Abstract
Background
In many eastern European countries, information is limited regarding (1) prevalence of diabetes and its complications, (2) health care provisions for diabetes, (3) diabetes management, and (4) the structure of postgraduate training in diabetes for doctors and nurses. These have been reviewed here.
Methods
Source material was derived from publications and through personal communication with diabetes specialists in leading clinical centers in Bulgaria, the Czech Republic, Hungary, Poland, Romania, Russia, Slovakia, and Ukraine.
Results
In many countries, information about diabetes prevalence is incomplete or inaccurate with many undiagnosed cases but varies from 7.7–9.6%. Diabetic complications and adverse outcomes (blindness, amputation, and chronic renal failure) are common, with a high mortality resulting from cardiovascular disease. State-funded and private systems often exist side by side. Diabetes care is provided by diabetologists, endocrinologists, internal medicine physicians, and general practitioners, but their involvement varies considerably between countries and some have too few specialists who are located only in large centers. Specialized dietetics and foot care services are, in general, poorly developed. Insulin is freely available although analogs may incur a cost to the patient, while newer drugs (glucagon-like peptide-1 agonists, dipeptidyl peptidase-4 inhibitors) are either expensive or unavailable. Glucose monitoring is often rationed. Postgraduate training in diabetes is now well established in most countries and specialist training for nurses is being developed.
Conclusions
Continuing disparities with western European countries are related mainly to deficient economic resources and inadequate financial investment. Some countries have introduced national programs to improve diabetes care with better clinical outcomes being obtained following treatment initiatives.
Keywords: diabetes prevalence, diabetic complications, eastern European countries, postgraduate training
Introduction
The end of the Cold War brought the removal of the iron curtain between East and West and changed the geopolitical map of Europe. Disintegration of the Soviet Union in 1991 released the eastern European countries from political and economic control. It started a process of geopolitical integration of Western, Central, and Eastern Europe. Information for this review was collected from eight countries situated geographically (Figure 1) in Central and Eastern Europe: Bulgaria (7.7 million inhabitants), the Czech Republic (10.5 million), Hungary (10.1 million), Poland (38.2 million), Romania (21.6 million), Russia (142.9 million), Slovakia (5.4 million), and Ukraine (46.5 million). Only Ukraine and Russia are not members of the European Union.
Figure 1.
Map of European countries.
Eastern European countries have undergone major social and economic changes. After the communist period, these countries retained some state-based system of health care, on which a new private system has been developed and superimposed. Radical differences exist between countries in the provision of health care and the systems used, which directly influence how diabetes care is provided. The aim of this review is to provide some insight into epidemiological data for diabetes, health care systems and reimbursement details, structure and organization of health care provision for diabetes, and systems of postgraduate training for doctors in some former socialist countries in Eastern Europe. Sources include publications and personal communications with health care providers from leading clinical centers in various countries. However, some data are not available and, therefore, the material collected is not sufficiently comprehensive to compare epidemiology, diabetes care, cost of treatment, and outcome between the countries. Few countries have a diabetic register while published analyses of data cover only part of the population over a limited time period and are not updated regularly.
Epidemiology of Diabetes
Epidemiological data about the prevalence of diabetes have been derived from different sources for individual countries (Table 1). A national diabetes register such as the one that exists in the Ukraine is seldom available. Even that one is incomplete and has incorporated only half the known diabetic population. Some data are reasonably accurate and are included in national statistics gathered by bodies responsible for health care information as in the Czech Republic and Slovakia. Other potential sources for statistical data are epidemiological studies and observations such as those performed in Bulgaria, where it was recognized that detection of diabetes was incomplete and that many people have undiagnosed diabetes. In Russia, the geographical territory is very large and includes many cities and towns in relatively remote parts of the country where the structure of diabetes care takes different forms. Publications describing the prevalence of diabetes in Russia are very scarce.
Table 1.
Prevalence of Diabetes in Chosen Countries in the European Region According to Diabetes Federation Data from 2010a
| Country/territory | Population (20–79) | Diabetes Prevalence | Number of people with DM (000s) in the 20–79 age-grouop | ||
|---|---|---|---|---|---|
| 000s | National | Comparativeb | Total | % undiagnosed | |
| Bulgaria | 5790 | 9.0% | 6.5% | 519.5 | 40% |
| Czech Republic | 7824 | 8.7% | 6.4% | 677.3 | – |
| Hungary | 7515 | 8.8% | 6.4% | 658.9 | 56% |
| Poland | 28,618 | 9.3% | 7.6% | 2674.6 | 50% |
| Romania | 16,129 | 8.4% | 6.9% | 1351.4 | 50% |
| Russian Federation | 107,184 | 9.0% | 7.6% | 9,624.9 | 75–80% |
| Slovakia | 4075 | 7.7% | 6.4% | 314.0 | 30% |
| Ukraine | 34,686 | 9.6% | 7.6% | 3328.4 | 50–66% |
Population numbers as described in the CIA World Factbook 2008, with growth and age distribution adjustment to that of developed world population from 2008 to 2010.
All comparisons should be done using the comparative prevalence which is adjusted to the world populaion. The national prevalence indicates the percentage of each country's population that has diabetes; it is ideal for assessing the burden of diabetes in each country.
