Abstract
Objective To assess the impact of exercise referral schemes on physical activity and health outcomes.
Design Systematic review and meta-analysis.
Data sources Medline, Embase, PsycINFO, Cochrane Library, ISI Web of Science, SPORTDiscus, and ongoing trial registries up to October 2009. We also checked study references.
Study selection Design: randomised controlled trials or non-randomised controlled (cluster or individual) studies published in peer review journals. Population: sedentary individuals with or without medical diagnosis. Exercise referral schemes defined as: clear referrals by primary care professionals to third party service providers to increase physical activity or exercise, physical activity or exercise programmes tailored to individuals, and initial assessment and monitoring throughout programmes. Comparators: usual care, no intervention, or alternative exercise referral schemes.
Results Eight randomised controlled trials met the inclusion criteria, comparing exercise referral schemes with usual care (six trials), alternative physical activity intervention (two), and an exercise referral scheme plus a self determination theory intervention (one). Compared with usual care, follow-up data for exercise referral schemes showed an increased number of participants who achieved 90-150 minutes of physical activity of at least moderate intensity per week (pooled relative risk 1.16, 95% confidence intervals 1.03 to 1.30) and a reduced level of depression (pooled standardised mean difference −0.82, −1.28 to −0.35). Evidence of a between group difference in physical activity of moderate or vigorous intensity or in other health outcomes was inconsistent at follow-up. We did not find any difference in outcomes between exercise referral schemes and the other two comparator groups. None of the included trials separately reported outcomes in individuals with specific medical diagnoses.Substantial heterogeneity in the quality and nature of the exercise referral schemes across studies might have contributed to the inconsistency in outcome findings.
Conclusions Considerable uncertainty remains as to the effectiveness of exercise referral schemes for increasing physical activity, fitness, or health indicators, or whether they are an efficient use of resources for sedentary people with or without a medical diagnosis.
Introduction
Physical activity contributes to the prevention and management of many medical conditions and diseases, including coronary heart disease, type 2 diabetes, some cancers, and mental illness, such as dementia and depression.1 2 Despite recommendations that adults should undertake at least 30 minutes of exercise of moderate intensity at least five times a week, only about a third are active to this level.3
Primary care is a key setting for the promotion of physical activity. Consequently, myriad primary care based interventions have developed over the past 20 years.4 A common model is the exercise referral scheme, in which a general practitioner (or another member of the primary care team) identifies and refers a sedentary individual with evidence of at least one cardiovascular risk factor to a third party service (often a sports centre or leisure facility). This service then prescribes and monitors an exercise programme tailored to the individual needs of the patient.5 In the United Kingdom, contemporary exercise referral schemes were first set up around 1990, with numbers growing rapidly; more than 600 schemes are now thought to be in operation. Many schemes operate across several sites, which all adhere to a core set of standards.6 The exercise referral scheme model is also being established in primary care practice in other areas, including Spain and Scandinavian countries.7 8
Several systematic reviews have examined the evidence base for exercise referral schemes and concluded that these schemes can increase the physical activity of sedentary adults in the short term.9 10 11 12 Although these reviews included several randomised controlled trials (21 in total), many of these were studies of physical activity interventions without a referral by a member of the primary care team to a third party exercise provider. Few randomised controlled trials, therefore, have assessed the specific impact of an exercise referral scheme. Furthermore, these trials have failed to address the impact of exercise referral schemes on health related outcomes (for example, changes in lipid profile and blood pressure) or for individuals with pre-existing conditions, who could be most likely to benefit from these schemes (for example, those with coronary heart disease or depression). In 2006, the UK’s National Institute for Health and Clinical Excellence (NICE) called for more controlled research on the effectiveness of exercise referral schemes.11
We therefore updated the evidence base for exercise referral schemes in the light of new controlled trials and revisited previous concerns about the applicability of this evidence to policy and practice. A cost effectiveness analysis of exercise referral schemes has also been undertaken.13
Methods
We conducted and reported this systematic review in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement.14
Search strategy
We searched the following electronic databases: Medline In-Process (Ovid) and Medline (Ovid), 1950 to October 2009; Embase (Ovid), 1980-2009, week 28; Cochrane Library (Wiley), 2009, issue 3 (Cochrane Database of Systematic Reviews, database of abstracts of reviews of effects, National Health Service economic evaluation database, and Health Technology Assessment database); SPORTDiscus, 1990 to October 2009; ISI Web Of Knowledge, 1900 to October 2009; Science Citation Index Expanded, 1900 to October 2009; and Social Sciences Citation Index, 1898 to October 2009. To maximise the specificity, we did an initial scoping search to develop “exercise referral” and other related synonym terms which we then combined with “primary care” search terms and a controlled trial filter. Studies were also sought by reviewing the bibliographies of included studies and those known to the researchers of the present study. Furthermore, we limited the search to studies in the English language and that were published from 1990 onwards. Web appendix 1 provides full details of the search strategies. Searches were updated until July 2011.
