Abstract
Background
The study evaluated the efficacy of an indicated prevention program for adolescent depression.
Methods
Fifty-seven adolescents with elevated depression symptoms were randomized to receive Interpersonal Psychotherapy-Adolescent Skills Training (IPT-AST) or school counseling (SC). Hierarchical linear modeling examined differences in rates of change in depression symptoms and overall functioning and analysis of covariance examined mean differences between groups. Rates of depression diagnoses in the 18-month follow-up period were compared.
Results
Adolescents in IPT-AST reported significantly greater rates of change in depression symptoms and overall functioning than SC adolescents from baseline to post-intervention. At post-intervention, IPT-AST adolescents reported significantly fewer depression symptoms and better overall functioning. During the follow-up phase, rates of change slowed for the IPT-AST adolescents, whereas the SC adolescents continued to show improvements. By 12-month follow-up, there were no significant mean differences in depression symptoms or overall functioning between the two groups. IPT-AST adolescents reported significantly fewer depression diagnoses in the first 6 months following the intervention but by 12-month follow-up the difference in rates of diagnoses was no longer significant.
Conclusions
IPT-AST leads to an immediate reduction in depression symptoms and improvement in overall functioning. However, the benefits of IPT-AST are not consistent beyond the 6-month follow-up, suggesting that the preventive effects of the program in its current format are limited. Future studies are needed to examine whether booster sessions lengthen the long-term effects of IPT-AST.
Keywords: prevention, adolescents, depression
INTRODUCTION
Adolescent depression is associated with significant impairment.[1] Few depressed adolescents receive services and those that do receive services may not improve.[2] This has led to an interest in developing preventive interventions, particularly programs that can be delivered in schools.[3] Preventive interventions are classified as universal, selective, and indicated.[4] Indicated interventions target individuals with subthreshold depression, one of the biggest risk factors for developing a disorder.[5] These symptoms persist over time[6] and are associated with psychosocial impairment.[7]
A number of indicated depression interventions have been developed and tested. The programs that have received the most evaluation are the Penn Resiliency Program (PRP)[8–10] and the Coping with Stress Program (CWS).[11–13] Recent meta-analyses of depression prevention studies have found small to moderate effect sizes for indicated programs at post-intervention and follow-up.[14–15] Given the magnitude of these effects, additional preventive interventions are worth developing.
Based on the need for innovative indicated programs, we developed Interpersonal Psychotherapy-Adolescent Skills Training (IPT-AST).[16] IPT-AST is a group intervention based on Interpersonal Psychotherapy for Depressed Adolescents (IPT-A).[17] The rationale for developing IPT-AST came from the positive IPT-A findings[18–19] and the research on risk and protective factors for depression. Research indicates that interpersonal conflict increases the risk for depression[20] and positive relationships protect against the development of depression.[21] These findings highlight the value of a preventive intervention that develops interpersonal skills to address problematic relationships and promote positive ones.
In a small initial study, adolescents in IPT-AST reported significantly fewer depressive symptoms, better overall functioning, and fewer depression diagnoses than adolescents who received school counseling (SC) post-intervention and at 6-month follow-up.[22] Horowitz et al. compared IPT-AST, CWS, and a no intervention control in a universal sample. At post-intervention, IPT-AST and CWS adolescents reported significantly lower levels of depressive symptoms than the control group; the two interventions did not differ significantly from each other. There were no significant differences between the three conditions at 6-month follow-up.[23]
INVOLVING PARENTS
Within the depression prevention literature, only two studies have included parents.[24–25] In a study of the Resourceful Adolescent Program, the addition of the parent sessions did not produce stronger preventive effects than the Resourceful Adolescent Program alone but parental attendance in the study was poor, with only 36% of parents attending at least one session.[24] Another study examined the feasibility of including parents in PRP and found that parents attended an average of 63% of sessions.[25] PRP adolescents reported better outcomes than the no intervention control, however, without an adolescent only condition, the specific benefit of involving parents is unclear. More research is needed on the feasibility and potential benefits of including parents in school-based depression prevention programs.[26]
This study presents results from a randomized trial comparing IPT-AST and SC. We hypothesized there would be significantly different rates of change in depressive symptoms and overall functioning between adolescents in IPT-AST and those in SC. We also anticipated different rates of depression disorders in the intervention conditions. As a supplemental goal, we assessed the feasibility of involving parents in IPT-AST.
METHODS
CASE-FINDING PROCEDURES
Screening
Adolescents with elevated symptoms of depression were identified through a two-stage screening procedure. Recruitment began in November 2005 and ended in February 2007. The first stage was a classroom-based screening in three single-sex high schools, two girls’ schools and one boys’ school. Parents of students in the 9th and 10th grades were sent a letter about the screening from school administrators. Parents sent back a notice of refusal if they did not want their child to participate. If we did not receive a refusal, another letter was sent, giving parents two opportunities to refuse participation. On the day of the screening, adolescents were informed of the procedures and those who wanted to participate signed a screening assent form. Three hundred forty-six (31.0%) parents and 125 (11.2%) adolescents refused to participate in the screening; 4 adolescents were repeatedly absent so were not screened.
