Abstract
Objective:
Fatigue is a pervasive symptom associated with HIV, resulting in significant functioning impairment; but little is known about its etiology or treatment. In patients with primary insomnia, data have shown improvement in fatigue following successful treatment of insomnia. However, little is known about the role of insomnia in patients with fatigue in HIV. This manuscript seeks to test the hypothesis that insomnia severity is correlated with increased fatigue in HIV-seropositive patients.
Methods:
Fifty-seven ambulatory HIV-seropositive patients, aged 18-60 years, with a DSM-IV-TR diagnosis of insomnia, were administered the Insomnia Severity Index (ISI), Piper Fatigue Scale (PFS), Hospital Anxiety and Depression scale, and Hamilton Depression Rating Scale (HAM-D). Their most recent CD4 count and time since diagnosis of HIV were recorded. Regression analysis was carried out with PFS as the dependent variable.
Results:
A higher ISI score correlated with higher PFS score, (R2 = 0.1713, P = 0.0042). Overall depression severity was not significantly correlated with PFS score, except in the most severely depressed subgroup, in which the HADS depression score was the strongest predictor of PFS (R2 = 0.182, P = 0.0009). In participants without depression, ISI accounted for most of the variance in fatigue (R2 = 0.6035, P = 0.0011).
Conclusions:
Greater insomnia severity is associated with greater fatigue severity in HIV seropositive patients. Depression may contribute to both fatigue and insomnia. In the absence of depression, the treatment of insomnia may emerge as a treatment strategy to help alleviate fatigue. Further studies are needed to confirm these data.
Clinical Trial Information:
Clinical Trials.Gov: The Treatment of Insomnia in Patients with HIV Disease. Registry Number: NCT00465972. URL: http://www.clinicaltrials.gov/ct2/show/NCT00465972?term = HIV+insomnia&rank = 1
Citation:
Low Y; Preud'homme X; Goforth HW; Omonuwa T; Krystal AD. The association of fatigue with depression and insomnia in hiv-seropositive patients: a pilot study. SLEEP 2011;34(12):1723-1726.
Keywords: HIV, insomnia, fatigue, depression
INTRODUCTION
Anti-retroviral therapy, early detection, scheduled monitoring, and prophylaxis against opportunistic infections have transformed the care of HIV into that of a chronic disease with a lengthened life expectancy as compared to a generation ago.1 There is thus a greater need to address aspects of HIV which impact function and quality of life. One of the most important factors affecting function and quality of life in HIV-seropositive patients has been demonstrated to be persistent fatigue.1
Fatigue is a frequent complaint that has been observed throughout the course of HIV. It is a common early presenting symptom, is encountered throughout the course of HIV treatment, and can be debilitating in advanced stages of disease.2–7 HIV-associated fatigue is associated with significant psychiatric and functional morbidity and lower quality of life,2,5,8–10 and is a strong predictor of disability and declining function in work, physical activity, and daily activities.2,8,11–13
Despite the impact of HIV-related fatigue, its etiology is poorly understood, and treatment options are currently limited. Authors have hypothesized that fatigue is a constitutional symptom of HIV resulting from impaired hepatic function,6 endocrine,14 or cytokine dysregulation6; is secondary to depression,5 anemia,15 opportunistic infections or malignancies15; or may be a side effect of certain anti-retrovirals.6 To date, there are reports of improved fatigue in response to desiccated thyroid hormone,16 hyperbaric oxygen,17,18 and psychostimulants19–21 including modafinil.22 While stimulants appear promising, these have been typically reserved for use in advanced stages of disease, where fatigue is debilitating and there is a lack of other intervention options.
One potentially modifiable factor associated with HIV-related fatigue is insomnia. In the HIV-seronegative population, patients with insomnia experience greater fatigue than healthy controls,32 and successful pharmacotherapy of insomnia is associated with improved fatigue33 in this general population. However, this relationship has yet to be studied in HIV-seropositive patients, whose fatigue may be the result of other factors and may be less modifiable through the treatment of insomnia.
There are several reasons why it is important to study the insomnia-fatigue relationship specifically in HIV-seropositive patients. Insomnia is more prevalent in HIV-seropositive patients than the general population.30 In addition to the factors associated with insomnia in the general population, such as mood23–26 and anxiety disorders,27–29 insomnia in HIV-seropositive patients is associated with several HIV-specific factors, including neuronal degeneration from viral infection of the CNS, antiretrovirals like efavirenz, and psychosocial stressors associated with living with HIV.30,31 Further, fatigue is a particularly prevalent and debilitating symptom in HIV-seropositive patients.1–13
The current study is intended to test the hypothesis that insomnia severity is correlated with fatigue severity in HIV-seropositive patients. Because of the established associations between major depression and both of insomnia and fatigue, we also controlled for depression severity and examined whether depression severity was independently associated with fatigue severity.