Inclusion criteria
We considered studies to be eligible for inclusion if they met criteria regarding study design, population, intervention, comparators, and outcomes (box).
Box: Inclusion criteria for eligible studies
Study design: randomised controlled trials and non-randomised controlled (cluster or individual) studies
Population: any individual with or without a medical diagnosis
Intervention: an exercise referral scheme was defined as comprising three core components—(1) referral by a primary care healthcare professional to a third party service provider, designed to increase physical activity or exercise; (2) physical activity or exercise programme tailored to individual needs; and (3) initial assessment and monitoring throughout the programme. The exercise referral scheme and the physical activity or exercise programme had to be more intensive than simple advice and needed to include at least one form or a combination of counselling (in person or by telephone, by use of written materials, or by supervised exercise training)
Comparator: any control, such as usual care (such as brief advice on physical activity); no intervention; or alternative forms of exercise referral schemes
Outcomes: physical activity (as a self report or objectively monitored), physical fitness, clinical outcomes (for example, blood lipids), health related quality of life, and adverse events (for example, musculoskeletal injury)
We excluded studies not published in a peer reviewed journal (for example, annual reports of exercise referral scheme programmes), editorials, opinions, and studies available only as meeting abstracts; programmes or systems of exercise referral initiated in secondary or tertiary care, such as conventional comprehensive cardiac or pulmonary rehabilitation programmes; and exercise programmes in which individuals were recruited from primary care but received no clear statement of referral by a member of the primary care team.
Study selection process
We screened titles and abstracts in three stages. At stage 1, one reviewer (TP) initially ruled out clearly irrelevant titles and abstracts. At stage 2, two reviewers (TP and RT, KF, MH, or AT) then independently screened the remaining titles and abstracts. At stage 3, full papers of abstracts categorised as potentially eligible for inclusion were screened by a consensus meeting of least two reviewers (TP and RT, KF, MH, AT) and disagreements were resolved in real time by consensus.
Data extraction
Data were extracted by one reviewer (TP) using a standardised data extraction form and checked by another (RT). Discrepancies were resolved by discussion, with involvement of a third reviewer if necessary. Extraction included data for patient characteristics (for example, age or disease diagnosis), intervention (for example, duration, location, intensity, and mode of the exercise intervention delivered), comparator, study quality, and reported outcomes pertinent to the review. We contacted all included study authors to seek information not available in study reports.
Risk of bias assessment
We derived risk of bias criteria from previous instruments assessing quality or risk of bias that used published criteria relevant to controlled studies.15 16
Data analysis and synthesis
In view of the heterogeneous nature of outcomes and variable quality of outcome reporting, the primary focus of our data synthesis was descriptive and detailed tabular summaries were presented. For a small number of outcomes, we were able to consistently extract data across studies to allow quantitative summaries using the meta-analysis. We expressed dichotomous outcomes as relative risks (95% confidence intervals) for each study. For continuous variables, we compared net changes (that is, the differences between the exercise group and control group) and calculated a weighted or standardised mean difference (95% confidence intervals) for each study.
We investigated heterogeneity by reviewing the study populations, methods, and interventions; by visualising the results; and by using the χ2 test for homogeneity and the I2 statistic. A fixed effects model for the meta-analysis was used unless statistical heterogeneity was identified (χ2 test, P≤0.05, or I2≥50%), where a random effects model was used. In view of the small number of studies consistently reporting outcomes in a format to allow a meta-analysis, we were not able to undertake a funnel plot and assessment of publication bias analysis. Analyses were conducted with RevMan version 5.0.
Results
Identification and selection of studies
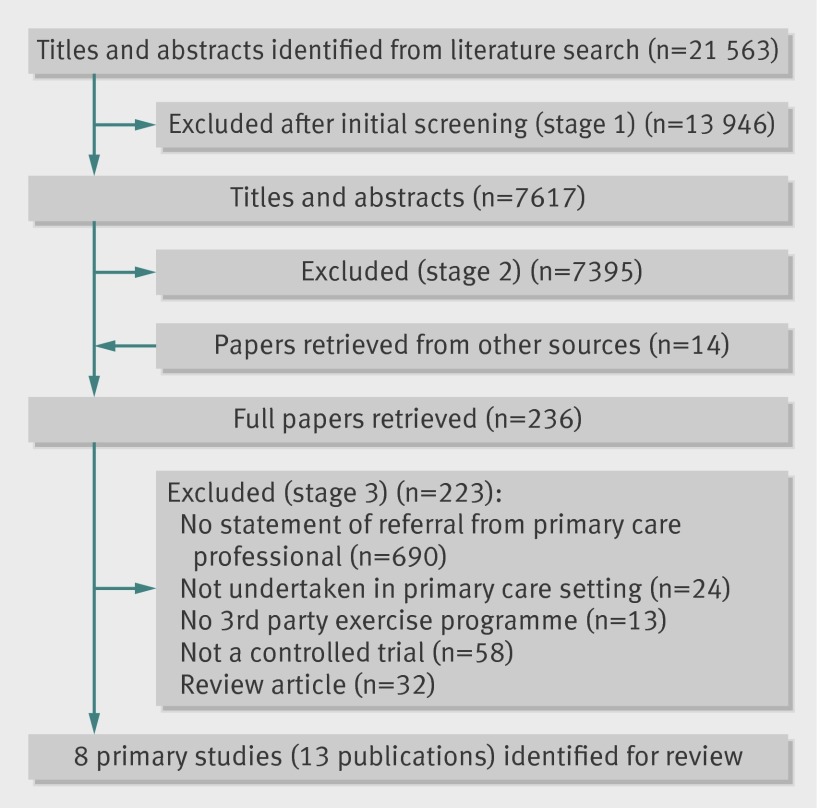
Our bibliographic search yielded 21 563 titles (fig 1). After a full review of the papers, the main reason for exclusion was that studies recruited primary care individuals into exercise programmes, with no clear statement of a referral by a member of the primary care team to a third party exercise provider. Web appendix 2 provides the full list of excluded studies.
