Abstract
BACKGROUND:
Reflexology is one of the non-pharmacological pain relief methods, and since it is a non-invasive, inexpensive and applicable technique, it can be used by a skilled and trained midwife. This study aimed to review the effect of reflexology on the pain and outcomes of the labor.
METHODS:
In this quasi-experimental study, 88 primiparous mothers referred to selected hospitals of Isfahan for vaginal delivery were selected using simple random sampling method and then randomized in two groups. Data collection tools were the demographic data questionnaire, profile and outcomes of the labor and the short-form of the McGill Questionnaire for Pain Rating Index (PRI) assessment. The intervention was general and specific reflexology in the active phase of labor. PRI was assessed before the intervention and four times after the intervention (3-5 cm, 6-8 cm and 9-10 cm dilatations and second stage of labor.
RESULTS:
There was no significant difference between groups before intervention. In the reflexology group, there was a significant difference between the PRI before and after the 4 stages intervention (p < 0.001). PRI was different significantly between studied groups after intervention (p < 0.001). The length of active phase of labor was different significantly between the two groups; but this difference was not significant during the second (p = 0.29), and the third (p = 0.27) stages. The difference between the 1st minute and the 5th minute Apgar score (p < 0.001) and rate of hemorrhage between the two groups were different significantly (p = 0.02).
CONCLUSIONS:
Reflexology can lead to decrease in the labor pain. Therefore, regarding to the safety of this technique, it can be replaced as an alternative for pharmacological methods.
Keywords: Reflexology, labor pain, primiparous
Labor can be considered as one of the human's physiological behaviors; which its creation cycle has remained unchanged from the beginning of the human creation. And meanwhile, labor pain -which in fact is one of the main symptoms of starting the labor process- perhaps, is the most unbearable part for the mothers, but indeed it also is the most mysterious parts.1 Labor pain is a process which can affect on all the aspects of the maternal life of the mother and other family members.2 In the first stage of uterine hypoxia all the following factors are affective on the pain feeling: accumulation of lactic acid, cervical and lower uterine segment dilatation, pressure on the fallopian tubes, pelvic bones and uterine ligaments. In the second stage, pelvic floor muscle tension, vagina, perineal, and vulva and pressure on the urethra, bladder and rectum can cause the pain.3
Fear of delivery leads to increase the irregular use of cesarean method. World Health Organization proposed the rate of 10-15% for delivery in cesarean method. However, despite the suggestion of the organization, in order to decline to the rate of 10% cesarean use until 2010, its growth rate is increasing so that it reached to 30% of the births.4 According to the statistics of Ministry of Health, Treatment and Medical Education, the prevalence of cesarean in Iran averagely is three times higher than the global statistics.5
According to the Isfahan Department of Treatment, rate of cesarean delivery in 2004 was 59% and in 2008 reached to 60% and in some of the private centers will reach to 98%. According to the Isfahan Department of Treatment the rate of announced cesarean delivery from 2004 to 2009 respectively were 59.5%, 59%, 60%, 60.5% and 59.82%. Considering this statistics, community health policymakers should predicate its complications over time and from now on think about a solution to reduce its rate.6
If the situation of our country continues the same in the next years, the primiparous mothers who had been cesarean with a high parentage would need repeated cesareans in the subsequent pregnancies. And if in the subsequent pregnancies, some of the mothers undergo cesarean (a number of them due to midwife's reasons and others due to personal request); it would be predictable that during the next twenty years, the cesarean rate would be higher than ever.7 In short, fear of the labor pain can be controlled through pregnancy preparation classes and also planning for pain relief of the labor and delivery.8
Labor pain management can be done in two methods: pharmacological and non-pharmacological methods.9 The non-pharmacological methods including massage, reflexology, touch therapy, relaxation, dancing, heat & cold therapy (e.g. taking a shower or hot bath), trance subcutaneous nerve stimulation and water therapy, acupressure, aromatherapy and music therapy. Some believed these techniques had been very effective on pain relief. The pharmacological methods of pain relieving including receiving narcotics drugs such as Pethidine, using Entonox gas and the types of topical anesthetics such as pudendal block, paracervical block, spinal block and epidural analgesia and etc.
