Abstract
OBJECTIVE:
To evaluate the effectiveness of a school nurse–delivered smoking-cessation intervention in increasing abstinence among adolescent smokers.
METHODS:
Thirty-five high schools were pair-matched and randomly assigned to 1 of 2 conditions, each of which consisted of 4 visits with the school nurse: (1) counseling intervention using the 5 A's model and cognitive-behavioral techniques; or (2) an information-attention control condition. Adolescents (n = 1068) who reported past 30-day smoking and interest in quitting completed surveys at baseline and at 3 and 12 months and provided saliva samples for biochemical validation of reported smoking abstinence.
RESULTS:
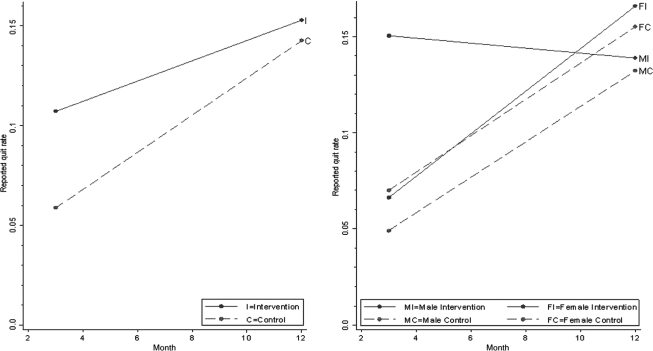
Intervention condition participants were almost twice as likely to be abstinent per self-report at 3 months (odds ratio: 1.90 [95% confidence interval: 1.12–3.24]; P = .017) compared with control participants; at 12 months there were no differences. The difference at 3 months was driven by quit rates in male students (15.0% [intervention] vs 4.9% [control]; odds ratio: 3.23 [95% confidence interval: 1.63–6.43]; P = .001); there was no intervention effect in female students at either time point (6.6% vs 7.0% at 3 months and 16.6% vs 15.5% at 12 months) and no intervention effect in male students at 12 months (13.9% vs 13.2%). Smoking amount and frequency decreased significantly in intervention compared with control schools at 3 but not at 12 months.
CONCLUSIONS:
A school nurse–delivered smoking-cessation intervention proved feasible and effective in improving short-term abstinence among adolescent boys and short-term reductions in smoking amount and frequency in both genders. Additional research is needed to enhance both cessation and maintained abstinence.
Keywords: adolescents, smoking cessation, intervention, school nurse
WHAT'S KNOWN ON THIS SUBJECT:
Most adolescent smokers want to quit and make serious attempts to quit. However, few seek medical assistance, and most are unsuccessful in their efforts to stop. Therefore, accessible, effective treatment approaches are needed for adolescents who want to quit smoking.
WHAT THIS STUDY ADDS:
Results demonstrate that a brief smoking-cessation intervention delivered by school nurses in the school health setting is feasible and moderately effective in helping adolescents to stop smoking.
Most adolescent smokers want to quit and have made a serious attempt in the past year (67% of girls and 56% of boys), but most adolescent quit attempts are unassisted and unsuccessful.1–4 Of those who have ever tried to quit, success is rare (11.5% for girls; 13.0% for boys).1,5 A meta-analysis of 64 teen tobacco-cessation programs showed an absolute increase in smoking-cessation rates of only 4.3%.6 Therefore, effective and accessible treatment approaches are needed. School nurses are uniquely positioned to deliver such treatment because they have the skills and credibility to offer health-related assistance,7 can provide ongoing support within the school setting, and are easily accessed by students without parental involvement, transportation, or cost given that more than 95% of adolescents attend school.8 Although there is great variability across school districts and states regarding the number of school nurses and the number of schools to which 1 school nurse is assigned, according to the National Association of School Nurses, about half (49%) of high schools across the country have at least 1 full-time registered nurse and another third have a part-time nurse.9 Also, although most states do not have a law that mandates a full-time school nurse for every school building, as is the position of National Association of School Nurses, many states do mandate the provision of nursing services related to administration of medication, health assessments, and special medical procedures.10
In a meta-analysis of 48 adolescent smoking-cessation trials, at a minimum of 3 months' follow-up, cessation rates were 9.1% for intervention conditions versus 6.2% for controls.11 Characteristics of successful programs included cognitive-behavioral strategies (goal setting, self-monitoring, development of coping and problem solving skills, and self-efficacy), motivation enhancement, and social influence content; delivery within the school setting (classroom and school clinic); and duration of at least 5 sessions. Another review also concluded that most effective programs were based on cognitive-behavioral principles.4,12 Clinical practice guidelines recommend a cognitive behavioral counseling approach adapting the adult “5 A's” model for adolescents: ask about tobacco use; advise users to quit; assess willingness to make a quit attempt; assist in their cessation attempt; and arrange follow-up to support their efforts.13 This approach, also endorsed by the American Academy of Pediatrics,14 was used in our study. We present here the results of a randomized controlled trial in which we evaluated the effectiveness of a school nurse–delivered smoking-cessation counseling intervention for adolescent smokers.
METHODS
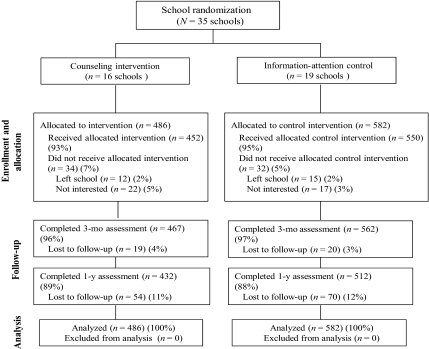
From 2006 to 2009, a pair-matched cluster-randomized controlled school-based trial was conducted with schools as the unit of randomization and students as the unit of analysis. All 290 public high schools in Massachusetts with an enrollment of at least 350 students (n = 290) were invited to participate. Thirty-five schools were recruited, pair-matched on demographics (percentage white, black, and Hispanic), school size, and percentage of students that are low-income, and were randomly assigned to either the counseling intervention (16 schools, n = 486 subjects) or attention control condition (19 schools, n = 582 subjects). Randomization was conducted after completion of baseline data collection in each school. A random number was generated using Excel for each matched pair of schools. Students were recruited through school announcements; posters; school nurse contacts; referrals from faculty, staff, and administrators; and word of mouth. Students were eligible to participate if they were enrolled in grades 9 to 12, had smoked within the past 30 days, and reported interest in quitting in the next 2 weeks. Passive consent letters were sent to parents, and students provided verbal assent as approved by the University of Massachusetts Medical School institutional review board. Recruitment continued until ∼30 students per school were enrolled (range: 17–42). In Fig 1 we show the study flow diagram.