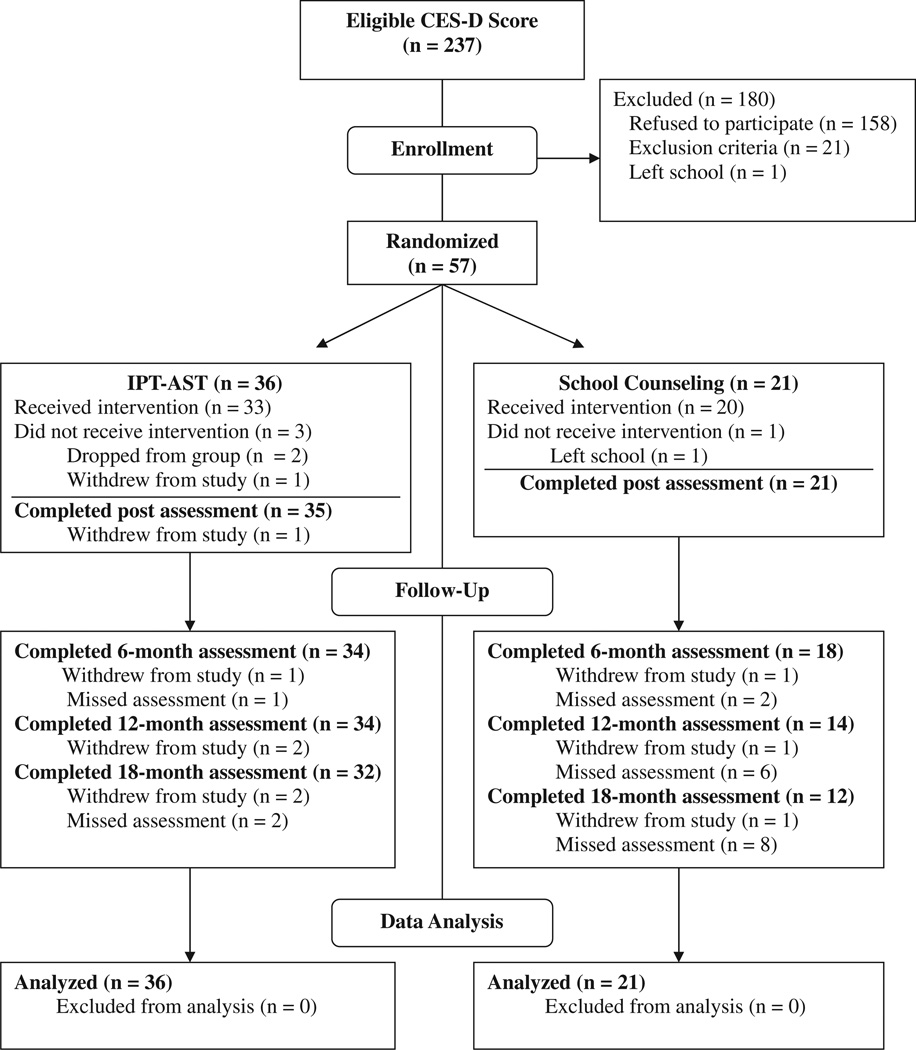
The screening consisted of the Center for Epidemiologic Studies-Depression Scale (CES-D),[27] a 20-item measure that assesses depressive symptoms over the past week. Adolescents with a CES-D score between 16 and 39 were eligible to be approached for the prevention project; those with a score of 40 or higher were seen by the Principal Investigator (PI) to assess clinical severity and determine potential eligibility. The average CES-D score of the 642 adolescents was 15.23 (SD = 10.27); 235 adolescents scored between 16 and 39. Two adolescents scored above 40 but did not meet criteria for depression in the assessment with the PI. The eligible adolescents and their parents were contacted by the research staff to describe the prevention project. Interested families came to the school to learn about the project and provide informed consent and assent. A third of families (N = 79) agreed to participate in an eligibility evaluation and the prevention program. The two most common reasons for refusing to participate were disinterest on the part of the adolescent (25.6%), parents (11.6%) or both (13.9%), and lack of perceived need (30.2%). There were no significant differences in age (14.42 versus 14.34; t(235) = −0.86) or gender (57.0% female versus 62.0% female; χ2 =.45) between those adolescents who consented to participate and those who did not. However, there was a significant difference on screening CES-D score (26.37 versus 22.83; t(235) = −4.10, p < .01); adolescents who agreed to participate had higher depression scores (Figure 1).
Figure 1.
Study flow chart.
Diagnostic evaluation
Adolescents who consented to the project completed the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS-PL)[28] and the Children’s Global Assessment Scale (CGAS)[29] to determine eligibility. Adolescents were eligible if they had at least two subthreshold or threshold depression symptoms on the K-SADS-PL, did not meet criteria for a current depressive episode, and had a CGAS score of 61 or higher. Adolescents were excluded from the study if they had a current diagnosis of depression, dysthymia, bipolar disorder, psychosis, panic disorder, obsessive–compulsive disorder, posttraumatic stress disorder, oppositional defiant disorder, conduct disorder, or untreated attention deficit hyperactivity disorder. Four adolescents were excluded because they did not have enough depression symptoms; 10 because of a current depression diagnosis, suicidal ideation or self-harm behaviors; 7 adolescents met criteria for one of the exclusionary diagnoses.
Randomization
Fifty-seven adolescents were randomly assigned to receive IPT-AST or SC using a table of random numbers. To ensure enough adolescents in the IPT-AST groups, the random number table was generated so that approximately two-thirds of adolescents in each school would be randomized to IPT-AST. Thirty-six adolescents were randomized to IPT-AST and 21 to SC. Each of the schools was randomized to include parents in IPT-AST during either the first or second year of the study. Twenty-one adolescents received IPT-AST without parental involvement and 15 received IPT-AST with parent involvement.
PARTICIPANTS
Participants were aged 13–17 in the 9th and 10th grades. The average age was 14.51 (SD = 0.76) years and the sample was 59.7% female. A majority of the adolescents (73.7%) identified themselves as Hispanic and lived in single-parent homes (70.2%). Several of the adolescents met criteria for a current nonaffective DSM-IV diagnosis, but the majority (82.5%) had only subthreshold depression symptoms with no current diagnosis (see Table 1). Four adolescents had a past diagnosis of major depression or dysthymia (two in each condition). None of these adolescents had received prior treatment.
TABLE 1.