Fig 1 Flow diagram of study inclusion process
In addition to the six trials that met the inclusion criteria,7 8 17 18 19 20 21 22 23 our searches identified published protocols for another two trials on exercise referral schemes.24 25 By contacting the trial authors, we were able to obtain the full unpublished trial report for one of these trials.26 Although a report of the other trial was not made fully available to us and unpublished at the time of this review, it is now available as a press release.27 We included both trials in our analysis.
Characteristics of included studies
The eight trials (13 publications) included 5190 participants (table 1). All studies were randomised controlled trials, six undertaken in the UK,18 20 21 22 26 27 one in Denmark,23 and one in Spain.8 Various geographical locations in England and Wales were provided for the UK based studies.
Table 1.
Summary of included study characteristics
| Study | Location | No of patients in randomised groups | Population | Exercise referral scheme intervention | Control | Outcomes assessed | Follow-up periods | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean age (years), men (%) | Disease groups | Exercise content, duration (per week), intensity, and provider | IC | EA | G or I | |||||||
| Taylor et al17-19 | UK (South East) | 97, 45 | 54, 37 | Hypertension, obesity |
10 weeks, 2×30-40 min, moderate intensity, leisure centre | Yes | NR | Both | No exercise programme | Physical activity, clinical outcomes, psychological wellbeing | 8, 16, 26, and 37 weeks | |
| Stevens et al20 | UK (London) | 363, 351 | 59, 40 | Obesity | 10 weeks, NR, NR, leisure centre | Yes | Yes | Both | No exercise programme | Physical activity | 8 months | |
| Harrison et al21 | UK (North West) | 275, 270 | NR, 33 | NR | 12 weeks, 2×1 h, individually based, leisure centre | Yes | Yes | Both | No exercise programme | Physical activity | 6, 9, and 12 months | |
| Isaacs et al22 | UK (Greater London) | 317, 315, 311 | 57, 35 | Hypertension, obesity, raised cholesterol, type II diabetes | 10 weeks, 2×45 min, NR, leisure centre | Yes | NR | Both | No exercise programme; or 10 week walking scheme, 2×45 min/week, 60-80% of maximum heart rate, group setting | Physical activity, physical fitness, clinical outcomes, psychological wellbeing, health related quality of life | 10 weeks, 6 and 12 months | |
| Sorensen et al23 | Denmark | 28, 24 | 54, 43 | Metabolic syndrome, depression, cardiovascular disease | 4 months, 2×1 h/1×1 h, >50% heart rate reserve (20 min), clinic | Yes | NR | Group | Motivational counselling (45-60 min/session) | Physical activity, physical fitness, clinical outcomes, health related quality of life | 4 and 10 months | |
| Gusi et al8 | Spain | 127, 160 | 71, 0 | Obesity, type II diabetes, depression | 6 months, 3×50 min, NR, walking scheme | NR | NR | Group | No exercise programme | Clinical outcomes, psychological wellbeing, health related quality of life | 6 months | |
| Jolly et al24,26 | UK (Midlands) | 184, 163 | NR, 24 | Hypertension, obesity, anxiety, depression | 12 weeks, NR, NR, leisure centre | Yes | Yes | Both | Usual programme of exercise referral scheme | Physical activity, clinical outcomes, psychological wellbeing, health related quality of life | 3 and 6 months | |
| Murphy et al25,27 | UK (Wales) | 1080, 1080 | NR, 34 | Mental health | 16 weeks, NR, NR, leisure centre | Yes | Yes | Both | No exercise programme | Physical activity, psychological wellbeing | 6 and 12 months | |
IC=initial consultation; EA=exit intervention; G or I=group or individual sessions; NR=not reported; h=hours; min=minutes.