FIGURE 1.
Consort diagram: participant flow through the study.
Assessments
Participants completed a confidential self-administered questionnaire at baseline and 3 and 12 months after enrollment to assess smoking status and potential modifying or mediating variables. Participants provided a saliva sample before survey completion; for participants who reported abstinence in the past 3 days, saliva samples were sent to the laboratory for cotinine analysis.15 Questions were taken from the Youth Risk Behavior Survey16 and National Longitudinal Study of Adolescent Health Survey17 and included age, gender, and race; frequency and amount of smoking in the past 30 days and the past 7 days; daily smoking; awareness of smoking-related health risks; age of smoking initiation; previous quit attempts; self-confidence to quit; perceived encouragement to quit from family, friends, school nurse, and doctor; parental permissiveness toward smoking; expectations of social and health effects of quitting; family and friends' smoking; academic performance; and quitting strategies used including nicotine replacement therapies and cessation medications. The following validated or established scales for adolescents were included: the Modified Fagerström Tolerance Questionnaire18 and the Hooked on Nicotine Checklist;19 the Children's Depression Inventory;20 the Perceived Stress Scale (4 items);21 Self Control Behavioral Capability;22 Multidimensional Anxiety Scale for Children-10;23 and Prochaska's Stages of Change.24 Process evaluation was used to document the number of sessions attended by students (dose) and adherence to treatment protocol by school nurse.
Counseling Intervention
The school nurse–delivered counseling intervention, Calling It Quits (Table 1), consisted of 4 weekly private 1-on-1 sessions conducted during 1 month in the school health clinic. Sessions were conducted during the school day and scheduled not to interfere with core academic classes. Two 30-minute sessions were conducted before the quit date, and 2 15-minute sessions after the quit date. The intervention was based on the 5 A's model adapted to be developmentally appropriate for adolescents through a workgroup with school nurses and representatives from the Massachusetts Department of Public Health School Nurse Unit and Tobacco Control Program, and the Department of Education. The intervention used a cognitive-behavioral approach based on social cognitive theory25,26 to develop health knowledge and positive outcome expectations and to build the adolescent's self-control and behavioral capacity skills (eg, goal-setting, self-monitoring, problem-solving) and self-efficacy to stop smoking. A patient-centered counseling approach was used in which school nurses asked open-ended questions to elicit the adolescent's thoughts and ideas, engage them actively in the discussion, and allow them to determine the course of action to take, tailoring the intervention to their individual needs. School nurses in the counseling intervention schools received a 1-day training, which included demonstration and practice delivering the intervention protocol in pairs.
TABLE 1.
Calling It Quits Counseling Intervention Protocol
| Visit | 5A Step | Intervention |
|---|---|---|
| 1 | Ask | Ask the adolescent about his or her smoking status (accomplished when eligibility for the study was conducted by the research assistant). |
| 1 | Advise | Advise the student to stop smoking with a statement that quitting smoking is the single best thing he or she can do for his or her health. |
| 1 | Assess | Assess motivation to stop smoking by asking if the adolescent is willing to make a quit attempt at this time (ie, stage of change). |
| 1 | Assist | Assist the adolescent to quit by addressing the following topics: (1) pros/cons of smoking; (2) personal reasons for quitting; (3) anticipated problems in quitting; (4) previous quit attempts; (5) nicotine addiction; (6) quit methods; (7) setting a quit date; and (8) triggers and strategies. |
| 2 | Assist | Assist the adolescent to quit by addressing the following topics: (1) managing triggers; (2) handling social situations; (3) withdrawal symptoms and their management; (4) 4 Ds for managing cravings (delay, deep breathing, drink water, do something else); (5) managing stress; (6) minimizing weight gain; (7) gaining support; (8) taking control of one's environment; and (9) rewarding oneself. |
| 3 and 4 | Assist | If the adolescent quit and maintained abstinence: (1) congratulate success; (2) review difficult situations and how they were handled; (3) assess benefits realized from quitting; and (4) discuss problems anticipated in maintaining abstinence and strategies to address them. If the adolescent has quit but relapsed: (1) congratulate attempt; (2) assess length of quit and what went well; (3) discuss what led to relapse and how the adolescent will handle when quitting again; (4) elicit recommitment to quit and set a new quit date; and (5) develop a new, modified plan. If the adolescent did not make a quit attempt: (1) assess barriers to making an attempt; (2) acknowledge difficulty of quitting; (3) elicit recommitment to quit and set new quit date; and (4) develop a new, modified plan. |
| 2–4 | Arrange | Arrange for follow-up. At each of the 3 follow-up visits the nurse reassessed current smoking status, stage of change, and any changes that occurred since the last contact (eg, stopped smoking, cut down on number of cigarettes smoked) then delivered the next session tailored to the adolescent's current smoking status. For example, if the adolescent quit, then the provider delivered a relapse prevention intervention consistent with the Public Health Service guideline tailored to adolescents. |
Information-Attention Control Condition
Students in the control condition also received 4 weekly visits with the school nurse during which the nurse delivered informational pamphlets, checked smoking status and efforts at quitting, and asked if the student had any questions. The informational pamphlets were selected from Journeyworks, which produces educational materials, on the basis of the appropriateness of their content, and their clear and attractive layout designed for a low-literacy audience and ease of reading. One pamphlet was used for each visit, covering health consequences of smoking, reasons to quit, a teen's guide to quitting, and social smoking. Sessions were conducted during the school day and scheduled to not interfere with core academic classes. The nurses in the control condition were trained 1-on-1 by the study program manager.
Analyses
All analyses were conducted by using Stata 10.1 (Stata Corp, College Station, TX).27 Baseline characteristics were compared by using t tests, Wilcoxon rank-sum tests, or Fisher's exact tests as appropriate.