Demographic and sample characteristics
| IPT-AST (N = 36) |
SC (N = 21) | p-value | |
|---|---|---|---|
| Demographics | |||
| Age, mean (SD) | 14.57 (0.68) | 14.52 (0.87) | 0.84 |
| Female (%) | 20 (55.6) | 14 (66.7) | 0.41 |
| Hispanic (%) | 25 (69.4) | 17 (80.9) | 0.34 |
| African American (%) | 15 (41.7) | 7 (33.3) | 0.53 |
| Baseline measures | |||
| CES-D, mean (SD) | 26.56 (6.72) | 26.05 (5.86) | 0.69 |
| CGAS, mean (SD) | 70.75 (4.12) | 70.10 (6.11) | 0.55 |
| CDRS-R, mean (SD) | 51.75 (11.17) | 48.43 (5.67) | 0.25 |
| Current diagnoses | |||
| No diagnosis (%) | 29 (80.6) | 18 (85.7) | 0.73 |
| DD NOS (%) | 1 (2.8) | 1 (4.8) | 1.00 |
| Adjustment (%) | 2 (5.6) | 1 (4.8) | 1.00 |
| GAD (%) | 1 (2.8) | 0 (0.0) | 1.00 |
| Specific phobia (%) | 2 (5.6) | 1 (4.8) | 1.00 |
| Tic disorder (%) | 1 (2.8) | 0 (0.0) | 1.00 |
Note: IPT-AST = Interpersonal Psychotherapy-Adolescent Skills Training; SC = school counseling.
ASSESSMENTS
Adolescents completed assessments at baseline, post-intervention, and at 6-, 12-, and 18-month post-intervention. Adolescents also completed the CES-D mid-intervention. Each assessment consisted of the K-SADS-PL, CGAS, CES-D, and the Children’s Depression Rating Scale-Revised (CDRS-R).[30] Adolescents were given $15 for completing each assessment. The CDRS-R is a 17-item clinician-rated instrument of depressive symptoms. The total score is converted to a t score, with higher scores indicating more symptoms. At each of the follow-up assessments, the Longitudinal Interval Follow-up Evaluation[31] was used in conjunction with the K-SADS-PL to provide more accurate information about disorders since the last assessment.
The evaluations were conducted by independent evaluators (IEs), Masters-level psychologists or social workers, who were blind to intervention condition. The IEs were trained in the assessments and participated in a reliability study of eight audiotaped assessments. Reliability for depression diagnoses on the K-SADS-PL was high (ICC = .89), as was inter-rater reliability for the CGAS (ICC = .98) and CDRS-R (ICC = .99). Each IE was asked to guess participants’ intervention assignment. Correct classification rates ranged from 42.9% (95% CI: 26.5–59.3%) to 58.8% (95% CI: 35.4–82.2%), providing no indication that the blind was broken.
INTERVENTIONS
IPT-AST
IPT-AST involves two pre-group sessions and eight 90 minute group sessions. During the post-group sessions, the leader meets with each adolescent to assess depressive symptoms, provide a framework for the group, and conduct the interpersonal inventory to identify specific interpersonal goals for the group. In the group, adolescents learn about the symptoms of depression, discuss the relationship between feelings and interpersonal interactions, and learn different communication and interpersonal strategies to apply to relationships in their lives. In the groups with parent involvement, the parents participate in one of the pre-group sessions, a mid-group parent–adolescent session to work on a particular interpersonal issue, and a post-group parent–adolescent session to review progress made and highlight additional work to be done. If a parent was unable to attend a session, the adolescent met alone with the leader.
Individual sessions occurred during students’ free periods or after school and the group sessions took place after school. Four IPT-AST groups without parental involvement and three IPT-AST groups with parental involvement were conducted over the course of 2 years. The first author co-led two of the groups. The remaining co-leaders were masters or doctoral level psychologists or child psychiatrists who were trained and supervised by the first author. Group size ranged from four to six adolescents. One adolescent in IPT-AST continued ongoing family counseling at a community mental health center during the intervention and follow-up. Three additional adolescents met with the school counselor during the follow-up period.
School counseling
The remaining adolescents were referred to the school counselor to be seen at a frequency determined by the adolescent and the counselor. SC was not intended to be an equivalent intervention to IPT-AST. It was chosen as the comparison group because it approximates what normally occurs in the schools when an adolescent is identified as having mild emotional difficulties. We were interested in whether IPT-AST was more effective than the counseling that normally occurs in these schools. The SC sessions were 30–45 minutes in duration and consisted of supportive individual counseling. The most commonly discussed topics in sessions were relationships with parents (35.1%) and academic issues (24.3%). A variety of other topics (e.g., stress, peer relations, extracurricular activities) were also discussed. One adolescent was hospitalized for several weeks for depression during the follow-up period and subsequently withdrew from the study. Five additional adolescents reported seeing the school counselor during the follow-up.
STATISTICAL ANALYSES
Tests of baseline differences in demographic and clinical characteristics were investigated using t-tests for continuous variables and χ2 tests for categorical variables. The Institute of Medicine recommends several approaches, including hierarchical models, to maximize information from small trials and increase statistical power.[32] Based on this recommendation, we used hierarchical linear modeling (HLM) to examine differences between the interventions on rates of change in depression and functioning. Like other investigators (e.g., Keller et al.[33]), we conducted a piecewise model looking at change from baseline to post-intervention and a second leg of time looking at post-intervention through the 18-month follow-up. The degrees of freedom were estimated with the Kenward–Roger’s approximation[34] which accommodates small sample inferences, and effect sizes (Cohen’s d) were derived as specified by Verbeke and Molenberghs.[35] To control for potential differences across schools, school was included in the models as a fixed effect. HLM models permit missing data and can fit individual trajectories over time even if time points are missing or unevenly spaced. However, the method assumes that data are missing at random and these missing data do not impact or bias the intervention effects.[36] We used pattern-mixture models[37] to assess whether intervention effects were dependent on missing data patterns. These pattern-mixture models indicated that the intervention effects were not sensitive to the missing data present in the HLM analyses.