Pharmaceutical measures are often expensive and have harmful effects for reducing labor pain.10 In the pharmacological methods, the pain feeling would be reduced physiologically but psychological and emotional conditions of the mothers are ignored.11
Reflexology as one of the branches of the complementary medicine is a gentle art and an individual healing form and type of a prospective comprehensive treatment which believes the individual and his/her disease cannot be divided into separate treatable parts, but he/she should be considered and treated as a whole person which consists of body, mind, emotions, spirit and feelings which each of them are influencing and contrasting the other. In fact, reflexology affects the physiological and psychological stimulation points.12–15 Reflexology in the pregnancy period, labor and postpartum period can be usable for treating many physiological conditions such as nausea, pregnancy vomiting, constipation, headache and low back pain even in the breastfeeding period.16
In the reflexology, with massage and skin contrast, enkephalins and endorphins are secreted and can reduce the anxiety and pain. This technique can bring about the sense of well being and healthy. In addition, analgesia may be established by pressure on the specific reflex points. Generally, reflexology techniques would stop the neural transmission of the pain message to the brain and subsequently the perception of pain relief through control gate.15,17,18
McNeill et al in their study found that reflexology had been effective on reduction of the labor pain and length.16 Furthermore, Motha & McGrath found that reflexology not only can reduce the labor pain and analgesic drugs using, but also can reduce the length of the labor with significant results.19
Based on several studies about using complementary medicine therapy (as a non-pharmacological methods for labor analgesics), very few studies with detailed design have been done on using complementary medicine in pregnancy and labor. However, many of the effective complementary medicine methods such as massage, reflexology, touch therapy, heat & cold therapy, water therapy, aromatherapy and music therapy which are done by the midwives, are also using to reduce the labor pain.20 Since there had not been any study on labor and delivery pain control, we decided to conduct this study to determine the effect of reflexology on pain and some of the other features of labor (labor length) and its consequences (Apgar score, hemorrhage rate and vital signs after the delivery) in the primiparous women who referred to the selected hospitals of Isfahan.
Method
This was a quasi-experimental study on primiparous mothers who had referred for vaginal delivery in 2010 to the selected hospital of Isfahan (Asgarieh and Shahid Beheshti Hospitals). The inclusion criteria were as the following:
Primiparous mothers with age range of 18-35 years old, originality Iranian-born, Muslim, dilatation 3-5 cm with regular uterine contractions, minimum 3 contractions per 10 min (proper in terms of intensity, duration and the number of contractions so that the duration be < 30 seconds and > 60 seconds), gestational age of full 37 to 41 weeks, single pregnancy and displaying fetus cephalic.
The non-inclusion criteria were as the following:
Multiparous women, originality non-Iranian, history of infertility, women who lived alone, history of incarceration in jail, infectious disease and fever, catching underlying diseases such as diabetes, hypertension, asthma, kidney, psychological disorders, epilepsy or seizures and any disease related to pregnancy such as gestational diabetes, pregnancy blood pressure, and poly-hydramnios or oligohydramnios, the history of any midwifery problem during this labor (placenta previa, abortion risk), and any disorder which may be inconsistent with a natural vaginal delivery (pelvic anatomic disorders, pelvic tight, prolongation in the latent phase of the labor and etc.), history of severe varicose veins, injuries and legions, mass, corns, calluses and foot mycosis.
The exclusion criteria also were as the following:
Unwillingness to continue the reflexology or routine labor hospital care, fetal distress, hemorrhage and etc during the study and incidence of any non-diagnosed dystocia.
