Abstract
Central nervous system tuberculosis in children presents commonly as tubercular meningitis, post-tubercular meningitis hydrocephalus, and much more rarely as space-occupying lesions known as tuberculomas. The occurrence of this condition, though previously reported only in the developing world, is now frequently reported in human immunodeficiency virus positive migrants in the western world. The exact pathogenesis of this condition is still incompletely understood, and the mainstay of treatment is chemotherapeutic regimes. Neurosurgical intervention is rarely necessary, and is confined to cases of hydrocephalus after tubercular meningitis and to large tubeculomas with space-occupying effects.
Keywords: Hydrocephalus, tuberculoma, post-tubercular hydrocephalus
Introduction
Central nervous system (CNS) disease caused by Mycobacterium tuberculosis is an uncommon, yet undoubtedly a devastating manifestation of tuberculosis. CNS tuberculosis accounts for only 10% of all cases of tuberculosis, carries a high mortality and a distressing level of neurological morbidity. There is clearly a preponderance of the disease type in children and human immunodeficiency virus (HIV)-infected individuals. The burden of CNS tuberculosis lies largely in resource-starved regions of the world although there has been recent resurgence of the disease itself in both the developing and the developed world. However, the challenge to adequately diagnose and deal with its morbidity has yet to be substantially met. It would not be out of place to remind ourselves that fundamental questions regarding the pathogenesis, diagnosis, treatment, and management of CNS tuberculosis remain unanswered. The best and most rapid method of diagnosis, optimal treatment drugs and duration of therapy are questions which have yet to be adequately addressed.
There is another problem. While the necessity of an appropriate animal model has been long recognized, no animal model truly mimics the human infection. Rich and McCordock's original experimental model[1] involved rabbits and guinea pigs, and while a number of animal models have been studied, the rabbit model still remains the best available experimental model to study this disease.
Pathogenesis
Most tuberculous infections are caused by M. tuberculosis. The bacilli reach the CNS by the hematogenous route secondary to disease elsewhere in the body. The original description by Rich[1] suggested a two-stage development of CNS tuberculosis-first tuberculous lesions (Rich's focus) develop in the brain during the stage of bacteremia or shortly afterward and later the rupture or growth of one or more of these lesions produces development of CNS tuberculosis. The initial Rich focus may occur in the meninges, the subpial or subependymal surface of the brain, and may indeed remain dormant for many years. The specific stimulus needed for rupture or growth of these lesions is still not completely understood although the mechanism is known to be immunological in nature.[2]
The type of lesions that result from discharge of the bacilli into the cerebrospinal fluid (CSF) depends on the virulence of the bacteria and the immune resistance of the host. Rarely, direct spread may occur to the meninges from the middle ear or the calvarial bone. A study of immunological parameters showed a relation between the development of tuberculous meningitis (TBM) in children and significantly lower count of CD4 T-lymphocytes when compared with children who had pulmonary complex only.[3] The brain lesion also originates from hematogenous spread from the lungs, and when there is a sizeable inoculation with inadequate cell-mediated immunity, the parenchymal lesion may develop into a tuberculoma or a tuberculous abscess. A recent study from Vietnam has speculated on the relationship between bacterial and host genotype as being responsible for genesis of extrapulmonary versus pulmonary disease.[4]
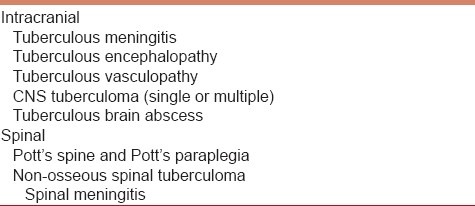
In TBM, a thick gelatinous exudate develops around the basal cisterns, the sylvian fissure and the brainstem. As this may cause obstruction to the outflow from the fourth ventricle or indeed from the cerebral aqueduct, hydrocephalus frequently develops in these children, and this further exacerbates the clinical condition by raising the intracranial pressure (ICP). The brain itself shows edema, perivascular infiltration with lymphocytes and mononuclear cells, and a microglial reaction. Indeed, a vasculitic-like syndrome may result, where inflammatory changes may be seen in the vessel wall, and the lumen of these vessels may be narrowed or even occluded by formation of the thrombi, and this may result in small areas of infarction. In the majority of patients, the location of the infarctions is in the distribution of the medial striate and thalamoperforating arteries. Rarely, hemorrhagic transformation of these infarcts may occur. The different types of CNS tuberculosis have been summed up in Table 1.[5]
Table 1.