We used analysis of covariance (ANCOVA) to examine mean differences between the intervention conditions at post-intervention and follow-up, controlling for baseline scores and school. For participants with missing data, we imputed missing data based on the last available observation. Effect sizes (Cohen’s d) were estimated as the standardized mean difference between groups, adjusted for baseline assessment and school. Both HLM and ANCOVA assume independent observations between individuals. This assumption may be violated because IPT-AST is a group program. We considered including random effects for group but decided against this model because the number of groups and small sample size resulted in statistically unreliable estimates, as evident by a lack of convergence of the statistical algorithms.
Rates of depression diagnoses on the K-SADS were compared using Fisher’s Exact Test. The significance level for all tests was 0.05 (two sided). With the given sample size (36 adolescents in IPT-AST and 21 in SC), the study had at least 80% power to detect a standardized mean difference between the two groups in excess of 0.80, corresponding to a large effect. Although smaller effects may be clinically meaningful, we were not sufficiently powered to detect such effects. All analyses were conducted using SAS Version 9.1.3. The study was approved by the Institutional Review Boards at New York State Psychiatric Institute and Rutgers University.
RESULTS
BASELINE DIFFERENCES AND ATTENDANCE
There were no significant differences at baseline on any of the measures. Attendance data were calculated for all adolescents assigned to intervention condition (including three adolescents who dropped out of IPT-AST before the first group and one SC adolescent who left the school before she could begin counseling). IPT-AST adolescents attended an average of 1.94 pre-group sessions (SD = 0.33) and 5.22 group sessions (SD = 2.55). SC adolescents attended an average of 3.76 sessions (SD = 2.53).
COMPARISON OF IPT-AST AND SC
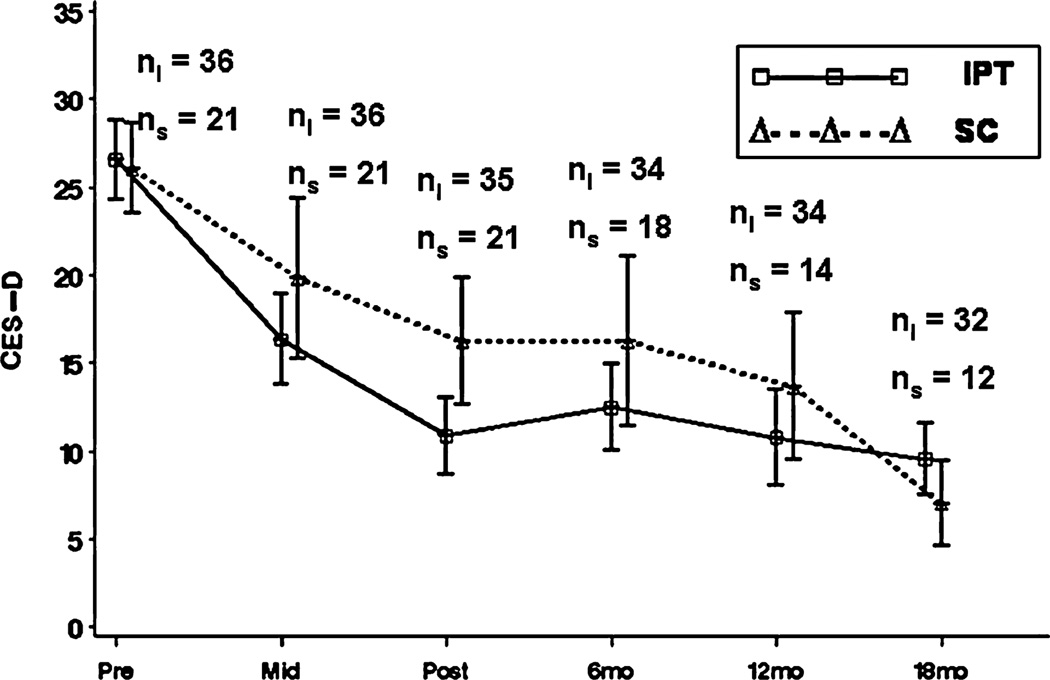
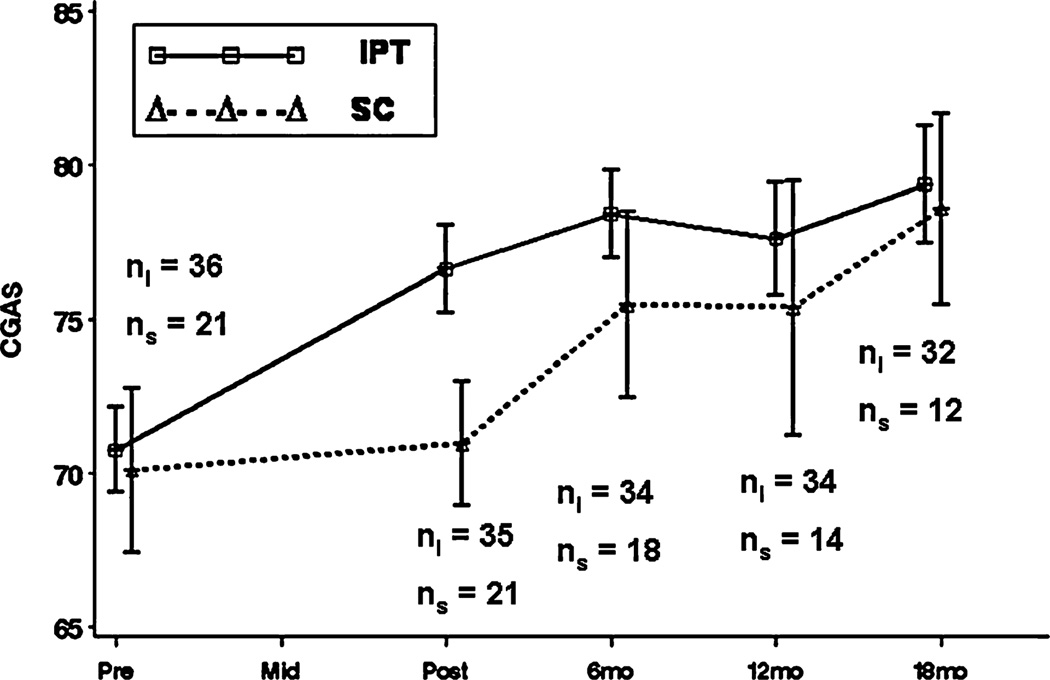
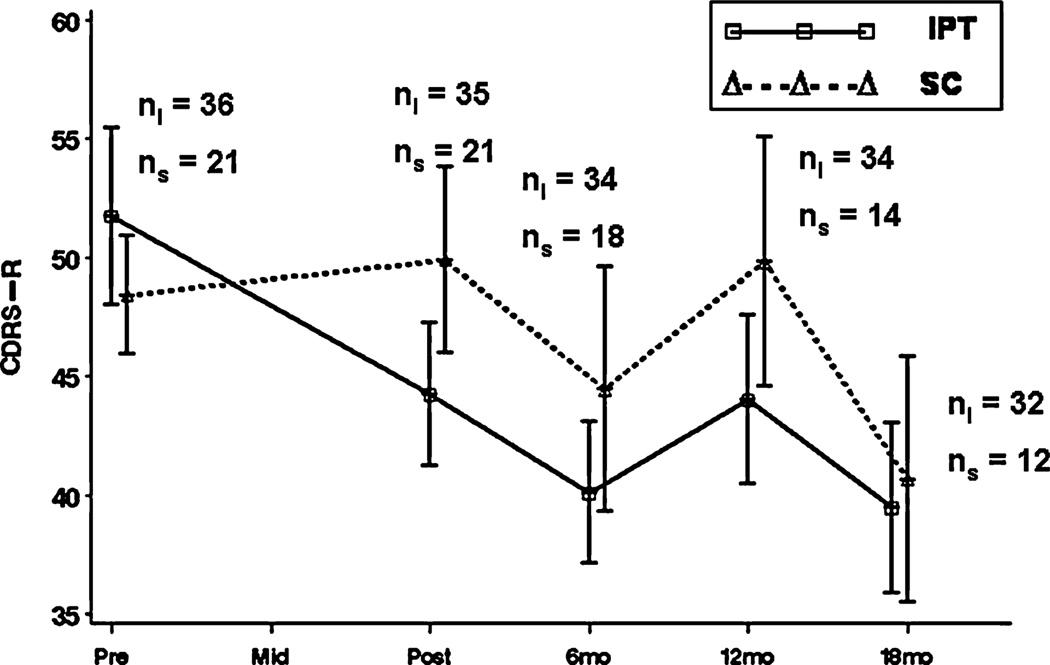