Duration of study follow-up ranged from 2 to 12 months. Six trials compared exercise referral schemes with a usual care control group that consisted of no exercise intervention or some simple advice on physical activity.8 18 20 21 22 27 Two trials compared exercise referral schemes with an alternative physical activity intervention: motivational counselling or an instructor led walking programme aimed at increasing daily physical activity.22 23 In their randomised controlled trial, Jolly and colleagues used a cluster design to compare exercise referral schemes alone with an exercise referral scheme plus a behaviour change intervention (that is, self determination theory).26 The authors stated that the intracluster correlation was so low (0.01) that they did not take account of adjustment for clustering in their analyses. Nevertheless, for the purposes of the present meta-analysis, we reduced the effective sample size for binary outcomes and increased the standard deviations for continuous outcomes on the basis of the design factor of 1.12 (based on an intracluster correlation of 0.01 and 13 clusters).16
Trials mainly recruited sedentary, middle aged, white adults who had no medical diagnosis but had evidence of at least one cardiovascular risk factor (that is, high blood pressure, raised serum cholesterol, smoking, or being overweight). In those trials that recruited a proportion of individuals with diabetes, hypertension, depression, coronary heart disease, or obesity, only aggregated outcomes across all trial participants were reported, restricting the use of subgroup analyses to determine effectiveness of exercise referral schemes within specific populations.
The general practitioner was the main referrer, often using a bespoke referral form to a fitness or exercise instructor or officer. All exercise referral schemes apart from the Gusi study8 included an initial consultation by the third party provider, such as a qualified exercise professional (table 1). Scheme duration was typically 10-12 weeks, and took place in a leisure centre,18 20 21 22 26 27 a clinic,23 or public parks and forest tracks.8 Exercise sessions were usually twice per week, between 30-60 minutes per session, and set at either a moderate or individually tailored intensity. Four studies reported the use of an exit assessment at the completion of the exercise referral scheme.20 21 26 27
Risk of bias
All trials generated a random allocation sequence although details of concealment were poorly reported (table 2). All trials reported good balance between groups in participant characteristics at baseline. Although blinding of participants and intervention providers was not feasible, the Jolly and Murphy studies reported outcome blinding.26 27 For both studies, self reported physical activity using the seven day physical activity recall was assessed via telephone by researchers blinded to group allocation. The reporting and handling of missing data were detailed for most studies, and all studies apart from one18 reported the use of intention to treat analyses. The level of missing data at follow-up ranged from 17% to 50%. Most studies used imputation methods (that is, the last observation carried forward or the average of complete case values) to replace missing data values at follow-up. Overall, three studies were judged to be at moderate overall risk of bias (Taylor,18 Harrison,21 and Stevens20) and five at a low overall risk of bias (Gusi,8 Isaacs,22 Jolly,26 Sorensen,23 and Murphy27).
Table 2.
Summary of risk of bias assessment
| Risk of bias criterion | Taylor et al18 | Stevens et al20 | Harrison et al21 | Isaacs et al22 | Sorensen et al23 | Gusi et al8 | Jolly et al26 | Murphy et al27 |
|---|---|---|---|---|---|---|---|---|
| Method of random sequence generation described | Yes | Yes | Yes | Yes | Yes | Yes | Yes* | Yes |
| Method of allocation concealment described | Yes* | Yes | Unclear | Unclear | Yes | Yes | Yes* | Yes |
| Method of outcome (assessment) blinding described | Unclear | Unclear | Unclear | No | Unclear | Unclear | Yes | Yes |
| Groups similar at baseline | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Intention to treat analysis used | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Any statistical handling of missing data | Unclear | Yes | Unclear | Yes | Yes | Yes | Yes | Yes |
| Missing data reported (dropout and loss to follow-up) | Yes* | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
*From correspondence with author.
Outcome findings
We reported outcome results according to the three categories of comparator group: usual care, alternative exercise interventions (or alternative physical activity interventions), and exercise referral schemes plus behaviour change interventions (or alternative exercise referral schemes).
Physical activity
All studies, with the exception of the Gusi study,8 relied on a self report measure of physical activity. No studies assessed physical activity using objective methods.
Exercise referral schemes versus usual care
The most consistently reported physical activity outcome across studies was the proportion of individuals achieving 90-150 minutes of activity of at least moderate intensity per week (table 3).28 After pooling data across studies, we found a 16% (95% confidence intervals 3% to 30%) increase in the relative risk of achieving this outcome with exercise referral schemes, compared with usual care, at 6 to12 months’ follow-up (fig 2, using denominators as reported by the study authors). The Taylor and Harrison studies reported this outcome based on the number of individuals who were available at follow-up.18 21 To assess the potential (attrition) bias in using completers, we adjusted the denominators of these two studies to all individuals undergoing randomisation. Assuming that all missing cases did not meet the physical activity threshold, we found that exercise referral schemes no longer differed significantly from usual care (fig 2, using denominators adjusted to all randomised groups).
Table 3.
