Abstract
BACKGROUND:
Coronary artery diseases are one of the causes of early death all over the world. In developed countries, ischemic heart disease is responsible for half of the entire mortalities; however in developing countries it is estimated that from 9 million deaths per year, 32 percent are due to coronary artery disease. Acute coronary syndromes are responsible for over 250,000 deaths per year caused by progressive atherosclerotic process which would lead to rupture of the atherosclerotic plaque and establishing thrombosis. This study aimed to determine time intervals between the onset of the heart attack symptoms to thrombolytic therapy in patients with ST segment elevation myocardial infarction (STEMI) in selected hospitals of Isfahan University of Medical Sciences.
METHODS:
In this study, 180 subjects with first time STEMI were enrolled by categorized random sampling in cardiac care units of four hospitals affiliated to Isfahan University of Medical Sciences during 9 months. Necessary information were collected by asking the patients and reviewing their records. The data included demographic, prehospital and in-hospital data of the patients.
RESULTS:
The mean duration of time interval from the onset of heart attack symptoms to the first action in order to seek medical care was 01:16’(01:36’) (h:m [SD]), from the symptoms onset to admission in emergency unit was 02:29’(02:00’) and from admission in emergency unit to administration of thrombolytic drug was 01:04’(01:14’).
CONCLUSIONS:
Time interval between onset of the acute coronary symptoms and seek for medical care and arrival to the emergency unit in this study had a better condition than other studies, but the interval between the emergency admission and thrombolytic therapy was longer than other studies.
Keywords: Acute coronary syndrome, acute myocardial infarction, thrombolytic therapy
Currently, non communicable diseases are one of the major causes of mortality in developed and developing countries. The mortality caused from these diseases is decreasing by implementing intervention programs in some of the countries; while, it is growing in many other countries.1
Heart requires a balance between supply and demand in oxygen in order to function properly. The integrity of the coronary artery is an important factor in supplying oxygen of the heart muscle. Any disorder that leads to stenosis of each one of the coronary arteries may cause reduction in blood flow and oxygen reduction to any area in myocardium (by which vessel it is supplied) and cause acute coronary syndromes, acute myocardial infarction or even sudden cardiac death.
Every 19 seconds in the United States, a person suffers from a coronary event and almost every one minute, one person passes away due to coronary event. Every year, 1.1 million people in the U.S. suffer from acute myocardial infarction and 529000 people also die due to it.
Annually, around 250000 people die before getting to the hospital. Studies have shown that half of the acute myocardial infarction victims had waited more than two hours to be helped. Furthermore, the study showed that 45 percent of the patients were under 65 years and 5 percent of them were under 40 years old; and 85 percent of the people who died were above 65 years and older. In-hospital mortality is more in women than in men; studies have shown that this was due to differences in receiving the treatment.2
In Iran also, cardiovascular diseases have been the cause of 46% of the mortalities and its incidence is increasing.3 Moreover, 40 percent of the patients with acute myocardial infarction die before getting into the hospital. Most of these deaths occurred at the first two hours after the infarction.4
The patients with acute myocardial infarction symptoms should be treated immediately. Any increase in the time before beginning the treatment may increase the heart damage and decrease the survival ratio. The aim of “door to needle time” treatment in acute myocardial infarction is to conduct begin medication in less than 30 minutes or specifically from pain onset to thrombolytic therapy in 30 seconds or coronary angioplasty within one hour. Many people neglect to ask for help due to wrong interpretation of the signs and their different expectation of acute myocardial infarction and what they feel.2
Studies have shown that the shorter the interval time between onset of the symptoms to treat patients with ST segment elevation acute myocardial infarction (STEMI), the less the mortality rate proportionally. Due to restriction in reducing the symptom onset to door time, national organizations have mainly focused on reducing the door to reperfusion time. If the patients receive proper medical care at the beginning of infarction, the mortality cause by acute myocardial infarction would be reduced significantly.5 Studies have shown that every one minute delay in treating the patients with acute myocardial infarction is effective on mortality risk during the first year.6
Another study by McGinn et al indicated that 49.5% of the patients with acute myocardial infarction arrived to the hospital more than 4 hours after the onset of the symptoms. The following items associated with longer delays (more than 4 hours): older age, female gender, African American race, not using the emergency services, lack of chest pain at the first 72 hours in the hospital admission, no history of acute myocardial infarction or revascularization procedure and history of hypertension, diabetes or cerebral stroke. it is demonstrated that the possibility of receiving thrombolytic therapy, catheterization procedure or cutaneous coronary intervention is lower in patients with delay of more than 4 hours from the onset of the symptoms, while the probability of heart failure, shock or in-hospital death is higher (univariate analysis, p < 0.05).7
