Abstract
Virus-specific CD8+ T lymphocytes select for escape mutations in human immunodeficiency virus (HIV) and simian immunodeficiency virus (SIV). To assess the effects of these mutations on viral fitness, we introduced escape mutations into 30 epitopes (bound by five major histocompatibility complex class I [MHC-I] molecules) in three different viruses. Two of these MHC-I alleles are associated with elite control. Two of the three viruses demonstrated reduced fitness in vivo, and 27% of the introduced mutations reverted. These findings suggest that T cell epitope diversity may not be such a daunting problem for the development of an HIV vaccine.
TEXT
Human immunodeficiency virus (HIV) sequence diversity may pose a significant problem for vaccine development. The majority of viral variation outside of the envelope protein is selected for by CD8+ T lymphocytes (1, 36). This sequence variation can either be maintained (18) or revert (2, 20, 21, 31, 41) after transmission to a new host with a disparate major histocompatibility complex class I (MHC-I) haplotype. Unfortunately, reversion has been examined only for a small number of previously studied and well-characterized CD8+ T cell epitopes.
Our group has characterized the peptide-binding properties of several MHC-I molecules (5, 11, 39), mapped CD8+ T lymphocyte epitopes (3, 12, 26, 27, 33, 38), and described viral escape (4, 13, 35, 36) in the Indian rhesus macaque model of immunodeficiency virus infection. We have now systematically identified all of the CD8+ T cell epitopes located within the cloned simian immunodeficiency virus (SIV) SIVmac239 that are restricted by 5 different rhesus macaque MHC-I alleles: Mamu-A1*00101 (3), Mamu-A1*00201 (27), Mamu-A1*01101 (38), Mamu-B*00801 (26), and Mamu-B*01701 (33). We previously infected rhesus macaques with a mutant SIVmac239 virus bearing escape mutations in three of these epitopes (14). The Mamu-A1*00101-restricted Tat28-35SL8 escape mutant was maintained in Mamu-A1*00101-negative macaques. Conversely, escape mutations within two other immunodominant epitopes, the Mamu-A1*00101-restricted Gag181-189CM9 epitope and the Mamu-B*01701-restricted Nef165-173IW9 epitope, reverted to the wild-type sequence in macaques that did not express the selecting alleles (14). In the present study, we sought to broaden these observations in a systematic fashion by examining the reversion characteristics of 30 separate CD8+ T lymphocyte escape mutations in epitopes restricted by five different MHC-I alleles (Table 1).
Table 1.
CD8+ T lymphocyte escape mutations engineered into three separate mutant SIVmac239 viruses
| MHC-I allele | Mutant virus | Epitope | SIVmac239 sequence | Mutant sequencea | Comment code(s)b |
|---|---|---|---|---|---|
| Mamu-A1*00101 | 14x-SIVmac239 | Gag372-379LF8 | LAPVPIPF | - - - G- - - - | 1 |
| Pol625-633SV9 | STPPLVRLV | - - - - - - - -A | 1 | ||
| Vif100-107VI8 | VTPNYADI | - - - - - - -T | 1 | ||
| Tat28-35SL8 | STPESANL | P- - - - - - P | 1 | ||
| Env233-241CL9 | CAPPGYALL | - - - - -FV- - | 1 | ||
| Env620-628TL9 | TVPWPNASL | - - - - - - - -I | 1 | ||
| Env726-735ST10 | SSPPSYFQQT | - - - - - - - - - I | 1 | ||
| Mamu-A1*00201 | 14x-SIVmac239 | Gag71-79GY9 | GSENLKSLY | S-D- - - - - - | 1 |
| Env788-795RY8 | RTLLSRVY | - - - -L- - - | 1 | ||
| Nef159-167YY9 | YTSGPGIRY | - - - - - - - -F | 1 | ||
| Nef221-229YY9 | YTYEAYVRY | H- - - - - - - - | 1 | ||
| Mamu-A1*01101 | 14x-SIVmac239 | Pol92-100AL9 | AERKQREAL | -G- - - - - - - | 1 |
| Env495-502GI8 | GDYKLVEI | - - - -V- - - | 1 | ||
| Nef124-132KI9 | KEKGGLEGI | -Q- - - - - - - | 1 | ||
| Mamu-B*00801 | 11x-SIVmac239 | Vif123-131RL9 | RRAIRGEQL | -K- - - - - - - | 2 |