In Bulgaria, only 60% of people with diabetes are thought to have been diagnosed. According to Borisova2 (based on data published in 2007), around 512,000 patients have diabetes and 377,000 have prediabetes, while an additional estimated 204,000 people with diabetes are yet to be diagnosed. All told, it is estimated that approximately 889,000 Bulgarians have disorders of carbohydrate metabolism. No national diabetes register exists and the epidemiological data are not representative of the entire population. In the Czech Republic, data from the National Institute of Health Information and Statistics (UZIS)3 in 2008 reported that 774,000 people had diabetes in the Czech Republic, a rise of 2.4% compared to 2007. Of these patients, 7% had type 1 diabetes (T1DM) and 91.6% had type 2 diabetes (T2DM). In Hungary, prevalence of T2DM in 2010 in the adult population was 7.5% (285 million). Incidence of T1DM is 1.3 patients per 1,000.4 Prevalence of diabetes in Poland is between 5.2 and 6.5% with 2.6 million people having diabetes. There are estimated to be more than 750,000 people in Poland with undiagnosed diabetes. Of additional concern is the large number (4.7 million) with prediabetes. Prevalence of diabetes in the adult population in Romania is estimated to be 4%. There is an estimated figure of over 500,000 people with diabetes living in Romania. The Bucharest Diabetes Registry was started in 1941, being one of the oldest national diabetes registers in Europe. Each year, about 1 in 1000 inhabitants of Bucharest are registered as having diabetes, the majority (93%) having T2DM and only 7% having T1DM, which is one of the lowest incidence rates of T1DM in Europe.
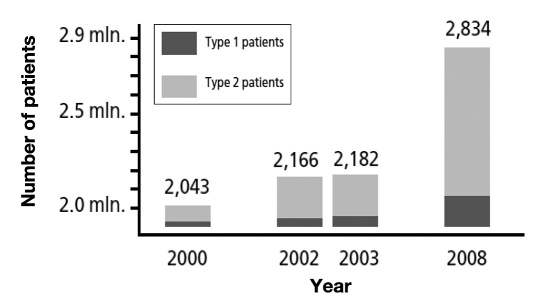
In Russia, according to data from the Federal Target Programme (FTP), Russia occupies third place in the top 10 countries with the highest number of people with diabetes in the world; diabetes is probably undiagnosed in more than 50% of cases. It is estimated that approximately 8 million people in Russia are affected by diabetes (5.5% of the total population). In January 2008, 2,834,000 patients were recorded as having diabetes in Russia5 (282,501 patients with T1DM, 2,551,115 patients with T2DM) (Figure 2).
Figure 2.
Increase of number of patients with diabetes in Russia from 2000 to 2008 (source: data from State Diabetes Registry – Sountsov YUI, 2008).
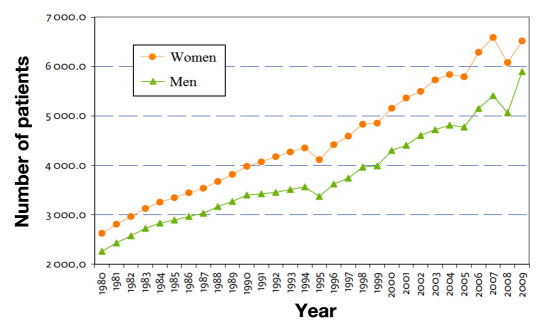
In Slovakia, the National Institute of Health Information and Statistics has reported that 337,187 patients had diabetes in 20096 (Figure 3). Prevalence of diabetes is 7–7.5% and up to 30% of diabetes is undiagnosed. Patients with T1DM accounted for 8.0% of all patients with diabetes, with 89.8% having T2DM, 0.7% having gestational diabetes, and 1.6% having other types of diabetes according to the World Health Organization classification.
Figure 3.
Development of treated patients with diabetes in Slovakia (source: www.uzis.sk).
In the Ukraine, the number of patients diagnosed with diabetes is 1.13 million, with a prevalence of around 2.5%7. This relatively low prevalence may result from many people with T2DM being undiagnosed.8 A national diabetes register was created in 2002 and includes over 509,000 patients, with many being insulin-treated (177,200). According to Ministry of Health data in 2006, the total number of patients with known diabetes is 1.04 million, so nearly half the patients with T2DM have yet to be added to the register.
Prevalence of Diabetes Complications
Bulgaria
Data have suggested that approximately half of those with diagnosed diabetes have identifiable complications, 70% of which are neuropathies, 10% retinopathies, with other complications having a prevalence of 22%. More than 20% of patients with diabetes have more than one complication. The low rate of retinopathy may be related to underdetection. Analysis of data in one diabetes study described 80% of patients as having hypertension, 60% having microalbuminuria, and most having poor glycemic control.2 Vascular complications underlie the high mortality associated with diabetes. In 2005, about 66% of deaths resulted from cardiovascular disease, a rate that was threefold higher than in Holland (Eurostat, 2006).9
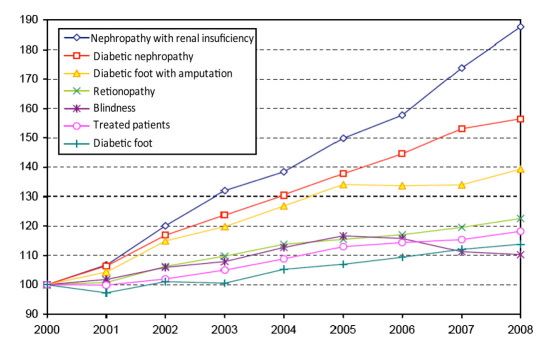
Czech Republic
The incidence of diabetic complications appears to have risen faster than the recognized prevalence of diabetes, although this may reflect improved identification3 (Figure 4). The steady increase in the number of people with individual complications is shown in Table 2 and Figure 4.
Figure 4.
Patients with diabetes and complications of diabetes (index year 2000 = 100%) (source: www.uzis.cz, statistic of outpatient departments of diabetology in 2008 in Czech Republic).
Table 2.