The primary outcome was the proportion of students who reported not smoking in the past 30 days assessed at 3 and 12 months after baseline. In secondary analyses we used cotinine-validated abstinence (cutoff of 11.4 ng/millisecond)28,29 and a cotinine-imputed abstinence that incorporated imputation of abstinence when cotinine was missing. Cotinine was available on a sample of 68 students (82%) at 3 months and 55 students (40%) at 12 months. Imputed values were based on a prediction model of cotinine-validated abstinence using gender, grade in school, smoking every day, parents permitting smoking at home, Multidimensional Anxiety Scale for Children and Hooked on Nicotine Checklist scores, time, and randomized group. Unadjusted quit rates are compared using Fisher's exact test. Quit rates and maintenance rates were modeled using generalized estimating equation (GEE) logistic regression to account for clustering according to school and provide population-averaged estimates of rates. All analyses were based on intent-to-treat. Estimates according to gender are based on a model that includes an interaction of gender and randomized group. Characteristics that differed between randomized groups at baseline and were associated with the outcome were used in the adjusted models.
Secondary outcomes were modeled by using GEE logistic regression models for dichotomous outcomes (outcome expectations, adjuncts to quit, helpfulness of nurse, helpfulness of written materials, pharmacotherapy, and nicotine use) and a linear mixed-effects model for estimating mean differences in continuous outcomes (change in cigarettes smoked, days smoked, knowledge, self-efficacy, time with nurse). Number of quit attempts was modeled using 0-inflated negative binomial models with a robust variance estimate, and longest number of days without smoking was modeled by using a GEE negative binomial model. Comfort level with the nurse was modeled by using mixed-effects logistic regression with student nested within school as random effects. Associations of randomized group and gender with number of nurse visits were tested by using GEE logistic regression.
RESULTS
Baseline Participant Characteristics
Participants were 1068 adolescents (46.7% female, 92.6% white, 10.3% Hispanic) with a mean age of 16.8 years (Table 2). Participants smoked on average 6.7 cigarettes per day; 61.8% were daily smokers. The sample was moderately nicotine dependent (Modified Fagerström Tolerance Questionnaire mean: 4.26 [SD: 1.70]). The 2 groups were similar in sociodemographic and smoking characteristics. Approximately 66% of intervention group students planned to quit within the next 12 months compared with 57% of control students. The intervention group had slightly higher depression and anxiety scores.
TABLE 2.
Characteristics of Student Participants at Baseline
| Intervention (n = 486) | Control (n = 582) | P | |
|---|---|---|---|
| Mean (SD) age, y | 16.8 (1.2) | 16.9 (1.1) | .10 |
| Female, % | 51.2 | 44.7 | .04 |
| White, % | 94.4 | 91.1 | .045 |
| Black, % | 4.1 | 4.8 | .6 |
| Hispanic, % | 8.0 | 12.2 | .03 |
| School performance average or better, % | 80.3 | 82.3 | .4 |
| Smoked every day in last 30 d, % | 58.4 | 64.6 | .04 |
| Mean (SD) No. of days smoked past 30 d | 26.7 (5.7) | 26.8 (6.1) | .13a |
| Mean (SD) No. of days smoked past 7 d | 6.3 (1.2) | 6.4 (1.3) | .009a |
| Mean (SD) No. of cigarettes per d smoked past 7 d | 6.6 (4.7) | 6.8 (5.1) | .4a |
| Mean (SD) No. of cigarettes smoked in past 7 d | 45.9 (33.1) | 47.9 (35.3) | .4a |
| Mean (SD) age first smoked whole cigarette | 12.7 (2.1) | 12.7 (2.2) | .7 |
| Mean (SD) HONC nicotine addiction score (range: 0–10) | 7.8 (2.2) (1 to 10) | 7.6 (2.2) (0 to 10) | .06a |
| Mean (SD) modified FTQ nicotine addiction score (range: 0–9) | 4.2 (1.7) (1 to 9) | 4.3 (1.7) (0 to 9) | .3 |
| Tried to quit in past 12 mo, % | 65.2 | 63.9 | .7 |
| Mean (SD) No. of times tried to quit | 1.9 (2.9) | 1.8 (2.3) | .9a |
| Mean (SD) time quit | 15.9 (32.0) | 16.8 (35.0) | .9a |
| Used the following to try to quit in past 12 mo, % | |||
| Nicotine-replacement therapies (gum, spray, patch, tablets) | 11.1 | 11.5 | .8 |
| Prescription medications (Wellbutrin/Zyban/bupropion) | 1.0 | 1.4 | .8 |
| Stop smoking program at school or community | 2.3 | 2.1 | .8 |
| Called a help line or quit line | 0.0 | 0.3 | .5 |
| None of above | 86.4 | 85.4 | .7 |
| Confident could quit if wanted to, % | .008b | ||
| Definitely yes | 19.3 | 14.6 | |
| Probably yes | 63.4 | 62.7 | |
| Probably not | 16.1 | 22.3 | |
| Definitely not | 1.2 | 0.3 | |
| With lots of encouragement to quit from, % | |||
| Family | 63.5 | 63.6 | .999 |
| Friends | 24.3 | 20.5 | .14 |
| School nurse | 76.1 | 67.8 | .003 |
| Doctor or other provider | 69.1 | 67.3 | .6 |
| Plan to quit, % | .006 | ||
| In the process of quitting | 21.9 | 24.9 | |
| Next 30 d | 33.8 | 29.7 | |
| Next 1–6 mo | 24.5 | 18.0 | |
| Next 6–12 mo | 7.6 | 9.6 | |
| No plans to quit | 12.2 | 17.7 | |
| With household members who smoke, % | 72.2 | 64.1 | .006 |
| With half or more friends who smoke, % | 79.6 | 79.6 | .999 |
| Able to smoke at home, % | 33.3 | 29.1 | .14 |
| Easy or very easy to get at home, % | |||
| Positive outcome expectations if quit, % definitely to probably yes | |||
| Breathe easier when I run | 80.4 | 81.3 | .8 |
| Have more money to spend on things I want | 81.9 | 82.0 | .999 |
| Others will respect me more | 46.0 | 43.1 | .4 |
| My breath, clothes, and hair will smell better | 85.0 | 83.1 | .4 |
| Negative outcome expectations if quit, % definitely to probably yes | |||
| Bad mood for a few days | 71.4 | 70.5 | .7 |
| Gain weight | 43.0 | 38.3 | .13 |
| Other kids will think I am less cool | 5.6 | 9.5 | .02 |
| Will have to work hard to keep from smoking | 81.1 | 81.4 | .9 |
| I will lose a way to handle stress | 59.7 | 62.5 | .35 |
| I will have more difficulty concentrating | 48.2 | 46.9 | .71 |
| Knowledge/beliefs, % very to somewhat true | |||
| People get addicted to cigarette smoking just like they can get addicted to a drug | 94.2 | 93.8 | .8 |
| Smokers die at a younger age than nonsmokers | 87.7 | 85.7 | .4 |
| 1 of 3 people who start smoking by age 18 will die because of their smoking | 58.2 | 61.5 | .3 |
| Smokers generally have less stress than nonsmokers and former smokers | 40.0 | 44.0 | .2 |
| Smoking decreases physical fitness | 85.2 | 84.7 | .9 |
| Mean (SD) depression score (range: 6–4) | 16.4 (4.0) (6–24) | 15.5 (4.1) (6–24) | .001 |
| Mean (SD) depressive symptoms score (range: 16–34) | 26.4 (4.0) (16–34) | 25.5 (4.1) (16–34) | .001 |
| Mean (SD) self-control scores (range: 12–53) | 31.6 (7.1) (12–53) | 32.4 (6.7) (13–53) | .06 |
| Mean (SD) stress scores (range: 2–18) | 9.3 (3.0) (2–18) | 8.9 (3.0) (2–18) | .06 |
| Mean (SD) anxiety scores (range: 0–30) | 10.4 (5.6) (0–30) | 9.7 (5.5) (0–29) | .04 |
Categorical variables were compared by using the χ2 test, and continuous variables were compared by using the t test unless otherwise noted. HONC indicates Hooked on Nicotine Checklist; FTQ, Fagerstrom Tolerance Questionnaire.