| Vif172-179RL8 | RRDNRRGL | -G- - - - - - | 2 | ||
| Vpr62-70IF9 | IRILQRALF | -K- - - - - - - | 3 | ||
| Rev12-20KL9 | KRLRLIHLL | -K- - - - - - - | 3 | ||
| Rev44-51RL8 | RRRWQQLL | -K- - - -I- | 2, 3 | ||
| Env573-581KL9 | KRQQELLRL | - - - - - - - -M | 2 | ||
| Env868-876RL9 | RRIRQGLEL | - - - - - - - -R | 4 | ||
| Nef8-16RL9 | RRSRPSGDL | - - - -Q- - - - | 2 | ||
| Nef137-146RL10 | (A)RRHRILDIYL | (P)- - - - - - - - - - | 2, 5 | ||
| Nef245-253RL9 | RRRLTARGL | KK- - - - - - I | 2, 3 | ||
| Nef246-254RL9 | RRLTARGLL | K- - - - - - II | 2 | ||
| Mamu-B*01701 | 5x-SIVmac239 | Vif66-73HW8 | HLEVQGYW | Y- - - - - - - | 6 |
| cRW9 | RHLAFKCLW | - - - - - - - -R | 7 | ||
| Env830-838FW9 | FHEAVQAVW | -Y- - - - - - - | 6 | ||
| Nef165-173IW9 | IRYPKTFGW | T- - - -I- - - | 8 | ||
| Nef195-203MW9 | MHPAQTSQW | V- - - - - - - - | 6 |
Dashes indicate residues identical to the wild-type sequence.
Comments: 1, MHC-I allele-specific variation observed in sequences published in reference 36 and in sequences found in File S1 in the supplemental material; 2, variant published in reference 26; 3, previously unpublished variant discovered during chronic SIVmac239 infection in Mamu-B*00801-positive macaques; 4, variation in Mamu-B*00801 anchor residue observed in an HIV-2 sequence from the Los Alamos National Laboratory online HIV sequence database (www.hiv.lanl.gov); 5, putative processing mutation (extraepitopic variant published in references 22 and 24); 6, variant published in reference 29; 7, cryptic reading frame variant published in reference 28; 8, variant published in reference 16.
Selection of CD8+ T lymphocyte escape mutations.
We began by identifying escape mutations selected for by CD8+ T lymphocytes that recognize epitopes bound by Mamu-A1*00101, Mamu-A1*00201, Mamu-A1*01101, Mamu-B*00801, and Mamu-B*01701. To do this, we utilized previously collected and published viral sequence data obtained from plasma samples taken at the time of death from a large cohort of MHC-I-typed, SIVmac239-infected macaques (36). We also obtained viral sequence data from 19 additional MHC-I-typed, SIVmac239-infected animals to increase the number of Mamu-A1*01101-postive macaques in our analysis. We have included the new sequencing data from these 19 animals in File S1 in the supplemental material. We have also provided a list of all the animals in this study, together with MHC-I typing information, in Table S1 in the supplemental material. We compiled the data to evaluate MHC-I-associated viral mutations within all identified CD8+ T lymphocyte epitopes for the five MHC-I alleles. Putative processing mutations within 3 amino acids of the described minimal epitopes were also included in our analysis. We categorized sequence data into two groups for all 54 animals: animals with and animals without the relevant MHC-I allele. We chose mutations seen exclusively in animals with the MHC-I allele that restricts the T cell response directed against the epitope of interest and not in animals without the selecting allele. In many of the studied epitopes, more than one mutation occurred within the epitope in different animals. For the construction of mutant viruses, we chose to limit the number of mutations to only a single variant per T cell epitope. Some of these variants contained more than one amino acid change, if they were naturally observed in that form within the same animal in our viral sequence data. We selected a single variant for each epitope that exhibited T cell escape based upon the frequency of the variant in animals with the selecting MHC-I allele and/or the presence of a mutation within a key MHC-I anchor residue.
Construction of mutant SIVmac239 viruses.
