Abstract
Classical swine fever virus (CSFV) and porcine parvovirus (PPV) are highly contagious pathogens, resulting in enormous economic losses in pig industries worldwide. Because vaccines play an important role in disease control, researchers are seeking improved vaccines that could induce antiviral immune responses against CSFV and PPV at the mucosal and systemic levels simultaneously. In this study, a genetically engineered Lactobacillus strain coexpressing the CSFV-specific cytotoxic T lymphocyte (CTL) epitope 290 and the VP2 antigen of PPV was developed, and its immunopotentiating capacity as an oral vaccine in pigs was analyzed. The data demonstrated that in the absence of any adjuvant, the recombinant Lactobacillus strain can efficiently stimulate mucosal and systemic CSFV-specific CD8+ CTL responses to protect pigs against CSFV challenge. Moreover, anti-PPV-VP2 serum IgG and mucosal IgA were induced in pigs immunized orally with the recombinant Lactobacillus strain, showing a neutralizing effect on PPV infection. The results suggest that the recombinant Lactobacillus microecological agent may be a valuable component of a strategy for development of a vaccine against CSFV and PPV.
INTRODUCTION
Classical swine fever virus (CSFV), a member of the genus Pestivirus of the family Flaviviridae, is a small, enveloped, single-stranded RNA virus. Under natural conditions, the pig is the only susceptible species, and the virus can cause acute, subacute, or chronic disease (10, 26, 29). Porcine parvovirus (PPV), characterized as a member of the autonomous parvoviruses, is a major cause of reproductive failure in swine, resulting in early embryonic death, fetal death, stillbirths, and delayed return to estrus (5, 24, 28). Enormous economic losses to pig industries have been caused by these two pathogens. Therefore, the development of an efficient vaccine against CSFV and PPV simultaneously is of practical significance.
For vaccines against CSFV, the important role of humoral immune responses has been investigated, particularly in terms of neutralizing antibodies. For instance, pigs that were immunized with recombinant virus expressing CSFV E0 or E2 protein were protected against CSFV challenge (47). In some cases, immunization of animals with recombinant virus expressing other CSFV proteins failed to induce detectable neutralizing antibodies, whereas the animals were protected against lethal CSFV infection, which indicated that virus-specific T lymphocytes participated in a protective immune response against CSFV (38, 44, 48). Currently, cellular immune responses, especially production of virus-specific cytotoxic T lymphocytes (CTL), are receiving more attention for their potential roles in developing efficient epitope vaccines against CSFV (18, 35). Several CSFV-specific T-cell epitopes have been identified (3, 8, 32). Of them, the epitope peptide 290 (KHKVRNEVMVHWFDD), located at amino acid residues 1446 to 1460 of the CSFV nonstructural protein NS2-3, could be advantageous, as it harbors a CSFV-specific helper T-cell epitope and a CTL epitope, which could elicit both CD4+ and CD8+ T-cell responses (3). Therefore, peptide 290 is a promising candidate for an epitope vaccine for the control of CSF. Among vaccines against PPV, the inactivated vaccine is the one most often used to prevent and control infection, and humoral immune responses, in particular, neutralizing antibodies, play an important role. Therefore, the development of efficient vaccines that induce antibodies which neutralize PPV infection is desirable. The VP2 protein of PPV encompasses major antigenic domains and is therefore regarded as a promising candidate immunogen with the capacity to induce neutralizing antibodies (27, 41).
Moreover, CSFV and PPV initiate their infectious cycle at the mucosal surfaces. Although parenteral vaccination is usually efficient in eliciting a protective immune response, the parenteral routes generally fail to stimulate mucosal immune responses and cannot efficiently prevent the pathogens from entering the body via the mucosae. Therefore, efficient protection against mucosal invasion requires the development of new vaccines to induce protective mucosal immune responses at the infection point (17, 21). In this respect, mucosal immunization has been proven to be an effective approach (9, 22). Thus, it is necessary to develop efficient and safe antigen vectors that could trigger mucosal and systemic immune responses. One promising approach relies on the use of live vehicles (2). Lactobacillus strains possess many properties that make them attractive candidates as antigens carriers for the presentation to the mucosae of compounds with pharmaceutical interest, in particular, immunomodulators and vaccines. Lactobacilli are well known for having beneficial effects on the health of humans and animals. In addition, lactobacilli can survive in and colonize the intestinal tract (1, 50) and, furthermore, induce a nonspecific immunoadjuvant effect (30). The potential of live recombinant Lactobacillus to deliver heterologous antigens to the immune system has been investigated (14, 31, 33, 34, 36, 40, 51), suggesting the feasibility of using lactobacilli as safe oral vaccines.
In the present study, a recombinant Lactobacillus strain coproducing a CSFV-specific CTL epitope and PPV VP2 protein was developed using the plasmid pPG612.1 as an expression vector, and its immunogenicity as an oral vaccine used to elicit antiviral mucosal and systemic immune responses in pigs was analyzed. Our data showed that oral immunization with the recombinant strain was able to induce CSFV-specific CTL responses against CSFV challenge and neutralizing antibodies against PPV infection in pigs, which indicate a new strategy for the development of CSFV and PPV vaccines.
MATERIALS AND METHODS
Bacteria, plasmids, and viruses.
Lactobacillus casei ATCC 393 and plasmid pPG612.1 were kindly gifted by J. Seegers (NIZO, Netherlands). CSFV strain Shimen and PPV NADL-2 strain were kindly supplied by the China Institute of Veterinary Drug Control. PPV strain LJL12 was preserved in the Veterinary Department, Northeast Agricultural University, Harbin, People's Republic of China.
Construction of the recombinant Lactobacillus strain.