Wilcoxon rank-sum test.
Fisher's exact test.
3- and 12-Month Abstinence Rates
In unadjusted analyses, at 3 months, 10.7% of students reported abstinence in the intervention group compared with 5.9% in the control group (P = .006); male students accounted for the difference (Fig 2; Table 3). At 3 months, the intervention increased the odds of quitting (odds ratio [OR]: 1.90 [95% confidence interval (CI): 1.12–3.24]) with the effect limited to boys. This gender effect remained after adjusting for baseline differences in depression and anxiety. There were no significant differences in self-reported quit rates between conditions at 12 months. In analyses of cotinine-confirmed abstinence with and without imputation for missing cotinine values, quit rates were lower but the conclusions were the same: an intervention effect was evident only for male students at 3 months.
FIGURE 2.
Unadjusted self-reported quit rates in intervention and control schools for all students and according to gender at the 3- and 12-month follow-ups.
TABLE 3.
Quit Rates and Adjusted Odds Ratios in Intervention Compared With Control Schools Among All Students and According to Gender
| 3 mo |
12 mo |
|||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted % Quit | Model 1, Adjusted OR (95% CI)a | Model 2, Adjusted OR (95% CI)b | Pb | Unadjusted % Quit | Model 1, Adjusted OR (95% CI)a | Model 2, Adjusted OR (95% CI)b | Pb | |
| Self-reported quitting among all students | — | 2.01 (1.16–3.49) | 1.90 (1.12–3.24) | .017 | — | 1.09 (0.80–1.50) | 1.00 (0.69–1.44) | .99 |
| Control | 5.9 | — | — | — | 14.3 | — | — | — |
| Intervention | 10.7 | — | — | — | 15.3 | — | — | — |
| Self-reported quitting among girls | — | 0.99 (0.47–2.11) | 0.94 (0.44–2.01) | .9 | — | 1.10 (0.69–1.77) | 1.08 (0.64–1.80) | .8 |
| Control | 7.0 | — | — | — | 15.5 | — | — | — |
| Intervention | 6.6 | — | — | — | 16.6 | — | — | — |
| Self-reported quitting among boys | — | 3.52 (1.76–7.04) | 3.23 (1.63–6.43) | .001 | — | 1.06 (0.65–1.72) | 0.92 (0.54–1.57) | .8 |
| Control | 4.9 | — | — | — | 13.2 | — | — | — |
| Intervention | 15.0 | — | — | — | 13.9 | — | — | — |
| Male vs female relative difference | — | 3.54 (1.37–9.16) | 3.43 (1.30–9.06) | .01 | — | 0.96 (0.47–1.96) | 0.85 (0.41–1.80) | .7 |
| Cotinine-validated quitting among all students | — | 2.63 (1.36–5.10) | 2.56 (1.35–4.86) | .004 | — | 1.39 (0.69–2.77) | 1.20 (0.56–2.58) | .6 |
| Control | 3.2 | — | — | — | 3.9 | — | — | — |
| Intervention | 7.8 | — | — | — | 5.3 | — | — | — |
| Cotinine-validated quitting among girls | — | 1.30 (0.55–3.07) | 1.35 (0.56–3.25) | .5 | — | 1.41 (0.60–3.29) | 1.38 (0.57–3.37) | .5 |
| Control | 4.3 | — | — | — | 5.3 | — | — | — |
| Intervention | 5.5 | — | — | — | 7.4 | — | — | — |
| Cotinine-validated quitting among boys | — | 5.01 (2.01–12.47) | 4.65 (1.88–11.53) | .001 | — | 1.15 (0.35–3.78) | 0.89 (0.26–3.05) | .9 |
| Control | 2.3 | — | — | — | 2.7 | — | — | — |
| Intervention | 10.4 | — | — | — | 3.1 | — | — | — |
| Male vs female relative difference | — | 3.85 (1.16–12.85) | 3.44 (1.00–11.75) | .049 | — | 0.81 (0.20–3.28) | 0.65 (0.16–2.68) | .5 |
| Cotinine-imputed quitting among all students | — | 2.52 (1.32–4.84) | 2.30 (1.22–4.33) | .01 | — | 1.61 (0.95–2.73) | 1.44 (0.79–2.62) | .2 |
| Control | 4.1 | — | — | — | 6.8 | — | — | — |
| Intervention | 9.2 | — | — | — | 10.7 | — | — | — |
| Cotinine-imputed quitting among girls | — | 1.40 (0.61–3.21) | 1.33 (0.57–3.06) | .5 | — | 1.63 (0.87–3.04) | 1.60 (0.81–3.14) | .2 |
| Control | 5.1 | — | — | — | 9.5 | — | — | — |
| Intervention | 6.6 | — | — | — | 14.8 | — | — | — |
| Cotinine-imputed quitting among boys | — | 4.24 (1.83–9.85) | 3.71 (1.62–8.51) | .002 | 1.36 (0.57–3.29) | 1.14 (0.45–2.87) | .8 | |
| Control | 3.3 | — | — | — | 4.6 | — | — | — |
| Intervention | 12.0 | — | — | — | 6.2 | — | — | — |
| Male vs female relative difference | — | 3.03 (1.03–8.91) | 2.80 (0.95–8.28) | .06 | — | 0.84 (0.31–3.28) | 0.71 (0.26–1.98) | .5 |
Overall model was adjusted for school. The model according to gender is adjusted for school, gender, and the interaction of gender and the intervention.