It may not be out of place to point out that the ventriculomegaly that occurs in these patients is not always due to obstructive hydrocephalus, and hence associated with high ICP, but may be due to brain “softening”[6] as reported by the author earlier, and in these cases the ICP is not raised.
Tuberculomas are firm, avascular, spherical masses, with size varying between 2 cm and 10 cm in diameter. They are well circumscribed, and the compressed surrounding brain tissue shows edema and gliosis. The inside of the masses contains necrotic areas of caseation in which tubercle bacilli may be found. Tuberculous brain abscess is a distinct condition. For the histopathological diagnosis of these lesions, microscopic evidence of pus in the cavity with microscopic changes in the abscess wall, together with presence of tubercle bacilli, is mandatory. Abscesses are generally larger and solitary and grow faster.
Clinical Features
In most children with TBM, there is a prodromal phase of malaise and myalgia lasting for 2-8 weeks prior to the development of symptoms and signs of meningeal irritation. The headaches become worse and continuous and neck stiffness is present in about 25% of the patients. Infants become increasingly irritable and develop bulging fontanelles and increasing head circumferences. Nausea, vomiting and altered sensorium may follow in these children. Low-grade pyrexia or “night sweats” are reported in 80% of the patients. A prior history of tuberculous infection is present in 50% of children and in 10% of adults.[7,8] Cranial nerve palsies occur in 20-30% of patients with TBM. Affection of both optic nerves may cause blindness. Optochiasmatic arachnoiditis, hydrocephalus causing compression of the optic nerves, optic nerve granulomas and ethambutol toxicity may be the cause of blindness in patients with TBM.[9,10]
Any focal neurological deficit may occur in the limbs, ranging from monoplegia to quadriplegia. Abnormal movement disorders may occur-choreoform or hemiballistic movements, athetosis, tremors and myoclonic jerks have all been described. Patients with hydrocephalus or with severe cerebral edema as well those with significant vascular injury may present with depressed level of consciousness. Seizures may be the presenting feature of patients with tuberculomas or tuberculous abscesses. Lethargy and confusion leading to stupor may occur in the terminal stages of untreated disease.
Clinical manifestations of tuberculomas and tuberculous abscesses depend obviously on their location, most being located in the supratentorial compartment, and headaches, seizures, papilledema and focal deficits may all occur. The presentation of brain abscess is more subacute (1 week to 3 months after infection), but much slower than pyogenic brain abscesses. Tuberculomas may present months to years after infection.
Diagnosis
CSF examination remains the mainstay of diagnosis of TBM. Usually, there is a lymphocytic reaction (60-400 per mm3), with raised protein levels (0.8-4 g/l). In the initial stages of the infection, the white cells seen in the CSF may be polymorphonuclear leukocytes, but soon these are replaced predominantly by lymphocytes. There is gradual decrease in the glucose level in the CSF, which is generally less than 50% of the serum levels, although it is never as low as in pyogenic meningitis.[11,12] Definitive diagnosis of TBM depends on detection of tuberculous bacilli in CSF either by smear examination or bacterial culture. It has been claimed that if large volumes of CSF can be obtained, repeated centrifugation detects bacteria in a high proportion of cases.[13] Measuring the levels of antibodies to different antigens of M. tuberculosis has also been suggested as a diagnostic tool.[14]
Radiological examination by Computerized Tomography (CT) Scans or Magnetic Resonance (MR) Imaging has limited value in the diagnosis of TBM. The following radiological signs have been described:[15,16] Enhancing exudates in the basal cisterns or sylvian fissure with or without presence of ventriculomegaly, infarcts in the basal ganglia, or gyral enhancement patterns. Contrast-enhanced MR scanning is superior to CT Scans in assessing meningeal and parenchymal abnormalities although it would not be out of place to mention that accessibility to this form of imaging is still limited in India and in much of the developing world. Moreover, children often require a general anesthetic to undergo MR scanning, whereas CT Scans may be possible with sedation. Kumar et al.[15] have proposed that basal meningeal enhancement or tuberculoma or both were 89% sensitive and 100% specific for TBM. Several specific characteristics of the basal enhancement have been described by various authors.[17–19] Long-term sequelae may include areas of calcifications.