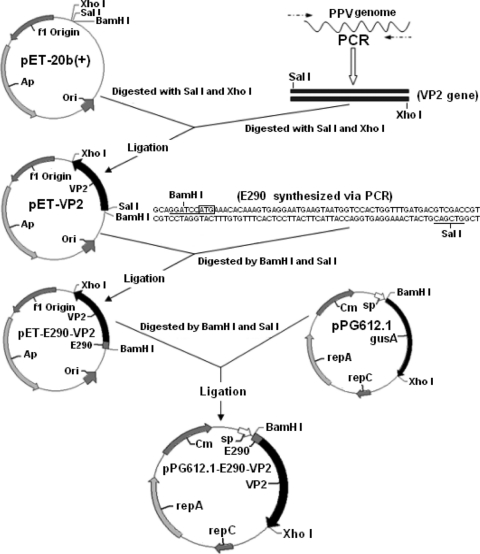
All DNA manipulations were performed according to standard procedures (39). The genomic DNA of PPV strain LJL12 propagated on swine testicular (ST) cells was extracted by the sodium dodecyl sulfate (SDS)-protease K (Sigma) method, and then the VP2 gene of PPV was obtained by PCR with the primers 5′-CGAGTCGACTATGGTTCACTGGTTCGACGACCG-3′ (upper) and 5′-GCTCTCGAGCCATGCTACCTGATTAACCGAG-3′ (lower), containing a SalI site and an XhoI site (underlined), respectively. The VP2 gene was cloned as a SalI/XhoI fragment into plasmid pET-20b(+), generating pET-VP2. The gene encoding CSFV peptide 290 was synthesized by PCR assay with the primers 5′-GCAGGATCCATGAAACACAAAGTGAGGAATGAAGTAATGGTC-3′ (upper) and 5′-TCGGTCGACGTCATCAAACCAGTGGACCATTACTTCATTCCT-3′ (lower), containing a BamHI site and a SalI site, respectively, which overlapped each other by 18 bases. The PCR product was cloned as a BamHI/SalI fragment into pET-VP2, giving rise to pET-E290-VP2. Then the BamHI/XhoI fragment of pET-E290-VP2 was subcloned into pPG612.1, generating pPG612.1-E290-VP2 (Fig. 1). Subsequently, the recombinant Lactobacillus was constructed by electroporation according to the method described previously (50). The resulting transformant, Lc393-rE290-VP2, was identified by enzyme digestion and sequencing.
Fig. 1.
Expression plasmid construction. The VP2 gene of PPV, amplified by PCR, and the CSFV-specific CTL epitope 290 gene, synthesized by PCR, were successively cloned as SalI/XhoI and BamHI/SalI fragments into pET-20b(+), generating pET-VP2 and pET-E290-VP2, respectively. The fusion genes were then subcloned as BamHI/XhoI fragments into plasmid pPG612.1, giving rise to pPG612.1-E290-VP2. “sp” is the secretion signal peptide of the pPG612.1 plasmid used to secrete antigen, which originated from the lactococcal Usp45 protein and was combined with the xylose operon promoter.
Colonization capacity of the recombinant strain in intestinal tracts.
The recombinant strain Lc393-rE290-VP2 was labeled with the fluorescent dye 5′ (and 6′)-carboxyfluorescein diacetate succinimidyl ester (cFDA-SE) (Sigma). In brief, a group of three pigs (2 weeks old) were fed approximately 1010 CFU/ml of the cFDA-SE-labeled recombinant strain. As controls, two other groups of three pigs were fed either cFDA-SE-labeled L. casei ATCC 393 or sterile PBS. On the 1st, 3rd, 5th, and 7th days after oral administration, the duodenum, jejunum, ileum, and colon of the pigs were extracted in compliance with ethical guidelines. Individual sections were cut longitudinally, and any visible residual food particles or fecal materials were removed prior to examination. cFDA-SE-labeled lactobacilli in different intestine sections were enumerated on an Epics Elite flow sorter at a 488-nm excitation wavelength with a 15-mW argon laser and a 75-mm sort sense flow cell at 82.7 kPa of pressure. Upon excitation at 488 nm in the flow cytometer (BD), cFDA-SE gives a maximal emission signal in the green fluorescence at 518 nm. Data were recorded in the FCSExpress 4.0 file format by using Coulter Epics Elite software and then were analyzed using WinMDI 2.9. The fully cFDA-SE-labeled lactobacilli were used as positive controls, and the unlabeled lactobacilli were used as negative controls.
Protein expression and Western blotting.
Lc393-rE290-VP2 and L. casei ATCC 393 harboring pPG612.1 were cultivated overnight in MRS medium supplemented with 2% xylose. The overnight cultures were centrifuged at 5,000 × g for 10 min, and the supernatant was collected, concentrated 10 times using an Ultrafree-CL PBCC centrifugal filter unit (Millipore), and analyzed by SDS–10% polyacrylamide gel electrophoresis (PAGE). Then, proteins were transferred onto a nitrocellulose membrane (Invitrogen). After blotting, nonspecific protein-binding sites were blocked overnight with blocking solution (Tiangen, Beijing, China) at 4°C, and the immunoblots were developed using mouse anti-PPV-VP2 serum and anti-CSFV peptide 290 mouse serum. Horseradish peroxidase (HRP)-conjugated goat anti-mouse IgG (Sigma) was used, and immunolabeled bands were then visualized with a chemiluminescent substrate reagent (Pierce) according to the manufacturer's instructions.
Immunization.
Lc393-rE290-VP2 was cultured and centrifuged. Cell pellets were resuspended in sterile suspension buffer to a concentration of ∼1 × 1010 CFU/ml. A vaccination group of 15 pigs (2 to 3 months old; no maternal antibodies to CSFV or PPV) obtained from the Harbin TianXiang pig farm, Harbin, People's Republic of China, and five miniature pigs of the d/d haplotype obtained from HuaiBei, Beijing, People's Republic of China, were immunized orally with 1010 CFU/ml recombinant strain per kg, and control groups were immunized with equivalent doses of Lc393:pPG612.1 and PBS (15 pigs per group). The immunization protocol was administered on two consecutive days (days 0 and 1). A booster immunization was given at days 14 and 15, and a second booster was given at days 28 and 29.
Cytotoxic-T-cell assays.
Five vaccinated miniature pigs of the d/d haplotype kept under specific-pathogen-free (SPF) conditions were bled on the 35th day after the first immunization, and then peripheral blood mononuclear cells (PBMC) were separated using density gradient centrifugation as described previously (42). At the same time, intestinal tissue was obtained by laparotomy, and lamina propria lymphocytes were prepared as previously described (4). The immune cells were seeded in 96-well round-bottom microplates to a concentration of 1 × 106/ml in RPMI 1640 supplemented with 10% fetal bovine serum (FBS) (Sigma) and restimulated with 1 × 105 50% tissue culture infective doses (TCID50) of CSFV Shimen per well for 5 days and were used as effector cells. MAX cells, a kind gift from G. H. Zhang (Northeast Agricultural University, Harbin, China) were infected with CSFV Shimen for 48 h and were used as target cells in cytotoxicity assays (3). In brief, 1 × 106/ml target cells were labeled with 100 μCi of Na251CrO4 (Amersham) for 1 h at 37°C in 5% CO2 and then washed and resuspended in culture medium. For the CTL with peptides, 1 × 105/ml noninfected chromium-labeled MAX cells were incubated with 25 μg of CSFV peptide 290 at 37°C in a 5% CO2 incubator for 2 h. CSFV-infected or peptide-loaded target cells (1 × 103 cells per well) were added to various concentrations of effector cells (ranging from 1.25 × 104 to 5.0 × 104 cells per well). All experiments were performed in triplicate cultures. The cells were centrifuged at 100 × g for 5 min and incubated at 37°C in 5% CO2 for 4 h. The chromium levels in the supernatants were measured using a COBRA Auto-Gamma model 5003 gamma counter (Packard). The percentage of specific cytolytic activity was calculated as follows: {[(cpm experimental release) − (cpm spontaneous release)]/[(cpm total release) − (cpm spontaneous release)]} × 100. Mock-infected or negative peptide-loaded target cells served as the controls. Furthermore, an enzyme-linked immunospot (ELISPOT) assay was used to detect peptide-specific gamma interferon (IFN-γ)-secreting cells as described previously (3), with minor modifications. PBMCs incubated with an irrelevant peptide served as the negative control.