Overall model was adjusted for baseline self-efficacy, stage of change, smoking every day, and school, and the model according to gender was adjusted for baseline self-efficacy, stage of change, and smoking every day, school, gender, and the interaction of gender and the intervention.
Population-averaged logistic regression models were used for all analyses.
Effect on Smoking Frequency
The intervention was associated with a reduction in the number of cigarettes smoked and the number of days smoked in the past 7 days at 3-month follow-up. This was true whether the analyses included all subjects or only those who remained smokers. No intervention effect on the number of cigarettes smoked or smoking days was seen at 12 months (Table 4).
TABLE 4.
Changes From Baseline in Mean Number of Cigarettes and Mean Number of Days Smoked in the Past 7 Days at 3 and 12 mo
| Unadjusted Mean Change from Baseline (SD) | Adjusted Mean Change Model 1a (95% CI) | Adjusted Mean Change Model 2b (95% CI) | Pb | Unadjusted Mean Change from Baseline (SD) | Adjusted Mean Change Model 1a (95% CI) | Adjusted Mean Change Model 2b (95% CI) | Pb | |
|---|---|---|---|---|---|---|---|---|
| Among all students | .003 | .1 | ||||||
| Control | −12.3 (30.6) | −11.8 (−14.8–−8.9) | −12.3 (−15.3–−9.3) | −4.3 (42.9) | −3.8 (−7.7–0.2) | −4.5 (−8.3–−0.7) | ||
| Intervention | −18.8 (33.7) | −19.2 (−22.4–−15.9) | −19.03 (−22.3–−15.8) | −9.3 (40.9) | −9.7 (−14.0–−5.4) | −8.8 (−13.0–−4.6) | ||
| Intervention effect | — | −7.37 (−11.8–−3.0) | −6.8 (−11.2–−2.3) | — | −5.9 (−11.8 to −0.1) | −4.3 (−10.0 to 1.4) | ||
| Among self-reported smokers | .01 | .08 | ||||||
| Control | −11.2 (30.1) | −10.3 (−13.2–−7.4) | −11.0 (−13.9–−8.1) | 1.7 (41.0) | 2.7 (−1.3–6.7) | 1.5 (−2.4–5.4) | ||
| Intervention | −17.0 (33.4) | −16.5 (−19.7–−13.2) | −16.4 (−19.6–−13.2) | −4.1 (39.8) | −4.0 (−8.4–0.3) | −3.6 (−7.9–0.6) | ||
| Intervention effect | — | −6.1 (−10.5–−1.8) | −5.4 (−9.8 to −1.1) | — | −6.7 (−12.7–−0.8) | −5.1 (−10.9–0.7) | ||
| Among all students | <.001 | .5 | ||||||
| Control | −0.73 (2.12) | −0.71 (−0.95–−0.46) | −0.72 (−0.95–−0.50) | −1.11 (2.72) | −1.10 (−1.34–−0.85) | −1.12 (−1.36–−0.88) | ||
| Intervention | −1.43 (2.43) | −1.46 (−1.72–−1.19) | −1.43 (−1.67–−1.18) | −1.25 (2.75) | −1.28 (−1.55–−1.01) | −1.26 (−1.52–−0.99) | ||
| Intervention effect | — | −0.75 (−1.11–−0.40) | −0.70 (−1.04–−0.36) | — | −0.18 (−0.55–0.18) | −0.13 (−0.49–0.23) | ||
| Among self-reported smokers | .001 | .2 | ||||||
| Control | −0.44 (1.77) | −0.40 (−0.59–−0.21) | −0.43 (−0.61–−0.24) | −0.32 (1.93) | −0.26 (−0.45–−0.07) | −0.31 (−0.49–−0.12) | ||
| Intervention | −0.94 (2.02) | −0.92 (−1.13–−0.71) | −0.90 (−1.11–−0.70) | −0.48 (2.06) | −0.48 (−0.68–−0.27) | −0.48 (−0.69–−0.28) | ||
| Intervention effect | — | −0.53 (−0.81–−0.24) | −0.48 (−0.75–−0.20) | — | −0.22 (−0.50 to 0.06) | −0.18 (−0.45 to 0.10) |
Adjusted for school and baseline number of cigarettes smoked in past 7 days.
Adjusted for gender; baseline stage of change, self-efficacy, support of friends, school; and baseline number of cigarettes smoked in past 7 days. Additional variables adjusted for mean number of cigarettes for smoked every day in past month, self-control score, perceived stress score, “Kids will think I'm less cool,” and for mean number of days for grade in school and living with a smoker.
Intervention Effect on Potential Mediators of Quitting
The intervention did not have any clear impact on students' expectations regarding the positive and negative outcomes they associated with quitting (Table 5). Knowledge scores showed no significant changes over time and between conditions (data not shown). Scores on confidence to quit improved more in the intervention group at 3 months (difference in adjusted mean change: 0.11 [95% CI: 0.02–0.21]; P = .02) but not at 12 months (0.08 [95% CI: −0.01–0.18]; P = .10). The number of quit attempts was significantly higher for the intervention group at 3 months (mean: 2.2 [SD: 2.2] vs 1.7 [SD: 2.1]; P = .003) but not at 12 months (2.1 [SD: 2.9] vs 2.1 [SD: 2.9]; P = .9). Of those who made a quit attempt, the length of time they were able to refrain from smoking was significantly longer among students in the intervention group at 3-month follow-up (20.8 days [SD: 23.0] vs 15.8 days [SD: 19.5]; P < .05) and at 12-month follow-up (58.4 days [SD: 76.9] vs 47.8 days [SD: 68.3]; P < .001). Additional analyses identified no gender differences in predictors of cessation outcomes.
TABLE 5.