On CT Scans, tuberculomas appear as low- or high-density round or lobulated masses with irregular walls showing homogenous enhancement after contrast administration [Figure 1]. They may be solitary or multiple [Figure 2] and have a predilection to occur in the frontal and parietal lobes.[20] The radiographic appearance of tuberculomas is thought to depend on whether the lesion is noncaseating, caseating with a solid center or caseating with a liquid center. The degree of perilesional edema has been described as being inversely proportional to duration of the lesion.[21] The so-called “target sign”[22] with a central nidus of calcification surrounded by a ring of enhancement was once thought to be diagnostic of a tuberculoma, but is now known to be quite non specific. Magnetic resonance spectroscopy has been suggested as a method to distinguish tuberculomas from cysticercosis. [23] It must be emphasized at this stage that tuberculous brain abscesses cannot be distinguished reliably from pyogenic brain abscesses by radiological parameters, and hence have to be treated in a similar manner to the pyogenic abscesses.
Figure 1.

Uniformly contrast-enhancing lesion in a 7-year-old girl
Figure 2.
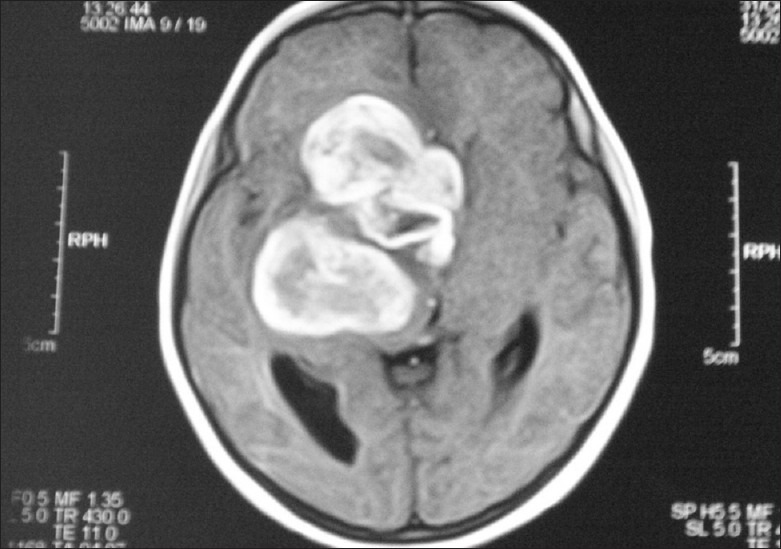
MR Scan of a 6-year-old with a double lesion which turned out to be turberculomas
Treatment
Medical therapy for CNS tuberculosis is with accepted practice norms and a discussion of details of this is outside the purview of this article. Suffice it is to note that isoniazid, rifampicin, pyrazinamide and ethambutol are recommended as a 4-drug regime to commence treatment. Second-line agents including aminoglycosides, capreomycin and fluoroquinolones may be added if there is a suspicion of multi-drug resistant (MDR) tuberculosis. There is still controversy regarding duration of therapy, with one school advocating 6-9 months therapy and another school advocating 18 months treatment.[24,25] The use of corticosteroids in CNS tuberculosis remains a controversial issue. A recent meta-analysis by Prasad[26] found the use of steroids resulted in fewer deaths in children, but the sample sizes of most of the quoted studies were fairly small. Thwaites[27] has reported on a large placebo-controlled trial of dexamethasone in TBM and noted a significant reduction in mortality though not in morbidity. However, all his patients were adults. Today most accept the use of dexamethasone as an adjunct in CNS tuberculosis. It has been postulated that dexamethasone reduces the deleterious effects of the immune response and also reduces the incidence of hydrocephalus and brain infarction.