CSFV challenge experiment for pigs immunized with Lc393-rE290-VP2.
CSFV Shimen was propagated in porcine kidney 15 (PK-15) cells at 37°C in a 5% CO2 incubator for 3 to 5 days. Virus titers were determined by endpoint dilution titrations on PK-15 cells according to the method described previously (19, 35). All groups of pigs (those that were orally fed with recombinant Lc393-rE290-VP2 and the Lc393:pPG612.1 and PBS controls) were challenged orally with a lethal dose of CSFV strain Shimen (105 TCID50/animal). The pigs were examined daily for disease symptoms and fever, defined by the rectal temperature of the pig (25). Survival rates were recorded during 15 days after challenge. Serum samples were collected at various time points before and after CSFV challenge, and virus titers of serum samples were determined by endpoint dilution titrations (18).
ELISA analysis for anti-PPV-VP2 antibody levels in pigs.
Sera were prepared on days 0, 7, 14, 21, 28, 35, and 42 after the first immunization and stored at −70°C until required. At the same time, intestinal lavage fluids of pigs were collected and prepared for enzyme-linked immunosorbent assay (ELISA) as previously described (11, 37). Polystyrene microtiter plates were coated overnight at 4°C with PPV strain LJL12 propagated on ST cells. The ELISA plates were washed three times with PBS containing 1% Tween 20 and then saturated with PBS–5% skim milk at 37°C for 2 h. Serum or intestinal lavage samples were diluted with PBS–1% bovine serum albumin (BSA) and used as primary antibodies. After incubation at 37°C for 1 h, the plates were washed another three times. Bound antibodies were detected using HRP-conjugated goat anti-pig IgA or IgG diluted 1:2,000 (Sigma), followed by color development using tetramethylbenzidine (TMB) as the substrate, and then absorbance was measured at 490 nm.
Neutralizing ability of antibodies to PPV obtained from immunized pigs.
Serum IgG and mucosal IgA samples obtained from the pigs immunized orally with Lc393-rE290-VP2 on days 0, 7, 14, 21, 28, 35, and 42 after the first immunization were evaluated using a plaque reduction assay to determine their ability to neutralize PPV infection. The samples obtained from pigs fed Lc393:pPG612.1 or PBS were used as controls. In brief, nondiluted 50-μl samples were prepared in a 96-cell plate. PPV adjusted to 200 TCID50 in 50 μl of virus diluent (10% concentrated Hanks balanced salt solution, 0.1% bovine serum albumin [pH 7.4]) was added to the cell plate, mixed, and incubated at 37°C for 1 h. Then 100 μl of ST cells (used for virus infection) was added to the antibody-virus mixture and incubated in a 5% CO2 incubator at 37°C for 5 days. The overlay medium was then discarded, after which the wells were washed three times with sterile PBS, pH 7.4, and stained with 1% crystal violet solution. Differences in the numbers of plaques formed on the cells receiving the different treatments were examined for the level of significance by Student's t test after analysis of variance.
RESULTS
Colonization by recombinant Lc393-rE290-VP2.
Pigs were orally given cFDA-SE-labeled Lc393-rE290-VP2, and then the different intestine sections were isolated on the 1st, 3rd, 5th, and 7th days after oral immunization. Following the collection of cFDA-SE-labeled Lc393-rE290-VP2, the ability of recombinant Lc393-rE290-VP2 to colonize swine intestine was determined by flow-cytometric analysis. Data showed that the recombinant strain was able to colonize the intestinal tract, including the duodenum, jejunum, ileum, and colon, with a colonization ability similar to that of L. casei ATCC 393 (Table 1).
Table 1.
Colonization efficacy of recombinant Lc393-rE290-VP2 compared with L. casei ATCC 393 in intestinal tracts of pigs
| L. casei strain | Day | No. of cells (avg ± SD) in: |
|||
|---|---|---|---|---|---|
| Duodenum | Jejunum | Ileum | Colon | ||
| ATCC 393 | 1 | 7.92E08 ± 0.58E08 | 8.97E08 ± 0.37E08 | 1.53E09 ± 0.55E09 | 9.85E08 ± 0.24E08 |
| 3 | 5.99E08 ± 0.35E08 | 7.85E08 ± 0.74E08 | 9.76E08 ± 0.71E08 | 8.79E08 ± 0.39E08 | |
| 5 | 3.68E08 ± 0.29E08 | 4.97E08 ± 0.79E08 | 8.37E08 ± 0.52E08 | 7.66E08 ± 0.46E08 | |
| 7 | 1.84E08 ± 0.75E08 | 3.22E08 ± 1.05E08 | 6.96E08 ± 0.23E08 | 6.43E08 ± 0.22E08 | |
| Lc393-rE290-VP2 | 1 | 7.86E08 ± 0.37E08 | 8.36E08 ± 0.36E08 | 1.47E09 ± 0.74E09 | 9.72E08 ± 0.36E08 |
| 3 | 5.85E08 ± 0.56E08 | 7.71E08 ± 0.48E08 | 9.58E08 ± 0.63E08 | 8.58E08 ± 0.25E08 | |
| 5 | 3.49E08 ± 0.33E08 | 4.55E08 ± 0.24E08 | 7.95E08 ± 0.62E08 | 7.53E08 ± 0.74E08 | |
| 7 | 1.57E08 ± 0.81E08 | 2.82E08 ± 0.65E08 | 6.37E08 ± 0.41E08 | 5.85E08 ± 0.59E08 | |
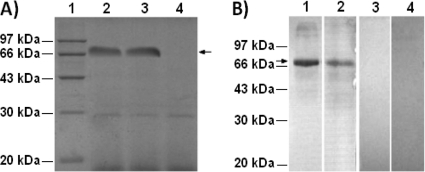
Expression of the fusion protein.
