The voltage deflections comprising the ERP reflect the reception and processing of sensory information, as well as higher-level processing involving selective attention, memory updating, and other types of cognitive activity. ERPs are linked in time with a physical or mental event, and typically extracted from the scalp-recorded electroencephalogram (EEG) by means of signal averaging.
Due to its high sensitivity to variables related to information processing (e.g., auditory discrimination), the ERP may complement traditional and limited performance measures, such as the accuracy and speed of behavioral responses. Monitoring changes in ERPs may also be used to assess the effects of sleep restriction and extension on early stages of information processing (e.g., occurring in tens of milliseconds). The cognitive operations reflected in ERP components are supported by specific brain systems, which in some cases have been well defined.13–15
As the human brain does not have a sufficient capacity to enable our consciousness to simultaneously detect all sensory information entering our sensory system, our cognitive processes involve an “automatic” mode as well as an “attentional” mode to process all of the incoming information. Therefore, following an initial phase (sensory input), only part of the incoming information gains access to consciousness.16 In the current theory of human attention-control, there is an assumption that the relatively large-capacity system performs the initial processing of sensory information, and the subsequent limited-capacity system takes over for task-related evaluation and decision-making processes.17,18 Thus, the entry of information to the limited-capacity system is controlled by two types of processes: focused attention and breakthrough of the unattended information (or passive attention).19 The balance between these two neuronal processes is very important for attention control. For example, lack of flexibility between the two processes may lead to either insufficient attention to potentially relevant events or easy distraction by irrelevant events. In laboratory studies, these two processes have been found to be greatly affected by sleep loss.20–22
There are auditory ERP components that can be used as a tool for assessing pre-attentive, attention-dependent, and memory-dependent brain mechanisms involved in attention control. Mismatch negativity (MMN) is an ERP component with a frontocentral scalp topographical distribution, elicited by infrequent stimuli presented among frequent stimuli. The MMN has been described as an “automatic” brain response occurring at a latency around 150 ms from deviance onset to any change in the acoustical environment and is relatively independent of the listener's perception of the sound or behavioral response to the sound.23 Thus, the MMN (amplitude and latency) reflects the outcome of a deviance-detection process associated with infrequent sound that is based on the memory of regularities in the auditory input formed by frequent sound.23–25 Because the MMN is elicited when an incoming sound does not “match” the series of previous stimuli, even when these stimuli occur outside of the subject's attention, it might be that the MMN-generating process (frontal counterpart of the MMN) could be involved in both the “passive” and “active” directing of attention.26,26,27 Therefore, in our study we used the MMN in passive and active tasks to evaluate the frontal lobe function in direction of attention to the novelty associated with automatic change-detection processes.
Another ERP component, the P3a (or novelty P3) is elicited by novel or deviant sounds during an “ignore” or “attend” task condition. The P3a is associated with involuntary attention switching (irrelevant to the task) to salient sounds.28,27 The P3a has latency at around 200-300 ms from deviance onset and a frontocentral scalp distribution. ERP studies in humans with frontal lobe lesions have found that such patients produce a clear diminution of the P3a from a distracting stimulus.29 Frontal lobe engagement is therefore necessary for P3a generation and mechanisms of attention control.30 It has been demonstrated that 36 hours of total sleep deprivation affects frontal neuronal processes involved in novelty detection as measured by P3a (or novelty P3).20 In this study, authors demonstrated the sensitivity of P3a amplitude to sleep deprivation (8.7 μV in control subjects vs. 3.5 μV following 36 h of total sleep deprivation). Following recovery sleep (TIB 10 hours), the P3a increased from 3.5 μV to 6.2 μV at frontal sites.20 Based on these previous studies, we expected that novel sounds would elicit the MMN and P3a complex with attenuated amplitudes in short sleepers with respect to these ERPs in normal-sleeping individuals.
Unlike the P3a, another ERP component termed “P3b” is task relevant and associated with target detection. It is elicited when a subject's attention is focused on a stimulus.31 The P3b is associated with the process of memory comparison in the context of the previous stimuli, generating a brain potential with a parietal scalp distribution. The initial processing of a new stimulus engages the switching of attention that underlies P3a production, whereas the subsequent memory comparison engages the operations associated with P3b production.32,33 According to previous research showing the effect of sleep deprivation on the amplitude and latency of the P3b,20,33 attenuation of amplitude and prolonged latency of the P3b are expected in habitually short sleepers compared to normal sleepers.
In the current study, we utilized “to-be-ignored” vs. “attend” novelty oddball tasks to evaluate the effect of habitual short sleep on brain function underlying attention control process measured by the MMN (index of pre-attentive stage), P3a (attention-dependent), and P3b (memory-dependent) ERP components (Study I). Extended time in bed was used to evaluate the possible reversal of the impairments of these processes in habitual short sleepers (Study II).
We expected novel sounds to elicit ERP components with predominantly frontal scalp distribution (MMN and P3a) in normal sleeping individuals, whereas in habitually short sleeping individuals these ERPs show amplitude attenuation over frontal areas due to the impact of habitual short sleep time on reducing markers of frontal lobe activity.20,41 We also hypothesized that attention load in the attend condition would contribute to the attenuation of the MMN, P3a, and P3b amplitudes with respect to the ERPs in normal-sleeping individuals. For the extended sleep condition, we hypothesized that longer time in bed would increase total sleep time, which subsequently would improve frontal activity in short sleeping individuals.
METHODS
Participants
All participants were recruited from advertisements posted at the Henry Ford Hospital website for employees. A total of 12 self-defined healthy short sleepers (1-week sleep diary total sleep time (TST) ≤ 6 h) were enrolled in the study. EEG/ERP data of 2 individuals were excluded due to extensive EEG artifacts. Thus, 10 habitual short sleepers (Mean age: 35 ± 10 y, 5 females) and 9 self-reported normal sleepers with TST 7-8 h, who served as a control group (mean age: 30 ± 6 y, 6 females) participated in study I. In study II, only habitually short sleeping individuals participated. Neither group had a history of sleep disorders; participants worked or attended school on a typical daytime schedule (∼08:00-17:00 hours, Monday-Friday). All participants underwent an initial phone interview to document their sleep quality and duration and to rule out known medical or psychiatric/neurological illness. Habitually short sleeping participants were confirmed to be free of excessive sleepiness and insomnia based on the Epworth Sleepiness Scale (mean 3.6 ± 2.2) and Insomnia Severity Index (mean 4.9 ± 3.8). The Stanford Sleepiness Scale was also collected during the week of habitual short sleep (mean 2.35 ± 0.64) and the week of extended sleep (mean 2.40 ± 0.98 for control). Although polysomnography was not performed in the current study, sleep apnea was screened out during the clinical evaluation using the Berlin Questionnaire,34 with each participant endorsing < 2 categories on the Berlin, indicating low risk for OSA in all participants. Habitual sleep time was determined by self-report with a one week sleep diary prior to participation.
In the EEG/ERP study (performed on the 8th day of either the habitual or extended week of sleep), the clock time of each ERP assessment was set between 14:00 and 16:00. The mean body mass index for short sleepers was 23.4 ± 5.9, and for the control population it was 22.6 ± 3.7. All participants have had ≤ 5 caffeinated beverages per week. Individuals using any CNS medication including over-the-counter sleep aids were excluded from participation. All study procedures were approved by the Institutional Review Board of Henry Ford Hospital, and informed consent was obtained from all participants. Individuals were paid for their participation.