METHODS
Participants and Setting
HIV-seropositive patients between 18-60 years of age, with a DSM-IV TR diagnosis of insomnia, were recruited through ads and physician referrals at a single academic medical center. Exclusionary criteria were as follows: (1) previous diagnosis of, or a history and physical examination suggesting obstructive sleep apnea (OSA), restless legs syndrome (RLS), periodic movements in sleep (PLMS), frequent nightly urination, or circadian phase-shift disorders; (2) a change in anti-retroviral therapy regimen within the past 30 days; (3) currently using any medication with sedating or stimulant effects, or psychotropic medication; (4) using any investigational drug in the past 30 days; (5) history within the past 6 months of alcohol or substance abuse; (6) having a clinically significant unstable medical condition, neurological disorder including epilepsy, or illness within 30 days of initial screening; or (7) BMI > 34.
Design and Procedures
After signing informed consent, participants were administered the Insomnia Severity Index (ISI),34 Piper Fatigue Scale (PFS),35 Hospital Anxiety and Depression Scale (HADS),36 and Hamilton-Depression Scale (HAM-D).37 The PFS was chosen for measuring fatigue because it is a commonly used scale for measuring fatigue in HIV patients to date. Each participant's most recent CD4 count and current anti-retroviral medication use were recorded, and they were also asked to recall the date of HIV diagnosis, which was used as an estimate of the duration of infection.
Data Analysis
A regression analysis in which PFS was the dependent variable was conducted with all other recorded variables as covariates to determine if there was a relationship between ISI and PFS, and if it was mediated by other factors including age, depression, or CD4 count. The depression analyses consisted of separate multiple regression analyses with forward selection of predictor variables (age; sex; ISI, Ham-D, HADS-D, and HADS-A scores; CD4 count; and duration of infection) in the group with greater depressive symptoms (Ham-D > 13; N = 22) and the group with mild or no depressive symptoms (HAM-D ≤ 13; N = 35).38
RESULTS
A total of 57 patients (37 male, 20 female) were recruited. The mean age of participants (± SD) was 47(± 7.6) years; mean CD4 count 475(± 291) cells/mm3; mean duration of infection 14(± 4.3) years; and the mean scores on the ISI, PFS, Ham-D, HADS-A, and HADS-D were 18(± 4.3), 116(± 43), 11(± 4.6), 8.7(± 3.9), and 8.2(± 4.5), respectively (Table 1).
Table 1.
Sample baseline characteristics
| Variable | Mean (SD) |
|---|---|
| Age (years) | 47 (7.6) |
| CD4 (cell/mm3) | 475 (291) |
| Duration of Infection (years) | 14 (4.3) |
| Insomnia Severity Index (ISI) | 18 (4.3) |
| Piper Fatigue Scale (PFS) | 116 (43) |
| Hamilton-D (Ham-D) | 11 (4.6) *Median: 11 |
| Hospital Anxiety & Depression (HADS-A) | 8.7 (3.9) |
| Hospital Anxiety & Depression (HADS-D) | 8.2 (4.5) |
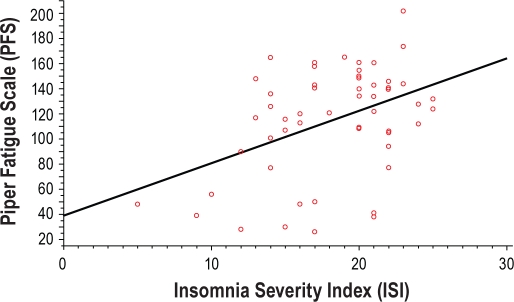
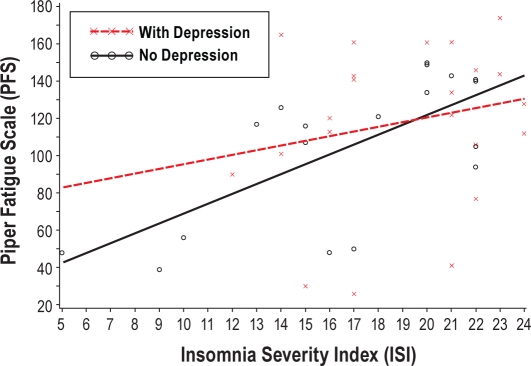
Multiple linear regression analyses showed a positive correlation between ISI and PFS after controlling for HAM-D score and CD4 count (R2 = 0.182, P = 0.0009; see Figure 1). In the subgroup with the more severe depression, the HADS-D score was the strongest correlate of PFS score, accounting for 37.8% of PFS variability (R2 = 0.378, P = 0.0146), while ISI did not contribute significantly to the regression model (Table 2 and Figure 2). In contrast, in those without clinically significant major depression, ISI was the strongest correlate of PFS score, accounting for 62.7% of the variance in PFS (R2 = 0.6035, P = 0.0011; Figure 2).