The supernatants of the recombinant strain Lc393-rE290-VP2 cultured overnight in MRS containing 2% xylose were concentrated 10 times and then analyzed by SDS-PAGE and Western blotting. The results of SDS-PAGE showed that a 70-kDa fusion protein was expressed and secreted into the supernatants of Lc393-rE290-VP2 but not Lc393:pPG612.1, as shown in Fig. 2 A. A 70-kDa immunoreactive band was detected in the supernatants of Lc393-rE290-VP2 using mouse anti-PPV-VP2 serum (Fig. 2B, lane 1) and anti-CSFV peptide 290 mouse antiserum (lane 2) as primary antibodies, whereas there was no band of interest with the control strain Lc393:pPG612.1 (lanes 3 and 4).
Fig. 2.
Secretion expression of fusion protein from Lc393-rE290-VP2. The supernatants were analyzed by SDS-PAGE and Western blotting. (A) SDS-PAGE analysis. Lane 1, molecular mass marker. A 70-kDa fusion protein was observed in the supernatants of Lc393-rE290-VP2 (lanes 2 and 3, arrow) but not in Lc393:pPG612.1 (lane 4). (B) Western blotting. An immunoreactive band was observed (lanes 1 and 2) in a position similar to that observed with SDS-PAGE using anti-PPV-VP2 monoclonal antibody 3C9 and anti-CSFV peptide 290 mouse antiserum as primary antibodies, respectively, but no immunoblots were observed with the supernatants of Lc393:pPG612.1 (lanes 3 and 4).
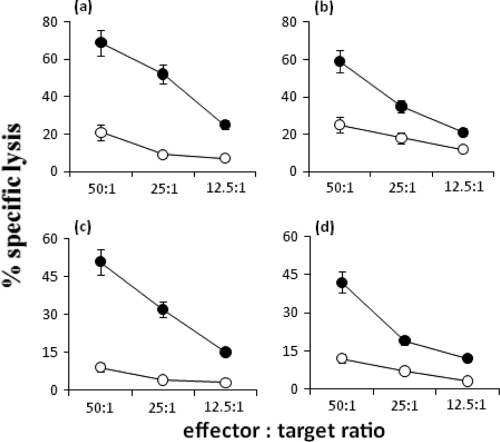
Induction of specific cytotoxic responses by the recombinant strain in vivo.
The capacity of the recombinant strain Lc393-rE290-VP2 to stimulate mucosal and systemic cytotoxic responses against CSFV was analyzed in vivo. The PBMC and lamina propria lymphocytes of vaccinated miniature pigs were obtained on the 35th day after the first immunization and restimulated in vitro with CSFV Shimen, and then the cytotoxic activity was tested by evaluating the lysis of peptide-loaded target MAX cells labeled with chromium. Mock-infected or negative-peptide-loaded target cells served as the controls. A cytolytic response against peptide 290-loaded MAX cells was observed not only in mucosal tissue (Fig. 3 d) but also at the systemic level (Fig. 3b), which indicated that Lc393-rE290-VP2 was able to stimulate a CSFV-specific CD8+ CTL response in vivo.
Fig. 3.
Specific cytotoxicity of CSFV CTL to target cells sensitized by CSFV Shimen (a and c) or peptide 290 (b and d). PBMCs (a and b) and lamina propria lymphocytes (c and d) of pigs vaccinated with Lc393-rE290-VP2 and restimulated with CSFV in vitro were used as effector cells. The cytotoxicity of the T cells was determined in a chromium release assay by lysis of virus-sensitized (a and c, •) or peptide-sensitized (b and d, •) MAX cells as targets. MAX cells incubated with supernatants of mock-infected cells (a and c, ○) or with irrelevant peptide (b and d, ○) were used as the controls. Data are means from triplicate samples ± standard errors of the means.
In order to confirm the reactivity of CSFV-specific T cells against CSFV antigens, PBMCs obtained after vaccination and challenge infection were tested for their ability to produce IFN-γ upon stimulation with virus peptide in ELISPOT assays. Data showed that high numbers of IFN-γ-secreting cells were observed when PBMCs from infected pigs were stimulated with peptide 290, while none of the unvaccinated animals had detectable circulating virus-specific IFN-γ-producing cells (Fig. 4). The release of IFN-γ by peptide 290 was sequence specific, because only a few spots were observed after incubation of PBMCs with an irrelevant peptide.
Fig. 4.
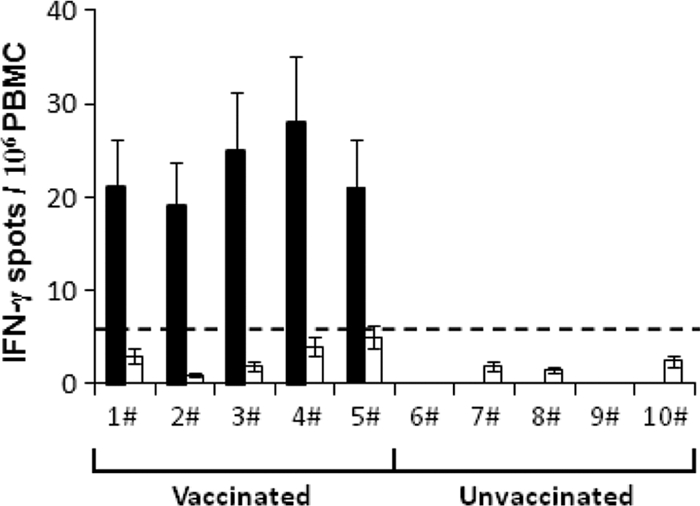
IFN-γ ELISPOT of PBMC obtained from pigs on the 35th day after immunization with Lc393-rE290-VP2 (1# to 5#). Unvaccinated pigs (6# to 10#) were used as controls. The data are numbers of IFN-γ spots from CSFV-stimulated cultures per 106 PBMCs (▪). PBMCs incubated with an irrelevant peptide served as the controls (□). The dotted line represents the threshold value used for the identification of antigen-specific spots based on the values obtained before infection. The means of triplicates plus standard errors of the means are shown.
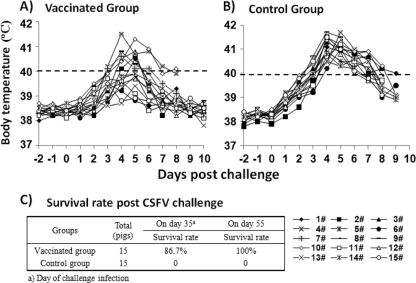
Recombinant Lc393-rE290-VP2 protects pigs against CSFV challenge.