Summary of physical activity data at follow-up, where reported in meta-analysis studies
| Study comparison and follow-up | Patients achieving physical activity guidance* (n/N) | Mean (SD) duration of at least moderate intensity (min/week) | Mean (SD) duration of total physical activity (min/week) | Mean energy expenditure (kJ/kg per day) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Exercise referral scheme | Comparator scheme | Exercise referral scheme | Comparator scheme | Exercise referral scheme | Comparator scheme | Exercise referral scheme | Comparator scheme | |||||
| Exercise referral scheme v usual care | ||||||||||||
| Taylor et al18†‡ | ||||||||||||
| 8 weeks | 51/63 | 20/31§ | 247 (174)/49 (60) | 145 (178)¶/21 (61)¶ | – | – | 145 (1.2) | 141 (1.7)¶ | ||||
| 16 weeks | 51/57 | 18/31§¶ | 226 (252)/59 (72) | 160 (262)/21 (72)¶ | – | – | 145 (1.2) | 142 (1.7)¶ | ||||
| 26 weeks | 39/47 | 18/31§¶ | 183 (234)/56 (108) | 206 (251)/34 (111) | – | – | 144 (1.8) | 144 (1.2) | ||||
| 37 weeks | 39/57 | 19/31§ | 158 (228)/42 (96) | 162 (245)/23 (106) | – | – | 143 (2.4) | 1 (2.2) | ||||
| Stevens et al20** | ||||||||||||
| 8 months | 204/363 | 174/351§ | – | – | – | – | – | – | ||||
| Harrison et al21‡ | ||||||||||||
| 6 months | 38/168 | 22/162§¶ | – | – | – | – | – | – | ||||
| 9 months | 36/149 | 31/140 | – | – | – | – | – | – | ||||
| 12 months | 40/155 | 32/157 | – | – | – | – | – | – | ||||
| Isaacs et al22 | ||||||||||||
| 10 weeks | 48/164 | 29/157§¶ | 93 (115) | 79 (114) | 584 (479) | 668 (555) | 142 (26) | 151 (32) | ||||
| 6 months | 70/179 | 66/200§ | 65 (106) | 58 (98) | 692 (496) | 647 (463) | 159 (27) | 147 (27) | ||||
| Murphy et al27** | ||||||||||||
| 12 months | – | – | – | – | 1.18 (0.99 to 1.42), 1.19 (1.00 to 1.42)¶†† | – | – | |||||
| Exercise referral scheme v alternative physical activity intervention | ||||||||||||
| Sorensen et al23‡,‡‡ | ||||||||||||
| 4 months | – | – | – | – | 63 (114) | 23 (107) | 43 (2.4) | 41 (4.8) | ||||
| 10 months | – | – | – | – | 20 (124) | 20 (152) | 41 (2.1) | 40 (5) | ||||
| Isaacs et al22 | ||||||||||||
| 10 weeks | 48/164 | 53/92§¶ | 93 (115) | 113 (291) | 584 (479) | 863 (1026)¶ | 142 (26) | 180 (38)¶ | ||||
| 6 months | 70/179 | 62//141§ | 65 (106) | 89 (150)¶ | 692 (496) | 759 (539) | 159 (27) | 176 (27) | ||||
| Exercise referral scheme v alternative exercise referral scheme | ||||||||||||
| Jolly et al26 | ||||||||||||
| 3 months3 | – | – | 319 (338) | 331 (336) | – | – | – | – | ||||
| 6 months3 | 66/156 | 83/169§ | 249 (356) | 246 (343) | – | – | – | – | ||||
*Referring to 90-150 minutes of physical activity per week of at least moderate intensity.
†Duration of at least moderate intensity presented as moderate/vigorous values.
‡Data refer to numbers of individuals with complete data or questionnaires.
§P value calculated by authors of present meta-analysis.
¶Significant difference at P≤0.05.
**Data refer to all participants in randomised groups.
††Only odds ratio (95% CI) data for physical activity available; odds ratios presented as data adjusted for all covariates (which shows a non-significant difference), and data with baseline physical activity measure omitted from adjustment (which shows a significant difference).
‡‡Data are mean change in score. Mean energy expenditure data presented as metabolic equivalent thresholds per hour per day.
Fig 2 Meta-analysis of patients achieving 90-150 minutes of physical activity of at least moderate intensity per week, using denominators as reported by study authors and denominators adjusted to all randomised groups. Fixed effects model used. M-H=Mantel-Haenszel
Murphy and colleagues showed a significantly higher level of total physical activity per week with exercise referral schemes than with usual care, but only if they omitted baselines measures of physical activity from the adjusted analysis (table 3).27 There was no difference between exercise referral schemes and usual care in either the minutes of activity spent in at least moderate intensity per week or in the estimated energy expenditure from physical activity (web figs 1 and 2). Harrison and colleagues reported no significant interaction between the effect of exercise referral schemes and prespecified baseline variables such as risk factors for coronary heart disease, sex, and age.21
Exercise referral schemes versus alternative physical activity intervention
Overall, we found no significant difference in the proportion of individuals achieving the 90-150 minutes’ increase in moderate activity threshold, total amount of physical activity, or energy expenditure between exercise referral schemes and alternative physical activity interventions (fig 2, web figs 3 and 4). The study by Isaac and colleagues observed an increase in the number of minutes spent in physical activity at moderate intensity for patients in the walking programme compared with those in the exercise referral scheme group.22
Exercise referral schemes versus exercise referral schemes plus behaviour change intervention
Jolly and colleagues reported that the proportion of patients achieving at least 150 minutes of moderate physical activity per week increased in the standard exercise referral scheme group from 27% at baseline to 63% at three months and 46% at six months, compared with the group participating in the referral scheme plus behaviour change intervention.26 However, we did not see a difference between the groups in these proportions (fig 2).