We implemented a piece-wise linear model, which examined change during the intervention and change during follow-up. Alternate models that accommodate nonlinear change over time, such as a logarithmic transformation of time, did not improve model fit. Table 2 lists the estimated slopes for each of the outcome measures. From baseline to post-intervention, IPT-AST adolescents showed significantly greater rates of change than SC adolescents on the CES-D (t(215) = −2.56, p = 0.01), CDRS-R (t(169) = −3.09, p < 0.01), and the CGAS (t(168) = 3.24, p < 0.01). In the 18 months following the intervention, there were no significant differences in rates of change on the CDRS-R (t(91) = 0.92, p = 0.36). However, there were significant differences in rates of change on the CES-D (t(102) = 2.51, p = 0.01) and the CGAS (t(76) = −2.31, p = 0.02). SC adolescents showed continued improvements during the follow-up, whereas IPT-AST adolescents showed minimal change (see Figures 2–4).
TABLE 2.
Estimated slopes for the outcome measures
| IPT-AST (N = 36) | SC (N = 21) | t | p-value | Cohen’s d (95% CI) | |
|---|---|---|---|---|---|
| Active phase | |||||
| CES-D | −7.26 (0.71) | −4.26 (0.93) | −2.56 | 0.01 | 0.68 (0.05–1.28) |
| CDRS-R | −4.12 (0.90) | 0.46 (1.18) | −3.09 | <0.01 | 0.82 (0.18–1.43) |
| CGAS | 3.08 (0.42) | 0.84 (0.55) | 3.24 | <0.01 | 0.86 (0.22–1.47) |
| Follow-up phase | |||||
| CES-D | −0.26 (0.50) | −2.51 (0.75) | 2.51 | 0.01 | 0.67 (0.04–1.27) |
| CDRS-R | −1.07 (0.69) | −2.22 (1.04) | 0.92 | 0.36 | 0.24 (−0.36–0.84) |
| CGAS | 0.72 (0.35) | 2.20 (0.53) | −2.31 | 0.02 | 0.62 (0.00–1.22) |
Note: Standard errors of the estimates are in parentheses. CES-D = Center for Epidemiologic Studies-Depression Scale; CDRS-R = Children’s Depression Rating Scale-Revised; CGAS = Children’s Global Assessment Scale.
Figure 2.
Mean profile plots for the Center for Epidemiologic Studies-Depression Scale (CES-D).
Figure 4.
Mean profile plots for the Children’s Global Assessment Scale (CGAS).
To examine mean differences, we conducted (see Figures 2–4) ANCOVA models at each assessment. post-intervention, IPT-AST adolescents had significantly lower CES-D (F(1, 52) = 8.66; p < .001; ES = 0.81), CDRS-R (F(1, 52) = 8.82; p < 0.001; ES = 0.80), and CGAS (F(1, 52) = 22.28; p < 0.001; ES = 1.27) scores than SC adolescents. At 6-month follow-up, there was a significant difference in CGAS scores (F(1, 52) = 4.86; p = 0.03; ES = 61), and a trend toward significance on the CES-D (ES = 0.51) and the CDRS-R (ES = 0.54). There were no significant differences between the groups at 12-month (effect sizes ranged from .33–.50) or 18-month follow-up (effect sizes ranged from .17–.40).