Stimuli and Procedure
A novelty oddball task utilized ignore and attend task-conditions, which were counterbalanced between participants. The presented sequence of stimuli in the ignore task consisted of a “standard” tone (pure tone = 600 Hz, 100 ms duration, probability of occurrence = 70%) and “deviant” tone (pure tone = 700 Hz, 100 ms duration, probability of occurrence = 20%), as well as a “novel” sound, presented as 110 unique environmental sounds (e.g., dog barking, baby sounds, bird sounds) randomly interspersed among standard and deviant tones. The novel sound was 100 ms duration with a probability of occurrence = 10%. All participants were pre-screened with a brief hearing test using standard procedure prior to the ERP study. All participants were seated comfortably in a sound-attenuated room in the sleep center and asked to ignore all sounds during the ignore task condition. A silent movie, chosen by the participants, was used for helping subjects to follow task instructions to ignore the auditory stimuli and to direct their attention away from the presented sounds. In the attend task condition, participants were asked to fixate their gaze on a cross presented on the screen of the computer positioned approximately 80 cm from participant's eyes. In the attend condition, 12 deviant sounds were replaced by the target sound (pure tone = 1000 Hz, duration 100 ms) in the previously described stimuli sequence. All participants were trained to recognize the target tone during a short (∼1 min) practice session. Participants were asked to count the target tones quietly in their head and report the total number of target tones after the EEG/ERP recording session. All participants counted the targets with > 85% accuracy. All sounds were presented through earplugs binaurally at a 75dB SPL (sound pressure level) with a 5 ms rise/fall time. All stimuli were presented at a constant interstimulus interval of 800 ms. A total of 1100 trials were presented for each task condition.
EEG Recording and Analysis
The EEG was recorded via a 64-channel EEG cap (Easycap GmbH Hersching, Germany), using the ASA-EEG system (ANT, Netherlands).The 64-channel EEG system is an appropriate tool for studying global brain regional differences that we expect to observe between sleep conditions in our participants. The 2 forehead electrodes (Fp1 and Fp2) as well as one left (F7) and one right (F8) served to monitor eye movement artifact during EEG recording. Impedance was kept < 10 kΩ. A band-pass filter was set from 0.1 to 100 Hz, and the sampling rate was 1024 Hz.
EEG data were analyzed using Brain Vision Analyzer software (Brain Products GmbH, Gilching, Germany). Data were segmented separately for each stimulus, starting with 100 ms prior to stimulus onset and continuing for 400 ms after the stimulus onset. A band-pass filter ranging from 1 to 20 Hz was applied to segmented data. Trials in which the EEG or EOG exceeded ± 70μV were excluded from the analysis. ERPs in response to the standard tone and novel sounds were averaged separately. On mean, ≥ 300 trials for the standard tone, and ≥ 100 trials for novel sounds were included for each participant in each task condition.
All statistical comparisons of the MMN and P3a, and P3b to novel sounds involved computing difference waves (ERPs in response to novel sounds minus ERPs to the standard tone). The time windows for mean amplitude comparisons were selected based on the peak amplitude of each brain response at Fz, F3, F4 (frontal); Cz, C3, and C4 (central); and Pz, P3, and P4 (parietal) electrodes. Thus, the mean amplitudes of the MMN components to novel sounds were measured in both task conditions within 120-150 ms from stimulus onset.
The mean amplitude of the P3a observed in the ignore and attend tasks were selected within a 200-240 ms time window for further comparison. As expected, the P3b was observed in the attend task only. The mean amplitude within the 280-320 ms time window was selected for further statistical evaluation of P3b amplitude differences between groups at frontal (Fz), central (Cz), and parietal (Pz) electrodes.
In study I, the MMN and P3a amplitudes were analyzed and compared between groups (control vs. short sleepers) on the 2 task conditions (ignore vs. attend) for frontality (frontal [F3, Fz, and F4] / central [C3, Cz, and C4] / and parietal [P3, Pz, and P4] electrodes) with 3-factor ANOVA. The P3b amplitude and latency differences were tested by 2-way ANOVA with factors: groups and electrodes (Fz, Cz, and Pz).
In study II, the MMN and P3a amplitudes were statistically compared within subjects for sleep condition (short vs. extended), task condition (ignore vs. attend), and frontality by 3-factor ANOVA (2 within, 1 between). The P3b amplitude difference was tested by 2-way ANOVA with factors: sleep condition (habitual vs. extended) and electrodes (Fz, Cz, and Pz). Sleep diary data were compared between and within group by t-tests. An α-level of 0.05 was used for all statistical tests.
In all statistical analyses of ANOVA, Greenhouse-Geisser corrections were applied when appropriate; significant effects were further specified by Newman-Keuls post hoc test.
Sleep in Study II
The sleep conditions (habitual and extended) were counterbalanced in short sleeping participants and performed for one week prior for the EEG/ERP assessment. A week of habitual time in bed was required between the 2 sleep conditions in order to “wash out” the effect produced by extended time in bed for each short sleeper. Sleep parameters were measured using an in-home monitor comprised of a headband containing dry fabric sensors that wirelessly transmitted single-channel EEG signals obtained from the forehead to a bedside device for processing (Zeo Inc, USA). Sleep parameters were computed in real-time by the device, using previously validated algorithms.35 Sleep variables measured included total sleep time (TST), latency to persistent sleep ([LPS] 10 min of consecutive sleep), wake time during sleep (WTDS), stage 1 and 2 sleep, slow wave sleep (SWS), and REM sleep. To facilitate accurate measures of LPS, participants were instructed to put on the wireless headband immediately prior the participant's intent to go to sleep, and to keep the headband on all night long and place it back on its bedside device upon rising from bed in the morning. For the sleep extension condition, participants were asked to go to bed earlier by 1 h and delay their habitual rise time by 1 h. The extended time in bed mean was ∼8.5 h.
The current study was designed to observe electrophysiological changes associated with individuals who have habitually short sleep compared to normal sleepers (study I), as well as potential improvement of sleep and electrophysiological indices of sensory memory and attention in short sleepers after one week of sleep extension (study II).
RESULTS
Study I: Short Sleepers vs. Controls
Sleep parameters
Data from the sleep diary indicated that TST was significantly shorter in the short sleeper group than normal sleepers (control group) (5.8 ± 0.5 h vs. 7.8 ± 0.4 h; t = 8.98, P < 0.001). Both controls and short sleepers reported their habitual bed time between 23:30 and 01:30. The latter group reported a significantly earlier wake up time than controls: 05:30 ± 0.49 h vs. 07:30 ± 0.51 h, respectively (P < 0.05). The control group reported sleep onset latency 16.2 ± 6.5 min, compared to 13.1 ± 6.3 min for short sleepers. This comparison, as well as sleep efficiency between groups (short sleep = 95.3% ± 1.9% vs. controls = 94.5% ± 1.8%) was not statistically significant.
The mean nap duration in the control group was 13.8 ± 27.2 min/day, and it was not significantly different from nap duration reported by habitual short sleepers (9.3 ± 17.0 min (P < 0.6).