Figure 1.
There is a positive correlation between ISI and PFS in HIV-seropositive patients (R2 = 0.1804, R = 0.4247, P = 0.0012)
Table 2.
Results of multiple regression analysis in depressed and non-depressed subgroups
| Step | Variable | Partial R2 | Model R2 | C(p) | F-value | Pr > F |
|---|---|---|---|---|---|---|
| DEPRESSION | ||||||
| 1 | HADSD | 0.38 | 0.38 | 2.7 | 7.9 | 0.015 |
| 2 | Age | 0.08 | 0.46 | −1.8 | 1.8 | 0.20 |
| 3 | ISI | 0.10 | 0.56 | −1.1 | 2.5 | 0.14 |
| NO DEPRESSION | ||||||
| 1 | ISI | 0.60 | 0.60 | −3.5 | 18 | 0.0011 |
| 2 | Age | 0.078 | 0.68 | −2.8 | 2.9 | 0.13 |
| 3 | CD4 | 0.041 | 0.72 | −1.45 | 1.5 | 0.25 |
Figure 2.
In the subgroup with depression, there is no significant correlation between PFS and ISI (R2 = 0.1007, P = 0.14). In the subgroup with no depression, there is a significant association between PFS and ISI (R2 = 0.6035, P = 0.0011).
DISCUSSION
In this study, insomnia was significantly correlated with fatigue in HIV-seropositive patients after controlling for depression severity and CD4 count. Further, in those with clinically significant depression, depression severity was the most important correlate of fatigue, whereas in those without significant depression, insomnia severity was the most important correlate, accounting for up to 62.7% of the variance in Piper Fatigue Scale score. Insomnia appears to be an important contributor to fatigue in non-depressed HIV-seropositive patients. However, a possibility that cannot be ruled out is that insomnia and fatigue both have a common antecedent in this population.
The insomnia-fatigue relationship persisted after controlling for CD4, which suggests that the relationship between insomnia and fatigue is not a consequence of current immune function. However, it must be appreciated that CD4 count is a limited measure of immune function, in that it reflects only recent disease control, but not prior poor low CD4 nadirs or history of opportunistic infections. These findings also suggest that the insomnia-fatigue relationship was not mediated by age, anxiety severity, self-reported duration of illness, or total number of medications.
It is possible that there are other factors responsible for the relationship between insomnia and fatigue that were not assessed in this study. However, the data suggest a relationship between insomnia and fatigue in non-depressed HIV-positive individuals such as has been observed in primary insomnia patients. The mechanisms by which fatigue occurs in association with insomnia remains unknown, and determining these mechanisms should be assessed in future research.
The findings of this study also have clinical implications for the assessment of fatigue in HIV-seropositive patients. In general, the findings suggest the need to screen for insomnia and depression as potential contributing factors. When insomnia occurs with significant depression in HIV-seropositive patients, it is likely that the depression is a greater contributor to fatigue than the insomnia, though appropriate treatment for both insomnia and depression is always indicated. However, in the absence of depression, insomnia should be kept in mind as an important contributor to fatigue in this population.
Future Directions
Future studies should be carried out employing polysomnography (PSG) to determine whether fatigue is associated with objective measures of sleep disturbance. Although insomnia is a diagnosis based solely on self-report, objective evidence of sleep disturbance is often present.39 Given the unique nature of insomnia and fatigue in HIV-seropositive patients, it will be important to determine if the fatigue is associated with subjective and not objective sleep indices, as has been reported in HIV-seronegative populations.40
A limitation of this study include that all of the subjects had insomnia and that the subjects were a convenience sample and not a random sample of the general population of HIV-seropositive patients. Thus, future work is needed with improved sampling ability.