Diabetic Complications in Patients with Diabetes in the Czech Republic (Source: www.uzis.cz, Statistics of Outpatient Departments of Diabetology in 2008)
| Diabetic complication | 2004 | 2005 | 2006 | 2007 | 2008 |
|---|---|---|---|---|---|
| Diabetic nephropathy (all cases) | 63,067 | 66,522 | 69,842 | 73,957 | 75,596 |
| Renal insufficiency | 19,265 | 20,864 | 21,960 | 24,196 | 26,131 |
| Diabetic retinopathy (all cases) | 84,077 | 85,294 | 86,527 | 88,315 | 90,586 |
| Proliferative | 18,644 | 19,055 | 20,339 | 20,902 | 21,505 |
| Blindness | 2364 | 2447 | 2429 | 2335 | 2313 |
| Diabetic foot | 39,753 | 40,402 | 41,328 | 42,337 | 42,992 |
| From those with amputation | 7444 | 7859 | 7834 | 7853 | 8169 |
| % of complications in treated diabetic patients | 26 | 26 | 26 | 27 | 27 |
Hungary
In Hungary, 4,000 amputations are carried out every year, 1,000 new cases of blindness occur every year, and 30% of people requiring dialysis suffer from diabetes.4
Poland
One in every two people with diabetes has coronary heart disease, diabetes is the most common reason for kidney failure, and over 3,000 patients are treated in a chronic dialysis program. A total of 14,000 amputations are carried out annually and it was estimated that diabetes would cause over 29,000 deaths in 2010.10 Approximate estimates have been made of the number with visual impairment (5,000), nephropathy (28,000) and coronary heart disease (200,000).
Romania
Very little accurate information is available regarding the prevalence of diabetic complications. It has been suggested that 50% of new cases of diabetes have no evidence of complications at diagnosis.
Russia
Prevalence of diabetic complications is thought to be very high, but few data are available and are either limited in scope or cover only part of the country such as the Moscow region where the diabetes service differs from remote rural areas. Annual incidence of foot amputation lies between 4.2 and 6.4 per 1,000 people with diabetes, indicating that the risks of diabetic foot disease and amputation are very high.11
As a result of the efforts of the FTP in Russia, a 13% reduction in the prevalence of diabetic retinopathy has been achieved, along with a 10% decrease in the prevalence of nephropathy and need for hemodialysis, a 24% reduction in the number of lower limb amputations, and a 28% reduction in the number of foot amputations. Direct costs of glucose-lowering therapies (insulin and oral medications) accounted for only 9% of all direct costs in 2003, while 91% of this sum was spent on treating diabetic complications.
Slovakia
The most accurate data are provided by the National Institute of Health Information and Statistics. In 2009, prevalence of diabetic nephropathy was 11% with 3.2% of patients on hemodialysis while 0.53% received kidney transplants. Prevalence of diabetic retinopathy was 18.5% with 1.6% being blind. Approximately 19,000 patients had diabetic foot disease, which is the most frequent reason for hospitalization; 14–24% of these patients are at risk of amputation. In 2009, prevalence of diabetic neuropathy was 23% and 1.3% for lower limb amputation.6
Ukraine
Prevalence data about diabetic complications were obtained from national statistics but only half the patients with diabetes had been included. As the rate of undiagnosed patients with diabetes is high (close to 50%), the data are not representative of the whole diabetic population. According to these data, of 29,700 patients with T1DM, proliferative retinopathy was present in 8.9% with 3.5% being blind. Prevalence of diabetic nephropathy was 34%, with renal failure in 28%.12 Because access to hemodialysis is very limited, death from renal failure is high in T1DM (28.4%).
The national diabetes register recorded a total of 105,480 people with T2DM in 2008, 36% of whom had hypertension. In that year, 3% suffered a myocardial infarction and 4.5% had a stroke. Prevalence of blindness was 2.2%. A detailed analysis of the causes of death showed that 46.6% died from renal failure, 40.3% from coronary heart disease, and 7% from stroke.12
Structure of Diabetes Services
Diabetes Speciality Provision
Two parallel health care systems exist in most eastern European countries. In one system, diabetes care is provided either by a specialist diabetologist, as in the Czech Republic, Romania, Slovakia, and Hungary or by an endocrinologist, as in Bulgaria and the Ukraine. In the second system, the care of people with diabetes is mixed, with partial provision by a diabetes specialist but provided in large part by general practitioners (GPs), as occurs in Russia and Poland.
Most countries have a mixed system of provision of diabetes care with simultaneous state-funded health care in conjunction with private practice.
Private medical services are either fully reimbursed, as in the Czech Republic, or are paid in part by the patient, as in Romania. As the systems of provision of diabetes care are country specific, these are described separately. Only the Czech Republic and Slovakia have very similar systems that were created before the division of Czechoslovakia in 1993, with the development of private medical practice occurring after the end of the communist era.
Bulgaria
Information on the provision of diabetes care in Bulgaria is limited but this is provided by endocrinologists and is free to the patients.
The Czech Republic and Slovakia
Diabetes outpatient departments provide a specialist diabetes service in almost every city of both countries and are mostly private. A higher level of diabetes care is provided in university hospitals and at the specialized national institutions. In the Czech Republic, diabetology centers have inpatient facilities and can offer a full range of diabetes care. Involvement of GPs in diabetes treatment is much lower in Slovakia than in the Czech Republic. Professional societies in both countries have guidelines for the health care of patients, which are consistent with those of the European Association for the Study of Diabetes. Health insurance is uniform and obligatory for everyone and is paid by the state. Basic health care is free of charge but there is a partial fee for medication that has to be paid by the patient.
Hungary
In Hungary, health care is paid via the National Health Insurance Company (every Hungarian citizen has to pay part of an insurance fee). Accredited diabetes outpatient clinics look after adult patients and separate clinics treat pediatric patients, which are 90% state owned. In private practice, where an individual has no contract with the state insurance company, all charges have to be paid by the patient. All patients with diabetes who have complications are supervised in a diabetes outpatient clinic.