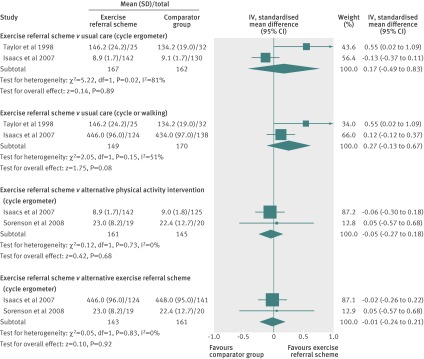
Physical fitness
Three studies reported physical fitness outcomes (web table 1).18 22 23 Pooling of the cardiorespiratory fitness measures showed no difference between exercise referral schemes and usual care or alternative physical activity intervention (fig 3). We found evidence of considerable statistical heterogeneity when comparing the schemes with usual care. The Jolly study did not assess physical fitness, so we could not compare standard referral schemes with those that included a behaviour change intervention.26
Fig 3 Meta-analysis of patients’ cardiorespiratory fitness, at 6-12 month follow-up. SD=standard deviation. Random effects model used. IV=inverse variance
Clinical outcomes
Five studies provided information on clinical outcomes (that is, blood pressure, serum lipids (web table 2), weight and obesity measures (web table 3), respiratory function (web table 4), and diabetes control.8 18 22 23 26
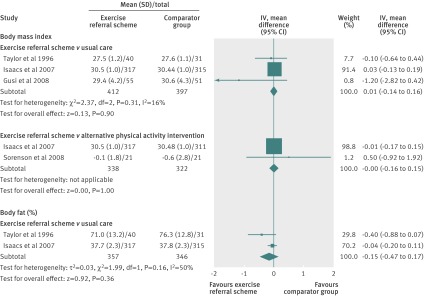
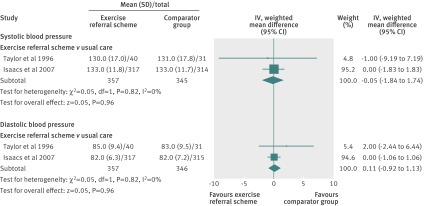
Exercise referral schemes versus usual care
Taylor and colleagues reported a lower percentage of body fat in exercise referral scheme participants than in the usual care group at follow-up.18 However, overall there was no difference between the two groups in body mass index or body fat (fig 4). There was also no between group difference in diastolic or systolic blood pressure (fig 5), serum lipids (web table 2), and respiratory function (web table 4) at follow-up.
Fig 4 Meta-analysis of body mass index and body fat (%) in patients, at 6-12 month follow-up. SD=standard deviation. Fixed effects model used. IV=inverse variance. Data for body mass index are values for weighted mean difference and data for body fat are values for standardised mean difference
Fig 5 Meta-analysis of systolic and diastolic blood pressure in patients, at 6-12 month follow-up. SD=standard deviation. Fixed effects model used. IV=inverse variance
Exercise referral schemes versus alternative physical activity intervention
Isaacs and colleagues reported no significant differences between exercise referral schemes and alternative physical activity intervention at follow-up in resting blood pressure (web table 2), body mass index or body fat (fig 4, web table 3), serum lipids (web table 2), and respiratory function (web table 4).22 Sorensen and colleagues reported reduced concentrations of glycolated haemoglobin (HbA1c %) in both the exercise referral scheme group (mean −0.26%, 95% confidence intervals −0.79 to 0.27) and physical activity counselling group (−0.23%, −0.47 to 0.02) at 4 months’ follow-up, although there was no statistical difference between them.23
Exercise referral schemes versus exercise referral schemes plus behaviour change intervention
Jolly and colleagues reported no differences between standard exercise referral schemes only and exercise referral schemes plus self determination theory in body mass index or blood pressure (web tables 2 and 3). Serum lipid samples were not collected in this trial.26
Psychological wellbeing
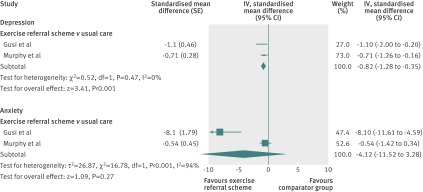
Five studies reported outcomes on psychological wellbeing (web table 5).8 17 22 26 27 The Taylor and Fox studies showed improvements in physical self worth and in perceptions of physical condition and physical health in the exercise referral scheme group, compared with the usual care group at 16 and 37 weeks’ follow-up (web table 5).17 The other studies showed a significant reduction in depression but not in anxiety for exercise referral schemes compared with usual care (fig 6). The Isaacs and Jolly studies reported no difference in anxiety or depression outcomes, respectively, between exercise referral schemes and the other two comparator groups at 6 months’ follow-up.22 26
Fig 6 Meta-analysis of depression and anxiety in patients, at 6-12 month follow-up. SE=standard error. Fixed effects model used. IV=inverse variance
Health related quality of life
Four studies reported outcomes on health related quality of life (web table 6).8 22 23 26 Because of the heterogeneity in outcome reporting, we were not able to undertake meta-analysis. Isaacs and colleagues did not see any differences between the exercise referral schemes and usual care groups at follow-up on the SF-36 mental health scale.22 Gusi and colleagues observed significantly higher EQ-5D scores in the exercise referral scheme group than in the usual care group at 6 month follow-up.8
The Isaacs study reported no differences between the referral schemes and walking groups (as an alternative physical activity intervention) at follow-up on the SF-36 mental health scale score.22 Similarly, Sorensen and colleagues found no differences between the groups at follow-up on the SF-12 mental and physical scales.23 Jolly and colleagues reported no difference in overall Dartmouth Cooperative chart scores between standard referral schemes and those including a behaviour change intervention. However, they found a difference in the feelings subscale at six months’ follow-up in favour of the schemes that included self determination (mean difference 0.21, 95% confidence intervals 0.01 to 0.40, P<0.05).26
Discussion
Main findings
In this systematic review of eight randomised controlled trials (5190 participants), we found weak evidence of a short term increase in physical activity and a reduction in levels of depression of sedentary individuals after participation in an exercise referral scheme compared with usual care. We did not find consistent evidence in favour of exercise referral schemes in outcomes based on physical fitness, psychological wellbeing, overall health related quality of life, blood pressure, serum lipid levels, indices of obesity, glycaemic control, or respiratory function.