ERP results
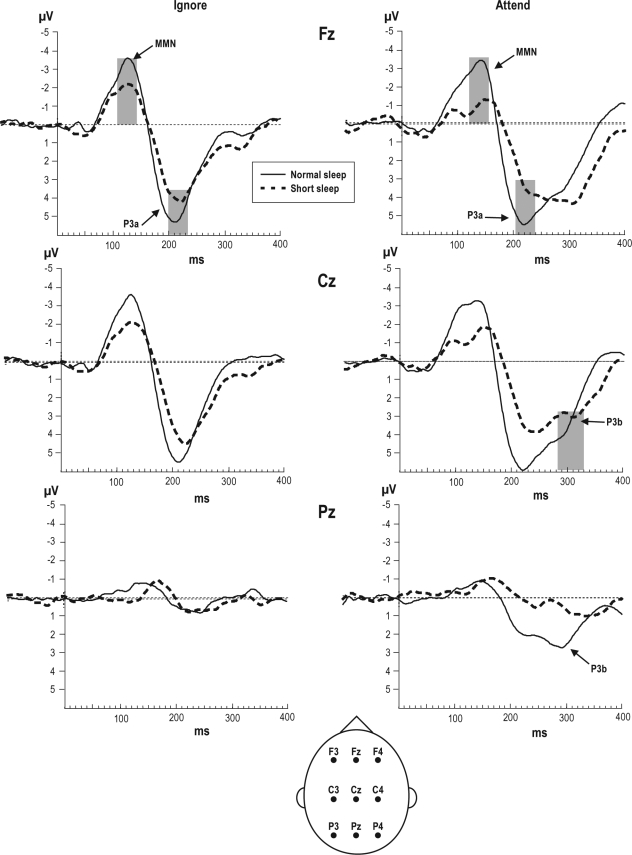
Figure 1 illustrates the ERP difference-waveforms between controls and short sleepers in both the ignore and attend task conditions for MMN, P3a, and P3b amplitudes. For the MMN amplitude, there was a significant main effect for group (F1,17 = 7.60; P < 0.01) across tasks and electrodes, indicating that normal sleepers have higher MMN amplitude than short sleepers. The main effect for cortical region differences was significant (F8,136 = 2.65; P < 0.001), confirming elevated amplitude for frontal and central electrodes as compared to parietal. The group × task × frontality interaction across 3 frontal, 3 central, and 3 parietal electrodes was significant (F8,136 = 2.40; P < 0.01). Post hoc tests revealed that the mean amplitude of the MMN was significantly reduced over frontal and central electrode sites in short sleepers in the ignore and attend tasks compared to controls (P < 0.05). This difference was minimal and did not reach statistical significance between task conditions or between groups over parietal electrodes. Also, in short sleepers the mean amplitude of the MMN at the Fz electrode was significantly reduced in the attend task (−0.14 ± 0.5 μV) as compared to the ignore task (−1.47 ± 0.8 μV) (P < 0.001).
Figure 1.
Group average ERP - difference waveforms (ERPs to novel sounds minus ERPs to standard tone) obtained from normal sleeping and short sleeping individuals in “ignore” and “attend” tasks. The gray bar indicates the latency time window for analyzed mean amplitude of the MMN, P3a, and P3b components with significant differences between groups (for details see results). The schematic illustration of the head with positions of frontal (F3, Fz, and F4), central (C3, Cz and C4), and parietal (P3, Pz, and P4) electrodes selected for statistical evaluation is on the bottom of the figure.
The large positive polarity P3a response with a frontocentral scalp distribution was observed in both task conditions and in both groups at the latency range of 200-240 ms from sound onset. There were 2 significant main effects found for the P3a amplitude. The main effect of task (F1,17 = 8.34; P < 0.01) was significant, with the P3a in the ignore task being lower in amplitude than in the attend task when all groups and electrodes were combined. The main effect of the cortical region showed a significant difference between frontal, central, and parietal electrodes (F8,136 = 44.06; P < 0.001), with the P3a amplitude being higher at frontal and central leads when compared to parietal. Finally, the group × task × frontality interaction confirmed that the P3a mean amplitude was significantly reduced (F8,136 = 2.96; P < 0.04) in short sleepers compared to controls (see Figure 1). Post hoc tests revealed that the largest difference between groups in the ignore task was observed at Fz (4.7 ± 0.9 μV [control] vs. 3.9 ± 1.2 μV [short sleep], P < 0.03) and at Cz (4.9 ± 0.8 μV [control] vs. 4.0 ± 1.3 μV [short sleep], P < 0.05) electrodes, whereas at Pz there were no significant differences between groups (2.6 ± 1.0 μV vs. 2.3 ± 0.7 μV, n.s.).
In the attend task, the post hoc test revealed that short sleepers had significantly reduced amplitude compared to controls at all electrode sites. For example, frontal (Fz) amplitude was 5.0 ± 0.5 μV (short sleep) vs. 5.7 ± 0.8 μV (controls; P < 0.02); at central (Cz) it was 4.5 ± 1.0 μV (short sleep) vs. 6.1 ± 0.9 μV (controls; P < 0.001); and at parietal (Pz) it was 4.4 ± 0.9 μV (controls) vs. 2.6 ± 1.2 μV (short sleep; P < 0.0001).
In the attend task, in order to detect the target sound among all auditory stimuli presented, our participants were instructed to focus their attention on sounds. This active and focused attention elicits the P3b brain response at a latency of 280-320 ms from sound onset. Typically, the P3b amplitude decreases from centroparietal to frontal sites, as observed in the control subjects. However, we found a group × frontality interaction (F2,34 = 16.88; P < 0.01), confirming a mean amplitude of P3b at Fz being significantly higher in short sleepers (4.6 ± 1.2 μV) than in controls (2.3 ± 0.7 μV; P < 0.002), while at the Pz electrode, the amplitude of P3b was significantly higher in controls (4.1 ± 1.0 μV) than in short sleepers (2.1 ± 0.7 μV; P < 0.002). Differences did not reach statistical value at the central electrode site, 4.8 ± 1.2 μV (controls) vs. 3.4 ± 1.1 μV (short sleepers; P > 0.05).
In addition to the amplitude difference between groups, there was also a latency difference for time to peak amplitude of the P3b response (see Figure 1, attend task), with short sleepers having a longer latency than controls. Specifically, at the Pz electrode this latency difference for the P3b peak was 316 ± 16 ms (short sleepers) vs. 284 ± 17 ms (controls) (P < 0.01).
Study II: Sleep Extension in Short Sleepers
Diary sleep parameters
The two sleep conditions were separated by one week with habitual sleep time in bed monitored by sleep diary. The mean nightly sleep duration was 6.0 ± 0.5 h across the 7 nights intervening between study conditions.
Diary data
For the sleep diary data, there was a statistically significant difference between short and extended sleep conditions in TST (5.4 ± 0.5 h vs. 7.9 ± 0.3 h, respectively; t = −14.27, P < 0.001). Sleep latency (13.8 ± 6 min [habitual] vs. 18.0 ± 7 min [extended]) and sleep efficiency (95.3% ± 1.9% [habitual] vs. 90.2% ± 2% [extended]) were not significantly different between conditions.
During the habitual short sleep condition, subjects had a mean nap duration of 9.3 ± 17.0 min per night, which was not significantly different from the mean nap duration during the extended sleep condition, 2.6 ± 4.4 min (P < 0.2).
Objective sleep parameters
Table 1 presents the means and standard deviations for sleep parameters recorded by the Zeo device in habitual vs. extended sleep conditions in short sleepers.
Table 1.