In order to analyze the capacity of the recombinant strain Lc393-rE290-VP2 to protect pigs against CSFV infection, the vaccinated pigs were challenged orally with a lethal dose (105 TCID50/animal) of CSFV strain Shimen on the 35th day after the first immunization, and the pigs immunized orally with Lc393:pPG612.1 or PBS were used as controls. Results demonstrated effective protection (86.7%) against CSFV challenge performed on day 35 in vaccinated pigs, while control groups of pigs developed severe clinical symptoms of CSF after viral challenge and were euthanized when moribund at 9 days after the challenge infection (Fig. 5). In addition, the surviving pigs were fully protected against an additional viral challenge performed on day 55, which indicated that the Lc393-rE290-VP2 was able to induce long-term protective immunity against CSFV. Vaccinated groups of pigs showed a virus challenge-induced fever peak from 4 to 6 days postchallenge, and on days 7 to 8 after challenge, the pigs recovered clinically from CSFV clinical signs, while the control groups developed severe symptoms of CSF with a high fever peak at 4 to 7 days after viral infection (Fig. 5). Little virus was detected in vaccinated groups of surviving pigs on day 15 after challenge, indicating efficient viral clearance (Table 2).
Fig. 5.
Body temperatures of pigs vaccinated orally with Lc393-rE290-VP2 after CSFV challenge (A) and control pigs immunized with Lc393:pPG612.1 (B). (C) Survival rate of animals after CSFV challenge. Effective protection (86.7%) against CSFV challenge performed on the 35th day was observed in vaccinated pigs, while control groups of pigs developed severe clinical symptoms of CSF after viral challenge and were euthanized when moribund.
Table 2.
Serum virus titers
| Vaccination | Postchallenge day | Titer (TCID50/ml serum) in piga |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | ||
| Lc393-rE290-VP2 | 3 | 102.3 | 102.0 | 101.8 | 103.0 | 101.2 | 102.4 | 101.7 | 101.5 | 102.2 | 103.3 | 102.1 | 102.3 | 101.8 | 102.4 | 101.9 |
| 6 | 101.2 | 101.1 | 100.5 | 104.2 | ND | 101.5 | ND | ND | 101.0 | 104.5 | 100.7 | 101.2 | 100.5 | 101.7 | 100.7 | |
| 9 | 100.3 | ND | ND | 105.3 | ND | 100.2 | ND | ND | ND | 105.6 | ND | 100.4 | ND | 100.3 | ND | |
| 12 | ND | ND | ND | — | ND | ND | ND | ND | ND | — | ND | ND | ND | ND | ND | |
| 18 | ND | ND | ND | — | ND | ND | ND | ND | ND | — | ND | ND | ND | ND | ND | |
| Lc393:pPG612.1 | 3 | 103.5 | 103.4 | 104.1 | 103.3 | 103.2 | 103.2 | 103.4 | 103.5 | 105.1 | 103.1 | 103.3 | 103.4 | 103.2 | 103.3 | 103.9 |
| 6 | 104.3 | 105.2 | — | 105.6 | 104.5 | 104.7 | 105.2 | 104.9 | — | 104.4 | 104.9 | 105.1 | 104.5 | 104.1 | 105.5 | |
| 9 | 105.8 | — | — | — | 105.6 | 105.5 | — | — | — | 105.6 | — | — | 105.3 | 105.5 | — | |
| 12 | — | — | — | — | — | — | — | — | — | — | — | — | — | — | — | |
| 18 | — | — | — | — | — | — | — | — | — | — | — | — | — | — | — | |
| PBS | 3 | 104.3 | 103.2 | 104.0 | 103.1 | 103.7 | 103.4 | 104.1 | 104.0 | 104.2 | 103.4 | 103.6 | 103.2 | 105.3 | 104.9 | 103.3 |
| 6 | — | 104.7 | 105.5 | 104.5 | 105.2 | 105.1 | — | 105.8 | — | 104.6 | 105.1 | 104.5 | — | — | 104.0 | |
| 9 | — | 105.8 | — | 105.7 | — | — | — | — | — | 105.8 | — | 105.9 | — | — | 105.7 | |
| 12 | — | — | — | — | — | — | — | — | — | — | — | — | — | — | — | |
| 18 | — | — | — | — | — | — | — | — | — | — | — | — | — | — | — | |
ND, not determined; —, animal was euthanized when moribund, in compliance with ethical guidelines.
Anti-PPV-VP2 immune responses induced in pigs.
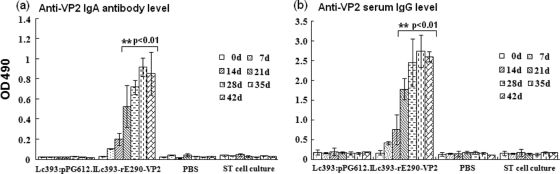
The local mucosal and systemic immune responses were investigated by measuring the anti-VP2 IgA level in intestinal lavage samples and the anti-VP2 IgG level in serum of pigs after oral immunization, respectively. The levels of IgA and IgG against VP2 were determined via ELISA using PPV strain LJL12 as a coated antigen. As shown in Fig. 6 a, there was no substantial difference (P > 0.05) in mucosal IgA level between the vaccinated group and the control groups prior to immunization, while oral immunization of Lc393-rE290-VP2 elicited an antigen-specific mucosal IgA response. After the second booster, high levels of anti-VP2 IgA were obtained in intestinal lavage fluids of the vaccinated pigs, showing a substantial difference (P < 0.01) relative to the control groups. Moreover, after the first booster, the pigs orally immunized with Lc393-rE290-VP2 exhibited a prompter and stronger anti-VP2 serum IgG response. No significant levels of anti-VP2 antibodies were observed in the control groups of pigs (P > 0.05) (Fig. 6b).
Fig. 6.
Anti-VP2 IgA levels in intestinal lavage fluid samples (a) and anti-VP2 IgG levels in serum (b). Pigs were immunized with Lc393-rE290-VP2 or with Lc393:pPG612.1. An additional control group of pigs received only PBS. Intestinal lavage fluids and sera were collected on days 7, 14, 21, 28, 35, and 42 after the first immunization. The VP2-specific IgA (a) and IgG (b) levels were tested by ELISA using PPV strain LJL12 as the coated antigen. ST cell culture was used as a negative control antigen. Values are means ± standard errors of the means.
PPV-neutralizing ability of antibodies.
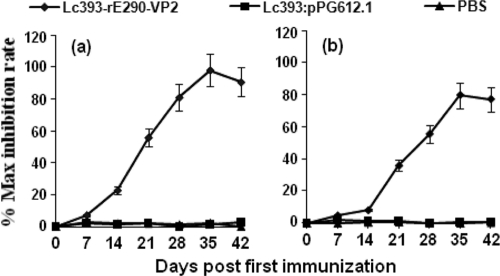
Plaque reduction assays were performed to test the PPV-neutralizing ability of antibodies collected from the pigs orally immunized with Lc393-rE290-VP2. The samples of serum antibody IgG and mucosal antibody IgA were obtained from the vaccinated pigs on days 0, 7, 14, 21, 28, 35, and 42 and after the first immunization. Neutralizing ability was expressed as the maximum inhibition rate. The results demonstrated that the presence of anti-VP2 IgA or IgG in the culture medium conferred a statistically significant (P < 0.05) ability to neutralize PPV infection. Maximum inhibition rates were nearly 96.7 ± 1.29% for anti-VP2 IgG (Fig. 7 a) and 70.6 ± 1.05% for anti-VP2 IgA (Fig. 7b), which indicated that Lc393-rE290-VP2 could induce neutralizing antibodies to PPV.