Sampling method was in simple sampling and the subjects, regarding the inclusion criteria, randomly divided into intervention and control groups. In this study, collecting the data was used by observation, examination and questionnaires. The questionnaire consisted of 3 parts; 1. Individual information (demographic characteristics and gestational age), 2. Features and outcomes of the labor (the length of the active phase of the first stage of the labor, the second and third stages, Apgar score in 1-5 minutes after the labor, hemorrhage rate after labor and vital signs in the first hour after the labor (the fourth stage of labor), and 3. Pain Rating Index (PRI) assessment using the short-form of McGill Questionnaire. The pain questionnaire was filled in by the study subjects of both groups once before the intervention in 3-5 cm dilatation, and four times after the intervention in 3-5 cm, 6-8 cm (after the first intervention) and 9-10 cm dilatations and in the second stage of labor (after the second intervention). The validity and reliability of the questionnaire have been confirmed in the previous studies.21
To calculate the length of different stages of the labor (the active phase of the first stage, second and third stages), an analog clock with second hand was used. The timer and the person who calculated the time was only one (researcher) to the end of the study to minimize the error. Apgar score in 1 to 5 minutes after the labor in the born neonate was assessed based on one of the five characteristics of heart rate, respiratory effort, muscle tone, reflex irritability, and skin color and zero score to two were dedicated to them and the total score was calculated. Hemorrhage in the fourth stage (1 hour after the labor) was calculated with counting the number of pads which were saturated with blood (in side lying position) and the remained blood stains on the pads in the desired duration was reviewed and assessed. Vital signs of heart rate and pulse were calculated by touching the radial next to the ulna bone and its counting in a full minute, respiratory rate by visual counting of the number of up and down of the chest in a full minute, blood pressure by a mercury barometer device which had been calibrated at beginning of every morning and body temperature by an instant personal tab of ever person were calculated by a certain researcher at the end of the study. At the end, the mean score of vital signs measurements which had been controlled four times were calculated.
In the intervention group, at the time of entering to the active phase of labor, the intervention was conducted as the following: carrying out reflexology for 30 minutes on each foot (60 minutes in total) as general reflexology including 15 stages; 1. Solar plexus, 2 & 3, Areas related to the digestive viscera, 4. Pelvic area, 5. Pituitary, 6. Sinuses, 7. upper and lower extremities (external sides of the feet), 8. Spinal cord (inner sides of the feet), 9. Lungs, 10. Shallow chest area, 11 & 12. The sides on the feet, 13. Ovaries, 14. Uterus and 15. fallopian tubes; and the specific reflexology including the areas related to labor pain such as liver, spleen, kidney, pituitary, solar plexus and uterus. Specific reflexology was performed during the first period and again for the second time in 9-10 cm dilatation by emphasis on specific points for at least five minutes. In this group, the mothers received 1000 cc dextrose-saline serum from the beginning of active phase to the labor time and after the labor. In the control group, routine cares was done as the following: controlling fetal heart and uterine contractions every 15 minutes and controlling vital signs every 1 hour. In this group, all the mothers received 1000 cc dextrose-saline ƒ serum containing Oxytocin 10 units which started from the beginning of active phase. Thereafter, additional Oxytocin 10 units added to the serum.
Results
In the routing care group, 112 people entered and 68 of them excluded from the study due to various reasons (using Pethidine for pain relieving, cesarean and postpartum hemorrhage). In the reflexology group, 45 people entered and one of them discharged from the hospital by the personal satisfaction. Mean age of the reflexology and routine care study subjects was 25.22 and 24.02 years, respectively and mean gestational age of the reflexology and routine care groups was 39.44 and 39.27 weeks, respectively. The majority of the participants in the reflexology group (23 people; 5.3%) and in the routine care group (27 people; 61.4%) lived in their own personal properties. The majority of the participants in the reflexology and routine care groups (41 people, 93.2%) were housekeepers. The educational level of most of the participants in the intervention group (43 subjects; 97.7%) and control group (44 subjects; 100%) was high school graduates and lower. Statistically there was no significant difference between the two groups in terms of demographic characteristics and gestational age.