Sleep data (means and ± SD) in habitual and extended sleep across 7 nights
| Habitual Short Sleep | Extended Sleep | P value | |
|---|---|---|---|
| TST (h) | 5.7 ± 0.5 | 7.4 ± 0.6 | P < 0.002 |
| SE (%) | 92.9 ± 4.2 | 90.3 ± 5 | n.s. |
| LPS (min) | 9.6 ± 5.6 | 19.2 ± 13.0 | P < 0.04 |
| Stage 1 and 2 sleep (min) | 203.6 ± 35.0 | 271 ± 37.1 | P < 0.003 |
| SWS (min) | 48.5 ± 22.0 | 52.6 ± 20.0 | n.s. |
| REM (min) | 90.0 ± 22.0 | 120.2 ± 34.0 | n.s. |
| WTDS (min) | 7.3 ± 7.0 | 18.8 ± 10.0 | P < 0.01 |
TST, total sleep time; SE, sleep efficiency; LPS, latency to persistent sleep; SWS, slow wave sleep; WTDS, wake time during sleep; n.s., P > 0.05.
Total sleep time was significantly increased (+1.7 h) during one week of extended time in bed as compared to habitual short sleep (TIB ≤ 6 h). Latency to persistent sleep and wake time during sleep were significantly longer in extended sleep vs. habitual short sleep. The increase in TST was due mainly to an increase in stages 1 and 2 sleep, while REM and SWS were not significantly different between conditions.
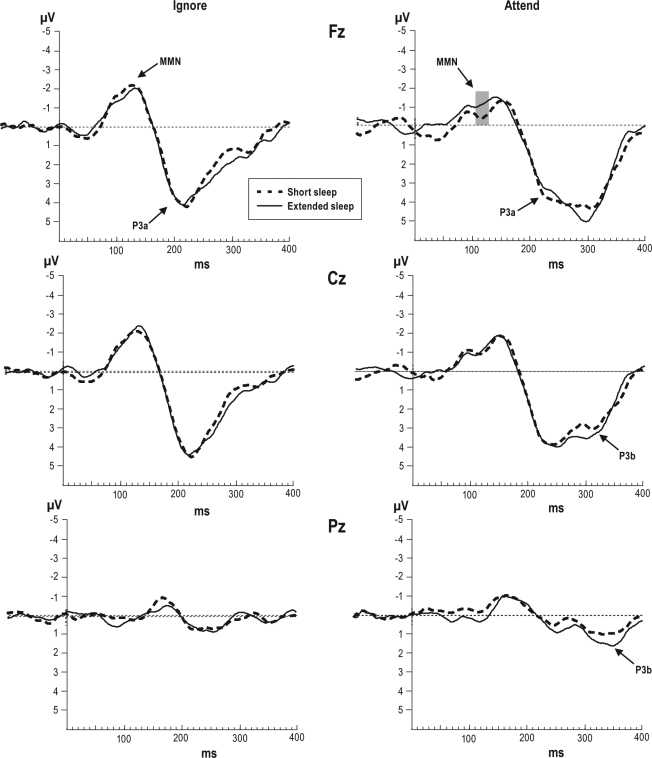
ERP results
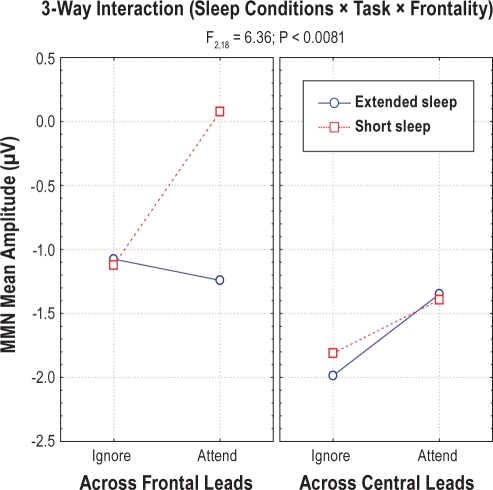
Figure 2 depicts difference-waveforms of ERPs to novel minus ERPs to standard tones for both task conditions and both sleep conditions. There was a significant main effect for frontality (F8,72 = 1.99; P < 0.05) confirming the MMN amplitude being lower for frontal electrodes than in central. A 2-way interaction: sleep condition × frontality (F8,72 = 2.31; P < 0.03) confirmed that the amplitude of MMN was lower following one week of habitual sleep than after one week of extended sleep over all frontal electrodes (F3, Fz, and F4). The 2-way interaction: task × frontality (F8,72 = 2.57; P < 0.01) confirmed that during the passive task, the MMN amplitude was higher over frontal electrodes than during the active task when all sleep conditions were combined. Finally, there was a 3-way interaction: sleep condition × task × frontality for the MMN amplitude (F2,18 = 6.36; P < 0.008). Post hoc tests revealed that there were no differences between sleep conditions for the MMN amplitude in the ignore task (−1.07 μV [habitual short sleep] vs. − 1.20 μV [extended sleep; P > 0.05]). In contrast, during the attend task, the MMN amplitude was significantly increased over frontal areas following extended sleep (−1.25 ± 0.5 μV across F3, Fz, and F4 [P < 0.05; Figure 3]) but not over central as compared to the habitual short sleep schedule.
Figure 2.
Group average ERP-difference waveforms obtained from short sleeping subjects after habitual sleep and extended sleep for ignore and attended tasks. The gray bar is indicating significant differences between sleep conditions for the MMN component (for details see results).
Figure 3.
Graph for 3-way interactions (sleep conditions × task × frontality) illustrating reduction of the MMN amplitude in “attend” task over frontal electrodes after short sleep with respect to extended sleep in habitually short sleeping individuals. Note this difference between tasks was minimal over central electrodes.
Observation of the individual subject data for the MMN shows that 80% of our short sleepers demonstrated increased MMN amplitude after sleep extension with respect to the MMN associated with habitual sleep.
The main effect for the P3a amplitude (see Figure 2) was significant for task condition (F1,9 = 25.5; P < 0.01), with a lower P3a amplitude for the ignore task compared with the attend task when sleep conditions were combined across all electrodes. The main effect for frontality was significant (F8,72 = 10.4; P < 0.001), confirming a higher amplitude of the P3a over frontal and central brain areas compared to parietal when sleep conditions and task conditions were combined. Finally, the 2-way interaction: task × frontality (F8,72 = 25.4; P < 0.001) confirmed that the amplitude of the P3a was lower at frontal (Fz and F4) electrodes in the attend task compared to the ignore task when sleep conditions were combined. The mean amplitude of the P3a in attend task was not significantly different between sleep conditions (P > 0.05).
The mean amplitude of the P3b response (Figure 2) was not different between habitual vs. extended sleep at the Fz, Cz, and Pz electrodes; however, there was an increase in amplitude following the extended sleep condition (at Pz = 3.0 ± 1.0 μV) with respect to habitual sleep (at Pz = 2.1 ± 0.6 μV), but it was not significant (P = 0.7).
The latency of the peak amplitude for the P3b response was similar between sleep conditions (P > 0.05).
