Abstract
BACKGROUND:
Since premenstrual syndrome (PMS) can cause suicide, dissociation of familial relationships, abnormalities in the daily work and inter-personal relationships in the patients, and bring about direct and indirect economic burden for the society, it is important to resolve the problems of the patients. The objective of the current study is to determine the effect of magnesium (Mg), combination of vitamin B6 and Mg, and the placebo on the severity of PMS in the patients affected by the disease referred to the health centers of Isfahan University of Medical Sciences during 2009-2010.
METHODS:
The participants were randomly assigned to two intervention groups and one control group. The study was carried out for four months in ten selected health centers in Isfahan. To confirm the PMS diagnosis in patients, they were asked to fill out the PMS daily symptom record form for two months and then, when the diagnosis was confirmed, the participants were randomly assigned to one of the three groups of the study (Mg, Mg plus vitamin B6, and placebo). Medical intervention was carried out in two menstrual cycles and the results of pre- and post-test were compared.
RESULTS:
After the intervention, the mean score of PMS significantly decreased in all the three groups (p < 0.05). The decrease was the greatest in the Mg plus vitamin B6 group, and was the least in the placebo group.
CONCLUSIONS:
The findings indicated that Mg plus vitamin B6 and placebo has the greatest and the least effect on the mean score of PMS, respectively.
Keywords: Premenstrual syndrome, magnesium, vitamin B6
Premenstrual syndrome (PMS) affects millions of women around the world and is known as the most important disorder in women.1 It has been estimated that 80-90% of women experience the symptoms of PMS in reproductive age, among whom the symptoms are severe in 3-8%.2 The diagnostic criteria of American Psychiatry Association (APA) for diagnosis of PMS are as follows: if at least five of the following symptoms and signs are present in the daily symptom record form during the last week of the luteal phase up to the first four day of the next menstrual cycle for at least two cycles, and the signs and symptoms interfere with the daily life and relationship of the individual, and the symptoms do not originate from the aggravation of psychiatric disorders.3
Various etiologies have been proposed to explain the underlying cause of the syndrome, and thus different therapeutic approaches have been introduced for the disease. This can be largely due to multi-factorial nature of the disorder and the role of different biological, psychological, and social factors in its development, as well as the overlap of the symptoms of the syndrome with those of many different psychological and gynecological diseases.4 One of the treatment approaches proposed for the syndrome is the supplementation therapy, including those containing magnesium (Mg).
Abraham was the first one who proposed magnesium deficiency as the underlying causes as well as the aggravation factor of the PMS symptoms. He believed that the relief of the symptoms after administration of Mg results from the relaxing effect of Mg in controlling the neuromuscular stimulations.5 The Mg level of erythrocytes and leukocytes of women with PMS is lower than that in the women without the syndrome.6 Although the effect of pure Mg supplement on treatment of PMS symptoms has been confirmed in different studies, it seems that better results can be achieved by combination of Mg and vitamins. One of the suggested combinations for treatment of PMS symptoms is the combination of vitamin B6 and Mg. Many studies have been carried out on effectiveness of these combinations, but so far no decisive result has been obtained in this regard, and further studies are required to confirm their effectiveness and safety. Thus, considering what was mentioned above, the importance of the syndrome in occurrence of personal and social problems, as well as the affordability, availability, and safety of Mg and vitamin B6, the current study was carried out to determine the effect of Mg, the combination of Mg-vitamin B6, and the placebo on the PMS symptoms.
Method
This is a double-blinded placebo-controlled clinical trial, in which coding method was used for blinding. To this end, the medicine boxes were coded and then handed in to the researcher, and only at the end of the study and after decoding, the contents of the boxes were specified. The study was approved by the Ethical Committee of Isfahan University of Medical Sciences. After checking to meet the inclusion and exclusion criteria and filling out the questionnaire on the symptoms of primary diagnosis of PMS, the patients were evaluated for depression and anxiety using Beck's depression test and Holms’ anxiety criteria. If a participant was not affected by depression or anxiety disorder, she was asked to fill out the PMS daily symptom record form for two months.