What is the role of surgery in TBM? There are three causes of deterioration in patients with TBM-seizures, infarcts and hydrocephalus. If hydrocephalus is the cause of clinical deterioration, repeated lumbar punctures or external ventricular drainage has been recommended.[6,28,29] All authors have advised caution, and indeed the Vellore series[28,29] clearly demonstrated that good results were only obtained if a) the clinical grades of the patients were good and 2) the CSF diversion procedure was done prior to clinical deterioration. More recently, endoscopic third ventriculostomy (ETV) was suggested as an option, but success with this condition has been variable[30,31] and the procedure itself is technically difficult in the acute stage of the disease. The floor of the third ventricle is thick and the subarachnoid space itself is completely filled with exudates, and anatomical landmarks are most often difficult to ascertain. There is no doubt that medical therapy should be tried prior to any form of surgical intervention; mannitol, frusemide, acetazolamide and of course dexamethasone should be used first. It has been reported that conservative management can avoid surgery in 70% of patients with post-tuberculous hydrocephalus.[32]
We have proposed[6] external ventricular drainage as the procedure of choice in combating hydrocephalus that does not respond to conservative measures, assessed both clinically and radiologically. This is because it is a quick, easy way to reduce ICP, permits ICP monitoring to assess whether clinical improvement correlates with reduction of ICP, and indeed establishes whether there is raised ICP in the children having significant ventriculomegaly. We are convinced that a group of children has ventriculomegaly secondary to "brain softening" possibly due to multiple small infarcts and children of this group (clinically poor grade in the Vellore studies) do not improve with ventricular drainage. Hence, it is easy to decide which children may benefit from a permanent CSF diversion procedure, be it ETV or ventriculoperitoneal shunt.
The complication rate of shunt surgery in these patients is much higher; poor general condition including malnutrition, as well as depressed levels of immunity have been cited as the two main causes of higher infection rate in these patients. Agarwal et al.[33] quoted a shunt complication rate of as high as 30% although the numbers were small. We[6] have reported a shunt infection rate of 15.6% in an earlier retrospective study.
As far as tuberculomas in children are concerned, Bhagwati[34] reported on 31 children, of whom 5 needed surgical intervention-in four of them because they were thought to harbor brain tumors and in the fifth one because of significant mass effect in spite of treatment. The indications of surgery today are very small because adequate chemotherapy with anti-edema measures and dexamethasone can preclude development of acute mass effects in the majority of cases. Most lesions completely disappear with conservative treatment [Figure 3]. Obviously, the two main indications remain the same-where there is diagnostic confusion from astrocytomas, even after MR spectroscopy and other tests, and where there are features of acute rise in intracranial tension in spite of medical treatment. Some authors have advocated subtotal removal in this situation to help diagnosis and reduction of ICP, rather than attempt any radical removal. The clinical manifestations of tuberculomas depend on their location-and this may be supratentorial, in the brainstem,[35] elsewhere in the posterior fossa, or even in the sella.[36] Multiple tuberculomas have even been described in the brain and spinal cord together.[37] Cases of intraventricular tuberculomas presenting as ventricular tumors have been described, and in these situations removal is necessary.[38]
Figure 3.

Small tuberculoma in a 7-year-old which completely resolved with conservative treatment (3 months after AT drug administration)