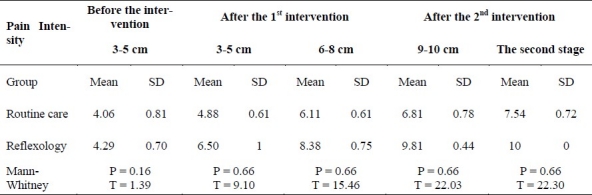
Mean pain intensity in PRI Scale in the study subjects of the both groups before and after the intervention is presented in Table 1. In a comparison which was done before and after the study in the intervention group based on PRI scale using Wilcoxon test, there was a significant difference between PRI before and after the intervention in each of the dilatations and the second stage of labor after the second intervention (p < 0.001).
Table 1.
Mean pain intensity in PRI Scale in the study subjects of the both groups before and after the intervention

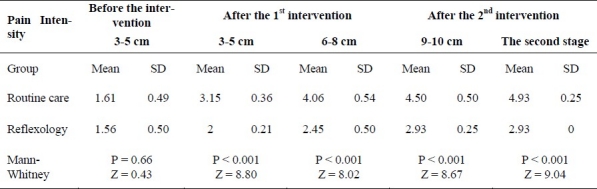
Mean pain intensity in VAS Scale in the study subjects of the both groups before and after the intervention is presented in Table 2. There was a significant difference before and after the study in the reflexology group based on VAS index, in each of the dilatations of 3-5 cm after the first intervention, 6-8 cm after the first intervention, 9-10 cm and the second stage of labor after the second intervention there was a significant difference before and after the intervention (p < 0.001).
Table 2.
Mean pain intensity in VAS Scale in the study subjects of the both groups before and after the intervention
Mean pain intensity was considered based on the assessment scale which was as zero i.e. no pain to 5 i.e. fatal pain. Mean score of the pain intensity after assessing the study subjects of the both groups before and after the intervention is presented in Table 3. Wilcoxon test indicated that in each of the dilatations of 3-5 cm after the first intervention, 6-8 cm after the first intervention, 9-10 cm and the second stage of labor after the second intervention four stage of intervention, there was a significant difference between pain intensity before and after the intervention in the reflexology group (p < 0.001).
Table 3.
Mean score of the pain intensity after assessing the study subjects of the both groups before and after the intervention
The length of active phase of the first stage of the labor in the study subjects showed that cervical dilatation of most of the participants of the study i.e. 23 subjects (52.2%) in the intervention group was completed during 60-120 minutes and 32 subjects (72.7%) in the routine care group over 301 minutes. The difference duration of active phase between the two groups was significant (p = 0.001). Mean and standard deviation in length of the second stage of labor in the study subjects of reflexology group and routine care group obtained 40.54 and 12.49 minutes and 43.63 and 14.79 minutes respectively and statistically was not significant (p = 0.29). Mean and standard deviation in length of the third stage of labor in the study subjects of reflexology group and routine care group obtained 7.25 and 2.48 minutes and 8.04 and 3.91 minutes respectively. ANOVA showed no difference between the two groups in terms of length of the third stage of the labor (p = 0.27).
The mean Apgar score in the first minute of birth in the reflexology and routine care groups was 9.75 and 8.97 respectively; but the mean Apgar score in the fifth minute the reflexology and routine care groups obtained 10 and 9.79 respectively. ANOVA showed that there was a significant difference between Apgar score in the first minute (p < 0.001) and the fifth minute after the birth (p < 0.001) in both groups. McNeill et al found that Apgar score in the mothers of two groups of test and control had no effect.16 The difference of the results of the mentioned study with the present study might be due to different implementation of the techniques and its time (in the study of McNill, this was done during the pregnancy period).
ANOVA indicated that the hemorrhage rate based on the number of used pads in the fourth stage (1 hour after the labor) in the routine care group significantly was higher than the reflexology group (p = 0.02). Mann-Whitney test showed that hemorrhage rate based on the blood stains left on the pads in this stage in the routine care group significantly was higher than the reflexology group (p < 0.001).