Poland
There is no organized system for diabetes care in Poland. Only 20% of outpatient departments for diabetes operate privately. About 80% of people with diabetes are treated entirely by their GPs but their levels of knowledge about diabetes and its management are limited and they have restricted access to the measurement of hemoglobin A1c (HbA1c). Koblik and colleagues (2007)13,14 have shown that most patients being treated by GPs have suboptimal glycemic control (Table 3).
Table 3.
| Results | PDAa criteria | |
|---|---|---|
| HbA1c (%) | 8.9 | ≤7 |
| Postprandial plasma glucose mg % (mmol/liter) | 201.9 (11.2) | ≤135 (7.5 mmol/liter) |
| Fasting plasma glucose mg % (mmol/liter) | 171 (9.5) | 70–110 (3.9–6.1 mmol/liter) |
PDA, Polish Diabetology Association
In an attempt to improve diabetes care in Poland, the Improve Glycaemic Control Programme was created for prevention and more effective control of diabetes. The program encourages greater cooperation between specialists and GPs for diabetes care; a shared care model of local networks was created. A diabetes specialist (as the team leader) cooperates with five GPs, and each GP enrolls 10 patients with diabetes every year. All results are sent to a web platform for data recording. A major function of the website is to educate GPs and specialists.
Romania
There are insufficient specialists in diabetes and around five times more private diabetes clinics in Romania than public clinics. The diabetes specialist has a contract with the National Health Insurance Company; the patient does not have to pay anything for therapy when consulting a specialist. However, as of April 2010, it has not been possible for a doctor to work in both a public and a private clinic simultaneously. The implementation of this measure has decreased the availability of diabetes care for patients by around 25%.
Russia
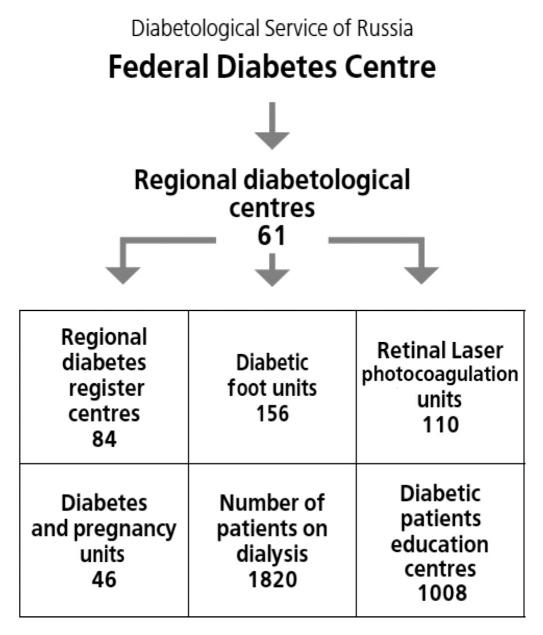
Treatment of people with diabetes in Russia is provided at three levels of health care: (1) primary in General Practice, (2) specialized endocrinology care, and (3) high-tech medical care. In 2002, the FTP was started and was continued for 7 years. The regulations of health care authorities stipulate that an endocrinologist should be available for every 50,000 people,3 but the number of available endocrinologists and the increasing number of patients with diabetes has overstretched the resources available. A structured diabetes service was established that was led by the Endocrinological Research Centre of the Russian Academy of Medical Sciences. The main center in each region is a diabetes institute, with regional diabetes centers. This structure of diabetes health care in Russia includes specialized units for treating diabetic foot disease, ophthalmology units, and renal hemodialysis departments for the management of patients with end-stage diabetic nephropathy. In addition, there are more than 1,000 education centers to teach patients and their family members about diabetes. Some have become centers of excellence that offer high-tech methods for predicting, diagnosing, and treating the vascular complications of diabetes5 (Figure 5).
Figure 5.
Structure of Diabetes Service in Russia according to the Federal Target Programme (source: adapted from Dedov, Shestakova, and Sounstov, 2008).
Mobile diabetes centers were established to provide diagnostic and therapeutic procedures for patients who live in remote areas of the country.
The FTP has produced significant benefits:
Prevalence of T1DM in adults has been reduced by 6.1%.
Mortality among patients with types 1 and 2 diabetes has declined by 8.4%.
Mean life expectancy in patients with T1DM has risen by 3.1 years, and that of patients with T2DM by 3.9 years.
Application of the FTP has been accompanied by a 92% reduction in the number of operations for neuropathic diabetic foot disease, a 10- to 15-year increase in the predialysis period in patients with nephropathy, and introduced a 15- to 20-year delay in the development of proliferative retinopathy and blindness.
Ukraine
While the offices of most endocrinologists are situated in outpatient clinics, regional hospitals and some major city hospitals have specialized endocrinology departments that offer a secondary level of diabetes care. Consultations with endocrinologists are state-funded but some services (e.g., some laboratory measurements) have to be paid by the patient.
Paramedical Support: Availability of Dietetic and Podiatry Services
Separately trained and registered dietitians, who are an integral part of the diabetes team in western countries, do not exist in eastern European countries. A specialized dietetic service, which is provided by nurses, is available only in those countries where specialist training has been established for these health care professionals, namely Hungary, Poland, the Czech Republic, and Slovakia. These nurses work mainly in the hospitals, which have departments that specialize in nutrition; they rarely practice in diabetes outpatient clinics.
Another major area of unmet need is in the provision of specialized podiatry services for management of diabetic foot problems. In most eastern European countries, provision of podiatry is piecemeal and what service exists has no nationally organized structure and is poorly developed. In 2005, a group of podiatry outpatient departments was established in the Czech Republic; specialized practices serve people with diabetes who have foot problems—again provided by specially trained nursing staff. Few podiatry outpatient facilities exist in Slovakia outside the main institutes of diabetology. No detailed information could be obtained about other eastern European countries with respect to the availability of podiatry services for people with diabetes, although in Russia there are a number of diabetic foot units.