We created two different viruses bearing mutations in epitopes bound by alleles that are associated with elite control. We developed 11x-SIVmac239, which included mutations found in epitopes bound by Mamu-B*00801 (25), and 5x-SIVmac239, which included mutations found in epitopes bound by Mamu-B*01701 (43) (Table 1). We then created a third virus, 14x-SIVmac239, containing mutations discovered within T cell epitopes restricted by the other three MHC-I alleles, Mamu-A1*00101, Mamu-A1*00201, and Mamu-A1*01101, which are not associated with elite control (Table 1). We did not include an escape mutation within the Mamu-A1*00101-restricted Gag181-189CM9 epitope in the 14x-SIVmac239 virus because of the fitness cost associated with an escape mutation in this epitope (14, 15). We have also already shown that an escape mutation in this epitope reverts after transmission (14).
We built 11x-SIVmac239 in an 8x-SIVmac239 virus backbone (40) using the QuikChange II site-directed mutagenesis kit (Agilent Technologies, Santa Clara, CA) and primers designed to incorporate the appropriate mutations (see Table S2 in the supplemental material). We used 5x-SIVmac239 virus that had been developed for a previous study (42). We had the 14x-SIVmac239 virus synthesized de novo by GeneArt (Regensburg, Germany). We generated each virus by ligation of two plasmids, one encoding the 5′ half of the SIVmac239 provirus and the other encoding the 3′ half. We cotransfected Vero cells with the ligated plasmids containing escape mutations and propagated the resulting virus using a previously described method (14, 40). We amplified each viral stock to high titer in CEMx174 cells. We sequenced each virus following production and verified that the correct mutations were incorporated.
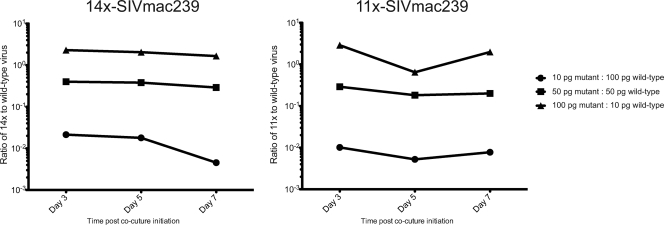
We tested the in vitro fitness of the 11x-SIVmac239 and 14x-SIVmac239 viruses relative to wild-type SIVmac239 using a previously described competition assay (40). The 11x-SIVmac239 and 14x-SIVmac239 viruses both demonstrated fitness similar to the wild-type virus in a 7-day in vitro competition assay (Fig. 1). An in vitro competition assay using 5x-SIVmac239 also did not reveal a fitness deficit (42).
Fig. 1.
In vitro viral fitness of 14x-SIVmac239 and 11x-SIVmac239 mutant viruses. We inoculated each mutant virus and wild-type SIVmac239 into cultures of concanavalin A-activated CD8-depleted peripheral blood mononuclear cell (PBMC) targets at the indicated ratio of mutant virus to wild-type virus (1:10, 1:1, or 10:1). We then harvested virus-containing supernatant at each time point indicated and quantified the proportion of each viral species by quantitative reverse transcription-PCR. The complete method, including primers used for quantitative PCR, has been described previously (40). Both mutant-inoculated cultures displayed relatively consistent ratios of wild-type to mutant virus over the 7 days of the assay, suggesting no in vitro fitness deficit or advantage for the introduced mutations. In vitro analysis of the 5x-SIVmac239 virus has been published previously (42).
Infection of macaques with mutant SIVmac239 viruses.
We infected three separate groups of four Indian rhesus macaques intravenously with each of our mutant SIVmac239 viruses. None of these animals expressed the relevant MHC-I alleles that had been involved in the selection of the escape mutants (see Table S3 in the supplemental material). We monitored viral loads in these animals using a previously published method (23) that can reproducibly detect viral loads of ≥30 viral RNA copies per ml of plasma. None of the introduced mutations affected the region of the virus detected by the primers in our viral load assay.