The study population was women of 15-45, referred to the selected health centers, who were affected by the PMS according to the criteria of American Psychiatry Association, and also met the inclusion criteria (being 15-45 years old, having regular menstrual cycle, not being affected by depression or anxiety, not having an acute or chronic disease, not taking medicines or supplements, and not taking regular exercise).
The study was carried out in two steps. In the first step, 170 women entered the study and were asked to fill out the daily symptom record form for two months. In this step, 165 women returned back the questionnaires, out of which 150 were affected by the syndrome, as indicated by the data analysis. They were randomly assigned to three groups, each consisting of 50 participants. Then, the participants of the Mg group daily received one Mg tablet (250 mg). The participants of Mg plus vitamin B6 daily received a tablet containing 250 mg Mg plus 40 mg vitamin B6, apparently similar to the Mg tablet. Each day, the participants of the placebo group received one placebo tablet, apparently similar to the tablets of the two other groups. The tablets given to the three groups were prepared by Isfahan Faculty of Pharmacy. In the second step, the participants were asked to continue regular record of their daily symptoms and also to begin taking the tablet regularly from the first day of the menstrual cycle to the start of the next cycle. From among the participants, 38, 41, and 37 participants in the Mg, Mg plus vitamin B6, and placebo groups followed the study to the end. The severity of symptoms was determined using daily symptom record form and symptom rating. The participants rated their daily symptoms as zero (not having), 1 (mild), 2 (moderate), and 3 (severe). The rating was explained as follows: zero means not having the symptom, 1 (mild) means the symptom is present but does not interfere with the daily activities such as education and work, 2 (moderate) indicate the symptom affects daily activities moderately, and 3 means the symptom prevents daily activities.
The exclusion criteria were pregnancy, willingness to use hormonal contraceptive methods or taking any hormonal treatment, not taking the drug or not filling out the forms regularly, and unwillingness to continue the treatment. Data analysis was carried out using one way ANOVA, paired t-test, chi square, and Kruskal-Wallis, by SPSS software, version 15.
Results
The mean age of the participants of Mg, Mg plus vitamin B6, and placebo groups were 28.71, 30.02, and 28.03 years, respectively. The three groups were matched with respect to the a marital status, educational level, contraception method, job, body weight, height, number of children, menarche age, the interval between menstrual bleedings, and duration of bleeding (p > 0.05).
The findings showed that the three groups were not significantly different with regard to the mean score of the PMS symptoms before the menstrual cycles (p > 0.76). This is while the three groups were significantly different in this respect after the treatment (p < 0.001). Table 1 provides the mean score of the PMS symptoms before and after the intervention in the three groups.
Table 1.
Mean PMS score before and after the intervention in the three groups
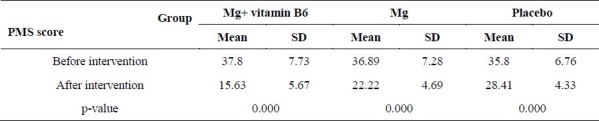
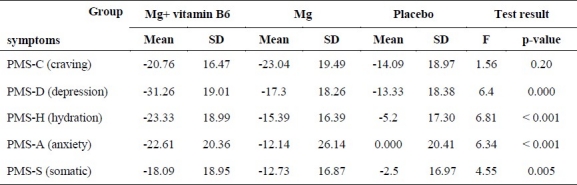
As can be observed in the table, the combination of Mg plus vitamin B6 is more effective that Mg and placebo in lowering the mean score of the PMS symptoms (p < 0.05). Considering the changes in the mean score of the PMS symptoms after the intervention, it was demonstrated that the mean score significantly decreased in all the three groups (p < 0.05). To simplify the comparison of effectiveness of each treatment, we categorized the 30 recorded symptoms into five sub-groups, according to the Abraham's classification, and then evaluated the effect of each treatment on the symptoms. The subgroups of symptoms were as follows:
Depression sub-group: including symptoms of depression and isolation, avoiding social activities, crying, dejection, inclination to remain at home, anger, forgetfulness, insomnia, and inability to concentrate.