Fig. 7.
Inhibition of viral plaque formation by sera (a) and intestinal lavage fluids (b) prepared from pigs orally immunized with Lc393-rE290-VP2. Sera and intestinal lavage fluids were collected on days 0, 7, 14, 21, 28, 35, and 42 after the first immunization. The value for each sample was expressed as maximum reduction in number of plaques. Results are means ± standard errors of the means.
DISCUSSION
In the development of virus vaccines, antigen delivery vehicles play a critical role in the effectiveness of vaccination against pathogens. Several strategies have been developed to deliver exogenous antigens into the cytosol. Protein or peptide antigens delivered in association with appropriate adjuvants (e.g., incomplete Freund's adjuvant, liposomes [52], ISCOMs [43], or complete Freund's adjuvant [16]) or in particulate form linked to latex microspheres efficiently stimulate cellular or humoral immune responses (20). Recombinant live vectors, including attenuated viruses (such as vaccinia virus [15], Mengo virus [2], or pseudorabies virus [48]) or bacteria (such as bacillus Calmette-Guérin [49], Lactobacillus [14, 31, 36, 50], Salmonella [13], or Listeria [12]), have also been shown to induce a protective immune response in vivo. In contrast, among the available approaches to stimulate efficient mucosal responses, using lactobacilli as carriers to deliver vaccine antigens constitutes one of the most successful strategies (23).
At present, CSF is controlled by stamping out-methods and vaccination, or a combination of the two, but the eradication strategy has inevitably resulted in enormous economic losses. Though traditional CSFV avirulent vaccines, in particular the lapinized C strain of CSFV, have been successfully used in several countries to prevent and control CSF, the use of traditional CSFV avirulent vaccines has been banned since 1990 by the European Union, mainly because infections with vaccine and field viruses cannot be distinguished serologically (32). Therefore, the design of new efficacious vaccines to protect animals against CSFV is being pursued. Previous studies have shown that a cellular immune response, especially production of CSFV-specific CD8+ CTLs, represents an important defense mechanism in the elimination of cells infected by CSFV (32, 35). Thus, further work should focus on the development of inducible CD8+ CTL response vaccines against CSFV.
PPV is a fairly ubiquitous virus that multiplies normally in the swine intestine without causing clinical signs. Initial PPV infection mainly occurs at the mucosa of the intestines (6). Therefore, the elicitation of an efficient immune response not only at the systemic but also at the mucosal level after vaccination is highly desirable (7, 46) and would represent a significant advantage in preventing PPV infection via the mucosa. This goal can be achieved only when the vaccination is administered by the mucosal route.
In this study, Lactobacillus casei was selected as the live oral vaccine vehicle to deliver a CSFV-specific CTL epitope and PPV-VP2 protein to induce a protective antiviral immune response against CSFV and PPV in pigs. The fusion protein was successfully expressed by Lc393-rE290-VP2, as determined by SDS-PAGE and Western blotting, and its antigenic properties were not compromised, as it can be recognized by a specific antiserum. Moreover, the recombinant plasmid pPG612.1-E290-VP2 showed good segregational and structural stability in L. casei ATCC 393 following serial subcultures.
For virus vaccine research, one critical step is the identification of immune responses and immune defenses stimulated by antigenic subunits against infection in the host. Most investigations have concentrated on the role of the humoral immune response in CSFV-infected animals (45, 47), while the cellular immune response is often ignored. The study of the cellular immune response to CSFV in the natural host is of the utmost importance for understanding the interaction between the pathogen and the swine immune system (3, 8, 32). This is the basis for the development of vaccines to control CSFV infection. In this work, the capacity of Lc393-rE290-VP2 to stimulate CSFV-specific CTL responses in vitro and in vivo was analyzed. In the absence of any adjuvants, a CSFV-specific CTL response was detected in the intestinal mucosal tissues of miniature swine vaccinated orally with the recombinant strain, and no measurable CTL activity was detectable in nonimmunized animals, which indicated that the effector cells were able to recognize naturally processed epitope from the infectious virus and kill peptide 290-coated target cells. This result suggests that the local mucosal immunity induced by the recombinant strain, in particular the induction of a local CD8+ cytotoxic T lymphocyte response, may control CSFV replication within local tissues prior to systemic dissemination. We also analyzed whether mucosal immunization with the strain could induce antigen-specific CD8+ CTLs systemically, and a significant cytolytic response was observed. The result is consistent with previously described CTL activity in other studies (3). Due to these promising results in vitro, the protective capacity of Lc393-rE290-VP2 was tested. Pigs immunized orally with this recombinant strain were effectively protected against CSFV challenge through induction of CSFV-specific major histocompatibility complex (MHC) class I-restricted CD8+ CTLs, while control groups of pigs developed severe clinical symptoms of CSF after viral challenge and were euthanized when moribund. In addition, Lc393-rE290-VP2 was able to induce long-term protective immunity against CSFV.
IgA is the predominant antibody at the mucosal surface, as it is produced locally at a level that exceeds that of all other immunoglobulins, and it plays an important role in preventing the invasion of pathogens (7). Thus, an efficient PPV oral vaccine will have to induce specific immune responses not only at the systemic level but also at the mucosal level, in particular the mucosal IgA response against virus invasion via the mucosa. We evaluated the immunogenicity of Lc393-rE290-VP2 in pigs and found that both mucosal and systemic immune responses could be efficiently elicited after intragastric administration. As experiments to test for protection of gravid pigs against PPV challenge are difficult, in order to confirm the efficacy of the induced antibodies in inhibiting the virus, we determined whether intestinal lavage fluids and sera could inhibit the infection of ST cells in a plaque reduction neutralization assay. Serum and intestinal samples collected from vaccinated pigs demonstrated statistically significant inhibition, which would be a first step to give the proof of principle for the protection efficacy in the target species. Moreover, the availability of a live oral vaccine that can colonize the intestinal tract is important and desirable. In this study, we investigated the colonization potential of Lc393-rE290-VP2 in pig intestines and showed that the recombinant strain was able to persistently colonize the intestinal tracts, similar to its native counterpart, L. casei ATCC 393. As it is a probiotic bacterium, a long residence time in the intestinal tracts would prolong its potential beneficial health effects.