In addition, we found no difference in any outcomes when comparing an exercise referral scheme with an alternative physical activity intervention (for example, walking programmes) or with schemes plus an additional behavioural intervention. Although several trials included individuals with a pre-existing medical diagnosis (for example, hypertension, myocardial infarction, and depression), because outcomes were not separately reported for such individuals, we were unable to judge the effectiveness of an exercise referral scheme in these subgroups.
Strengths and limitations
We made every effort to reduce potential bias in this review. We used comprehensive electronic searches, including the searching of reference lists of included studies, and used predefined inclusion criteria which were applied by consensus across two or more reviewers.
We carefully selected exercise referral scheme studies on the basis that there was a clear statement of referral of participants by a primary care health professional to a third party exercise provider. The referral process of the scheme is, in itself, a key motivator and driver for individuals to take up and adhere to exercise interventions.29 Although this approach resulted in the exclusion of several trials investigating exercise intervention in primary care (for example, Elley,30 Lamb,31 Harland32, and Munro33), it allowed us to focus on the effectiveness of exercise referral schemes themselves.
We found several potential biases in the included trials. The methodological detail of trials was often poorly reported, in respect of allocation concealment and outcome blinding, and subsequently we saw potential for selection and assessment bias. With the exception of self reported physical activity, we found limited consistency in the collection and reporting of alternative outcomes across trials. Finally, we found considerable evidence of heterogeneity in the nature of exercise referral scheme interventions across studies, which could have contributed to the inconsistency in outcome findings.
Implications
NICE has previously commented that there was insufficient evidence to support the widespread adoption of exercise referral schemes, and recommended that the UK’s National Health Service (NHS) should only make these schemes available as part of a controlled trial.11 Although we have identified four additional trials since the NICE review, there remains very limited support for the potential role of exercise referral schemes on increasing physical activity and consequently improving public health. Arguably, such an uncertain impact provides a case for the disinvestment in exercise referral schemes. We also found little evidence of how the exercise referral scheme interventions sought to develop a sustainable active lifestyle in participants, as recommended in the NHS National Quality Assurance Framework.34 Although exercise referral scheme programmes in our review aimed to increase physical activity in the medium term to long term, they were typically based on only a 10-12 week period in leisure centres. With the exception of the Jolly and Murphy trials,26 27 the studies made little reference to the delivery, theories, or techniques of health behaviour change that typically underpin interventions to promote an increase in long term physical activity.35
This review has identified some key uncertainties. The impact of exercise referral schemes in people with a medical diagnosis, in terms of effects on prognostic outcomes such as blood pressure and serum lipids, remains unknown. Furthermore, are any short term gains in physical activity with exercise referral schemes maintained in the long term? Although others have argued to the contrary, we believe that there remains a need for further trials of these schemes.36 Future trials should consider incorporating theory driven interventions to complement an exercise referral scheme, compare the outcomes and costs associated with alternative approaches to physical activity promotion in primary care (for example, advice on physical activity delivered at the primary healthcare level), and report outcomes and costs in individuals with pre-existing medical diagnoses. This evidence is essential in the light of new NHS reform, for both service delivery (that is, councils) and general practitioner based commissioning; councils, through health and wellbeing boards, will be expected to work closely with new general practitioner commissioning consortiums and Public Health England to deliver public health.37
Conclusions
We found weak evidence of a short term increase in physical activity and reduction in the levels of depression of sedentary individuals after participation in an exercise referral scheme (typically a 10-12 week, leisure centre based programme) when compared with usual care. We did not find consistent evidence to support the benefit of exercise referral schemes for other outcomes (for example, health related quality of life). In view of this limited evidence, exercise referral schemes remain a potentially valuable primary care intervention for promoting physical activity. Particularly, since outcomes were not separately reported for individuals with a pre-existing diagnosis, we were unable to judge the effectiveness of an exercise referral scheme in these subgroups. High quality, randomised controlled trials are still needed to incorporate theory driven approaches to behaviour change (such as self determination, goal setting) and compare the outcomes and costs of exercise referral schemes with alternative, primary care based interventions that promote physical activity5, especially involving individuals with a pre-existing medical condition.