At the post-intervention assessment, none of the adolescents met criteria for a depressive disorder. By the 6-month follow-up, four SC adolescents (19.1%) met criteria for a diagnosis (three for major depression, one for dysthymia). One of these adolescents had a prior depressive episode. No IPT-AST adolescents met criteria for a depressive disorder. This difference in rates is significant (Fisher’s Exact Test, p < 0.05). By the 18-month follow-up, no additional adolescents in SC developed a depressive diagnosis (cumulative percent 19.1%), whereas three IPT-AST adolescents reported a new diagnosis (two for major depression, one for DD NOS) (cumulative percent 8.3%). The difference in rates is not significant (Fisher’s Exact Test, p = 0.40).
FEASIBILITY OF INCLUDING PARENTS IN IPT-AST
A third of the adolescents assigned to IPT-AST with parent involvement lived with both their mother and father. Of these five dual-parent families, only one adolescent had both parents attend sessions. In all of the other families, sessions were attended by one parent, typically the mother. Parents attended an average of 62.2% of the sessions; 84.6% of parents attended a pre-group session, 46.2% attended the mid-group session, and 53.9% of the parents attended the final meeting. Although this study was not designed to compare the effects of IPT-AST with and without parental involvement, we felt it would be informative for future studies to examine differences across the outcome measures.
We conducted ANCOVA models at each assessment to examine mean differences between adolescents who were assigned to the parent involvement condition and those in IPT-AST without parent involvement, controlling for baseline scores and school. At post-intervention, there was a trend toward significance on the CES-D (F(1, 31) = 2.78; p = 0.11; ES = 0.61) and CDRS-R (F(1, 31) = 3.56; p = 0.07; ES = 0.71). Adolescents who were assigned to the parental involvement condition reported lower post-intervention depression scores (CES-D: M = 8.35; SD = 5.18; CDRS-R: M = 40.82, SD = 8.60) than adolescents who were assigned to IPT-AST without parental involvement (CES-D: M = 12.07, SD = 6.68; CDRS-R: M = 46.58, SD = 7.84). There was no significant difference on overall functioning post-intervention (F(1, 31) = 0.26; p = 0.62). At the follow-up assessments, there were no significant differences on any of the measures.
DISCUSSION
This study compared the efficacy of IPT-AST and SC for the prevention of depression in adolescents with elevated symptoms. IPT-AST adolescents showed greater decreases in depression symptoms and greater improvements in overall functioning than SC adolescents following the intervention. They also reported fewer depression symptoms and better overall functioning at post-intervention and at 6-month follow-up. The large effect sizes at post-intervention and medium effects at the 6-month follow-up exceed those found in other studies of indicated depression programs.[14–15] However, by 12-month follow-up, the differences between IPT-AST and SC were no longer significant. SC adolescents continued to show improvements in depression symptoms and functioning from the 6-month follow-up assessment through the 18-month assessment, whereas IPT-AST trajectories stabilized during this time.
Gillham et al.[38] suggested that the term prevention be used only if there is an increase in symptoms or disorders in the control group and no such increase in the intervention group. Based on this definition, the changes in depression symptoms and functioning in this study are considered treatment effects. We were able to examine whether IPT-AST reduced the occurrence of new cases of depression, the ultimate goal of prevention programs.[39] We found significantly higher rates of depression diagnoses in SC adolescents in the first 6 months after the program. Thus, IPT-AST appears effective at reducing depression symptoms (treatment effect) and preventing the onset of depression (prevention effect) in the short term. However, similar to the continuous measures, the prevention benefits of IPT-AST were no longer apparent at the 12-month follow-up. Although we would have liked the prevention effects to have persisted, even the short-term prevention of depressive episodes may have a significant impact on school performance, social functioning, and adolescent developmental tasks.
This study points to the promise of IPT-AST in reducing depression symptoms and improving functioning following the intervention. However, the findings suggest that IPT-AST, in its current format, does not have long-term preventive effects. This is consistent with many other “prevention” programs.[38] Due to the limited long-term effects, it is premature to classify IPT-AST as an efficacious prevention program. The positive short-term results indicate that the intervention strategies taught in IPT-AST are effective but that we need to do more to support adolescents’ continued use of the interpersonal techniques to get longer-term benefits. Treatment studies have found that continuation cognitive behavioral therapy reduces the likelihood of relapse of depression[40] and accelerates recovery among adolescents who have not fully recovered after acute treatment.[41] Similarly, booster sessions may prolong the effects of preventive interventions.[42] The recently completed multi-site study of CWS included 6 monthly continuation sessions.[13] Future studies of IPT-AST should include booster sessions with the aim of enhancing the long-term effects of the program.
An additional question was whether it is feasible to include parents in IPT-AST. We found that parental attendance was variable, particularly for the latter two parent–adolescent sessions. Although parents attended almost two-thirds of the sessions, this often required rescheduling meetings, which may not be feasible in ordinary practice. Our design does not permit us to make any definitive conclusions about IPT-AST with and without parental involvement. An examination of the mean differences suggests that the adjunct parent–adolescent sessions may have an impact on depression symptoms post-intervention. However, it is difficult to disentangle whether it was the parental involvement or the additional adolescent attention that was beneficial. Further research is needed to better understand the impact of parental involvement in IPT-AST.