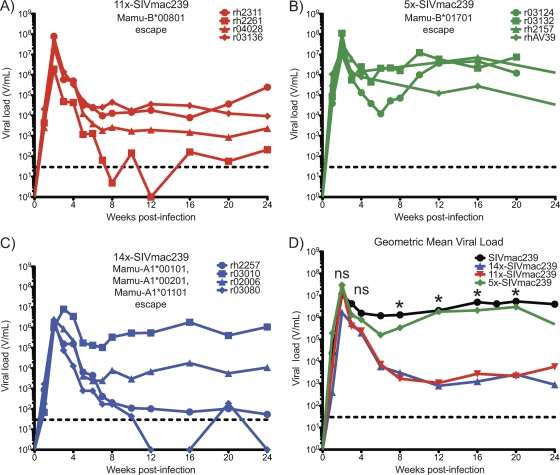
To our surprise we discovered that, despite apparent fitness in vitro, the viruses 14x-SIVmac239 (containing Mamu-A1*00101, Mamu-A1*00201, and Mamu-A1*01101 escape mutations) and 11x-SIVmac239 (containing Mamu-B*00801 escape mutations) did not replicate as well as wild-type SIVmac239 in vivo (Fig. 2C and A). Geometric mean viral loads during chronic infection in animals infected with these two viruses were more than 2 log10 lower than the geometric mean viral load of SIVmac239-infected historical controls (Fig. 2D). In contrast, viral loads in animals infected with 5x-SIVmac239 (containing Mamu-B*01701 escape mutations) (Fig. 2B) were indistinguishable from those in wild-type SIVmac239-infected animals (Fig. 2D). The discrepancy between apparent fitness levels of the 14x-SIVmac239 and 11x-SIVmac239 viruses in vitro and in vivo underscores the limitations of short-term in vitro viral fitness assays, including growth competition assays. Such short-term assays (7 days in this case) cannot be relied upon to quantify the potential impact mutations may have upon viral fitness over the course of many months in a host organism.
Fig. 2.
Viral loads following mutant SIVmac239 virus infection. We infected four rhesus macaques with each of the indicated viruses. We measured viral loads with a previously described method (23). Viral loads of ≥30 viral RNA copies per ml of plasma (V/ml; dashed lines) can be reliably quantified using this method. (A to D) 11x-SIVmac239 (carrying Mamu-B*00801-restricted T cell epitope mutations) (A) and 14x-SIVmac239 (carrying Mamu-A1*00101-, Mamu-A1*00201-, and Mamu-A1*01101-restricted T cell epitope mutations) (C) do not replicate in vivo as well as 5x-SIVmac239 (carrying Mamu-B*01701-restricted T cell epitope mutations) (B) and wild-type SIVmac239 (D). (D) Geometric mean viral loads were calculated for each group of infected animals (n = 4) and wild-type SIVmac239-infected historical controls (n = 33). A Kruskal-Wallis test was performed with Dunn's multiple-comparison posttest comparing viral loads at the indicated time points postinfection among all wild-type SIVmac239-infected animals and each of the three mutant virus-infected groups of animals. Significant differences were discovered at weeks 8, 12, 16, and 20 postinfection in comparisons of 11x-SIVmac239-infected animals to wild-type SIVmac239-infected animals and of 14x-SIVmac239-infected animals to wild-type SIVmac239-infected animals (ns, not significant; *, P < 0.05). No significant differences were detected between 5x-SIVmac239- and wild-type SIVmac239-infected animals.
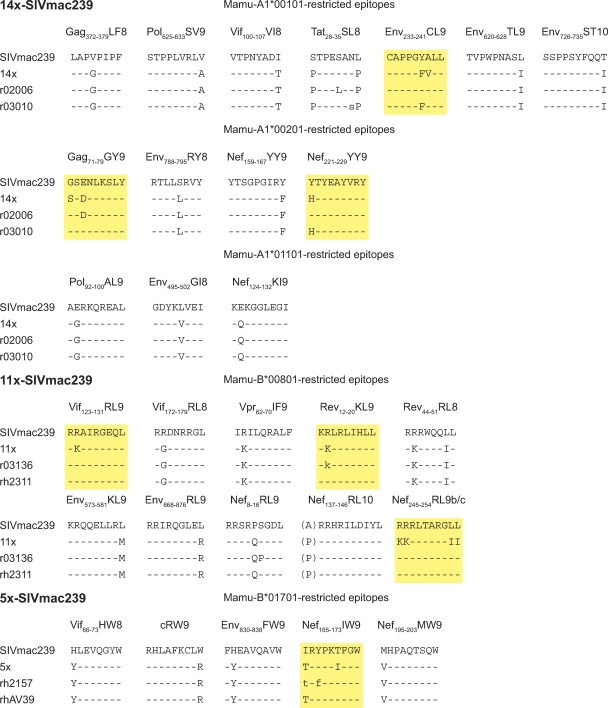
We next evaluated the stability of the introduced mutations. We sequenced plasma virus samples from two animals in each group at approximately 26 weeks postinfection. We discovered that 3 of 14 epitopes (21%) with mutations in 14x-SIVmac239, 4 of 11 epitopes (36%) with mutations in 11x-SIVmac239, and 1 of 5 epitopes (20%) with mutations in 5x-SIVmac239 reverted, at least in part, to the wild-type sequence (Fig. 3). It is possible that the proportion of these epitopes that revert may actually be higher than 8 of 30 (27%); however, our experiment was limited by low viral loads in two of the 11x-SIVmac239- and two of the 14x-SIVmac239-infected animals. In addition, permitting the animals to progress beyond 6 months may have allowed for the detection of additional reversion. Therefore, the measured rate of reversion (27%) in our experiment is likely a conservative estimate of the actual rate of reversion for these 30 variant epitopes were the experiment continued until pathological sequelae developed. Taken together, these data suggest that a substantial proportion of all CD8+ T lymphocyte escape mutations which develop in SIVmac239, as represented by the 30 selected by these five MHC-I alleles, revert in vivo in the absence of the selecting allele.