Changes in Outcome Expectations for Quitting Smoking at 3 and 12 Months
| Baseline % | 3 Mo |
12 Mo |
|||
|---|---|---|---|---|---|
| % | OR (95% CI); P | % | OR (95% CI); P | ||
| Positive outcome expectations | |||||
| Will be able to breathe easier when I run | — | — | 0.67 (0.47–0.98); .037 | — | 0.81 (0.51–1.28); .366 |
| Control | 81.3 | 86.6 | — | 90.0 | — |
| Intervention | 80.5 | 83.0 | — | 87.3 | — |
| Have more money to spend on things I want | — | — | 0.90 (0.66–1.23); .522 | 0.86 (0.56–1.33); .500 | |
| Control | 82.0 | 83.6 | — | 89.2 | — |
| Intervention | 81.9 | 83.2 | — | 88.0 | — |
| Others will respect me more | — | — | 1.16 (0.92–1.48); .215 | — | 0.82 (0.62–1.09); .164 |
| Control | 43.1 | 49.0 | — | 54.0 | — |
| Intervention | 46.0 | 54.1 | — | 51.4 | — |
| My breath, clothes, and hair will smell better | — | — | 0.87 (0.64–1.17); .347 | 0.84 (0.56–1.26); .391 | |
| Control | 83.1 | 85.0 | — | 90.9 | — |
| Intervention | 85.0 | 84.9 | — | 89.9 | — |
| Negative outcome expectations | |||||
| Bad mood for a few days | — | — | 0.80 (0.59–1.07); .132 | — | 0.92 (0.65–1.29); .625 |
| Control | 70.5 | 70.2 | — | 72.8 | — |
| Intervention | 71.4 | 66.8 | — | 71.7 | — |
| Gain weight | — | — | 0.98 (0.73–1.31); .886 | — | 0.74 (0.56–0.98); .034 |
| Control | 38.3 | 39.0 | — | 42.9 | — |
| Intervention | 43.0 | 41.0 | — | 39.0 | — |
| Other kids will think I am less cool | — | — | 1.07 (0.68–1.69); .765 | — | 0.93 (0.61–1.40); .717 |
| Control | 9.5 | 9.3 | — | 9.1 | — |
| Intervention | 5.6 | 8.8 | — | 8.0 | — |
| I will lose a way to handle stress | — | — | 0.88 (0.65–1.18); .376 | — | 0.86 (0.64–1.14); .288 |
| Control | 62.5 | 64.7 | — | 60.0 | — |
| Intervention | 59.7 | 62.1 | — | 57.0 | — |
| Will have to work hard to keep from smoking | — | — | 0.62 (0.48–0.80); <.001 | — | 0.96 (0.72–1.30); .812 |
| Control | 81.4 | 82.1 | — | 78.0 | — |
| Intervention | 81.1 | 75.2 | — | 76.8 | — |
| I will have more difficulty concentrating | — | — | 0.86 (0.66–1.12); .275 | — | 1.04 (0.83–1.31); .724 |
| Control | 46.9 | 48.7 | — | 43.4 | — |
| Intervention | 48.2 | 47.2 | — | 44.1 | — |
All models were adjusted for gender, race, smoking every day, depression score, perceived stress score, self-control score, MASC score, school, and baseline outcome expectations.
Only 2% to 3% of students reported use of prescription medications while trying to quit smoking, and this did not differ according to condition at either time point. More students used nicotine replacement therapies, and this was somewhat higher in the control group at 3 months (12.6% vs 8.8%; P = .07) and at 12 months (19.0% vs 13.7%; P = .04). Use of pharmacologic adjuncts did not differ according to gender.
Treatment Fidelity and Acceptability
School nurses reported that >70% of students attended 4 or more visits with no differences according to gender or group. The time spent with the nurse was similar for female and male students within each group and was consistent with the expected time commitment (for the counseling intervention, ∼30 minutes for each of sessions 1 and 2 and 15 minutes for each of sessions 3 and 4; for the attention-control condition, ∼10 minutes each session).
Fidelity to the counseling intervention protocol was generally high. During the first visit, the majority of intervention steps were completed 95% or more of the time. During subsequent visits, the rates of completion were more variable, but still generally high for the majority of the intervention steps. School nurses were able to work the delivery of the intervention into their daily routine without added expense; therefore there were no costs associated with the nurses delivering the intervention.
The majority of students who received the counseling intervention reported the school nurse was very helpful in their efforts to quit, and this was higher in the intervention group (78% vs 60%, respectively, at 3 months [P < .001] and 72% vs 60%, respectively, at 12 months [P < .001]). The majority of students who received the counseling intervention also reported they were very comfortable in discussing their smoking with the nurse, and this was higher but not significantly different in the intervention compared with control conditions (70% vs 62% averaged over all visits; P = .05 unadjusted and .06 adjusted for gender). About half the students felt the written materials were very helpful in their efforts to quit smoking in both conditions and at each time point.
DISCUSSION
The findings of the present study indicate that a brief smoking-cessation counseling intervention on the basis of the 5 A's model using cognitive-behavioral strategies and delivered by school nurses within the school health setting can be effective in promoting short-term abstinence among adolescent smokers. The self-reported 30-day abstinence at 3 months (11% across both genders) was similar to the mean for adolescent cessation trials (9%),11 and was higher than the 6% reported for immediately post program in the well-known school-based Not on Tobacco program.30
This intervention effect was driven entirely by boys who were 3 times more likely to be abstinent at 3-month follow-up, which suggests the brief counseling provided by the school nurse was effective in assisting boys to achieve short-term abstinence, whereas nurse contact with information-sharing was not sufficient, producing a quit rate (5%) similar to the 6% quit rate for control groups in the meta-analysis.11 Although no intervention effect was found in boys at 12 months, abstinence rates in both conditions were relatively high (13%–14%).