In conclusion, our results clearly demonstrate that the recombinant strain Lc393-rE290-VP2, constructed in this study, provides a safe and efficient vaccine to induce CSFV-specific CTLs against CSFV and PPV-neutralizing activity with the probiotic effects of L. casei ATCC 393, which suggests that this is a promising expression and delivery system for presenting different CTL epitopes or viral antigens to the immune system.
ACKNOWLEDGMENTS
We sincerely thank Jos Seegers for kindly providing the bacterial strain L. casei ATCC 393 and the plasmid pPG612.1.
This work was supported by grants from the National Natural Sciences Funds of China (30371074), Harbin Scientific and Technological Projects (2005AA6CN087), and Heilongjiang Province Postdoctoral Fund (LBH-Z09).
Footnotes
Published ahead of print on 21 September 2011.
REFERENCES
- 1. Alander M., et al. 1999. Persistence of colonization of human colonic mucosa by a probiotic strain, Lactobacillus rhamnosus GG, after oral consumption. Appl. Environ. Microbiol. 65:351–354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Altmeyer R., et al. 1995. Attenuated Mengo virus: a new vector for live recombinant vaccines. J. Virol. 69:3193–3196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Armengol E., et al. 2002. Identification of T-cell epitopes in the structural and non-structural proteins of classical swine fever virus. J. Gen. Virol. 83:551–560 [DOI] [PubMed] [Google Scholar]
- 4. Belyakov I. M., et al. 2001. Mucosal AIDS vaccine reduces disease and viral load in gut reservoir and blood after mucosal infection of macaques. Nat. Med. 7:1320–1326 [DOI] [PubMed] [Google Scholar]
- 5. Bergeron J., Menezes J., Tijssen P. 1993. Genome organization and mapping of transcription and translation products of the NADL-2 strain of porcine parvovirus. Virology 197:86–98 [DOI] [PubMed] [Google Scholar]
- 6. Bican J., Svoboda M., Drabek J. 2002. Porcine parvovirus infection in boars in the Czech Republic. Acta Vet. Brno 71:45–49 [Google Scholar]
- 7. Brandtzaeg P. 1994. Distribution and characteristics of mucosal immunoglobulin producing cells, p. 251–279 In Strober W., Mestecky J., Lamm M. E., Bienenstock J., Ogra P. L. (ed.), Handbook of mucosal immunology. Academic Press, San Diego, CA [Google Scholar]
- 8. Ceppi M., et al. 2005. Identification of classical swine fever virus protein E2 as a target for cytotoxic T cells by using mRNA-transfected antigen-presenting cells. J. Gen. Virol. 86:2525–2534 [DOI] [PubMed] [Google Scholar]
- 9. Chen H. 2000. Recent advances in mucosal vaccine development. J. Control. Release 67:117–128 [DOI] [PubMed] [Google Scholar]
- 10. Edwards S., et al. 2000. Classical swine fever: the global situation. Vet. Microbiol. 73:103–119 [DOI] [PubMed] [Google Scholar]
- 11. Elson C. O., Ealding W., Lefkowiz J. 1984. A lavage technique allowing repeated measurement of IgA antibody in mouse intestinal secretion. J. Immunol. Methods 67:101–108 [DOI] [PubMed] [Google Scholar]
- 12. Goossens P. L., Milon G., Cossart1 P., Saron M. F. 1995. Attenuated Listeria monocytogenes as a live vector for induction of CD8+ T cells in vivo: a study with the nucleoprotein of the lymphocytic choriomeningitis virus. Int. Immunol. 7:797–805 [DOI] [PubMed] [Google Scholar]
- 13. Harding C. V., Pfeife J. D. 1994. Antigen expressed by Salmonella typhimurium is processed for class I major histocompatibility complex presentation by macrophages but not infected epithelial cells. Immunology 83:670–674 [PMC free article] [PubMed] [Google Scholar]
- 14. Ho P. S., Kwang J., Lee Y. K. 2005. Intragastric administration of Lactobacillus casei expressing transmissible gastroenteritis coronavirus spike glycoprotein induced specific antibody production. Vaccine 23:1335–1342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Irvine K. R., McCabe B. J., Rosenberg S. A., Restifo N. P. 1995. Synthetic oligonucleotide expressed by a recombinant vaccinia virus elicits therapeutic cytolytic T lymphocytes. J. Immunol. 154:4651–4657 [PMC free article] [PubMed] [Google Scholar]
- 16. Ke Y., Li Y., Kapp J. A. 1995. Ovalbumin injected with complete Freund's adjuvant stimulates cytolytic responses. Eur. J. Immunol. 25:549–553 [DOI] [PubMed] [Google Scholar]
- 17. Kilian M., Russel M. W. 1994. Functions of mucosal immunoglobulins, p. 127–143 In Strober W., Mestecky J., Lamm M. E., Bienenstock J., Ogra P. L. (ed.), Handbook of mucosal immunology. Academic Press, San Diego, CA [Google Scholar]
- 18. Kimman T. G., Bianchi A. T. J., Wensvoort G., de Bruin T. G. M., Meliefste C. 1993. Cellular immune response to hog cholera virus (HCV): T cells of immune pigs proliferate in vitro upon stimulation with live HCV, but the E1 envelope glycoprotein is not a major T-cell antigen. J. Virol. 67:2922–2927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Knoetig S. M., Summerfield A., Spagnuolo-Weaver M., McCullough K. C. 1999. Immuno-pathogenesis of classical swine fever: role of monocytic cells. Immunol. 97:359–366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kovacsovics-Bankowski M., Clark K., Benacerraf B., Rock K. L. 1993. Efficient major histocompatibility complex class I presentation of exogenous antigen upon phagocytosis by macrophages. Proc. Natl. Acad. Sci. U. S. A. 90:4942–4946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. London S. D. 1994. Cytotoxic lymphocytes in mucosal effector sites, p. 325–336 In Strober W., Mestecky J., Lamm M. E., Bienenstock J., Ogra P. L. (ed.), Handbook of mucosal immunology. Academic Press, San Diego, CA [Google Scholar]
- 22. McGhee J. R., et al. 1992. The mucosal immune system: from fundamental concepts to vaccine development. Vaccine 10:75–88 [DOI] [PubMed] [Google Scholar]
- 23. Medina E., Guzman C. A. 2001. Use of live bacterial vaccine vectors for antigen delivery: potential and limitation. Vaccine 19:1573–1580 [DOI] [PubMed] [Google Scholar]
- 24. Mengeling W. L., Lager K. M., Vorwald A. C. 2000. The effect of porcine parvovirus and porcine reproductive and respiratory syndrome virus on porcine reproductive performance. Anim. Reprod. Sci. 60-61:199–210 [DOI] [PubMed] [Google Scholar]