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Rich AR, McCordock HA. The pathogenesis of tuberculous meningitis. Bull Johns Hopkins Hosp. 1933;52:5–37. [Google Scholar]
- 2.Bermudez LE, Sangari FJ. Cellular and molecular mechanisms of internalizationof mycobacteria by host cells. Microbes Infect. 2001;3:37–42. doi: 10.1016/s1286-4579(00)01355-1. [DOI] [PubMed] [Google Scholar]
- 3.Bryan-Rock R, Olin M, Baker CA, Molitor TW, Peterson PK. Central nervous system tuberculosis: Pathogenesis and clinical aspects. Clin Microbiol Rev. 2008;21:243–61. doi: 10.1128/CMR.00042-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Caws M, Thwaites G, Dunstan S, Hawn TR, Lan NT, Thuong NT, et al. The influence of host and bacterial genotype on the development of disseminated disease with mycobacterium tuberculosis. PLoS Pathog. 2008;4:e1000034. doi: 10.1371/journal.ppat.1000034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cherian A, Thomas SV. Central nervous system tuberculosis. Afr Health Sci. 2011;11:121–7. [PMC free article] [PubMed] [Google Scholar]
- 6.Sil K, Chatterjee S. Shunting in tuberculous meningitis: A surgeon's nightmare. Childs Nerv Syst. 2008;24:1029–32. doi: 10.1007/s00381-008-0620-x. [DOI] [PubMed] [Google Scholar]
- 7.Garg RK. Tuberculosis of the central nervous system. Postgrad Med J. 1999;75:133–40. doi: 10.1136/pgmj.75.881.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sütlaş PN, Unal A, Forta H, Senol S, Kirbaş D. Tuberculous meningitis in adults: Review of 61 cases. Infection. 2003;31:387–91. doi: 10.1007/s15010-003-3179-1. [DOI] [PubMed] [Google Scholar]
- 9.WHO report. Geneva: World Health Organization; 2007. WHO. Global tuberculosis control: Surveillance, planning, financing. WHO/HTM/TB2007.376ed. [Google Scholar]
- 10.Kumar R, Singh SN, Kohli N. A diagnostic rule for tuberculous meningitis. Arch Dis Child. 1999;81:221–4. doi: 10.1136/adc.81.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ahuja GK, Mohan KK, Prasad K, Behari M. Diagnotic criteria for tuberculous meningitis and their validation. Tuber Lung Dis. 1994;75:149–52. doi: 10.1016/0962-8479(94)90045-0. [DOI] [PubMed] [Google Scholar]
- 12.Kulkarni SP, Jaleel MA, Kadival GV. Evaluation of an in-house-developed PCR for the diagnosis of tubertculous meningitis in Indian children. J Med Microbiol. 2005;54:369–73. doi: 10.1099/jmm.0.45801-0. [DOI] [PubMed] [Google Scholar]
- 13.Pai M, Zwerling A, Menzies D. T-cell based assays forthe diagnosis of latent tuberculosis infection: An update. Ann Intern Med. 2008;149:177–84. doi: 10.7326/0003-4819-149-3-200808050-00241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chandramukhi A, Bothamley GH, Brennan PJ, Ivanyi J. Levels of antibody to detect antigens of mycobacterium tuberculosis in tuberculous meningitis. J Clin Microbiol. 1989;27:821–5. doi: 10.1128/jcm.27.5.821-825.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kumar R, Kohli N, Thaynani A, Kumar P, Kohli N. Value of CT scan in the diagnosis of meningitis. Indian Pediatr. 1996;33:465–8. [PubMed] [Google Scholar]
- 16.Kumar R, Pandey CK, Bose N, Sahay S. Tuberculous brain abscess: Clinical presentation, pathophysiology and treatment(in children) Childs NervSyst. 2002;18:118–23. doi: 10.1007/s00381-002-0575-2. [DOI] [PubMed] [Google Scholar]
- 17.Andronikou S, Wieselthaler N. Modern imaging of tuberculosis in children: Thoracic, central nervous system and abdominal tuberculosis. Pediatr Radiol. 2004;34:861–75. doi: 10.1007/s00247-004-1236-2. [DOI] [PubMed] [Google Scholar]
- 18.Andronikou S, Smith B, Hatherhill M, Douis H, Wilmshurst J. Definitive neuroradiological diagnostic features of tuberculous meningitis in children. Pediatr Radiol. 2004;34:876–85. doi: 10.1007/s00247-004-1237-1. [DOI] [PubMed] [Google Scholar]
- 19.Przbojewski S, Andronikou S, Wilmshurst J. Objective CT criteria to determine the presence of abnormal basal enhancement in children with suspected tuberculous meningitis. Pediatr Radiol. 2006;36:687–96. doi: 10.1007/s00247-006-0160-z. [DOI] [PubMed] [Google Scholar]