The findings of this study also support the need for further studies of the impact of the treatment of insomnia on fatigue in HIV-seropositive patients. A previous fatigue study reported that fatigue improved with the pharmacological treatment of primary insomnia,33 suggesting that the treatment of insomnia could be a useful intervention to reduce HIV-related fatigue, which is a common problem with limited treatment options. However, no placebo-controlled studies of the treatment of insomnia in HIV-seropositive patients have been conducted.
Future studies should take into account drug interactions with commonly used medications like anti-retrovirals and anti-microbials, common comorbidities like substance abuse, and the possibility that there may be a unique pathophysiology of insomnia in HIV.41 Such studies have significant potential for improving the understanding and treatment of fatigue in this at-risk group of individuals.
DISCLOSURE STATEMENT
The results in this manuscript were presented as part of a 10-minute oral presentation, in a session on Sleep disorders and Medical Co-morbidities, on June 7th 2010 at the Sleep 2010 Meeting of the Associated Professional Sleep Societies at San Antonio, Texas. The results have not otherwise been presented or published.
This was not an industry supported study. Dr. Krystal has received grants from the NIH, Sanofi-Aventis, Cephalon, GlaxoSmithKline, Merck, Neurocrine, Pfizer, Sepracor, Somaxon, Takeda, Transcept, Respironics, Neurogen, Evotec, and Astellas. Dr. Krystal is also currently or previously a consultant for Abbott, Actelion, Arena, Astellas, Axiom, AstraZeneca, BMS, Cephalon, Eli Lilly, GlaxoSmithKline, Jazz, Johnson and Johnson, King, Merck, Neurocrine, Neurogen, Neuronetics, Novartis, Organon, Ortho-McNeil-Janssen, Pfizer, Respironics, Roche, Sanofi-Aventis, Sepracor, Somaxon, Takeda, Transcept, Astellas, Research Triangle Institute, Kingsdown Inc., CHDI. Dr. Goforth has consulted for Bristol Myers Squibb and has received grants from Forest Laboratories. He has also served as a speaker for Bristol, Myers, Squibb. Dr. Preud'homme has received research grants from Pfizer, NIDDK, and Astellas. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENT
This Study was funded by the Department of Psychiatry and Behavioral Sciences, Duke University school of Medicine.
ABBREVIATIONS
- HAM-D
Hamilton Depression Rating Scale
- HADS
Hospital Anxiety and Depression Scale
- PFS
Piper Fatigue Scale
- ISI
Insomnia Severity Index
- HIV
human immunodeficiency virus
- OSA
obstructive sleep apnea
- RLS
restless legs syndrome
- PLMS
periodic limb movements in sleep
- HAART
highly active anti-retroviral therapy
- NNRTI
non-nucleoside reverse transcriptase inhibitor
- CDC Stage
Center for Disease Control and Prevention HIV staging system
- HAD
HIV-1 associated dementia
REFERENCES
- 1.Miles SA. HIV infection and AIDS: new biology, therapeutic advances, and clinical implications. Introduction. J Acquir Immune Defic Syndr Hum Retrovirol. 1997;16(Suppl 1):S1–2. [PubMed] [Google Scholar]
- 2.Breitbart W, McDonald MV, Rosenfeld B, Monkman ND, Passik S. Fatigue in ambulatory AIDS patients. J Pain Symptom Manage. 1998;15:159–67. doi: 10.1016/s0885-3924(97)00260-1. [DOI] [PubMed] [Google Scholar]
- 3.Ferrando S, Evans S, Goggin K, Sewell M, Fishman B, Rabkin J. Fatigue in HIV illness: relationship to depression, physical limitations, and disability. Psychosom Med. 1998;60:759–64. doi: 10.1097/00006842-199811000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Vogl D, Rosenfeld B, Breitbart W, et al. Symptom prevalence, characteristics, and distress in AIDS outpatients. J Pain Symptom Manage. 1999;18:253–62. doi: 10.1016/s0885-3924(99)00066-4. [DOI] [PubMed] [Google Scholar]