In contrast, among girls the counseling intervention did not improve quit rates above that seen in the control group at either time point (6.6% vs 7.0% at 3 months and 16.6% vs 15.5% at 12 months). At 12-month follow-up, both conditions produced equally high abstinence rates in both boys and girls (13.9% and 16.6%, respectively, in the counseling condition; 13.2% and 15.5%, respectively, in the information control condition), exceeding the average abstinence rate for treatment programs in the recent meta-analysis (9%).11 One interpretation of these results is that girls needed less intensive intervention than boys to quit and that information with nurse contact alone was as effective as intensive 1-on-1 counseling in the long-term. However, we found no gender differences in predictors of cessation outcomes, including depression, anxiety, confidence in quitting, positive and negative expectations of quitting, and perceived helpfulness of the nurse. Also, the counseling intervention resulted in a reduction in number of cigarettes smoked and number of smoking days at 3 months without gender differences. The reason for the gender difference in quitting is unclear because gender differences are not typical in adolescent smoking-cessation studies.11 In addition, it seems the information plus nurse contact attention control intervention may have contributed to smoking cessation in both genders at 12-month follow-up. This may be because of the fact that this condition provided information on quitting that the smoker was able to apply in future quit attempts. Also, this condition provided a minimum level of contact with the nurse along with ongoing support from the school nurse for their efforts to quit, which may have been sufficient to motivate those interested in quitting to quit within the year. We know anecdotally from the nurses that adolescent participants in both conditions frequently checked in with the nurse regarding their smoking status, challenges, and success, which may have contributed to the effect of the information and nurse contact control condition. Unfortunately, we do not know if the high rates of abstinence achieved at 12-month follow-up in both conditions reflect a secular trend because we did not have a no-contact control. Therefore, although promising, these findings indicate the need to explore strengthening the counseling intervention to enhance its effect on abstinence and long-term maintenance and the need to include a no-contact control condition in the study design. A number of intervention effects on potential mediators of quitting were identified. First, adolescents' confidence in their ability to quit improved more from baseline to 3 months in intervention compared with control schools, although not at 12 months. It is possible that the initial success in quitting during and soon after the intervention boosted confidence, but with relapse back to smoking, their confidence eroded. Second, adolescents in the counseling condition had made more than twice as many quit attempts by 3 months compared with the controls and were able to refrain for a greater number of days at both 3 and 12 months. This suggests the counseling intervention stimulated more attempts to quit in the short-term and enhanced the ability to quit over a longer time-period during each attempt.
Consistent with many previous studies demonstrating dependence and failed cessation in nondaily smokers of all ages,31–33 we note that although 38.2% of our subjects were nondaily smokers, the overall abstinence rate at 3 months was only 11%. Our analysis of predictors of cessation outcomes is the subject of a separate report, but it is obvious that the majority of nondaily smokers failed to maintain abstinence. We conclude that nondaily smokers are in need of assistance in quitting.
Use of pharmacologic adjuncts for quitting was relatively low in this study, comparable with lifetime use of buproprion (7%) and nicotine gum (17%) and nicotine patch (16%) in surveys of youth who have attempted to quit.34 Nicotine replacement therapy use was somewhat higher in control compared with intervention schools at both time points. At 3 months, gum use was twice as high in control compared with intervention participants in both genders, so the higher quit rates seen in boys in the intervention condition at 3 months are not because of gum use. One possible reason for the greater use of nicotine replacement therapy in the control condition was that they received written materials on pharmacotherapy, whereas pharmacotherapy was mentioned only briefly in the counseling intervention. Also, adolescents in the control group may have felt they needed more assistance because they were not receiving structured counseling from the nurse. There were no gender differences in pharmacotherapy use.
Delivering smoking-cessation treatment to adolescents through school nurses is an ideal vehicle for a number of reasons. First, in the meta-analysis of adolescent smoking-cessation trials, delivery within the school setting was 1 of the characteristics of successful programs.11 Second, this approach leverages existing resources by capitalizing on the placement of skilled health care providers in the school setting. Because 95% of US adolescents attend school,8 schools and their nurses provide a uniquely practical venue for delivering smoking-cessation treatment. School nurses are easily accessed by students in confidence, at no cost, and without parental involvement. This venue obviates issues of transportation, cost, and confidentiality from parents that arise with pediatricians' offices and other venues, reducing barriers to adolescent smokers seeking and receiving treatment. In addition, there was no additional cost to the schools to deliver this intervention because school nurses incorporated delivery of the intervention into their daily schedule. As such, the field of adolescent smoking cessation should continue to explore the use of school nurses and school health services to provide treatment to adolescent smokers interested in quitting.
Study strengths include the large sample size and heterogeneous population in terms of duration of tobacco use and frequency and quantity of use. Additional strengths include the carefully designed intervention on the basis of current recommendations and tailored for adolescents; a rigorous, randomized controlled design with a condition controlling for contact with the school nurse and access to information on smoking and cessation; biochemical validation of self-reported abstinence; long-term follow-up; use of an intent-to-treat analysis; use of real-world providers to deliver the intervention; and strong retention rates of 96.4% at 3-month and 88.4% at 12-month follow-up. Limitations of the study include potential variability between school nurses in fidelity to delivering the intervention protocol given this was an effectiveness trial, that we did not address forms of tobacco use other than cigarette smoking, and the study was limited to 1 geographical area.
CONCLUSIONS
The results of this study demonstrate the feasibility and short-term effectiveness of a novel, school nurse–delivered smoking-cessation intervention for improving short-term abstinence among adolescent male smokers, and short-term reductions in smoking amount and frequency in both genders. Given that few adolescents will successfully quit smoking without intervention despite a strong interest in quitting, treatment approaches are needed that are accessible and can help those interested in quitting be successful in their cessation efforts. As the primary health care professional in the school setting, school nurses are in a unique position to deliver such smoking-cessation treatments given their training, skills, and accessibility to teens. Additional research is needed to enhance the effect of school nurses in helping teens quit and maintain abstinence. Such a smoking-cessation intervention delivered by school nurses in the school health setting would have tremendous potential to reach large numbers of adolescent smokers and have significant public health effect.
ACKNOWLEDGMENTS
This study was supported by National Cancer Institute, National Institutes of Health grant R01 CA114556 (awarded to Dr Pbert).
We thank Nancy O'Mealey and Dante Simone, who served as research coordinators for the study; Drs Jonathan Klein, Henry Feldman, and Martin Young for serving on the study's data and safety monitoring board; and the students who participated in this study. We dedicate this work to the school nurses for hard work and dedication and their daily commitment to the health of our children.
All authors participated in study conception and design, analysis and interpretation of data, and drafting and revising of the manuscript; and all authors approved the manuscript as submitted.
This trial has been registered at www.clinicaltrials.gov (identifier NCT00682474).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
Funded by the National Institutes of Health (NIH).