- 20.Bernaerts A, Vanhoenacker FM, Parizel PM, Van Goethem JW, Van Altena R, Laridon A, et al. Tuberculosis of the central nervous system: Overview of neuroradiological findings. Eur Radiol. 2003;13:1876–90. doi: 10.1007/s00330-002-1608-7. [DOI] [PubMed] [Google Scholar]
- 21.Pauranik A, Behari M, Maheshwari MC. Appearance of tuberculoma during treatment of tuberculous meningitis. Jpn J Med. 1987;26:332–4. doi: 10.2169/internalmedicine1962.26.332. [DOI] [PubMed] [Google Scholar]
- 22.Bargalló J, Berenguer J, García-Barrionuevo J, Ubeda B, Bargalló N, Cardenal C, et al. The “target sign”: Is it a specific sign of CNS tuberculoma? Neuroadiology. 1996;38:547–50. doi: 10.1007/BF00626095. [DOI] [PubMed] [Google Scholar]
- 23.Pretell EJ, Martinot C, Jr, Garcia HH, Alvarado M, Bustos JA, Martinot C Cysticercosis Working Group in Peru. Differential diagnosis between cerebral tuberculosis and neurocysticercosis by magnetic resonance spectroscopy. J Comput Assist Tomogr. 2005;29:112–4. doi: 10.1097/01.rct.0000149959.63294.8f. [DOI] [PubMed] [Google Scholar]
- 24.Donald PR, Schoeman JF, Van Zyl LE, De Villiers JN, Pretorius M, Springer P. Intensive short course chemotherapy in the management of tuberculous meningitis. Int J Tuberc Lung Dis. 1998;2:704–11. [PubMed] [Google Scholar]
- 25.Misra UK, Kalita J, Srivastava M, Mandal SK. Prognosis of tuberculous meningitis: A multivariate analysis. J NeurolSci. 1996;137:57–61. doi: 10.1016/0022-510x(95)00334-x. [DOI] [PubMed] [Google Scholar]
- 26.Prasad K, Volmink J, Menon GR. Dteroids for treating tuberculous meningitis. Cochrane Database Syst Rev. 2000:CD002244. doi: 10.1002/14651858.CD002244. [DOI] [PubMed] [Google Scholar]
- 27.Thwaites GE, Tran TH. Tuberculous meningitis: Many questions, too few answers. Lancet Neurol. 2005;4:160–70. doi: 10.1016/S1474-4422(05)01013-6. [DOI] [PubMed] [Google Scholar]
- 28.Palur R, Rajshekhar V, Chandy MJ, Joseph T, Abraham J. Shunt surgery for hydrocephalus in tuberculous meningitis: A long term follow-up study. J Neurosurg. 1991;74:64–9. doi: 10.3171/jns.1991.74.1.0064. [DOI] [PubMed] [Google Scholar]
- 29.Rajsekhar V. Management of hydrocephalus in patients with tuberculous meningitis. Neurol India. 2009;57:368–74. doi: 10.4103/0028-3886.55572. [DOI] [PubMed] [Google Scholar]
- 30.Figaji AA, Fieggen AG, Peter JC. Endoscopic third ventriculostomy in tuberculous meningitis. Childs Nerv Syst. 2003;19:217–25. doi: 10.1007/s00381-003-0730-4. [DOI] [PubMed] [Google Scholar]
- 31.Jonathan A, Rajsekhar V. Endoscopic third ventriculostomy for chronic hydrocephalus following tuberculous meningitis. Surg Neurol. 2005;63:32–4. doi: 10.1016/j.surneu.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 32.Lamprecht D, Schoeman J, Donald P, Hartzenberg H. Ventriculoperitoneal shunting in childhood tuberculous meningitis. Br J Neurosurg. 2001;15:119–25. doi: 10.1080/02688690020036801. [DOI] [PubMed] [Google Scholar]
- 33.Agarwal D, Gupta A, Mehta VS. Role of shunt surgery in pediatric tubercular meningitis with hydrocephalus. Indian Paediatr. 2005;42:245–50. [PubMed] [Google Scholar]
- 34.Bhagwati S, Parulekar GD. Management of intracranial tuberculoma in children. Childs Nerv Syst. 1986;2:32–4. doi: 10.1007/BF00274030. [DOI] [PubMed] [Google Scholar]
- 35.Rajsekhar V, Chandy MJ. Tuberculomas presenting as isolated brain stem masses. Br J Neurosurg. 1997;11:127–33. doi: 10.1080/02688699746474. [DOI] [PubMed] [Google Scholar]
- 36.Ghosh S, Chandy MJ. Intrasellartuberculoma. Clin Neurol Neurosurg. 1992;94:251–2. doi: 10.1016/0303-8467(92)90098-n. [DOI] [PubMed] [Google Scholar]
- 37.Yen HL, Lee RJ, Lin JW, Chen HJ. Multiple tuberculomas in the brain and spinal cord: A case report. Spine (Phila Pa 1976) 2003;28:E499–502. doi: 10.1097/01.BRS.0000099114.40764.46. [DOI] [PubMed] [Google Scholar]
- 38.Desai K, Nadkarni T, Bhatjiwale M, Goel A. Intraventriculartuberculoma. Neurol Med Chir (Tokyo) 2002;42:501–3. doi: 10.2176/nmc.42.501. [DOI] [PubMed] [Google Scholar]