Anxiety sub-group: including the signs of nervous tension, irritability, and anxiety.
Water retention sub-group: including breast pain and tenderness, lower extremity edema, bloating, and abdominal discomfort.
Somatic symptom sub-group: including the symptoms of feeling cold, nausea, urination frequency, flushing, low back pain, headache, acne, greasy skin, arthralgia, and muscular pain.
The effect of the interventions on each subgroup of the symptoms is presented in Table 2.
Table 2.
Comparison of the changes in the PMS symptom scores before and after the intervention in the three groups
Discussion
The results indicated that combination of Mg and vitamin B6 was more effective than Mg and placebo on decreasing the PMS symptoms. De souza et al carried out a study to determine the potential effect of combination of Mg and vitamin B6, and demonstrated that both Mg and combination of Mg and vitamin B6 can relieve the PMS symptoms.5 They reported that vitamin B6 decrease the severity of the symptoms more effectively. However, in the current study, the combination of Mg and vitamin B6 showed the highest effectiveness in relieving the PMS symptoms. The difference between the two studies can probably be explained by the higher dosage of Mg (250 mg versus 200 mg) and longer duration of treatment (two months versus one month) in the current study. Reviewing various studies on the effect of Mg on the PMS symptoms indicate that at least two months is required for presentation of the therapeutic effects of Mg. This is also true for the combination of Mg and vitamin B6.5,7 One of the main differences of the study carried out by De souza et al with the current study is the shorter intervention in the former study, which seems to affect the results.
The difference can also be partly explained by the difference in the methodologies. For instance, the study carried out by De souza et al had a Latin square design, and each patient receive each of the combinations for one month and then immediately another combination was administered for the patient. This method would affect the results. One problem of their study was not to consider the wash-out period among the interventions, such that the observed results after administration of one drug in one patient can partially result from the previously taken drug. In the current study, the results of the study was evaluated two months after the end of the intervention, and because of the study design, the drugs could not interfere with each other.
In another study on the effect of Mg on the PMS symptoms, Facchinetti et al reported that after two months of Mg administration, the group that received Mg experienced a significant decrease in the severity of the PMS symptoms compared with the placebo group (p < 0.04).8 Moreover, they reported a significant decrease in the severity of water retention (p < 0.03) and pain (p < 0.04) symptoms. The effectiveness of Mg administration on more symptoms in the current study compared with the study by Facchinetti et al is probably because of the pattern of Mg administration. In the current study, Mg tablets (250 mg/day) was administrated from the beginning of the menstrual cycle to the start f the next cycle, while in the latter study, Mg tablets (360 mg) with magnesium pyrolidone carboxylic acid formulation was administered from the 15th day of the menstrual cycle to the start of the next cycle. By reviewing the literature, it was concluded that the daily need of magnesium in a normal individual is 320 mg, and the normal kidney excretes extra load of Mg in the urine to prevent toxicity. Thus, administration of Mg with higher doses and for shorter courses is not helpful in alleviating the symptoms, because the extra load of Mg would be excreted in the urine. In the study carried out by Quaranta et al on effectiveness and safety of slow release Mg (Sincromag) in treatment of 41 women with PMS, it was demonstrated that Mg has the highest effectiveness on the severity of depression, craving, and anxiety symptoms.9 With regard to reducing the severity of other symptoms, Mg was effective as well. After administration of Mg for two months, a significant decrease in the severity of water retention symptoms (p = 0.009) was also reported by Walker et al Although it was reported that Mg decreased the severity of all the PMS symptoms, the decrease was not statistically significant.7 The difference observed between the study carried out by Walker et al and the current one can be partially because of the lower mean age of the participants in the Walker et al's study (15-25 years versus 28-30 years). Because of the younger ages, the participants’ diet included more chocolates, cocoa candies, and caffeine, which can lead to higher severity of the symptoms and lower effectiveness of the intervention.