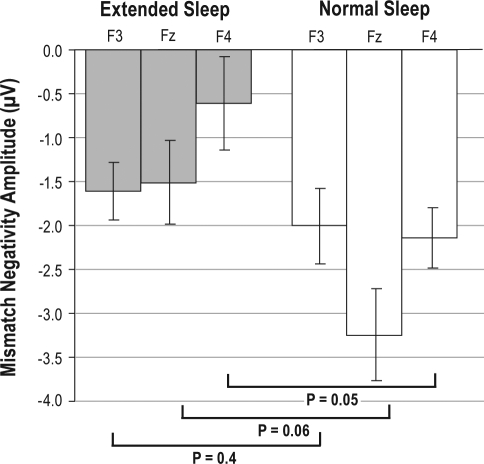
ERPs in extended sleep vs. controls
Figure 4 illustrates that the MMN amplitude in the attend task was larger in controls than in short sleepers after extended sleep. The t-test confirmed significant differences between controls and extended sleep for the right frontal electrode (at F4), while amplitude of the MMN at Fz and F3 electrodes did not reach statistical significance. This lack of significance reveals that the MMN after sleep extension increased to levels similar to the control group at Fz and F3 electrodes (P < 0.4 and P < 0.06, respectively). In contrast, differences at F4 indicate that MMN amplitude did not increase to the level of controls following the 1-week sleep extension condition.
Figure 4.
Illustration of recovery of the MMN amplitude after sleep extension in habitually short sleeping individuals with respect to normally sleeping subjects.
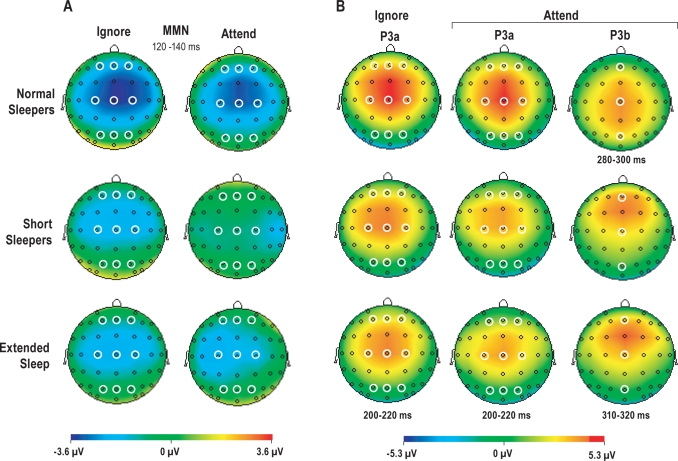
Figure 5 illustrates ERP results of a voltage mapping of electrophysiological activity associated with ignore and attend tasks and highlights differences in brain activity underlying the MMN (coded in blue) and P3a (coded in red) between groups. The MMN and P3a responses that were measured at 9 electrodes and statistically evaluated for the differences are shown on the topographical maps (Figure 5). In the ignore task, habitual short and extended sleep were associated with lower electrophysiological activity underlying the MMN (Figure 5A) and P3a (Figure 5B) as compared to normal sleepers. In the attend task, during the habitual short sleep schedule there was minimal activity related to the MMN and reduced activity related to P3a as compared to the extended sleep condition and the control group. Importantly, sleep extension appeared to improve MMN activity, but did not reach the same level of activity seen in normal sleepers. The topographic distribution of electrical activity underlying the P3b response illustrates a more anterior location relative to normal sleepers. These observations are in correspondence with the statistical evaluation of the amplitude and latency associated with MMN, P3a, and P3b components.
Figure 5.
Topographic scalp distribution of brain potentials associated with the MMN and P3a in ignore and the MMN, P3a, and P3b in attend tasks. The time latencies are corresponding to each ERP component recorded from normal sleeping individuals (n = 9) as compared to short sleeping participants (n = 10) after habitual vs. extended sleep. The open circles on the maps indicate the electrodes selected for comparison of the brain responses and statistical evaluation.
DISCUSSION
The main findings of the present study show that habitually short sleeping individuals have deficiency in activity of the MMN and P3a brain responses over frontal areas as compared to normal sleeping subjects. The P3b amplitude increased over frontal areas and decreased over parietal with respect to the control group. Furthermore, one week of sleep extension was enough to partially normalize frontal counterpart of the MMN brain response in habitually short sleeping individuals, while attention-dependent brain responses (P3a and P3b) did not recover after one week of sleep extension.
This study supports the growing literature demonstrating that shortened sleep time negatively affects various aspects of cognitive functioning and performance, including reduced alertness,6,7 impaired psychomotor performance,8,36 increased risk-taking,37 and impaired performance in complex cognitive behavioral tasks.38
The present study adds to that literature by demonstrating that habitual short sleep is associated with deficits in frontal neuronal processing of novelty. Our results show that the MMN in the ignore and attend task was significantly reduced in short sleepers compared to controls. However, the greatest reduction of the MMN amplitude was observed during the attend task over frontal electrodes relative to the rest of the brain in the short sleep condition as compared to extended sleep. The MMN is characterized as an index of pre-attentive sensory memory operations in detection of changes in the auditory stream; our results suggest that habitual short sleep reduces the efficiency of this frontal mechanism, especially with regard to tasks that require attention. Extension of time in bed for one week increased total sleep time (from 5.7 h to 7.4 h) and concomitantly MMN amplitude increased from −0.1 μV up to −1.25 μV across frontal electrodes (F3, Fz, and F4). We did not find a significant correlation between increased sleep duration and the MMN response. In control subjects the mean amplitude of the MMN across frontal electrodes was −2.3 μV in the attend task, suggesting that sleep extension did, at least in part, normalize neurophysiological deficits in short sleepers in this attentional task, although a similar additional increase (∼1 μV) would be required for complete normalization of the habitual short sleepers. The lack of complete recovery after sleep extension might be related to the relatively short period of extension, both in terms of number of nights as well as hours per night. Chronic short sleepers may require an additional week of sleep extension for normalization of their neurophysiological impaired processes. In fact, while one week of sleep extension in a previous study did not produce normalization of alertness10 a subsequent study providing two weeks of sleep extension (TIB = 10 h) did provide evidence of normalization of alertness.12 Thus, an additional week of sleep extension in the present study may have further improved the MMN deficits to a point where impairments were no longer present. Future studies with longer duration sleep extension are required to test this possibility.
Based on the results of the ignore task of study II, the lack of ERP-differences between extended and habitual short sleep suggest a potential adaptation effect to chronic sleep restriction of neuronal network as compared to ERPs in normal sleeping subjects. Such an interpretation is consistent with a previous sleep restriction study, showing that when sleep is reduced gradually (as with chronic sleep restriction) adaptive processes occur which minimize expected impairments relative to similar amounts of sleep loss experienced rapidly.7 However, when the attentional system is challenged in an attend task, the deficits in frontal regions involved in novelty processing are exposed, reflected by a greater reduction of the MMN amplitude in short sleepers. This latter result is consistent with numerous sleep deprivation studies, which show that more complex tasks requiring greater levels of attentional processing are more sensitive to the effects of sleep deprivation.38
In a previous sleep deprivation study,39 it was shown that the degradation of the pre-attentive processes which is reflected by the MMN response may also lead to disruption of the “reflexive shift” of attention to novelty. Our ERP results (illustrated in Figure 5) show this difference in brain activity associated with an attention switch (P3a response) between controls and short sleepers. The sleep extension period did not alter the P3a amplitude in either the ignore or the attend task-conditions. Therefore, our finding suggests that this process is impaired in short sleepers and not recovered after one week of sleep extension. This result is consistent with the study of Salmi et al.,40 which also suggests that the involuntary attention switching system (reflected by the P3a) is sensitive to sleep duration reduction, and suggests that some types of tasks may require substantially longer periods for full recovery. Alternatively, such deficits may not fully recover in chronic short sleepers.