Availability of Treatment for Diabetes
Availability of treatment for diabetes differs between countries. Conventional therapy with human insulins is supplied free in all countries and is funded by national diabetes programs in Bulgaria, Romania, Russia, and the Ukraine. However, the use of insulin analogs is restricted and reimbursement is only for patients who have poor glycemic control after 6 months of treatment with human insulin or are experiencing frequent severe hypoglycemia. The HbA1c threshold for determining conversion to analog insulins varies between countries that apply this policy. Dipeptidyl peptidase-4 (DPP-4) inhibitors and glucagon-like peptide-1 (GLP-1) agonists are available for T2DM. In the Czech Republic and Slovakia, they are used as an alternative to insulin analogs but they can be reimbursed only after 6 months of inadequate glycemic control with oral antidiabetes drugs. In some countries, the patient has to pay, at least in part, for DPP-4 inhibitors and GLP-1 agonists (30% in Hungary and 100% in Bulgaria and Poland). Country-specific approaches to diabetes treatment and availability of therapies are shown in Table 4.
Table 4.
Country-Specific Approaches to Diabetes Treatment and Availability of Therapiesa
| Medicament/device | Bulgaria | Czech Republic | Hungary | Poland | Russia | Romania | Slovakia | Ukraine |
|---|---|---|---|---|---|---|---|---|
| Glucometer | Insulin-treated | Insulin-treated | Insulin-treated | Free | – | Insulin-treated | Insulin-treated | No reimbursement |
| Strips | 150/y | 3 inj/400 s/y | 4 inj/150/m | 0.8 Eur/50 s | 50–100/m <18 y 200/3m for insulin patients in Moscowb | 300/3m <18 y | 3 inj/150/2 m | 200 s/12 m <18 y >18 y – no reimbursement |
| <18 y/400 s/y | 3 inj/100/m | |||||||
| 2 inj/200 s/y | 2 inj/100/3m | >18y -100/3m | 1 inj/50/2 m | |||||
| tablets/100/y | Tablets/50/4 m | |||||||
| Tablets | 100% | 100% | 100% | 100% | 100% | 100% | 100% | No reimbursement |
| DPP-4i | No reimbursement | 100% | 0.7 | no reimbursement | No reimbursement | 100% | 100% | No reimbursement |
| GLP-1 | No reimbursement | 100% | – | no reimbursement | – | 100% | 100% | No reimbursement |
| Regular insulin | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 1 |
| Insulin analogs | 100% | 100% | 3 inj/100% | no reimbursement | Reimbursed for some groups | 100% | 80–100% | No reimbursement |
| 1 inj/50% | ||||||||
| premix ins/70% | ||||||||
| Insulin pump | No reimbursement | 100% | 100% <18 y | 100% <18 y% | No reimbursement | Up to 30 new patients per year | 100% | Not available |
| >18 y–20% reimbursement | 18–26 y – accessories | |||||||
inj, number of insulin injections; m, month; y, year; s, strip; EUR, Euro.
Dependent on territorial law, also no reimbursement.
Access to Superspecialized Services
(a) Continuous subcutaneous insulin infusion (CSII) with insulin pumps
Insulin pump therapy for CSII has been developed to the greatest degree in the Czech Republic where approximately 3,900 patients with diabetes are receiving therapy. Insulin pump therapy has to be recommended by a diabetologist and approved by the center for insulin pump therapy and the medical insurance reimbursement company. Treatment is free of charge but has to meet criteria, which include severe hypoglycemia, poor metabolic control, and presence of serious diabetic complications. In Slovakia, an estimated 1,500 patients are receiving fully reimbursed treatment with insulin pumps. In Hungary, insulin pump therapy is provided free for children but for patients aged over 18 years, 80% of the cost has to be paid by the patient. There are approximately 2,500 patients receiving this form of treatment. In Poland, every child with T1DM has access to free insulin pump treatment if desired; between 18–26 years, only the pump accessories are reimbursed but not after this age. An estimated 10,000 patients are treated by insulin pump in Poland. In Romania, reimbursement covers 30 new patients receiving insulin pump therapy annually.
(b) Pancreatic transplantation
A pancreatic transplant program for diabetes exists in only two of the countries that have been included in this article, namely the Czech Republic and Poland. In the Czech Republic, the Institute of Experimental Medicine in Prague has provided kidney and pancreas transplantation for people with diabetes since 1983. As of 2011, this center has performed 51 whole pancreas transplants and 359 combined whole kidney and pancreas transplants, and in 2010, the center performed 14 successful islet cell transplants. In 2009, the number of whole pancreas transplants was 2.7 per million population and 2.5 per million of population received combined whole pancreas and kidney transplants. In Poland, in 2009, a total of 20 whole pancreas transplants were performed with a similar number of combined pancreas and kidney transplants (a comparable rate of 2.5 transplants per million). However, very few pancreatic transplants have been performed in other countries (Slovakia and Hungary).
Bulgaria
Glucose meters are provided free only for insulin-treated patients but strips are rationed. The National Insurance Company pays for most antidiabetes drugs and insulin is free of charge. Dipeptidyl peptidase-4 inhibitors and GLP-1 agonists are fully reimbursed.
Czech Republic
Basic health care is free but patients have to pay in part for their medication. The insurance system covers the cost of glucose meters and strips for patients who require a minimum of three injections of insulin per day. A total of 400 strips can be prescribed annually. Patients with diabetes on oral medication have to purchase a glucose meter and can receive 100 strips per year without charge. Analog insulins are provided free but are restricted to patients who have HbA1c below 6% or for patients who are experiencing frequent severe hypoglycemia. It is necessary thereafter to demonstrate a 10% reduction in HbA1c after 3 months of analog therapy or a lower frequency of hypoglycemia.