Fig. 3.
Plasma virus sequence. We selected two animals with high viral loads from each group for viral sequencing. Plasma virus samples from r02006, r03010, r03136, and rh2311 were sequenced approximately 26 weeks postinfection using whole-SIVmac239-genome Roche 454 sequencing (7). Mixed-base annotation indicates viral mutations encompassing more than 30% of total viral quasispecies. Capital-letter annotation indicates a mutation encompassing more than 70% of viral quasispecies. rh2157 and rhAV39 samples were sequenced using standard viral Sanger sequencing methods (22) at approximately 28 weeks postinfection. Reverting mutations are noted in yellow boxes. The Mamu-B*00801-restricted Nef245-254RL9 epitope encompasses two overlapping T cell epitopes (Table 1), both containing mutations that reverted. Dashes indicate residues identical to the wild-type sequence.
To understand the potential relevance of our model system to the study of reversion in HIV isolates, it is important to discuss the origins of the SIVmac239 clonal virus. SIVmac239 (34) was cloned from infected cells that had been inoculated with various tissues from a rhesus macaque, Mm239-82, with simian AIDS (10). Prior to the infection of Mm239-82, the ancestral virus from which SIVmac239 originated was passaged through at least 7 other rhesus macaque hosts (17, 30). Therefore, SIVmac239 may be most analogous to a clonal HIV type 1 (HIV-1) isolate obtained early in the HIV-1 pandemic. Indeed, the immunodominant Tat28-35SL8 epitope is intact in clonal SIVmac239, yet this epitope quickly escapes in animals expressing the high-frequency Mamu-A1*00101 allele (expressed in 27% of captive rhesus macaques) via mutations that are maintained after transmission.
The relatively high frequency of escape mutation reversion that we detected in this experiment suggests that some CD8+ T cell populations can target regions of the virus where mutations affect viral fitness. Because SIVmac239 likely represents a very early isolate after cross-species transmission of an immunodeficiency virus from its natural to a nonnatural host, many epitopes are still intact. This may not be the case in individuals infected with HIV today. Previous passage of today's viral isolates through many different individuals that express various HLA class I alleles may have left us with a preponderance of reverting epitopes rather than epitopes that do not revert. However, the creation of de novo epitopes from the buildup of nonreverting mutations and the selection of disparate escape mutations at the same residue by different MHC-I alleles may limit the frequency of reverting epitopes at the population level (6). Nevertheless, we suggest that the frequency of CD8+ T lymphocyte escape mutation reversion relative to maintenance in currently circulating HIV-1 isolates that have undergone many transmission cycles may be higher than our conservative measurement of 27%.
Compensatory mutations can promote replication of viruses bearing T cell escape mutations that, in isolation, diminish viral replication capacity (8, 9, 15, 19, 32, 37). Unfortunately, associations between potential compensatory mutations and specific T lymphocyte escape mutations are difficult to establish in the setting of limited sequence data (15, 19). For most mutations characterized in this study, only 1 to 5 individual animals harbored viruses that contained the mutation. This makes the establishment of connections between viral escape patterns and specific compensatory mutations impossible or nearly impossible. Only a single rhesus macaque T cell epitope in SIVmac239 with known compensatory mutations exists (15). It is possible that some of the mutations we have characterized as reverting in the present study may have associated compensatory mutations that remain undefined at this time.