Another study by Fokuoka et al the interval time between admission in the hospital to start thrombolytic treatment or entering the catheterization lab were defined as door to needle time and door-to-catheter time. The results of this study showed that out of 155 patients, 23.9% (37 patients) received a single bolus dose of tissue plasminogen activator (TPA) in the emergency unit; and the rest of the patients, except one person, were transferred to catheterization lab for cutaneous coronary intervention. Median and mean of door to needle times were 19 and 26 minutes (SD = 21’), respectively. For the patients who have been transferred from emergency unit to the catheterization room, median and mean of door to catheterization room (door-to-catheter) were estimated around 60 and 80 minutes (SD = 62’), respectively. Besides, in this study, not calling the emergency ambulance, direct admission to the hospital and lack of sweating were the time predictors of door to catheterization room of more than 60 minutes.8
Currently, in emergency services system and in hospital level, the increase of ischemia times, complications and mortality have a significant statistics in patients with acute myocardial infarction and it is necessary to investigate the association of essential provided services characteristics in the emergency services system and also individual characteristics and records and clinical characteristics with these times and its impact on the complications and prognosis of the disease which in our society are considered as a basis for subsequent empirical researches. On the other hand, it should be noted that in the health care centers, nurses are at the front line of contacting with the patients and can have an important role in educating the warning signs of the acute coronary syndrome and appropriate measures at the time of exposure of the people with these signs to themselves or others, including self-care measures and calling the emergency services system to reduce the interval time of admission to the hospital and understand the importance of this incident. Furthermore, most of the emergency technicians in the urban ambulance service system are nursing expertise and therefore, their knowledge from factors affecting on pre-hospital time intervals and complications in patients with acute coronary syndrome can be effective on the quality of the performance and services. In-hospital coordination between a unit for admission and transferring the client is also done by the nursing managers. Furthermore, the emergency and cardiac care units (CCU) nurses implement the prescribed infusion of the clot-dissolving drugs (thrombolytics) and they are also responsible for management of the coronary angioplasty units; and therefore having knowledge about the factors affecting the complications of this situation and in-hospital emergency and medical measures can improve quality of the nursing managers performance and quality of providing health and medical services in the mentioned wards can be effective on reducing the complications and in-hospital mortality. The present study aimed to determine time intervals from onset of the symptoms to thrombolytic therapy in patients with ST segment elevation acute myocardial infarction in the selected hospitals affiliated to Isfahan University of Medical Sciences and the specific objectives including the mean time intervals between onset of the acute coronary syndrome to the initial attempt to receive the help, admission in the emergency unit and receiving thrombolytic therapy.
Methods
This was a single step, one-group descriptive study. The study population included all the admitted men and women in CCUs of the four selected hospitals affiliated to Isfahan University of Medical Sciences. The inclusion criteria were direct admission in the emergency unit, no history of mental disorders and memory impairment, medical diagnosis of acute myocardial infarction with ST segment elevation for the first time in their life and receiving in-hospital streptokinase. The exclusion criteria were lack of cooperation in response to the questionnaire questions during the study and not remembering onset time of the acute coronary syndrome symptoms. Participants were included by categorized random sampling method from men and women admitted in cardiac care units of the selected hospitals. In this method, first the admission size of the patients with acute coronary syndrome was estimated in the past six months in the studied hospital (the early six months in 2008), thereafter, according to it, the required percentage of samples in each class (each hospital) was determined; then each one of the persons referred to the hospital who had inclusion criteria was given a code and randomly, even codes were considered as the samples.
The required sample size was 80 people according to statistical formula and standard deviation with 95% confidence coefficient and 80% test power; so that 36.1% (65 samples) were allocated to Nour and Ali Asghar Hospital, 25% (45 samples) to Feiz Hospital, 22.2% (40 samples) to Alzahra Hospital and 16.7% (30 samples) to Shahid Chamran Hospital.