A recent study done by Gosselin et al.20 demonstrated the effects of total sleep deprivation on novelty detection in an attended sound stream. Their finding suggests a “deactivation” of frontal regions associated with total sleep deprivation, as reflected by a reduction of the P3a amplitude. The authors also found the amplitude of the “P300” response (to novelty and to target) increased over parietal areas in sleep deprived subjects as compared to controls. They suggested that these amplitude enhancements might reflect a compensatory process in specific brain areas. A positron emission tomography study by Thomas et al.41 provided evidence that 24 hours of sleep deprivation produces global decreases in activity across all brain areas, with larger reductions in activity of the thalamus, prefrontal, and posterior parietal cortices involved in attentional and memory functions. Another sleep deprivation (restriction) study demonstrated a differential regional brain response to continuous (one week) sleep restriction by 33% per night.42 In this study, there is EEG/ERP evidence of the immediate response (after day one) to sleep restriction by reduced activity in frontal regions, while parietal regions showed maintenance of function until restriction progressed (after fourth day). More studies are needed to investigate this differential brain-regional response to sleep deprivation and chronic sleep restriction conditions.
In the attend task condition, in addition to a reduction of neuronal activity underlying the MMN and P3a responses in short sleeping individuals, we found increased amplitude and latency prolonged for the P3b response over frontal brain regions in short sleepers compared to controls. In fMRI studies on normal healthy subjects using a novelty task found that the P3a response appears related to the neural changes in the anterior cingulate when incoming stimuli replace the contents of working memory. Communication of this representational change is transmitted to infero-temporal lobe representation maintenance mechanisms.43,44
The P3b response results from memory storage operations that are initiated in the hippocampal formation with the updated output transmitted to parietal cortex.45 Thus, P3a is produced when a demanding stimulus commands frontal lobe attention; P3b is produced when attention resources are allocated for memory updating in association cortex. It is possible that acute total sleep deprivation impacts anterior cingulate and hippocampal formation differently from the impact associated with chronic sleep restriction. The increased amplitude of the P3b at the frontal electrode in the present study might be related to a compensatory mechanism for impaired frontal attention involved in the memory updating processes and occurs with chronic restriction of sleep but not acute sleep loss. Previous neuroimaging (fMRI) investigations have found that some verbal learning tasks are associated with a compensatory brain response (stronger linear responses) in several brain regions, including bilateral temporal, parietal lobes, and prefrontal cortex to short duration and more difficult tasks.46 These regions are highly significant for attention and memory. The prolonged wakefulness produces a decrease in metabolic rates in widespread cortical and subcortical areas, specifically in the thalamus, hypothalamus, and brainstem reticular formation.41,47 The reduction of the P3b amplitude in habitual short sleepers over parietal areas might be explained by the reduction of activity in parietal cortex in response to the prolonged wakefulness.
In our previous study,22 we found hyperactivation in novelty processing in shift work disorder subjects known to experience chronic sleep loss. Thus, the increased frontal brain activity underlying late ERP components at a latency of ∼250-320 ms in auditory processing may be associated with reduced sleep. In fact, insomnia patients show an increased N1 ERP component to rare (or deviant) auditory stimuli during the sleep initiation process48 and upon morning awakening49 as a result of possible cortical hyperarousal.50 However, an ERP study on P300 brain response, done by Devoto et al.51 suggested that cortical hyperarousal is not a “stable individual characteristic” of insomnia, but rather is associated directly with the poor quality of patient's nocturnal sleep of the prior night. Thus, sleep loss may differently affect the brain regions involved in attention and memory, and importantly, the compensation of the network also may contribute to the reduction of the MMN and P3a and increasing P3b responses to chronic sleep restriction. Finally, in a clinical fMRI study in primary insomnia, the authors demonstrated the recovery effect of the prefrontal brain region after 6 weeks of intensive behavioral therapy.52 In our study, we found that the neuronal process associated with automatic change detection function may recover after one week of sleep extension, whereas attention-dependent neural processes do not normalize after this period of time in habitually short sleeping individuals and may require longer recovery periods. Further studies are required to confirm this possibility and to understand more about compensatory mechanisms of the neuronal network involved in the response to sleep loss and chronic sleep restriction.
In conjunction with previous behavioral-ERP studies looking at the relation between function and ERP measures, it is important to emphasize that the three cognitive components measured in our study (MMN, P3a, and P3b) have been utilized in clinical and basic research intensively and have established clinical utility. Moreover, each of these components has been operationally related to neurocognitive processes such as stimulus change-detection, sensory memory formation, novelty detection, orienting attention to new events, target detection, memory updates, and decision making.32 Since our study was carried out on healthy subjects, it would be logical to compare our results to previous literature addressing healthy populations where it was shown that the inter-individual differences or abilities to learn and process information can be measured by behavioral performance and ERPs such as the MMN, P3a, and P3b. Thus, in a fundamental study of the MMN component in regard to development of a memory trace for a complex sound, Näätänen and colleagues53 demonstrated differences between good and poor learners of complex sound discrimination and processing. In that study, it was shown that subjects with a 93% correct response rate showed amplitude of the MMN of −1.4 μV with no further increase, even after intensive training. In contrast, if a participant had 19% hit rate, there was no MMN amplitude elicited to the complex sounds. Further, there were some “middle” learners who improved their behavioral performance and corresponding MMN amplitude with further training from 0.20 μV to −1.12 μV. In a study combining the MMN with psychophysical indexes of perceptual accuracy of the sound duration, Amenedo and Escera54 demonstrated how the brain can detect decreasing or increasing changes in the duration of a tone and predict the accuracy of the behavioral detection of these same changes as indicated by MMN amplitude. This combined ERP-behavioral study of distractibility demonstrated the relation between prolonged reaction time due to load of working memory and P3a amplitude attenuation elicited by novel sounds in relation to not loaded working memory condition in healthy subjects.55
In relating these simultaneous behavioral-ERP results and our findings, there may be a link that indicates short sleepers have less ability to learn new information, and their attention capacity as well as their memory related function is likely limited compared to normal sleeping subjects. However, new studies need to be conducted to further investigate this link.
The question arises as to whether the short sleepers in the current study exemplify trait short sleepers where sleep need may be less than that typically seen in the general population or rather are state short sleepers where their habitual short sleep habits prevent them from obtaining adequate sleep. Although the initial evaluation could not clearly differentiate these possibilities, the findings from both studies favor the latter interpretation. For example, the ERP data associated with the habitual short sleep condition showed significantly lower MMN, P3a, and P3b amplitudes as compared to the ERP data obtained from normal sleeping individuals (i.e., control group). Further, the extended time in bed significantly increased TST in short sleepers. This finding is in correspondence with previous studies demonstrating that as time in bed increases, both TST and alertness increase.10,12 Moreover, our ERP results show that short sleepers after extended sleep have enhancement (i.e., towards normalization) of the MMN brain response as compared to the MMN during habitual short sleep. The implications of our findings contribute to the conclusion that our short sleepers correspond to a “state” rather than “trait” group.