ANOVA also showed that there was a significant difference between systolic (p = 0.005) and diastolic (p < 0.001) blood pressure and pulse (p = 0.003) in the study subjects in minutes 0-15 in both groups; but this difference was not significant in both groups in minutes 16-30. ANOVA also showed that there was no significant difference between the RR of the mother in minutes 0-15 (p = 0.06), 16-30 (p = 0.8), 31-45 (p = 0.69) and minutes 46-60 (P value = 0.18) in both groups. In addition, there was no significant difference between the temperature of the mother in minutes 0-15 (p = 0.9), 16-30 (p = 0.11), 31-45 (p = 0. 9) and minutes 46-60 (p = 0.14) in both groups.
The data were analyzed by Software SPSS18 using descriptive and inferential statistics.
Discussion
The results of the present study showed that there was a significant difference between the two groups in terms of pain intensity. In the reflexology group, the results indicated a significant reduction of the pain before and after the intervention. In a study in Gentofte Hospital, Copenhagen, 58 women out of 65, who had been received reflexology in the labor, experienced a more significant pain relief.22 Feder et al in a study on the effect of reflexology on the labor found that reflexology can facilitate the labor through increase in uterine contractions, reduce the pain and the need to the intervention.23
Quinn et al in their study found that reflexology was effective in reducing the low back pain.24 Kim et al also emphasized the effect of reflexology on the premenstrual pain.25
According to the results of the present study and the mentioned studies it can be concluded that reflexology can bring about relaxation and comfort in the individual through physiological changes and release of endorphins and anesthesia feeling can create comfort. Mentioned effects can cause reduction in the maternal stress and increase her peace of mind, which consequently would have a positive effect on the labor progression and her satisfaction.
In general, reflexology can relief the pain due to several reasons: touching and skin contrast can cause the release of endogenous endorphins of the body and would reduce the stress; therefore, with stress reduction, the pain would consequently reduce and the opposite is also true, and the second reason is that, reflexology can remove the fatigue and anxiety.26
The findings of the present study indicated a difference in length of the first stage of the labor (active phase) between the two groups, but this difference in terms of duration was not significant in the second and third stages of the labor. Confirmation and supporting the present study results, McNeill et al also showed that implementing reflexology for 60 minutes could reduce the length of the labor. Dr. Cecil Mossey in White Cross Hospital also discussed that women who had received reflexology at the time of labor, their labor duration was averagely reduced 6-7 hours.22,27
Explaining the results of the present study, it should be stated that anxiety is the triggering point of pain, fear and muscle rigidity which can cause to increase the adrenaline and epinephrine level which has Anti oxytocin properties and can disrupt the uterine muscle activity and prolong the labor length.28,29 Reflexology by decreasing the adrenaline and noradrenaline and increasing endorphins and inner oxytocin, would increase uterine muscle contractions and activities and can affect the duration of the labor.30–32
The results of the study indicated that APGAR score at the first and fifth minute after the labor was significantly higher in reflexology group. Continuous pain and fear in the labor affects respiratory system, circulatory, endocrines and other activities of the body which would lead to hard and difficult labor and consequently would increase the rate of labor with instruments and cesarean and reduce the APGAR score.33
Postpartum hemorrhage in the study subjects of the routine care group was significantly higher. The results of the study done by Zhixing in Hangzhou Traditional Medical Hospital showed that from 28 patients with heavy menstrual bleeding 23 patients (82.2%) were completely healed and even in the subsequent cycles, there was no evidence of hypermenorrhea recurrence. The other 5 patients (17.8%) got improved in the same cycle, but in order for recovery in the subsequent cycles they needed continuity in the treatment using reflexology.34,35
The first hour of the labor is the most important and most dangerous time for the mother. Among the postpartum cares, controlling hemorrhage rate and maternal vital signs (blood pressure, body temperature, pulse rate and respiration) are of high importance. In the present study, the vital signs of the study subjects were measured and recorded. ANOVA showed a statistical significant difference in terms of the average pulse rate and systolic and diastolic blood pressure in the first 15-minute after the labor. But the difference in temperature and RR significantly was not significant. The results indicated that despite the non-significant difference of systolic and diastolic blood pressure and pulse rate in 16-60 minutes, systolic and diastolic blood pressure and pulse rate in the study subjects of reflexology group was lower than study subjects of routine care group.