- 25. Mittelholzer C., Moser C., Tratschin J. D., Hofmann M. A. 2000. Analysis of classical swine fever virus replication kinetics allows differentiation of highly virulent from avirulent strains. Vet. Microbiol. 74:293–308 [DOI] [PubMed] [Google Scholar]
- 26. Moennig V. 2000. Introduction to classical swine fever: virus, disease and control policy. Vet. Microbiol. 73:93–102 [DOI] [PubMed] [Google Scholar]
- 27. Molitor T. W., Joo H. S., Collett M. S. 1983. Porcine parvovirus: virus purification and structural and antigenic properties of virion polypeptides. J. Virol. 45:842–854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Molitor T. W., Joo H. S., Collett M. S. 1984. Porcine parvovirus DNA: characterization of genomic and replicative form DNA of two virus isolates. Virology 137:241–254 [DOI] [PubMed] [Google Scholar]
- 29. Moormann R. J. M., et al. 1990. Molecular cloning and nucleotide sequence of hog cholera virus strain Brescia and mapping of the genomic region encoding envelope protein El. Virology 177:184–198 [DOI] [PubMed] [Google Scholar]
- 30. Ogawa T., Asai Y., Yasuda K., Sakamoto H. 2005. Oral immunoadjuvant activity of a new symbiotic Lactobacillus casei subsp casei in conjunction with dextran in BALB/c mice. Nutr. Res. 25:295–304 [Google Scholar]
- 31. Oliveira M. L. S., et al. 2003. Expression of Streptococcus pneumoniae antigens, PsaA and PspA by Lactobacillus casei. FEMS Microbiol. Lett. 227:25–31 [DOI] [PubMed] [Google Scholar]
- 32. Pauly T., et al. 1995. Classical swine fever virus-specific cytotoxic T lymphocytes and identification of a T cell epitope. J. Gen. Virol. 76:3039–3049 [DOI] [PubMed] [Google Scholar]
- 33. Perdigon G., Fuller R., Raya R. 2001. Lactic acid bacteria and their effect on the immune system. Curr. Issues Intest. Microbiol. 2:27–42 [PubMed] [Google Scholar]
- 34. Raha A. R., Varma N. R., Yusoff K. 2005. Cell surface display system for Lactococcus lactis: a novel development for oral vaccine. Appl. Microbiol. Biotechnol. 68:75–81 [DOI] [PubMed] [Google Scholar]
- 35. Rau H., Revets H., Balmelli C., McCullough K. C., Summerfield A. 2006. Immunological properties of recombinant classical swine fever virus NS3 protein in vitro and in vivo. Vet. Res. 37:155–168 [DOI] [PubMed] [Google Scholar]
- 36. Reveneau N., Geoffroy M. C., Locht C., Chagnaud P., Mercenier A. 2002. Comparison of the immune responses induced by local immunizations with recombinant Lactobacillus plantarum producing tetanus toxin fragment C in different cellular locations. Vaccine 20:1769–1777 [DOI] [PubMed] [Google Scholar]
- 37. Robinson K., Chamberlain L. M., Schofield K. M., Wells J. M., Le Page R. W. F. 1997. Oral vaccination of mice against tetanus with recombinant Lactococcus lactis. Nat. Biotechnol. 15:653–657 [DOI] [PubMed] [Google Scholar]
- 38. Rümenapf T., Stark R., Meyers G., Thiel H. J. 1991. Structural proteins of hog cholera virus expressed by vaccinia virus: further characterization and induction of protective immunity. J. Virol. 65:589–597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sambrook J., Russell D. W. 2001. Molecular cloning: a laboratory manual, 3rd ed. Cold Spring Harbor Laboratory, Cold Spring Harbor, NY [Google Scholar]
- 40. Scheppler L., et al. 2002. Recombinant Lactobacillus johnsonii as a mucosal vaccine delivery vehicle. Vaccine 20:2913–2920 [DOI] [PubMed] [Google Scholar]
- 41. Sedlik C., et al. 1999. Intranasal delivery of recombinant parvovirus-like particles elicits cytotoxic T-cell and neutralizing antibody responses. J. Virol. 73:2739–2744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Summerfield A., Rziha H. J., Saalmüller A. 1996. Functional characterization of porcine CD4+ CD8+ extrathymic T lymphocytes. Cell. Immunol. 168:291–296 [DOI] [PubMed] [Google Scholar]
- 43. Takahashi H., et al. 1990. Induction of CD8+ cytotoxic T cells by immunization with purified HIV-1 envelope protein in ISCOMs. Nat. 344:873–875 [DOI] [PubMed] [Google Scholar]
- 44. Tarradas J., et al. 2010. Interferon-gamma induction correlates with protection by DNA vaccine expressing E2 glycoprotein against classical swine fever virus infection in domestic pigs. Vet. Microbiol. 142:51–58 [DOI] [PubMed] [Google Scholar]
- 45. Terpstra C., Wensvoort G. 1988. The protective value of vaccine-induced neutralising antibody titres in swine fever. Vet. Microbiol. 16:123–128 [DOI] [PubMed] [Google Scholar]
- 46. Underdown B. J., Mestecky J. 1994. Mucosal immunoglobulin, p. 79–98 In Strober W., Mestecky J., Lamm M. E., Bienenstock J., Ogra P. L. (ed.), Handbook of mucosal immunology. Academic Press, San Diego, CA [Google Scholar]
- 47. van Gennip H. G. P., Bouma A., van Rijn P. A., Widjojoatmodjo M. N., Moormann R. J. M. 2002. Experimental non-transmissible marker vaccines for classical swine fever (CSF) by transcomplementation of Erns or E2 of CSFV. Vaccine 20:1544–1556 [DOI] [PubMed] [Google Scholar]
- 48. van Zijl M., et al. 1991. Live attenuated pseudorabies virus expressing envelope glycoprotein E1 of hog cholera virus protects swine against both pseudorabies and hog cholera. J. Virol. 65:2761–2765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Winter N., et al. 1995. Recombinant BCG strains expressing the SIV mac-251 nef gene induce proliferative and CTL responses against nef synthetic peptides in mice. Vaccine 13:471–478 [DOI] [PubMed] [Google Scholar]
- 50. Xu Y. G., Li Y. J. 2007. Induction of immune responses in mice after intragastric administration of Lactobacillus casei producing porcine parvovirus VP2 protein. Appl. Environ. Microbiol. 73:7041–7047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Xu Y. G., Li Y. J. 2008. Construction of recombinant Lactobacillus casei efficiently surface displayed and secreted porcine parvovirus VP2 protein and comparison of the immune responses induced by oral immunization. Immunology 124:68–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Zhou F., Rouse B. T., Huang L. 1992. Induction of cytotoxic T lymphocytes in vivo with protein antigen entrapped in membranous vehicles. J. Immunol. 149:1599–1604 [PubMed] [Google Scholar]