With respect to the placebo effect, it should be noted that in the studies carried out on the PMS, the placebo effect on the syndrome is considerable.10 Response to placebo was different, ranging from 0.3 to 0.4, and it seems that paying attention to the women under study can bring about a positive psychological effect on treatment of the PMS.6 In the study carried out by De souza, placebo led to a significant decrease in all the PMS symptoms, varied from 16% for depression symptoms to 31% for depression symptoms.
Conclusion
Considering the results, the combination of Mg and vitamin B6 is an effective and affordable treatment in PMS. With regard to the periodic and chronic nature of the syndrome, administration of the drug seems to be feasible.
The authors declare no conflict of interest in this study.
Acknowledgments
The study was funded by the Research Chancellor of Isfahan University of Medical Sciences.
References
- 1.Rim Shin K, Young Ha j, Jung Park H, Heitkemper M. The Effect of Hand Acupuncture Therapy and Hand Moxibustion Therapy on Premenstrual Syndrome Among Korean Women. Western Journal of Nursing Research. 2009;31(2):171–86. doi: 10.1177/0193945908323650. [DOI] [PubMed] [Google Scholar]
- 2.Khajehei M, Abdali K, Parsanezhad ME, Tabatabaee HR. Effect of treatment with dydrogesterone or calcium plus vitamin D on the severity of premenstrual syndrome. International Journal of Gynecology & Obstetrics. 2009;105(2):158–61. doi: 10.1016/j.ijgo.2009.01.016. [DOI] [PubMed] [Google Scholar]
- 3.Gharekhni P, Sadatian SA. 4th ed. Tehran: Noor Danesh; 2005. Women's Diseases. [Google Scholar]
- 4.Jurgens T, Whelan AM. Advising patients on the use of natural health products to treat premenstrual syndrome. Canadian Pharmacists Journal. 2009;142(5):228–33. [Google Scholar]
- 5.De Souza MC, Walker AF, Robinson PA, Bolland K. A synergistic effect of a daily supplement for 1 month of 200 mg magnesium plus 50 mg vitamin B6 for the relief of anxiety-related premenstrual symptoms: a randomized, double-blind, crossover study. J Womens Health Gend Based Med. 2000;9(2):131–9. doi: 10.1089/152460900318623. [DOI] [PubMed] [Google Scholar]
- 6.Salamat S, Ismail KMK, O’ Brien S. Premenstrual syndrome. Obstetrics, Gynaecology and Reproductive Medicine. 2008;18(2):29–52. [Google Scholar]
- 7.Walker AF, De Souza MC, Vickers MF, Abeyasekera S, Collins ML, Trinca LA. Magnesium supplementation alleviates premenstrual symptoms of fluid retention. J Womens Health. 1998;7(9):1157–65. doi: 10.1089/jwh.1998.7.1157. [DOI] [PubMed] [Google Scholar]
- 8.Facchinetti F, Borella P, Sances G, Fioroni L, Nappi RE, Genazzani AR. Oral magnesium successfully relieves premenstrual mood changes. Obstet Gynecol. 1991;78(2):177–81. [PubMed] [Google Scholar]
- 9.Quaranta S, Buscaglia MA, Meroni MG, Colombo E, Cella S. Pilot study of the efficacy and safety of a modified-release magnesium 250 mg tablet (Sincromag) for the treatment of premenstrual syndrome. Clin Drug Investig. 2007;27(1):51–8. doi: 10.2165/00044011-200727010-00004. [DOI] [PubMed] [Google Scholar]
- 10.London RS, Bradley L, Chiamori NY. Effect of a nutritional supplement on premenstrual symptomatology in women with premenstrual syndrome: a double-blind longitudinal study. Journal of the American College of Nutrition. 1991;10(5):494–9. doi: 10.1080/07315724.1991.10718176. [DOI] [PubMed] [Google Scholar]