The results also showed that mean respiratory rate in the study subjects of the reflexology group was lower than study subjects of routine care group and this was due to remove stress and anxiety and create comfort in their body due to reflexotherapy and skin contact between the therapist and the client, and this effect was also stable over time. Respiratory rate has been reduced along with increase of relaxation of the mother in the reflexology group; but if specifically it was conducted on breathing reflex points, it could also statistically be significant. In addition, despite lack of significant difference between the two groups in terms of temperature, the mean temperature of the reflexology study subjects was slightly lower than routine care study subjects.
When the reflex points are stimulated, general relaxation is created in the body. Following this relaxation, stress messages are stopped and sympathetic nervous system activity would be decrease. Therefore, there is an assumption that the patients who receive reflexology, due to reduction of their anxiety and stress level, have lower blood pressure, heart rate and respiratory rate than those who do not receive it.36
In a study by McVicar et al in 2007 about the effect of reflexology on the vital signs and other body organs; reflexology had reduced the stress of the volunteers. Vicar by measuring of cardiovascular parameters (pulse and blood pressure) showed that reflexology had been effective on reducing these parameters. In this study, the reduction of stress in the volunteers had no significant difference with the control group.37
In a study by Mirzai et al (2009) which was done to review the effect of reflexology on the primiparous women in the Afzalipour Hospital in Kerman, before the intervention, the mean scores of anxiety, pulse, systolic and diastolic blood pressure of the mothers in the case and control group had no significant difference. After the intervention, the mean score of anxiety in the case group had significantly reduced, while this score had been increased in the control group; but no significant difference was observed between the pulse and blood pressure variables of the two groups. The reason of the difference in the obtained results with the presents result was due to the method of implementing the technique.23
Conclusion
Confirmation of the effect of reflexology on labor pain, it seems that this simple and inexpensive technique can be applied in the hospitals and maternity hospitals and it can be expected that this technique would be welcomed by the physicians, treatment team members and mothers. Properly using of this technique, reflexology can reduce the labor pain and consequently prevent from using pharmacological methods such as palliative medicines which unconsciously can impose certain side effects to the individual. Generally, the results of this study which include reducing the length of the labor, labor pain intensity, postpartum hemorrhage and improving Apgar score can play an important role in promoting mothers’ health and their satisfaction. Furthermore, the results of this study should be considered in fields such as increase midwives skills in labor pain relief and wider application of midwifery staff and also educational and care planning in promoting women's health and application of the new techniques in complementary medicine.
The authors declare no conflict of interest in this study.
Acknowledgments
Thanks go to the Department of Midwifery of School of Nursing & Midwifery and Research Vice Chancellor of Isfahan University of Medical Sciences who helped us in conducting this research.