DISCLOSURE STATEMENT
This study was partially supported (e.g., subjects compensation) by ZEO Inc. Dr. Roth has received research support from Aventis, Cephalon, GlaxoSmithKline, Neurocrine, Pfizer, Sanofi-Aventis, Schering Plough, Sepracor, Somaxon, Syrex, Takeda, TransOral, Wyeth, XenoPort; has consulted for Abbott, Accadia, Acoglix, Actelion, Alchemers, Alza, Ancil, Arena, AstraZeneca, Aventis, BMS, Cephalon, Cypress, Dove, Elan, Eli Lilly, Evotec, Forest, GlaxoSmithKline, Hypnion, Johnson and Johnson, King, Ludbeck, McNeil, MediciNova, Merck, Neurim, Neurocrine, Neurogen, Novartis, Orexo, Organon, Orginer, Prestwick, Procter and Gamble, Pfizer, Purdue, Resteva, Roche, Sanofi, Schering Plough, Sepracor, Servier, Shire, Somaxon, Syrex, Takeda, TransOral, Vanda, Vivometrics, Wyeth, Yamanuchi, and XenoPort and has participated in speaking engagements for Sanofi, Cephalon, and Takeda. Dr. Drake has received research support from Merck, Inc., Cephalon, Zeio, Inc., and Takeda. He has also participated in speaking engagements for Cephalon and Asante Communications. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Ashley Kick, BS, and Sarah Eklov, BA, for their great help with data collection on this research.
REFERENCES
- 1.Knutson KL, Van Cauter E, Rathouz PJ, DeLeire T, Lauderdale DS. Trends in the prevalence of short sleepers in the USA: 1975-2006. Sleep. 2010;33:37–45. doi: 10.1093/sleep/33.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh M, Drake CL, Roehrs T, Hudgel DW, Roth T. The association between obesity and short sleep duration: a population-based study. J Clin Sleep Med. 2005;1:357–63. [PubMed] [Google Scholar]
- 3.Spiegel K, Tasali E, Leproult R, Van Cauter E. Effects of poor and short sleep on glucose metabolism and obesity risk. Nat Rev. 2009;5:253–61. doi: 10.1038/nrendo.2009.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Cauter E, Spiegel K, Tasali E, Leproult R. Metabolic consequences of sleep and sleep loss. Sleep Med. 2008;9(Suppl 1):S23–8. doi: 10.1016/S1389-9457(08)70013-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 33:585–92. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dinges DF, Pack F, Williams K, et al. Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4-5 hours per night. Sleep. 1997;20:267–77. [PubMed] [Google Scholar]
- 7.Drake CL, Roehrs TA, Burduvali E, Bonahoom A, Rosekind M, Roth T. Effects of rapid versus slow accumulation of eight hours of sleep loss. Psychophysiology. 2001;38:979–87. doi: 10.1111/1469-8986.3860979. [DOI] [PubMed] [Google Scholar]
- 8.Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:117–26. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 9.Kamdar BB, Kaplan KA, Kezirian EJ, Dement WC. The impact of extended sleep on daytime alertness, vigilance, and mood. Sleep Med. 2004;5:441–8. doi: 10.1016/j.sleep.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 10.Roehrs T, Timms V, Zwyghuizen-Doorenbos A, Roth T. Sleep extension in sleepy and alert normals. Sleep. 1989;12:449–57. doi: 10.1093/sleep/12.5.449. [DOI] [PubMed] [Google Scholar]
- 11.Rupp TL, Wesensten NJ, Balkin TJ. Sleep history affects task acquisition during subsequent sleep restriction and recovery. J Sleep Res. 2010;19:289–97. doi: 10.1111/j.1365-2869.2009.00800.x. [DOI] [PubMed] [Google Scholar]
- 12.Roehrs T, Shore E, Papineau K, Rosenthal L, Roth T. A two-week sleep extension in sleepy normals. Sleep. 1996;19:576–82. [PubMed] [Google Scholar]
- 13.Nieuwenhuis S, Yeung N. Neural mechanisms of attention and control: losing our inhibitions? Nat Neurosci. 2005;8:1631–3. doi: 10.1038/nn1205-1631. [DOI] [PubMed] [Google Scholar]
- 14.Giard MH, Fort A, Mouchetant-Rostaing Y, Pernier J. Neurophysiological mechanisms of auditory selective attention in humans. Front Biosci. 2000;5:84–94. doi: 10.2741/giard. [DOI] [PubMed] [Google Scholar]
- 15.Perrin F, Bertrand O, Giard MH, Pernier J. Precautions in topographic mapping and in evoked potential map reading. J Clin Neurophysiol. 1990;7:498–506. doi: 10.1097/00004691-199010000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Broadbent DE. Perception and communication. New York: Pergamon Press; 1958. [Google Scholar]
- 17.Cowan N. Sensory memory and its role in information processing. Electroencephalogr Clin Neurophysiol. 1995;44:21–31. [PubMed] [Google Scholar]
- 18.Näätänen R. Attention and brain function. Hillsdale, NJ: L. Erlbaum; 1992. [Google Scholar]
- 19.James W Rouben Mamoulian Collection. The principles of psychology. New York: H. Holt; 1890. [Google Scholar]
- 20.Gosselin A, De Koninck J, Campbell KB. Total sleep deprivation and novelty processing: implications for frontal lobe functioning. Clin Neurophysiol. 2005;116:211–22. doi: 10.1016/j.clinph.2004.07.033. [DOI] [PubMed] [Google Scholar]
- 21.Santhi N, Horowitz TS, Duffy JF, Czeisler CA. Acute sleep deprivation and circadian misalignment associated with transition onto the first night of work impairs visual selective attention. PloS One. 2007;2:1233. doi: 10.1371/journal.pone.0001233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gumenyuk V, Roth T, Korzyukov O, et al. Shift work sleep disorder is associated with an attenuated brain response of sensory memory and an increased brain response to novelty: an ERP study. Sleep. 2010;33:703–13. doi: 10.1093/sleep/33.5.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Naatanen R, Winkler I. The concept of auditory stimulus representation in cognitive neuroscience. Psychol Bull. 1999;125:826–59. doi: 10.1037/0033-2909.125.6.826. [DOI] [PubMed] [Google Scholar]
- 24.Picton TW, Alain C, Otten L, Ritter W, Achim A. Mismatch negativity: different water in the same river. Audiol Neurootol. 2000;5:111–39. doi: 10.1159/000013875. [DOI] [PubMed] [Google Scholar]
- 25.Sussman E, Winkler I. Dynamic sensory updating in the auditory system. Brain Res. 2001;12:431–9. doi: 10.1016/s0926-6410(01)00067-2. [DOI] [PubMed] [Google Scholar]
- 26.Alho K, Woods DL, Algazi A, Knight RT, Naatanen R. Lesions of frontal cortex diminish the auditory mismatch negativity. Electroencephalogr Clin Neurophysiol. 1994;91:353–62. doi: 10.1016/0013-4694(94)00173-1. [DOI] [PubMed] [Google Scholar]
- 27.Escera C, Alho K, Schroger E, Winkler I. Involuntary attention and distractibility as evaluated with event-related brain potentials. Audiol Neurootol. 2000;5:151–66. doi: 10.1159/000013877. [DOI] [PubMed] [Google Scholar]