It is notable that reverting CD8+ T lymphocyte escape mutations were selected by the two MHC-I alleles associated with elite control of SIVmac239 replication, Mamu-B*00801 and Mamu-B*01701. Four of 11 Mamu-B*00801-restricted T cell epitopes in the 11x-SIVmac239 virus and 1 of 5 Mamu-B*01701-restricted T cell epitopes in the 5x-SIVmac239 virus reverted to the wild-type sequence after inoculation of the viruses into animals that did not express these alleles. In addition, we had previously observed reversion of the mutation introduced into the Mamu-B*00801-restricted epitope Env573-581KL9 in a single Mamu-B*00801-negative animal in a separate study (40). Therefore, in total, 38% of mutations (6 of 16) introduced into epitopes restricted by these two rhesus macaque MHC-I alleles reverted in the absence of the selecting MHC-I allele.
None of the viruses in this study were designed to completely mimic naturally occurring escape mutant viruses in SIVmac239-infected rhesus macaques. Instead, we desired to create a model system to measure the effects of escape mutations within epitopes restricted by these five MHC-I alleles. Therefore, it is not surprising that two of the three viruses developed for this study did not appear to be fit in vivo. Of interest, the 5x-SIVmac239 virus containing Mamu-B*01701-restricted T cell epitope escape mutations was the only mutant virus in this study with fitness comparable to that of wild-type SIVmac239 in vivo. Mutations in 11 or 14 T cell epitopes, regardless of the restricting MHC-I allele, affected in vivo viral fitness more than the 5 mutations restricted by the protective MHC-I allele Mamu-B*01701. This suggests an additive effect of multiple CD8+ T lymphocyte escape mutations upon viral fitness in the absence of compensatory mutations. In addition, at least with regard to Mamu-B*01701, escape mutations found in T cell epitopes restricted by a rhesus macaque allele associated with elite control do not affect viral fitness.
To summarize, in our study 27% of CD8+ T lymphocyte escape mutations found in SIVmac239-infected rhesus macaques (32% if mutations in Gag181-189CM9 [14] and Env573-581KL9 [40] are included) reverted after transmission to hosts without the selecting MHC-I allele. The measured frequency of reverting mutations may increase with multiple viral transmission cycles through hosts with diverse MHC-I alleles, as nonreverting T cell epitope variants become the new consensus sequence. This suggests that CD8+ T lymphocyte-selected HIV diversity may be limited by substitutions that revert in the absence of selecting pressure.
One of the major concerns in developing an HIV vaccine is the immense diversity and seemingly endless evolution of viral sequences. Our data from the SIV-infected Indian rhesus macaque model suggest that almost a third of T cell epitopes will be naturally preserved as vaccine targets. These mutations revert in the absence of selecting pressure after transmission to a new host. Therefore, vaccines containing consensus sequences that span the epitopes in which reversion is observed should be effective in inducing useful CD8+ T cell responses. A carefully designed vaccine containing such targets may overcome the problem of T cell-selected HIV-1 diversity.
Supplementary Material
Acknowledgments
This work was supported by National Institutes of Health (NIH) grants R37 AI052056, R01 AI049120, R01 AI076114, R24 RR015371, R24 RR016038, and R21 AI081590 to D.I.W. This publication was made possible in part by grant number P51 RR000167 from the National Center for Research Resources (NCRR), a component of the NIH, to the Wisconsin National Primate Research Center, University of Wisconsin—Madison.
This publication's contents are solely the responsibility of the authors and do not necessarily represent the official views of the NCRR or the NIH.
Footnotes
Supplemental material for this article may be found at http://jvi.asm.org/.
Published ahead of print on 28 September 2011.