References
- 1.Margaret S. Psychiatric aspects of infertility and infertility treatments. Psychiatr Clin North Am. 2007;30(4):689–716. doi: 10.1016/j.psc.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 2.Leifer G, Alper MM, Penzias AS. 2nd ed. New York: Informa Healthcare; 2007. The Boston IVF handbook of infertility: a practical guide for practitioners who care for infertile couples. [Google Scholar]
- 3.Huntley AL, Coon JT, Ernst E. Complementary and alternative medicine for labor pain: a systematic review. Am J Obstet Gynecol. 2004;191(1):36–44. doi: 10.1016/j.ajog.2003.12.008. [DOI] [PubMed] [Google Scholar]
- 4.Mohammaditabar SH, Kiani A, Heidari M. The Survey on Tendencies of Primiparous Women for Selecting the Mode of Delivery. Journal of Babol University of Medical Sciences. 2009;11(3):54–9. [Google Scholar]
- 5.JamshidiManesh M, Oskouie SF, Jouybary L, Sanagoo A. The Process of Women's Decision Making for Selection of Cesarean Delivery. Iran Journal of Nursing. 2008;21(56):55–67. [Google Scholar]
- 6.Mahoney D. Infertility and mood disorders: breaking the cycle. [Cited 2009 Sep 10]. Available from: http://findarticles.com/p/articles/mi_hb4345/is_11_36/ai_n31062427/
- 7.Moayed Mohseni S, Mohammadi KH. Trend of increasing cesarean rate forecasts based on current available data, some. Bimonthly Official Publication of Shahed University. 2011;14(66):59–62. [Google Scholar]
- 8.Seyed Nouri T, Jamshidi Avanaki F. Relationship between knowledge and attitudes of pregnant women referred to the Health - Treatment Center of Rasht by caesarean of their choice with reasons. Journal of Medical Sciences, Gilan University School of Medicine. 2006;15(59):75–84. [Google Scholar]
- 9.Davim RMB, Vasconcelos Torres G, Melo ES. Non-pharmacological strategies on pain relief during labor: pre-testing of an instrument. Revista Latino-Americana de Enfermagem. 2007;15(6) doi: 10.1590/s0104-11692007000600015. [DOI] [PubMed] [Google Scholar]
- 10.Simkin P, Ancheta RS. 1st ed. Corporate Headquarters US: Wiley-Blackwell; 2000. The Labor Progress Handbook: Early Interventions to Prevent and Treat Dystocia. [Google Scholar]
- 11.Funai EF, Norwitz ER. Management of normal labor and delivery [Online] 2009. Available from: URL: http://www.uptodate.com/
- 12.Kuhn MA. 1st ed. Philadelphia: Lippincott Williams & Wilkins; 1999. Complementary Therapies for Health Care Providers. [Google Scholar]
- 13.Wright Janet, Sharma G, Mahajan KK, Sharma L. Shavasana--Relaxation technique to combat stress. Journal of Bodywork and Movement Therapies. 2007;11(2):173–80. [Google Scholar]
- 14.Berman AJ, Snyder SH, Kozier BJ, Erb G. 8th Edition. 8th ed. New Jersey: Prentice Hall; 2008. Kozier & Erb's Fundamentals of Nursing. [Google Scholar]
- 15.Pitman V, Mackenzie K. 2nd Edition.2nd ed. Nashville, Tennessee: Nelson Thornes; 2002. Reflexology: A Practical Approach. [Google Scholar]
- 16.McNeill JA, Alderdice FA, McMurray F. A retrospective cohort study exploring the relationship between antenatal reflexology and intranatal outcomes Complement Ther Clin Pract. 2006;12(2):119–25. doi: 10.1016/j.ctcp.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 17.Tiran D. Complementary medicine in pregnancy and childbirth in UK. International Congress Series. 2006;1287:340–4. [Google Scholar]
- 18.Tiran D, Chummun H. Complementary therapies to reduce physiological stress in pregnancy Complement Ther Nurs Midwifery. 2004;10(3):162–7. doi: 10.1016/j.ctnm.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 19.Bayer SR, Alper MM, Penzias AS. 2n ed. New York: Informa Healthcare; 2007. The Boston IVF handbook of infertility: a practical guide for practitioners who care for infertile couples. [Google Scholar]