- 28.Friedman D, Cycowicz YM, Gaeta H. The novelty P3: an event-related brain potential (ERP) sign of the brain's evaluation of novelty. Neurosci Behav Rev. 2001;25:355–73. doi: 10.1016/s0149-7634(01)00019-7. [DOI] [PubMed] [Google Scholar]
- 29.Knight RT. Decreased response to novel stimuli after prefrontal lesions in man. Electroencephalogr Clin Neurophysiol. 1984;59:9–20. doi: 10.1016/0168-5597(84)90016-9. [DOI] [PubMed] [Google Scholar]
- 30.Knight RT, Nakada T. Cortico-limbic circuits and novelty: a review of EEG and blood flow data. Rev Neurosci. 1998;9:57–70. doi: 10.1515/revneuro.1998.9.1.57. [DOI] [PubMed] [Google Scholar]
- 31.Squires KC, Squires NK, Hillyard SA. Decision-related cortical potentials during an auditory signal detection task with cued observation intervals. J Exp Psychol. 1975;1:268–79. doi: 10.1037//0096-1523.1.3.268. [DOI] [PubMed] [Google Scholar]
- 32.Duncan CC, Barry RJ, Connolly JF, et al. Event-related potentials in clinical research: guidelines for eliciting, recording, and quantifying mismatch negativity, P300, and N400. Clin Neurophysiol. 2009;120:1883–908. doi: 10.1016/j.clinph.2009.07.045. [DOI] [PubMed] [Google Scholar]
- 33.Polich J. Updating P300: an integrative theory of P3a and P3b. Clin Neurophysiol. 2007;118:2128–48. doi: 10.1016/j.clinph.2007.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485–91. doi: 10.7326/0003-4819-131-7-199910050-00002. [DOI] [PubMed] [Google Scholar]
- 35.Shambroom JR, Fabregas SE, Johnstone J. Validation of an automated wireless system to monitor sleep in healthy adults. J. Sleep Res. 2011 doi: 10.1111/j.1365-2869.2011.00944.x. (in press) [DOI] [PubMed] [Google Scholar]
- 36.Balkin TJ, Bliese PD, Belenky G, et al. Comparative utility of instruments for monitoring sleepiness-related performance decrements in the operational environment. J Sleep Res. 2004;13:219–27. doi: 10.1111/j.1365-2869.2004.00407.x. [DOI] [PubMed] [Google Scholar]
- 37.Roehrs T, Greenwald M, Roth T. Risk-taking behavior: effects of ethanol, caffeine, and basal sleepiness. Sleep. 2004;27:887–93. doi: 10.1093/sleep/27.5.887. [DOI] [PubMed] [Google Scholar]
- 38.Bonnet MH, Arand DL. Performance and cardiovascular measures in normal adults with extreme MSLT scores and subjective sleepiness levels. Sleep. 2005;28:685–93. doi: 10.1093/sleep/28.6.685. [DOI] [PubMed] [Google Scholar]
- 39.Raz A, Deouell LY, Bentin S. Is pre-attentive processing compromised by prolonged wakefulness? Effects of total sleep deprivation on the mismatch negativity. Psychophysiology. 2001;38:787–95. [PubMed] [Google Scholar]
- 40.Salmi J, Huotilainen M, Pakarinen S, Siren T, Alho K, Aronen ET. Does sleep quality affect involuntary attention switching system? Neurosci Lett. 2005;390:150–5. doi: 10.1016/j.neulet.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 41.Thomas M, Sing H, Belenky G, et al. Neural basis of alertness and cognitive performance impairments during sleepiness. I. Effects of 24 h of sleep deprivation on waking human regional brain activity. J Sleep Res. 2000;9:335–52. doi: 10.1046/j.1365-2869.2000.00225.x. [DOI] [PubMed] [Google Scholar]
- 42.Cote KA, Milner CE, Osip SL, Baker ML, Cuthbert BP. Physiological arousal and attention during a week of continuous sleep restriction. Physiol Behav. 2008;95:353–64. doi: 10.1016/j.physbeh.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 43.McCarthy G, Luby M, Gore J, Goldman-Rakic P. Infrequent events transiently activate human prefrontal and parietal cortex as measured by functional MRI. J Neurophysiol. 1997;77:1630–4. doi: 10.1152/jn.1997.77.3.1630. [DOI] [PubMed] [Google Scholar]
- 44.Verbaten MN, Huyben MA, Kemner C. Processing capacity and the frontal P3. Int J Psychophysiol. 1997;25:237–48. doi: 10.1016/s0167-8760(96)00748-9. [DOI] [PubMed] [Google Scholar]
- 45.Kandel ER, Squire LR. Neuroscience: breaking down scientific barriers to the study of brain and mind. Science. 2000;290:1113–20. doi: 10.1126/science.290.5494.1113. [DOI] [PubMed] [Google Scholar]
- 46.Drummond SP, Brown GG, Salamat JS, Gillin JC. Increasing task difficulty facilitates the cerebral compensatory response to total sleep deprivation. Sleep. 2004;27:445–51. [PubMed] [Google Scholar]
- 47.Dang-Vu TT, Desseilles M, Petit D, Mazza S, Montplaisir J, Maquet P. Neuroimaging in sleep medicine. Sleep Med. 2007;8:349–72. doi: 10.1016/j.sleep.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 48.Yang CM, Lo HS. ERP evidence of enhanced excitatory and reduced inhibitory processes of auditory stimuli during sleep in patients with primary insomnia. Sleep. 2007;30:585–92. doi: 10.1093/sleep/30.5.585. [DOI] [PubMed] [Google Scholar]
- 49.Bastien CH, St-Jean G, Morin CM, Turcotte I, Carrier J. Chronic psychophysiological insomnia: hyperarousal and/or inhibition deficits? An ERPs investigation. Sleep. 2008;31:887–98. doi: 10.1093/sleep/31.6.887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Perlis ML, Smith MT, Andrews PJ, Orff H, Giles DE. Beta/Gamma EEG activity in patients with primary and secondary insomnia and good sleeper controls. Sleep. 2001;24:110–7. doi: 10.1093/sleep/24.1.110. [DOI] [PubMed] [Google Scholar]
- 51.Devoto A, Violani C, Lucidi F, Lombardo C. P300 amplitude in subjects with primary insomnia is modulated by their sleep quality. J Psychosom Res. 2003;54:3–10. doi: 10.1016/s0022-3999(02)00579-2. [DOI] [PubMed] [Google Scholar]
- 52.Altena E, Van Der Werf YD, Sanz-Arigita EJ, et al. Prefrontal hypoactivation and recovery in insomnia. Sleep. 2008;31:1271–6. [PMC free article] [PubMed] [Google Scholar]
- 53.Näätänen R, Schröger E, Karakas S, Tervaniemi M, Paavilainen P. Development of a memory trace for a complex sound in the human brain. Neuroreport. 1993;4:503–6. doi: 10.1097/00001756-199305000-00010. [DOI] [PubMed] [Google Scholar]
- 54.Amenedo E, Escera C. The accuracy of sound duration representation in the human brain determines the accuracy of behavioral perception. Eur J Neurosci. 2000;12:2570–4. doi: 10.1046/j.1460-9568.2000.00114.x. [DOI] [PubMed] [Google Scholar]
- 55.SanMiguel I, Corral MJ, Escera C. When loading working memory reduces distraction: behavioral and electrophysiological evidence from an auditory-visual distraction paradigm. J Cogn Neurosci. 2008;20:1131–45. doi: 10.1162/jocn.2008.20078. [DOI] [PubMed] [Google Scholar]