Data collection tool was a questionnaire which was completed through inquiry and reviewing study samples’ records and documentations. Validity of the data collection tool was done using content validity method. Thus, the researcher prepared a questionnaire by studying nursing and medical reference books and related published articles and in order for content quality, it was investigated by 10 faculty members of School of Nursing and Midwifery, four skilled and high experienced nursing staff in cardiac intensive care units and urban emergency services systems and one cardiologist and their corrective comments were applied in designing the questionnaire. In this study, to determine the reliability of the questionnaire, 10 people who were matched with the characteristics of the study samples were selected and the questionnaires were filled in using interviewing by them in two phases within two weeks. Thereafter, the obtained responses in these phases were investigated using test-retest and it was confirmed finally (r = 0.81). The participatants for determining the reliability of the questionnaire were excluded from the study. The researcher reviewed the inclusion criteria by the people who referred to the mentioned hospitals and had symptoms suggestive of acute coronary syndrome and the qualified individuals selected for completing the questionnaire after obtaining the consent form. In order to prevent the information bias, the questionnaire was completed after stability of the clinical condition of the patients. The obtained data included demographic characteristics of the patients and prehospital and in-hospital time intervals from onset of the symptoms to beginning the thrombolytic therapy. Analyzing the data, frequency distribution and mean of the studied variables was carried out using Software SPSS16.
Results
Mean age and standard deviation of the study samples were 59.5 (± 11.8) years. The frequency of the first time incidence of acute myocardial infarction until the sixth decade of the life gradually would increase and would reach to its highest level at the sixth decade of the life and then its frequency would be reduced after age of 60. The minimum frequency of the age was under 40 years old (4.4%) and the maximum frequency also was associated with age group 50-59 years (31.7%). The frequency of the first time incidence of acute myocardial infarction in men was more than in women and was tree times more (76.7% in men vs. 23.3% in women). Most of the study samples (96.7%) were married. The mean age of the first time incidence of acute myocardial infarction in women was 5.5 years more than men [63.5 (10.5) years in women vs. 58 (11.8) years in men]. The most frequency of the first time incidence of acute myocardial infarction in men was at the sixth decade of their life (27.8%) and in women was at seventh decade of their life (11.1%).
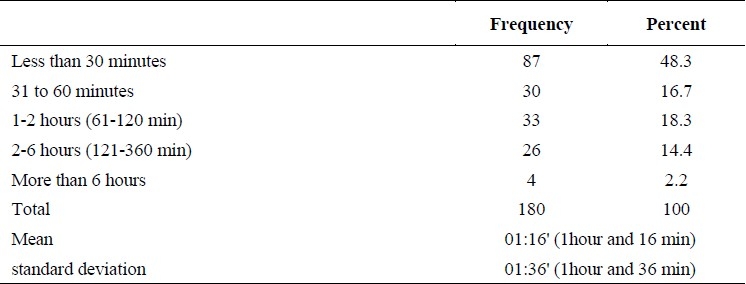
The mean time interval between onset of the first symptom to the first action for the help was 01:16’ (01:36’) (Table 1). Moreover, for most of the study samples (48.3%), it took less than 30 minutes to call for help or refer to the health care centers after onset of the symptoms.
Table 1.
Frequency distribution and mean time interval between onset of the myocardial infarction symptoms to the first action in receiving help
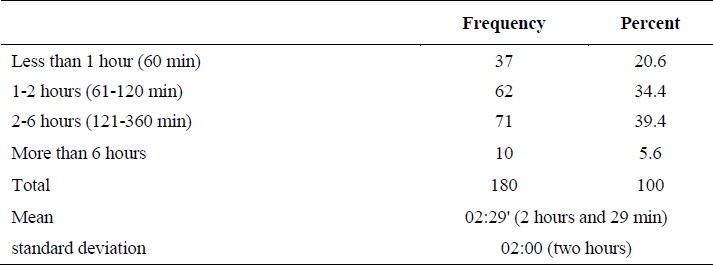
The mean time interval between onset of the symptom in heart attacks to admission time in emergency was 02:29’ (02:00’) (Table 2). In most of the study samples (39.4%), time interval between onset of the symptoms to admission into the emergency unit took 2 to 6 hours. Time intervals from 1 to 2 hours and less than 1 hour also placed at the subsequent intervals (respectively as 34.3% and 20.6%) and delay of more than 6 hours had the lowest frequency.