- 5.Sullivan PS, Dworkin MS. Prevalence and correlates of fatigue among persons with HIV infection. J Pain Symptom Manage. 2003;25:329–33. doi: 10.1016/s0885-3924(02)00676-0. [DOI] [PubMed] [Google Scholar]
- 6.Barroso J. A review of fatigue in people with HIV infection. J Assoc Nurses AIDS Care. 1999;10:42–9. doi: 10.1016/S1055-3290(06)60342-7. [DOI] [PubMed] [Google Scholar]
- 7.Henderson M, Safa F, Easterbrook P, Hotopf M. Fatigue among HIV-infected patients in the era of highly active antiretroviral therapy. HIV Med. 2005;6:347–52. doi: 10.1111/j.1468-1293.2005.00319.x. [DOI] [PubMed] [Google Scholar]
- 8.Cleary PD, Fowler FJ, Jr, Weissman J, et al. Health-related quality of life in persons with acquired immune deficiency syndrome. Med Care. 1993;31:569–80. doi: 10.1097/00005650-199307000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Cunningham WE, Shapiro MF, Hays RD, et al. Constitutional symptoms and health-related quality of life in patients with symptomatic HIV disease. Am J Med. 1998;104:129–36. doi: 10.1016/s0002-9343(97)00349-5. [DOI] [PubMed] [Google Scholar]
- 10.Darko DF, Mitler MM, Miller JC. Growth hormone, fatigue, poor sleep, and disability in HIV infection. Neuroendocrinology. 1998;67:317–24. doi: 10.1159/000054329. [DOI] [PubMed] [Google Scholar]
- 11.Walker K, McGown A, Jantos M, Anson J. Fatigue, depression, and quality of life in HIV-positive men. J Psychosoc Nurs Ment Health Serv. 1997;35:32–40. doi: 10.3928/0279-3695-19970901-17. [DOI] [PubMed] [Google Scholar]
- 12.Semple SJ, Patterson TL, Temoshok LR, et al. Identification of psychobiological stressors among HIV-positive women. HIV Neurobehavioral Research Center (HNRC) Group. Women Health. 1993;20:15–36. doi: 10.1300/J013v20n04_02. [DOI] [PubMed] [Google Scholar]
- 13.Fleishman JA, Crystal S. Functional status transitions and survival in HIV disease: evidence from the AIDS Costs and Service Utilization Survey. Med Care. 1998;36:533–43. doi: 10.1097/00005650-199804000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Abbott M, Khoo SH, Hammer MR, Wilkins EG. Prevalence of cortisol deficiency in late HIV disease. J Infect. 1995;31:1–4. doi: 10.1016/s0163-4453(95)91116-2. [DOI] [PubMed] [Google Scholar]
- 15.Groopman JE. Fatigue in cancer and HIV/AIDS. Oncology (Williston Park) 1998;12:335–44. discussion 45-6, 51. [PubMed] [Google Scholar]
- 16.Derry DM. Thyroid therapy in HIV-infected patients. Med Hypotheses. 1995;45:121–4. doi: 10.1016/0306-9877(95)90058-6. [DOI] [PubMed] [Google Scholar]
- 17.Jordan WC. The effectiveness of intermittent hyperbaric oxygen in relieving drug-induced HIV-associated neuropathy. J Natl Med Assoc. 1998;90:355–8. [PMC free article] [PubMed] [Google Scholar]
- 18.Reillo MR. Hyperbaric oxygen therapy for the treatment of debilitating fatigue associated with HIV/AIDS. J Assoc Nurses AIDS Care. 1993;4:33–8. [PubMed] [Google Scholar]
- 19.Wagner GJ, Rabkin JG, Rabkin R. Dextroamphetamine as a treatment for depression and low energy in AIDS patients: a pilot study. J Psychosom Res. 1997;42:407–11. doi: 10.1016/s0022-3999(96)00366-2. [DOI] [PubMed] [Google Scholar]
- 20.Wagner GJ, Rabkin R. Effects of dextroamphetamine on depression and fatigue in men with HIV: a double-blind, placebo-controlled trial. J Clin Psychiatry. 2000;61:436–40. doi: 10.4088/jcp.v61n0608. [DOI] [PubMed] [Google Scholar]
- 21.Breitbart W, Rosenfeld B, Kaim M, Funesti-Esch J. A randomized, double-blind, placebo-controlled trial of psychostimulants for the treatment of fatigue in ambulatory patients with human immunodeficiency virus disease. Arch Intern Med. 2001;161:411–20. doi: 10.1001/archinte.161.3.411. [DOI] [PubMed] [Google Scholar]