- GEE
- generalized estimating equation
- OR
- odds ratio
- CI
- confidence interval
REFERENCES
- 1. Centers for Disease Control and Prevention Cigarette use among high school students: United States, 1991–2009. MMWR Morb Mortal Wkly Rep. 2010;59(26):797–801 [PubMed] [Google Scholar]
- 2. Grimshaw G, Stanton A, Blackburn C, et al. Patterns of smoking, quit attempts and services for a cohort of 15- to 19-year-olds. Child Care Health Dev. 2003;29(6):457–464 [DOI] [PubMed] [Google Scholar]
- 3. Mermelstein R. Teen smoking cessation. Tob Control. 2003;12(suppl 1):i25–i34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sussman S. Effects of sixty-six adolescent tobacco use cessation trials and seventeen prospective studies of self-initiated quitting. Tob Induc Dis. 2002;1(1):35–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention High school students who tried to quit smoking cigarettes: United States, 2007. MMWR Morb Mortal Wkly Rep. 2009;58(16):428–431 [PubMed] [Google Scholar]
- 6. Sussman S, Sun P. Youth tobacco use cessation: 2008 update. Tob Induc Dis. 2009;5:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Broussard L. School nursing: not just band-aids anymore! J Spec Pediatr Nurs. 2004;9(3):77–83 [DOI] [PubMed] [Google Scholar]
- 8. US Department of Commerce Historical Statistics of United States Colonial Times to 1970; Current Population Reports, Series P-20, Various Years; and Current Population Survey, October 1970 through 2007. Washington, DC: US Department of Commerce; 2009 [Google Scholar]
- 9. National Association of School Nurses School nursing in the United States Quantitative Study: Burkhardt Research Services, 2007. Available at: www.nasn.ore/portals/0/2007/_burkhardt_report.pdf Accessed February 23, 2011
- 10. School Nursing Management of Students With Chronic Health Conditions. Silver Spring, MD: National Associations of School Nurses Inc; 2006 [Google Scholar]
- 11. Sussman S, Sun P, Dent CW. A meta-analysis of teen cigarette smoking cessation. Health Psychol. 2006;25(5):549–557 [DOI] [PubMed] [Google Scholar]
- 12. McDonald P, Colwell B, Backinger CL, Husten C, Maule CO. Better practices for youth tobacco cessation: evidence of review panel. Am J Health Behav. 2003;27(suppl 2):S144–S158 [DOI] [PubMed] [Google Scholar]
- 13. Fiore MC, Jaen CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Rockville, MD: US Department of Health and Human Services; 2008 [Google Scholar]
- 14. Sims TH. Technical report: tobacco as a substance of abuse. Pediatrics. 2009;124(5). Available at: www.pediatrics.org/cgi/content/full/124/5/e1045 [DOI] [PubMed] [Google Scholar]
- 15. Mermelstein R, Colby SM, Patten C, et al. Methodological issues in measuring treatment outcome in adolescent smoking cessation studies. Nicotine Tob Res. 2002;4(4):395–403 [DOI] [PubMed] [Google Scholar]
- 16. Centers for Disease Control and Prevention Youth Risk Behavior Survey, May 21, 2004. Available at: www.cdc.gov/mmwr/PDF/ss/ss5302.pdf Accessed May 3, 2011
- 17. National Longitudinal Study of Adolescent Health Constructed measures of risk behavior, family context, school context, and individual characteristics. Available at: www.cpc.unc.edu/projects/addhealth/focus.html Accessed March 18, 2002
- 18. Heatherton TF, Kozolowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test of Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict. 1991;86(9):1119–1127 [DOI] [PubMed] [Google Scholar]
- 19. DiFranza JR, Savageau JA, Rigotti NA, et al. Development of symptoms of tobacco dependence in youths: 30-month follow up data from the DANDY study. Tob Control. 2002;11(3):228–235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Choi WS, Patten CA, Gillin JC, Kaplan RM, Pierce JP. Cigarette smoking predicts development of depressive symptoms among U.S. adolescents. Ann Behav Med. 1997;19(1):42–50 [DOI] [PubMed] [Google Scholar]
- 21. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396 [PubMed] [Google Scholar]
- 22. Tangney JP, Baumeister RF, Boone AL. High self-control predicts good adjustment, less pathology, better grades, and interpersonal success. J Pers. 2004;72(2):271–324 [DOI] [PubMed] [Google Scholar]
- 23. March JS, Sullivan K. Test-retest reliability of the Multidimensional Anxiety Scale for Children. J Anxiety Disord. 1999;13(4):349–358 [DOI] [PubMed] [Google Scholar]
- 24. Prochaska J, DiClemente C. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51(3):390–395 [DOI] [PubMed] [Google Scholar]
- 25. Bandura A. Social Foundation of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986 [Google Scholar]
- 26. Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice-Hall; 1977 [Google Scholar]
- 27. Stata Statistical Software Release 8.2 College Station, TX: Stata Corp; 2004 [Google Scholar]
- 28. Backinger CL, McDonald P, Ossip-Klein DJ, et al. Improving the future of youth smoking cessation. Am J Health Behav. 2003;27(suppl 2):S170–S184 [PubMed] [Google Scholar]
- 29. Caraballo RS, Giovino GA, Pechacek TF. Self-reported cigarette smoking vs. serum cotinine among U.S. adolescents. Nicotine Tob Res. 2004;6(1):19–25 [DOI] [PubMed] [Google Scholar]
- 30. Kohler CL, Schoenberger YM, Beasley TM, Phillips MM. Effectiveness evaluation of the N-O-T smoking cessation program for adolescents. Am J Health Behav. 2008;32(4):368–379 [DOI] [PubMed] [Google Scholar]
- 31. Gervais A, O'Loughlin J, Meshefedjian G, Bancej C, Tremblay M. Milestones in the natural course of onset of cigarette use among adolescents. CMAJ. 2006;175(3):255–261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Scragg R, Wellman RJ, Laugesen M, DiFranza JR. Diminished autonomy over tobacco can appear with the first cigarettes. Addict Behav. 2008;33(5):689–698 [DOI] [PubMed] [Google Scholar]
- 33. Wellman RJ, DiFranza JR, Wood C. Tobacco chippers report diminished autonomy over smoking. Addict Behav. 2006;31(4):717–721 [DOI] [PubMed] [Google Scholar]
- 34. Centers for Disease Control and Prevention Use of cessation methods among smokers aged 16–24 years: United States, 2003. MMWR Morb Mortal Wkly Rep. 2006;55(50):1351–1354 [PubMed] [Google Scholar]