Table 2.
Frequency distribution and mean time interval between onset of the myocardial infarction symptoms to admission into the emergency unit
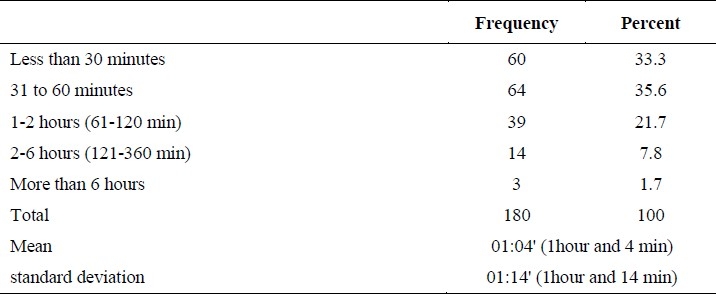
In this study, in 5.6% of the study subjects, the mean time interval between admission in the emergency unit to receive streptokinase took 01:4’ (01:14) (Table 3). And more than 60 percent of the study subjects received streptokinase in less than 1 hour from admission into the emergency unit.
Table 3.
Frequency distribution and mean time interval between admission into the emergency unit to receive streptokinase
Discussion
Lovlien et al, showed that more than half of the men and women of the study waited more than 1 hour before calling the emergency service and only 23% of the men and 28% of the women had a delay of less than half an hour.9 Furthermore, the study of Goldberg et al showed that mean time interval between onset of the myocardial infarction symptoms to seek the medical care in patients transferred by the ambulance was 3.9 hours and with other ways (vehicles or devices) was 4.7 hours.10 The results of the present study had a better results than other studies; however, it was far from the standard time.
In relation to time interval between onset of the myocardial infarction symptoms to admission into the emergency unit, the study of Lovlien et al showed that more than half of the men and women of the study had prehospital delay of over 2 hours. In this study, the most frequent delay interval in the male and female group were more than 6 hours (26% of the men) and between 2 to 6 hours (30% of the women), respectively. In addition, study results of McGinn et al7 showed that 49.5% of the patients referred to the hospital more than 4 hours after onset of the symptoms. The study of Soleiman and Mohammadi showed that 67% of the patients referred to the hospital at the first 6 hours and 23% of them at the second 6 hours after onset of the symptoms.11 The study results of Mohseni Kiasari also showed that 75% of the patients referred to the physician at the first 6 hours of acute myocardial infarction incidence.12
The present study showed a better result about time intervals between onset of the myocardial infarction symptoms to admission into the emergency unit than other studies. Home studies also investigated these time intervals in a wider time intervals; and considering newer time protocols for implementation of the emergency interventions related to acute myocardial infarction, more studies with more accurate time intervals seems necessary. Delay in searching for help and referring to the hospital depends on different factors for those who suffer from myocardial infarction for the first time. Different studies have shown that factors such as individual characteristics, underlying diseases, the first consulted person and how to transfer the patient to the hospitals are associated with these time intervals. In the present study, the researcher believed one of the major causes of delay was lack of awareness from the importance of the occurred clinical condition and referring to the clinic instead of referring to the emergency unit. In relation to the time intervals between admission into the emergency until receiving streptokinase, the study results of Fokuoka et al, showed that time interval between admission into the hospital and start of thrombolytic therapy was 00:26’ (± 00:21’).8 In the study of Samadikhah et al13, mean time interval between admission into the hospital and receiving streptokinase was reported 123’.30” minutes (± 9.79). In addition, study results of McNemara et al5 showed that nearly half of the studied patients (47%) received fibrinolytic therapy at the standard time interval (less than 30 min) and 24.1% of them also recived it between 31 to 45 minutes and 28.8% in time interval more than 45 minutes. The study results of the present study and Samadikhah showed a longer time to receive thrombolytic therapy in comparison with Fokuoka and McNemara; however, in the present study, 33.3% of the patients, received thrombolytic drug less than 30 minutes. Time interval between admission into the hospital and receiving thrombolytic drug depends upon different factors like prehospital time intervals. Demographic situation, the way of transferring to the hospital, clinical records and admission time to the hospital are some of the variables associated with time intervals. In the study of Fokuoka, lack of transferring with ambulance, direct admission to the hospital and sweating in the mentioned symptoms are reported as the predictors of delay in receiving thrombolytic therapy.