REFERENCES
- 1. Allen T. M., et al. 2005. Selective escape from CD8+ T-cell responses represents a major driving force of human immunodeficiency virus type 1 (HIV-1) sequence diversity and reveals constraints on HIV-1 evolution. J. Virol. 79:13239–13249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Allen T. M., et al. 2004. Selection, transmission, and reversion of an antigen-processing cytotoxic T-lymphocyte escape mutation in human immunodeficiency virus type 1 infection. J. Virol. 78:7069–7078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Allen T. M., et al. 2001. CD8+ lymphocytes from simian immunodeficiency virus-infected rhesus macaques recognize 14 different epitopes bound by the major histocompatibility complex class I molecule Mamu-A*01: implications for vaccine design and testing. J. Virol. 75:738–749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Allen T. M., et al. 2000. Tat-specific cytotoxic T lymphocytes select for SIV escape variants during resolution of primary viraemia. Nature 407:386–390 [DOI] [PubMed] [Google Scholar]
- 5. Allen T. M., et al. 1998. Characterization of the peptide binding motif of a rhesus MHC class I molecule (Mamu-A*01) that binds an immunodominant CTL epitope from simian immunodeficiency virus. J. Immunol. 160:6062–6071 [PubMed] [Google Scholar]
- 6. Allen T. M., et al. 2005. De novo generation of escape variant-specific CD8+ T-cell responses following cytotoxic T-lymphocyte escape in chronic human immunodeficiency virus type 1 infection. J. Virol. 79:12952–12960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bimber B. N., et al. 2010. Whole-genome characterization of human and simian immunodeficiency virus intrahost diversity by ultradeep pyrosequencing. J. Virol. 84:12087–12092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Brockman M. A., et al. 2007. Escape and compensation from early HLA-B57-mediated cytotoxic T-lymphocyte pressure on human immunodeficiency virus type 1 Gag alter capsid interactions with cyclophilin A. J. Virol. 81:12608–12618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Crawford H., et al. 2007. Compensatory mutation partially restores fitness and delays reversion of escape mutation within the immunodominant HLA-B*5703-restricted Gag epitope in chronic human immunodeficiency virus type 1 infection. J. Virol. 81:8346–8351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Daniel M. D., et al. 1985. Isolation of T-cell tropic HTLV-III-like retrovirus from macaques. Science 228:1201–1204 [DOI] [PubMed] [Google Scholar]
- 11. Dzuris J. L., et al. 2000. Conserved MHC class I peptide binding motif between humans and rhesus macaques. J. Immunol. 164:283–291 [DOI] [PubMed] [Google Scholar]
- 12. Evans D. T., et al. 2000. Definition of five new simian immunodeficiency virus cytotoxic T-lymphocyte epitopes and their restricting major histocompatibility complex class I molecules: evidence for an influence on disease progression. J. Virol. 74:7400–7410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Evans D. T., et al. 1999. Virus-specific cytotoxic T-lymphocyte responses select for amino-acid variation in simian immunodeficiency virus Env and Nef. Nat. Med. 5:1270–1276 [DOI] [PubMed] [Google Scholar]
- 14. Friedrich T. C., et al. 2004. Reversion of CTL escape-variant immunodeficiency viruses in vivo. Nat. Med. 10:275–281 [DOI] [PubMed] [Google Scholar]
- 15. Friedrich T. C., et al. 2004. Extraepitopic compensatory substitutions partially restore fitness to simian immunodeficiency virus variants that escape from an immunodominant cytotoxic-T-lymphocyte response. J. Virol. 78:2581–2585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Friedrich T. C., et al. 2004. Consequences of cytotoxic T-lymphocyte escape: common escape mutations in simian immunodeficiency virus are poorly recognized in naive hosts. J. Virol. 78:10064–10073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gardner M. B. 1996. The history of simian AIDS. J. Med. Primatol. 25:148–157 [DOI] [PubMed] [Google Scholar]
- 18. Kawashima Y., et al. 2009. Adaptation of HIV-1 to human leukocyte antigen class I. Nature 458:641–645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kelleher A. D., et al. 2001. Clustered mutations in HIV-1 gag are consistently required for escape from HLA-B27-restricted cytotoxic T lymphocyte responses. J. Exp. Med. 193:375–386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Leslie A. J., et al. 2004. HIV evolution: CTL escape mutation and reversion after transmission. Nat. Med. 10:282–289 [DOI] [PubMed] [Google Scholar]