- 22.Rabkin JG, McElhiney MC, Rabkin R, Ferrando SJ. Modafinil treatment for fatigue in HIV+ patients: a pilot study. J Clin Psychiatry. 2004;65:1688–95. doi: 10.4088/jcp.v65n1215. [DOI] [PubMed] [Google Scholar]
- 23.Norman SE, Chediak AD, Freeman C, et al. Sleep disturbances in men with asymptomatic human immunodeficiency (HIV) infection. Sleep. 1992;15:150–5. doi: 10.1093/sleep/15.2.150. [DOI] [PubMed] [Google Scholar]
- 24.Perkins DO, Leserman J, Stern RA, et al. Somatic symptoms and HIV infection: relationship to depressive symptoms and indicators of HIV disease. Am J Psychiatry. 1995;152:1776–81. doi: 10.1176/ajp.152.12.1776. [DOI] [PubMed] [Google Scholar]
- 25.Franck LS, Johnson LM, Lee K, et al. Sleep disturbances in children with human immunodeficiency virus infection. Pediatrics. 1999;104:e62. doi: 10.1542/peds.104.5.e62. [DOI] [PubMed] [Google Scholar]
- 26.Rubinstein ML, Selwyn PA. High prevalence of insomnia in an outpatient population with HIV infection. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;19:260–5. doi: 10.1097/00042560-199811010-00008. [DOI] [PubMed] [Google Scholar]
- 27.Brown S MM, Atkinson H. Correlation of subjective sleep complaints, absolute T-4 cell number and anxiety in HIV illness. Sleep Res. 1991;20:363. [Google Scholar]
- 28.Junqueira P, Bellucci S, Rossini S, Reimao R. Women living with HIV/AIDS: sleep impairment, anxiety and depression symptoms. Arq Neuropsiquiatr. 2008;66:817–20. doi: 10.1590/s0004-282x2008000600008. [DOI] [PubMed] [Google Scholar]
- 29.Lee KA, Portillo CJ, Miramontes H. The influence of sleep and activity patterns on fatigue in women with HIV/AIDS. J Assoc Nurses AIDS Care. 2001;(12 Suppl):19–27. doi: 10.1177/105532901773742257. [DOI] [PubMed] [Google Scholar]
- 30.Reid S, Dwyer J. Insomnia in HIV infection: a systematic review of prevalence, correlates, and management. Psychosom Med. 2005;67:260–9. doi: 10.1097/01.psy.0000151771.46127.df. [DOI] [PubMed] [Google Scholar]
- 31.Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med. 2007;3:S7–10. [PMC free article] [PubMed] [Google Scholar]
- 32.Lichstein KL, Means MK, Noe SL, Aguillard RN. Fatigue and sleep disorders. Behav Res Ther. 1997;35:733–40. doi: 10.1016/s0005-7967(97)00029-6. [DOI] [PubMed] [Google Scholar]
- 33.Walsh JK, Krystal AD, Amato DA, et al. Nightly treatment of primary insomnia with eszopiclone for six months: effect on sleep, quality of life, and work limitations. Sleep. 2007;30:959–68. doi: 10.1093/sleep/30.8.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 35.Piper BF, Dibble SL, Dodd MJ, Weiss MC, Slaughter RE, Paul SM. The revised Piper Fatigue Scale: psychometric evaluation in women with breast cancer. Oncol Nurs Forum. 1998;25:677–84. [PubMed] [Google Scholar]
- 36.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 37.Faries D, Herrera J, Rayamajhi J, DeBrota D, Demitrack M, Potter WZ. The responsiveness of the Hamilton Depression Rating Scale. J Psychiatr Res. 2000;34:3–10. doi: 10.1016/s0022-3956(99)00037-0. [DOI] [PubMed] [Google Scholar]
- 38.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Krystal AD, Edinger JD, Wohlgemuth WK, Marsh GR. NREM sleep EEG frequency spectral correlates of sleep complaints in primary insomnia subtypes. Sleep. 2002;25:630–40. [PubMed] [Google Scholar]
- 40.Watson NF, Kapur V, Arguelles LM, et al. Comparison of subjective and objective measures of insomnia in monozygotic twins discordant for chronic fatigue syndrome. Sleep. 2003;26:324–8. doi: 10.1093/sleep/26.3.324. [DOI] [PubMed] [Google Scholar]
- 41.Omonuwa T, Goforth HW, Preud'homme X, Krystal AD. The pharmacologic management of insomnia in patients with HIV. J Clin Sleep Med. 2009;5:251–62. [PMC free article] [PubMed] [Google Scholar]