In addition to the above mentioned factors, delays in the process of admission and triage of the patients, delay in diagnosis of acute myocardial infarction, lack of drug stock of streptokinase in the emergency unit, crowded emergency and shortage of manpower are the other effective factors of the time intervals. Drug stock containing streptokinase and creating a specific environment to treat clot-dissolving (thrombolytics) treatment in emergency can reduce these time intervals.
The authors declare no conflict of interest in this study.
References
- 1.Zakeri-Mogaddan M, Ali-Asgarpour M. Tehran: Andishe Rafi; 2008. Critical care nursing. [In Persian] [Google Scholar]
- 2.Black JM, Hawks JH. 7th ed. Philadelphia: Elsevier Saunders; 2005. Medical-surgical nursing: clinical management for positive outcomes. [Google Scholar]
- 3.Isfahan Healthy Heart Program. [cited 2008 Sep 9]. Available from: http://ihhp.mui.ac.ir/
- 4.Newberry L, Sheehy SB. 5th ed. St. Louis: Mosby; 2003. Sheehy's emergency nursing: principles and practice. [Google Scholar]
- 5.McNamara RL, Herrin J, Bradley EH, Portnay EL, Curtis JP, Wang Y, et al. Hospital improvement in time to reperfusion in patients with acute myocardial infarction, 1999 to 2002. J Am Coll Cardiol. 2006;47(1):45–51. doi: 10.1016/j.jacc.2005.04.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.LeMone P, Burke KM. 4th ed. Upper Saddle River, NJ: Pearson/Prentice Hall; 2008. Medical-surgical nursing: critical thinking in client care. [Google Scholar]
- 7.McGinn AP, Rosamond WD, Goff DC, Jr, Taylor HA, Miles JS, Chambless L. Trends in prehospital delay time and use of emergency medical services for acute myocardial infarction: experience in 4 US communities from 1987-2000. Am Heart J. 2005;150(3):392–400. doi: 10.1016/j.ahj.2005.03.064. [DOI] [PubMed] [Google Scholar]
- 8.Fukuoka Y, Dracup K, Ohno M, Kobayashi F, Hirayama H. Predictors of in-hospital delay to reperfusion in patients with acute myocardial infarction in Japan. J Emerg Med. 2006;31(3):241–5. doi: 10.1016/j.jemermed.2005.12.019. [DOI] [PubMed] [Google Scholar]
- 9.Lovlien M, Schei B, Hole T. Prehospital delay, contributing aspects and responses to symptoms among Norwegian women and men with first time acute myocardial infarction. Eur J Cardiovasc Nurs. 2007;6(4):308–13. doi: 10.1016/j.ejcnurse.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 10.Goldberg RJ, Kramer DG, Yarzebski J, Lessard D, Gore JM. Prehospital transport of patients with acute myocardial infarction: a community-wide perspective. Heart Lung. 2008;37(4):266–74. doi: 10.1016/j.hrtlng.2007.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Soleiman HF, Mohammadi SM. Evaluation of early onset complications (Hospital phase) of AMI in CCU and Heart Unit of Imam Reza Hospital in Birjand. Journal of Birjand University of Medical Sciences. 1997;4(8-9):77–83. [In Persian] [Google Scholar]
- 12.Mohseni Kiasari A. Demographic characteristics of patients with acute myocardial infarction in Sari from 1991-96. Behbood. 2000;4(7):52–8. [In Persian] [Google Scholar]
- 13.Samadikhah J, Alizade M, Rezaeifar P, Ahadpour A, Ebrahim iB. Delays in Administration of Streptokinase in Patients with Acute Myocardial Infarction Hospitalized in Shahid Madani Hospital of Tabriz University of Medical Sciences. Medical Journal of Tabriz University of Medical Sciences & Health Services. 2007;29(3):71–5. [In Persian] [Google Scholar]