Hungary
In private practice where there is no contract with the state insurance company, all charges are paid by the patient. Insulin-treated patients receive a 50% discount for the purchase of designated brands of glucose meters and the prescription of strips depends on the number of insulin injections per day, of which only 20% is reimbursed. The cost of analog insulin is fully reimbursed for patients who require four injections per day; fewer injections attract only 50% reimbursement, while premixed analog insulins receive 90% reimbursement.
Poland
There are problems in accessing the specialized medical service (necessitating long queues). Each diabetologist has an average of 4,000 patients. There are eight accredited diabetes centers and 37 public outpatient units specializing in diabetes. Only nine centers offer laser treatment and nine public centers provide dialysis. Glucose meters for insulin-treated patients are provided free, while glucose strips have to be purchased. Conventional human insulin and fast-acting insulin analogs are provided free but the patient has to pay for long-acting insulin analogs, DPP-4 inhibitors, and GLP-1 agonists.
Romania
The diabetes specialist has a contract with the National Health Insurance Company that pays for both the consultation and for all diabetes prescriptions so that the patient receives free treatment. Optional private health insurance can be made but in most of the private clinics, the patient has to pay a variable sum for treatment, administrative issues, and some blood or urinary measurements. However, National Health Insurance pays for their diabetes prescription, which is always free. The insulin-treated patient may receive a glucose meter and glucose strips but these are rationed. All antidiabetes medications, including insulin, are provided free.
Russia
Complete reimbursement is funded from government and intraurban budgets in Moscow and St. Petersburg but in other parts of the country, regional funding is required. Only patients at increased risk of acute metabolic complications (children, adolescents, and pregnant women) receive authorization for the use of genetically engineered human insulin or insulin analogs. Test strips are reimbursed only in Moscow and St. Petersburg. Newer methods of treatment, DPP-4 inhibitors and GLP-1 agonists, have to be paid for by patients.
Slovakia
Part (90%) of routine care is provided in private practice by diabetologists and part is provided in hospitals. The cost of examination and laboratory tests performed by the diabetologist is free for patients. Glucose meters and some strips are free for insulin-treated patients (50–150 strips per month). Patients on oral medications receive a total of 150 strips per year. Of the different classes of medications, some are free while some newer drugs are paid for in part by the patient (some insulin analogs, GLP-1 agonists, DPP-4 inhibitors). Newer drugs are for second-line treatment and are only prescribed if glycemic control is suboptimal.
Ukraine
Implementation of a National Diabetes Plan in 1999 enabled insulin to be supplied free to patients. Insulin is provided to patients by their endocrinologist. In addition to their preferred insulins, other insulins can be purchased in pharmacies or drug stores.7 Analog insulins are more expensive and are prescribed mainly for patients with poor glycemic control. Long-acting analog insulins are recommended when the total daily insulin dose is more than 50 units or if diabetic complications are present.8 In most regions, oral antidiabetes drugs have to be purchased by patients as with self-monitoring equipment and routine HbA1c measurements.
Diabetes Training for Health Care Professionals
Postgraduate education and specialist training differs between countries, as does the structure of diabetes care (Table 5). In some eastern European countries such as the Czech Republic, Romania, and Slovakia, diabetology exists as a separate speciality distinct from endocrinology. From 2010 in the Czech Republic, the separate training of diabetologists was discontinued and postgraduate specialist education was combined with endocrinology. Specialist training requires residency experience and training in internal medicine, followed by postgraduate examinations and 2 years of specialist practice at a certified center of diabetology. From 2011 in Romania, where diabetes remains a separate speciality, residency training for diabetologists has been shortened from 5 to 4 years. Funding for specialist training (expenses for training in a certified diabetes department away from home) is expensive and usually requires some form of sponsorship, sometimes provided by pharmaceutical companies.
Table 5.
Specialist Training
| Different training for specialists in eastern European countries: | ||
|---|---|---|
| 1. Endocrinology | Czech Republic, European Union system | 3 years of internal medicine + 2 years of endocrinology |
| Ukraine | 2 years of internal medicine + 3 months of endocrinology | |
| Bulgaria | 1 year of internal medicine + 3 years of endocrinology | |
| Russia | 2 years of endocrinology or bacic speciality + 4 months of endocrinology | |
| 2. Diabetology | Slovakia, Hungary | 3 years of internal medicine + 2 years of diabetology |
| Romania | 4 years not specified duration of internal medicine + diabetology | |
To train diabetes specialists in Hungary, in 1996 the Hungarian Diabetes Association organized a 2-year course for specialists in internal medicine, pediatrics, and ophthalmology, leading to a specialist examination and qualification as a recognized diabetes specialist. A specialist course for nurses was started in 1995, and those who successfully complete this training work in diabetes specialist centers, including hospital wards, outpatient clinics, and the primary health care network. In Bulgaria, postgraduate training is directed at endocrinology, which requires 3 years of specialist training and study and 1 year of internal medicine. In the Ukraine, a specialist qualification as an endocrinologist can be obtained after 2 years of training in internal medicine and specialist training in endocrinology for an additional 3 months. Alternatively, medical graduates who wish to become specialists in endocrinology can go directly into an endocrinology residency program after graduating from medical school. In Poland, GP training in diabetes has been developed with training conferences and GP workshops, and conferences for diabetes specialists are held regularly. The National Diabetes Programmes (NDP) provides training for GPs to diagnose diabetes and undertake routine management.
Dietitians and educators are not commonly included in clinical diabetes teams. Several countries such as the Czech Republic, Hungary, and Slovakia have nurses who provide specialized dietetic advice, and in the Czech Republic, nurses are being trained to specialize in podiatry. Each podiatry center has a nurse with a minimum of 3 years practice in internal medicine or surgery, an orthotist, a surgeon, and a diabetologist. The obligatory training with certification for nurses is based on the Diabetic Foot Care Education Programme for the training of certified Diabetic Foot Care Assistants published by the International Diabetes Federation (IDF) in 2008. In Romania, the centers of excellence in major university cities have a podiatry care system with one doctor, usually a dermatologist, and one nurse.