The main limitation of this study is that only a third of adolescents with elevated symptoms agreed to participate in the eligibility evaluation. The high refusal rate limits our ability to generalize these findings. High refusal rates have been found in other indicated depression studies,[11,12,22] suggesting a need to better engage adolescents in prevention programs to increase their public health impact. Similarly, a large number of adolescents and their families refused to participate in the depression screening. It is unclear whether the findings from this study extend to those adolescents who were not screened. Another limitation is the small sample size which limited power and may have inflated the effect sizes.[43] Our study was only adequately powered to detect large effect sizes. Although smaller effects may be clinically meaningful, we were not sufficiently powered to detect small or medium differences between the two conditions. Third, given that SC involved individual counseling, it is unclear whether the benefits of IPT-AST are attributable to general group processes or the specific IPT-AST techniques. Fourth, a number of SC adolescents failed to complete the follow-up assessments. Although the HLM analyses included all participants and the pattern-mixture models indicated no sensitivity to missing data, the long-term outcomes for the SC group should be interpreted cautiously. Fifth, the majority of the sample was Hispanic and over a third of the sample was African American. The inclusion of Hispanic and African American adolescents is an asset of the study as most prevention studies have been with Caucasian adolescents, and inner city minority adolescents are an underserved population.[44] However, it is unclear whether the findings from this study would generalize to adolescents of other races and ethnicities. Finally, given that adolescents in IPT-AST were not randomly assigned to groups with or without parent involvement, no definitive conclusions can be made about the benefits of parental involvement.
CONCLUSION
The findings from this study add further evidence that IPT-AST leads to an immediate reduction in depression symptoms and improvement in functioning in adolescents with subthreshold depression. Furthermore, adolescents in IPT-AST are less likely to develop depression than adolescents who receive regular SC in the 6 months following the intervention. Unfortunately, the benefits of IPT-AST do not persist beyond 6 months following the intervention. This limits the public health implications of this program in its current format and suggests the need for replication and extension of the findings before IPT-AST should be classified as a preventive intervention. Additional research is needed to determine whether booster sessions can enhance the long-term preventive effects of IPT-AST. If future studies can demonstrate a sustained impact of IPT-AST, subsequent efforts could be made to train school counselors to deliver this program effectively. Providing an effective prevention program in schools would allow more adolescents to receive help before the onset of depression with its associated impairments.
Figure 3.
Mean profile plots for the Children’s Depression Rating Scale-Revised (CDRS-R).
Footnotes
The authors report they have no financial relationships within the past 3 years to disclose.
REFERENCES
- 1.Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Arch Gen Psychiatry. 2002;59:225–231. doi: 10.1001/archpsyc.59.3.225. [DOI] [PubMed] [Google Scholar]
- 2.Weisz JR, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychol Bull. 2006;132:132–149. doi: 10.1037/0033-2909.132.1.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.US Public Health Service. Washington, DC: US Public Health Service; 2000. Report of the Surgeon General’s conference on children’s mental health: a national action agenda. [PubMed] [Google Scholar]
- 4.Gordon RS. An operational classification of disease prevention. Public Health Rep. 1983;98:107–109. [PMC free article] [PubMed] [Google Scholar]
- 5.Fergusson DM, Horwood J, Ridder EM, Beautrais AL. Subthreshold depression in adolescence and mental health outcomes in adulthood. Arch Gen Psychiatry. 2005;62:66–72. doi: 10.1001/archpsyc.62.1.66. [DOI] [PubMed] [Google Scholar]
- 6.Garrison CZ, Jackson KL, Marsteller F, et al. A longitudinal study of depressive symptomatology in young adolescents. J Am Acad Child Adolesc Psychiatry. 1990;29:581–585. doi: 10.1097/00004583-199007000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Lewinsohn PM, Solomon A, Seeley JR, Zeiss A. Clinical implications of “subthreshold” depressive symptoms. J Abnorm Psychol. 2000;109:345–351. [PubMed] [Google Scholar]
- 8.Gillham JE, Hamilton J, Freres DR, et al. Preventing depression among early adolescents in the primary care setting: a randomized controlled study of the Penn Resiliency Program. J Abnorm Child Psychol. 2006;34:203–219. doi: 10.1007/s10802-005-9014-7. [DOI] [PubMed] [Google Scholar]
- 9.Gillham JE, Reivich KJ, Jaycox LH, Seligman MEP. Prevention of depressive symptoms in schoolchildren: two-year follow-up. Psychol Sci. 1995;6:343–351. [Google Scholar]
- 10.Jaycox LH, Reivich KJ, Gillham J, Seligman MEP. Prevention of depressive symptoms in school children. Behav Res Ther. 1994;32:801–816. doi: 10.1016/0005-7967(94)90160-0. [DOI] [PubMed] [Google Scholar]
- 11.Clarke GN, Hawkins W, Murphy M, et al. Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: a randomized trial of a group cognitive intervention. J Am Acad Child Adolesc Psychiatry. 1995;34:312–321. doi: 10.1097/00004583-199503000-00016. [DOI] [PubMed] [Google Scholar]
- 12.Clarke GN, Hornbrook M, Lynch F, et al. A randomized trial of a group cognitive intervention for preventing depression in adolescent offspring of depressed parents. Arch Gen Psychiatry. 2001;58:1127–1134. doi: 10.1001/archpsyc.58.12.1127. [DOI] [PubMed] [Google Scholar]