- 21. Li B., et al. 2007. Rapid reversion of sequence polymorphisms dominates early human immunodeficiency virus type 1 evolution. J. Virol. 81:193–201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Loffredo J. T., et al. 2008. Patterns of CD8+ immunodominance may influence the ability of Mamu-B*08-positive macaques to naturally control simian immunodeficiency virus SIVmac239 replication. J. Virol. 82:1723–1738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Loffredo J. T., et al. 2007. The antiviral efficacy of simian immunodeficiency virus-specific CD8+ T cells is unrelated to epitope specificity and is abrogated by viral escape. J. Virol. 81:2624–2634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Loffredo J. T., et al. 2007. CD8+ T cells from SIV elite controller macaques recognize Mamu-B*08-bound epitopes and select for widespread viral variation. PLoS One 2:e1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Loffredo J. T., et al. 2007. Mamu-B*08-positive macaques control simian immunodeficiency virus replication. J. Virol. 81:8827–8832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Loffredo J. T., et al. 2009. Two MHC class I molecules associated with elite control of immunodeficiency virus replication, Mamu-B*08 and HLA-B*2705, bind peptides with sequence similarity. J. Immunol. 182:7763–7775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Loffredo J. T., et al. 2004. Identification of seventeen new simian immunodeficiency virus-derived CD8+ T cell epitopes restricted by the high frequency molecule, Mamu-A*02, and potential escape from CTL recognition. J. Immunol. 173:5064–5076 [DOI] [PubMed] [Google Scholar]
- 28. Maness N. J., et al. 2007. AIDS virus specific CD8+ T lymphocytes against an immunodominant cryptic epitope select for viral escape. J. Exp. Med. 204:2505–2512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Maness N. J., et al. 2008. Comprehensive immunological evaluation reveals surprisingly few differences between elite controller and progressor Mamu-B*17-positive simian immunodeficiency virus-infected rhesus macaques. J. Virol. 82:5245–5254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mansfield K. G., Lerch N. W., Gardner M. B., Lackner A. A. 1995. Origins of simian immunodeficiency virus infection in macaques at the New England Regional Primate Research Center. J. Med. Primatol. 24:116–122 [DOI] [PubMed] [Google Scholar]
- 31. Matthews P. C., et al. 2008. Central role of reverting mutations in HLA associations with human immunodeficiency virus set point. J. Virol. 82:8548–8559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Miura T., et al. 2009. HLA-associated viral mutations are common in human immunodeficiency virus type 1 elite controllers. J. Virol. 83:3407–3412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mothe B. R., et al. 2002. Characterization of the peptide-binding specificity of Mamu-B*17 and identification of Mamu-B*17-restricted epitopes derived from simian immunodeficiency virus proteins. J. Immunol. 169:210–219 [DOI] [PubMed] [Google Scholar]
- 34. Naidu Y. M., et al. 1988. Characterization of infectious molecular clones of simian immunodeficiency virus (SIVmac) and human immunodeficiency virus type 2: persistent infection of rhesus monkeys with molecularly cloned SIVmac. J. Virol. 62:4691–4696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. O'Connor D. H., et al. 2002. Acute phase cytotoxic T lymphocyte escape is a hallmark of simian immunodeficiency virus infection. Nat. Med. 8:493–499 [DOI] [PubMed] [Google Scholar]
- 36. O'Connor D. H., et al. 2004. A dominant role for CD8+-T-lymphocyte selection in simian immunodeficiency virus sequence variation. J. Virol. 78:14012–14022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Schneidewind A., et al. 2009. Transmission and long-term stability of compensated CD8 escape mutations. J. Virol. 83:3993–3997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sette A., et al. 2005. Characterization of the peptide-binding specificity of Mamu-A*11 results in the identification of SIV-derived epitopes and interspecies cross-reactivity. Immunogenetics 57:53–68 [DOI] [PubMed] [Google Scholar]
- 39. Sidney J., et al. 2000. Definition of the Mamu A*01 peptide binding specificity: application to the identification of wild-type and optimized ligands from simian immunodeficiency virus regulatory proteins. J. Immunol. 165:6387–6399 [DOI] [PubMed] [Google Scholar]
- 40. Valentine L. E., et al. 2009. Infection with “escaped” virus variants impairs control of simian immunodeficiency virus SIVmac239 replication in Mamu-B*08-positive macaques. J. Virol. 83:11514–11527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wang Y. E., et al. 2009. Protective HLA class I alleles that restrict acute-phase CD8+ T-cell responses are associated with viral escape mutations located in highly conserved regions of human immunodeficiency virus type 1. J. Virol. 83:1845–1855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Weinfurter J. T., et al. 2011. Macaque long-term nonprogressors resist superinfection with multiple CD8+ T cell escape variants of simian immunodeficiency virus. J. Virol. 85:530–541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Yant L. J., et al. 2006. The high-frequency major histocompatibility complex class I allele Mamu-B*17 is associated with control of simian immunodeficiency virus SIVmac239 replication. J. Virol. 80:5074–5077 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.