Availability of Diabetes Specialists
The number of doctors specializing in diabetes varies in different eastern European countries. Diabetes care is also provided in many countries by general practitioners and internal medicine specialists. While the total number of doctors specializing in diabetes can be identified in most countries, the absolute number involved does not indicate what percentage of patients have access to specialist input for their diabetes care within each country. This is further obscured by the provision of private specialist care in some centers for patients who can afford to have private treatment. In the Czech Republic in 2008, 323 diabetologists and 350 specialist nurses were recorded as working in specialist diabetes departments, with one diabetologist looking after an average number of 2,100 patients. In the same year in Slovakia (where the population is half the size of that in the Czech Republic), the number of diabetologists was 158, so the ratio of patients to individual specialists is similar in these two countries. General practitioners are also treating diabetes in the Czech Republic for 15.8% of patients, while 84.2% patients attend a diabetes specialist department. In Slovakia, few patients receive diabetes care from GPs as a network of diabetologists providing private treatment is available throughout the country.
In Hungary, there are 172 accredited doctors and 26 certified pediatricians who specialize in diabetes. In Ukraine, the care of people with diabetes is principally undertaken by endocrinologists, most of whom are employed by the government; in 2006, there were 1,929 endocrinologists to look after the diabetic population. Diabetes care in Romania is provided by diabetologists with provision by the state and also on a private basis but Romania has a very low number of diabetes specialists considering the large number of people who have diabetes. There is a substantial shortage of diabetes specialists in Poland, with only an estimated 500 diabetologists whereas approximately 1,500 are required for the size of the population. As a consequence, most diabetes care is provided by GPs.
The Russian health authorities have advocated having one endocrinologist/diabetologist available for a population of 50,000 people. However, in Russia, the total number of specialists who treat people with diabetes (an estimated 5,000) is recognized to be insufficient. One of the reasons for the relative deficiency of endocrinologists in Russia is that aspiring specialists have to self-fund their specialist training at certified centers, but for many, their income from clinical practice does not cover this relatively high investment required to obtain specialist education and certification (personal communication). In Ukraine, the primary care of people with diabetes is undertaken by a total of 1,939 endocrinologists who are mostly employed by the state-run health service, but also by GPs.
Discussion
In eastern European countries, diabetes is managed in different ways and with variable levels of health care. Data about prevalence differ between those reported by the countries and those estimated in data from the IDF Atlas or other sources (Table 1). One reason is an alarmingly high rate of undiagnosed diabetes (30–80%); some data are inaccurate or are not available. There are several problems in eastern European countries:
A lack of economic resources in societies, which is vital to improve the outcome for patients with diabetes;
The lower income of people limits payment for health care, medication, and diagnostic tools;
A lack of legal status for nongovernmental organizations (NGOs).
There are many other factors that are uncommon in western countries as was reported by surveys of patients: financial stringencies, bureaucracy (Russia), interference with NGO activity by governments (Russia), and passivity of national diabetes associations.15 Only in countries where the government has accepted diabetes as a priority disease state requiring urgent and aggressive management can a substantial reduction in diabetic complications and economic cost of this disorder be achievable. Three important pillars from government are required: involvement in national programs, creation and maintenance of a national register of patients with diabetes with accurate and adequate data, and health support for people in lower social classes. In some eastern European countries, the service for patients with diabetes is reasonably good, with only partial financial outlay for patients. It is important to appreciate that because of lower economic standards existing in these countries, without government funding, present levels of health care services cannot be secured. Apart from these economic factors, which are crucial, some other proposals may improve the situation:
More round-table discussion sessions in countries involving professionals, patients, health authorities, and state representatives;
Training courses for volunteers and health care providers (specialized for dietetics and podiatry);
Training courses for representatives of national diabetes associations about the development of organizations;
Direct contacts from the IDF to governments of countries;
Creation of projects to join different countries focusing on reducing particular complications;
More mobile and regularly operating units for the remote parts of the country;
Data obtained from diabetes treatment should be analyzed and published and show clearly the real situation and danger of diabetes in society.
As Dedov and colleagues11 clearly showed from the data of the Russian FTP, reducing the mean HbA1c concentration by just 1% saved an expenditure of USD 246.7 million each year. Effective treatment of patients with diabetes not only preserves an active and working member of society but also saves an enormous amount of the state's budget.
Only a strong, common, and cooperative movement among patients' organizations, health care representatives, and government and local political authorities can encourage activities in societies for changing the progression of diabetes and its devastating consequences.
Summary and Conclusions
Although the reported prevalence of diabetes varies in eastern European countries (Hungary 9.8%, Poland 9.1%, Czech Republic 9.7%, Slovakia 8.9%, Bulgaria 4.0% and Romania 4.0%), the real prevalence in all of these countries is probably higher than is registered by the IDF. However, all are struggling to cope with the rising prevalence of diabetes despite having lower economic resources than western countries. Attempts are being made to limit development and progression of T2DM and provide effective therapies for this disorder to limit its devastating consequences.
In some eastern European countries where the health care system is underdeveloped, diabetes services remain inadequate and unsatisfactory. This is particularly evident in the lack of specialist provision to treat diabetic foot disease and the seriously insufficient renal replacement (dialysis) capacity in some countries. National diabetes registers are either absent or only partial, and demographic and statistical data of diabetes-related parameters and outcomes are often incomplete and unreliable. In recognition of these deficiences in diabetes health care, several countries have devised methods to improve diabetes care. National diabetes programs are receiving government support in many countries, particularly in Poland, Romania, and Russia, which augurs well for future management of people with diabetes. Fortunately, despite economic constraints, there is no shortage of insulin in any of these countries. Mobile units offer basic diabetes care in remote rural areas of some countries such as parts of Russia. Effective podiatry care is being developed in the Czech Republic and in other countries. The Polish authorities have created a shared care model for diabetes involving GPs. In some countries, the training for endocrinology has been shortened to create more specialists (as in Bulgaria and Romania).