- 13.Garber J, Clarke G, Weersing VR, et al. Prevention of depression in at risk-adolescents: a randomized controlled trial. J Am Med Assoc. 2009;301:2214–2215. doi: 10.1001/jama.2009.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Horowitz JL, Garber J. The prevention of depressive symptoms in children and adolescents: a meta-analytic review. J Consult Clin Psychol. 2006;74:401–415. doi: 10.1037/0022-006X.74.3.401. [DOI] [PubMed] [Google Scholar]
- 15.Stice E, Shaw H, Bohon C, et al. A meta-analytic review of depression prevention programs for children and adolescents: factors that predict magnitude of intervention effects. J Consult Clin Psychol. 2009;77:486–503. doi: 10.1037/a0015168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Young JF, Mufson L. Manual for Interpersonal Psychotherapy-Adolescent Skills Training (IPT-AST) New York: Columbia University; 2003. [Google Scholar]
- 17.Mufson L, Dorta KP, Moreau D, Weissman MM. Interpersonal psychotherapy for depressed adolescents. 2nd ed. New York: Guilford Press; 2004. [Google Scholar]
- 18.Mufson L, Weissman MM, Moreau D, Garfinkel R. Efficacy of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry. 1999;56:573–579. doi: 10.1001/archpsyc.56.6.573. [DOI] [PubMed] [Google Scholar]
- 19.Mufson L, Dorta KP, Wickramaratne P, et al. A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry. 2004;63:577–584. doi: 10.1001/archpsyc.61.6.577. [DOI] [PubMed] [Google Scholar]
- 20.Sheeber LB, Davis B, Leve C, et al. Adolescents’ relationships with their mothers and fathers: associations with depressive disorder and subdiagnostic symptomatology. J Abnorm Psychol. 2007;116:144–154. doi: 10.1037/0021-843X.116.1.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Young JF, Berenson K, Cohen P, Garcia J. The role of parent and peer support in predicting adolescent depression: a longitudinal community study. J Res Adolesc. 2005;15:407–423. [Google Scholar]
- 22.Young JF, Mufson L, Davies M. Efficacy of interpersonal psychotherapy-adolescent skills training: an indicated preventive intervention for depression. J Child Psychol Psychiatry. 2006;47:1254–1262. doi: 10.1111/j.1469-7610.2006.01667.x. [DOI] [PubMed] [Google Scholar]
- 23.Horowitz JL, Garber J, Ciesla JA, et al. Prevention of depressive symptoms in adolescents: a randomized trial of cognitive-behavioral and interpersonal prevention programs. J Consult Clin Psychol. 2007;75:693–706. doi: 10.1037/0022-006X.75.5.693. [DOI] [PubMed] [Google Scholar]
- 24.Shochet IM, Dadds MR, Holland D, et al. The efficacy of a universal school-based program to prevent adolescent depression. J Clin Child Adolesc Psychol. 2001;30:303–315. doi: 10.1207/S15374424JCCP3003_3. [DOI] [PubMed] [Google Scholar]
- 25.Gillham JE, Reivich KJ, Freres DR, et al. School-based prevention of depression and anxiety symptoms in early adolescence: a pilot of a parent intervention component. School Psychol Q. 2006;21:323–348. [Google Scholar]
- 26.Collins KA, Dozois DJA. What are the active ingredients in preventative interventions for depression? Clin Psychol Sci Pract. 2008:313–330. [Google Scholar]
- 27.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1997;1:385–401. [Google Scholar]
- 28.Kaufman J, Birmaher B, Brent D, Rao U. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 29.Shaffer D, Gould MS, Brasic J, et al. A Children’s Global Assessment Scale (CGAS) Arch Gen Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- 30.Poznanski EO, Mokros HB. Children’s Depression Rating Scale, Revised (CDRS-R) Los Angeles: Western Psychological Services; 1996. [Google Scholar]
- 31.Keller MB, Lavori PW, Friedman B, et al. The longitudinal interval follow-up evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- 32.Institute of Medicine. Small Clinical Trials: Issues and challenges. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 33.Keller MB, McCullough JP, Klein DN, et al. A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. New Engl J Med. 2000;342:1462–1470. doi: 10.1056/NEJM200005183422001. [DOI] [PubMed] [Google Scholar]
- 34.Kenward MG, Roger JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53:983–997. [PubMed] [Google Scholar]
- 35.Verbeke G, Molenberghs G. Linear Mixed Models for Longitudinal Data. New York: Spinger; 2000. [Google Scholar]
- 36.Rubin DB. Inference and missing data. Biometrika. 1976;63:581–592. [Google Scholar]
- 37.Hedeker D, Gibbons RD. Application of random-effects pattern-mixture models for missing data in longitudinal studies. Psychol Methods. 1997;2:64–78. [Google Scholar]
- 38.Gillham JE, Shatté AJ, Freres DR. Preventing depression: a review of cognitive-behavioral and family interventions. Appl Prev Psychol. 2000;9:63–88. [Google Scholar]
- 39.Mrazek PJ, Haggerty RJ. Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research. Washington, DC: National Academy Press; 1994. [PubMed] [Google Scholar]
- 40.Kroll L, Harrington R, Jayson D, Fraser J. Pilot study of continuation cognitive-behavioral therapy for major depression in adolescent psychiatric patients. J Am Acad Child Adolesc Psychiatry. 1996;35:1156–1161. doi: 10.1097/00004583-199609000-00013. [DOI] [PubMed] [Google Scholar]
- 41.Clarke GN, Rohde P, Lewinsohn PM, et al. Cognitive-behavioral treatment of adolescent depression: efficacy of acute group treatment and booster sessions. J Am Acad Child Adolesc Psychiatry. 1999;38:272–279. doi: 10.1097/00004583-199903000-00014. [DOI] [PubMed] [Google Scholar]
- 42.Merry SN. Prevention and early intervention for depression in young people: a practical possibility? Curr Opin Psychiatry. 2007;20:325–329. doi: 10.1097/YCO.0b013e3281bc0d19. [DOI] [PubMed] [Google Scholar]
- 43.Kraemer HC, Mintz J, Noda A, et al. Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch Gen Psychiatry. 2006;63:484–489. doi: 10.1001/archpsyc.63.5.484. [DOI] [PubMed] [Google Scholar]
- 44.Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among US children: variation by ethnicity and insurance status. Am J Psychiatry. 2002;152:1548–1555. doi: 10.1176/appi.ajp.159.9.1548. [DOI] [PubMed] [Google Scholar]