- 20.Wickham S. Vol. 5. Amsterdam: Elsevier; 2008. Midwifery: Best Practice. [Google Scholar]
- 21.Keshavarz M, Dadgari A, Miri F. Evaluation of the Short Form McGill pain questionnaire in primiparous pregnant women referring to Fatemieh maternity. Knowledge and Health Quarterly. 2007;2(2) [Persian] [Google Scholar]
- 22.Firoozi M. Application of Reflexology in midwifery. Journal of Nursing and Midwifery Mashhad University of Medical Sciences. 2003;9(2) [Persian] [Google Scholar]
- 23.Mirzai f, Kaviani M, Jafari P. Effects of foot reflexology on pain intensity and duration of first stage labor. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2009;13(1) [Persian] [Google Scholar]
- 24.Quinn F, Baxter GD, Hughes CM. Complementary therapies in the management of low back pain: a survey of reflexologists. Complement Ther Med. 2008;16(1):9–14. doi: 10.1016/j.ctim.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 25.Kim YH, Cho SH. The Effect of Foot Reflexology on Premenstrual Syndrome and Dysmenorrhea in Female College Students. Korean J Women Health Nurs. 2002;8(2):212–21. [Google Scholar]
- 26.Peterson BD, Newton CR, Rosen KH, Skaggs GE. Gender differences in how men and women who are referred for IVF cope with infertility stress. Hum Reprod. 2006;21(9):2443–9. doi: 10.1093/humrep/del145. [DOI] [PubMed] [Google Scholar]
- 27.Miriam Z. Reflexology: Can it Help You Cope with Labor? [Online] 1999. Available from: URL: http://www.ivillage.com/
- 28.Shamaeyan Razavi N, Hadizadeh F. The Survey and Grading Stressor Factors of Delivery Unit from The View of Primigravida Women in 22- Bahman Hospital of Gonabad. Ofogh-e-Danesh. 2004;9(2):69–76. [Persian] [Google Scholar]
- 29.Alehagen S, Wijma B, Lundberg U, Wijma K. Fear, pain and stress hormones during childbirth. J Psychosom Obstet Gynaecol. 2005;26(3):153–65. doi: 10.1080/01443610400023072. [DOI] [PubMed] [Google Scholar]
- 30.Abasi Z, Abedian Z, Fadaii A. The Effect of massage on the duration of first stage labor. Arak Medical University Journal. 2008;11(1) [Persian] [Google Scholar]
- 31.Yildirim G, Sahin NH. The effect of breathing and skin stimulation techniques on labour pain perception of Turkish women. Pain Res Manag. 2004;9(4):183–7. doi: 10.1155/2004/686913. [DOI] [PubMed] [Google Scholar]
- 32.Speroff L. Clincal gynecologic endocrinology and infertility. In: Ghazijahani B, Mohajerani S, Fadaei A, translators. Tehran: Golban Arian Teb Ghazijahani; 2008. [In Persian] [Google Scholar]
- 33.Safarzadeh A, Khodakarami N, Fathizadeh N, Safdari Deh Cheshme F. Massage therapy effects on labor pain in primiparous women. Sahre Kord University of Medical Sciences Journal. 2008;9(4) [Persian] [Google Scholar]
- 34.Katz VL. 5th ed. Philadelphia: Mosby Elsevier; 2007. Comprehensive gynecology. [Google Scholar]
- 35.Endrikat JS, Milchev NP, Kapamadzija A, Georgievska J, Gerlinger C, Schmidt W, et al. Bleeding pattern, tolerance and patient satisfaction with a drospirenone-containing oral contraceptive evaluated in 3488 women in Europe, the Middle East and Canada. Contraception. 2009;79(6):428–32. doi: 10.1016/j.contraception.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 36.Gunnarsdottir TJ, Jonsdottir H. Does the experimental design capture the effects of complementary therapy? A study using reflexology for patients undergoing coronary artery bypass graft surgery. J Clin Nurs. 2007;16(4):777–85. doi: 10.1111/j.1365-2702.2006.01634.x. [DOI] [PubMed] [Google Scholar]
- 37.McVicar AJ, Greenwood CR, Fewell F, D’Arcy V, Chandrasekharan S, Alldridge LC. Evaluation of anxiety, salivary cortisol and melatonin secretion following reflexology treatment: a pilot study in healthy individuals. Complement Ther Clin Pract. 2007;13(3):137–45. doi: 10.1016/j.ctcp.2006.11.001. [DOI] [PubMed] [Google Scholar]