Enormous effort and progressive changes in diabetes care have brought commendable and highly encouraging results in reducing the rate of diabetes complications and have increased life expectancy (Ukraine). However, the results achieved are still modest and need to be continued. In some eastern European countries, the service for diabetic patients is reasonably satisfactory by western standards, with only partial financial investment being required by patients. It is important to appreciate that, because economic standards in these countries are lower, the present levels of health care services cannot be secured without government funding. Despite strenuous efforts being made in countries such as Ukraine, Russia, and Poland, which have produced significant improvements in diabetes control in some of the diabetic population, many serious problems and challenges remain to be solved to improve diabetes care for individual patients and to relieve the overall burden on society.
Acknowledgments
The authors wish to thank Professor Wladyslaw Grzeszczak, M.D., Ph.D., Eszter Madarász, M.D., Ph.D., and Sylvia Pashkunova, M.D. for information and data about diabetes treatment in their countries.
Glossary
Abbreviations
- (CSII)
continuous subcutaneous insulin infusion
- (DPP-4i)
dipeptidyl peptidase-4 inhibitor
- (FTP)
Federal Target Programme
- (GLP-1)
glucagon-like peptide-1
- (GP)
general practitioner
- (HbA1c)
hemoglobin A1c
- (IDF)
International Diabetes Federation
- (IFG)
impaired fasting glucose
- (NGO)
nongovernmental organization
- (PDA)
Polish Diabetology Association
- (T1DM)
type 1 diabetes mellitus
- (T2DM)
type 2 diabetes mellitus
References
- 1.International Diabetes Federation. Brussels: International Diabetes Federation; 2009. Diabetes atlas. 4th ed. http://www.idf.org/diabetesatlas. Accessed July 19, 2010. [Google Scholar]
- 2.Borisova AM, Kovacheva R, Shinkov A, Atanasova I, Aslanova N, Vlachov J, Dokovska L. A study of the influence of diabetes mellitus among not selected Bulgarina population like cross-sectional study. Endocrinology. 2007;12(1):42–49. [Google Scholar]
- 3.Institute of Health Information and Statistics of the Czech Republic. Statistic of outpatient departments of diabetology in 2008 Czech Republic. 2011. http://www.uzis.cz/system/files/36_09.pdf. Accessed July 16.
- 4.Barkai L, Blatniczky L, Halmos T, Hidvégi T, Jermendy G, Kaló Z, Madácsy L, Vándorfi G, Winkler G, Wittmann I. National Diabetes program 2011. Diabetologia Hungarica. 2011;19(Suppl 3):5–39. [Google Scholar]
- 5.Novo Nordisk; Russian Diabetes Federation. Diabetes: the hidden pandemic and its impact on Russia. 2011. http://www.changingdiabetesbarometer.com/docs/Diabetes%20The%20hidden%20pandemic%20and%20its%20impact%20on%20Russia.pdf. Accessed July 16.
- 6.National Health Information Center. Statistic of outpatients departments of diabetology in Slovakia. 2011. http://data.nczisk.sk/publikacie/zs1011.pdf. Accessed July 16.
- 7.International Diabetes Federation. Country report – Ukraine. 2011. http://www.idf.org/webdata/docs/idf-europe/Country%20report%20Ukraine%20pub.pdf. Accessed July 17.
- 8.Khalangot M, Tronko M. Primary care diabetes in Ukraine. Prim Care Diabetes. 2007;1(4):203–205. doi: 10.1016/j.pcd.2007.10.041. [DOI] [PubMed] [Google Scholar]
- 9.Eurostat. Europe in figures: Eurostat yearbook 2006-07. 2011. http://epp.eurostat.ec.europa.eu/cache/ITY_OFFPUB/KS-CD-06-001/EN/KS-CD-06-001-EN.PDF. Accessed July 16.
- 10.Sieradzki J, Grzeszczak W, Karnafel W, Wierusz-Wysocka B, Manikowski A, Szymoński T. The PolDiab Study. Part I. Analysis of diabetes treatment in Poland. Diabetol Prakt. 2006;7(1):8–15. [Google Scholar]
- 11.Federal State Establishment Endocrinological Research Centre. Diabetes in Russia: problems and solutions. 2011. http://www.changingdiabetesbarometer.com/docs/Diabetes%20in%20Russia%20problems%20and%20solutions.pdf. Accessed July 16.
- 12.Khalanogot MD, Tronko MD, Kravcenko VI, Kovtun VA, Okhrimenko NV, Bolgarska SV. Some mortality risk factors for type 1 diabetes mellitus patients in Ukraine evaluated according to data from National Register. Endocrinologia. 2010;15(1):62–70. [Google Scholar]
- 13.Koblik T, Wolnik B, Sieradzki J, Kot W. Changing diabetes - an international project taking into account activities to improve efficacy of type 2 diabetes management. Part I. Objectives of the project. Diabetol Prakt. 2007;8(8-9):354–357. [Google Scholar]
- 14.Koblik T, Sieradzki J, Kot W. Changing diabetes - an international project taking into account activities to improve efficacy of type 2 diabetes management. Part II. The Polish program for improving glycaemia control. Diabetol Prakt. 2007;8(10):365–370. [Google Scholar]
- 15.Augustiniene V. Real situation on association development, social aspects and patients rights in Eastern European countries. 2011. http://www.powershow.com/view/3f05-NjllZ/Real_Situation_on_Association_Development_Social_Societal_Aspects_and_Patients_Rights_in_Eastern_E_flash_ppt_presentation. Accessed July 16.