What is already known on this topic
Exercise referral schemes are a common model of physical activity promotion in primary care
Previous reviews have concluded that exercise referral schemes can increase the physical activity of sedentary adults in the short term
What this study adds
We found weak evidence supporting an association between exercise referral schemes and a short term increase in physical activity and a reduction in the levels of depression in sedentary individuals with and without pre-existing disease
Further trials should clarify whether exercise referral schemes offer important benefits in terms of health related outcomes and how these benefits compare with other primary care interventions to promote physical activity
Contributors: TGP coordinated the review, with RST (guarantor) and AT as principal investigators. TM developed the search strategy, in consultation with TGP, RST, AHT, KRF, and MH, and undertook the searches. TGP, RST, AHT, KRF, and MH screened abstracts and full papers against the inclusion criteria. TGP appraised the quality of the papers and abstracted data from them. TGP and RST analysed the data and drafted the review. All authors, including the Project Advisory Group (NA, JLC, CF, CG, NM, JS, PT) provided input to interpretation of findings, commented on various drafts of the chapters, and contributed to their editing.
Funding: This project was funded by the National Institute for Health Research Health Technology Assessment (NIHR HTA) programme (project number 08/72/01) (www.hta.ac.uk/).
Competing interests: All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: TGP, AHT, KRF, MH, PT, and RST have support from NIHR HTA for the submitted work; JS is chief medical officer of the Fitness Industry Association, which meets his receipted expenses, but the post attracts neither a salary nor fees; no non-financial interests that may be relevant to the submitted work.
Ethical approval: not required.
Data sharing: no additional data available.
Cite this as: BMJ 2011;343:d6462
Web Extra. Extra material supplied by the author
Web appendix 1: Literature search strategies
Web appendix 2: Summary of excluded studies from systematic review
Web figure 1: Meta-analysis of patients’ minutes spent in physical activity of at least moderate intensity per week, at 6-12 month follow-up
Web figure 2: Meta-analysis of patients’ estimated energy expenditure (kcal/kg per day; from self reports) during exercise referral schemes versus usual care, at 6-12 month follow-up
Web figure 3: Meta-analysis of patients’ total physical activity per week, at 6-12 month follow-up
Web figure 4: Meta-analysis of patients’ estimated energy expenditure (kcal/kg per day; from self reports during exercise referral schemes versus alternative physical activity interventions, at 6-12 month follow-up
Web table 1: Summary of physical fitness outcomes at follow-up
Web table 2: Summary of reported data for blood pressure and serum lipids at follow-up
Web table 3: Summary of weight and obesity measures at follow-up
Web table 4: Summary of reported data for respiratory function at follow-up
Web table 5: Summary of psychological outcomes at follow-up
Web table 6: Summary of reported data for health related quality of life at follow-up
References
- 1.Department of Health. At least five a week. Evidence on the impact of physical activity and its relationship to health. A report for the Chief Medical Officer. DH, 2004.
- 2.US Department of Health and Human Services. Physical activity guidelines for Americans. 2008. www.health.gov/paguidelines/pdf/paguide.pdf.
- 3.HSE. Health Survey for England—2008: physical activity and fitness. Summary of key findings. DH, 2009.
- 4.Fox K, Biddle S, Edmunds L, Bowler I, Killoran A. Physical activity promotion through primary health care in England. Br J Gen Pract 1997;47:367-9. [PMC free article] [PubMed] [Google Scholar]
- 5.National Institute for Clinical Excellence. Four commonly used methods to increase physical activity: brief interventions in primary care, exercise referral schemes, pedometers and community-based exercise programmes for walking and cycling. NICE, 2006.
- 6.British Heart Foundation National Centre. A toolkit for the design, implementation and evaluation of exercise referral schemes. Guidance for referring health professionals, exercise referral professionals and exercise referral scheme commissioners. www.bhfactive.org.uk/sites/Exercise-Referral-Toolkit/.
- 7.Sorensen JB, Kragstrup J, Kjaer K, Puggaard L. Exercise on prescription: trial protocol and evaluation of outcomes. BMC Health Serv Res 2007;7:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gusi N, Reyes MC, Gonzalez-Guerrero JL, Herrera E, Garcia JM. Cost-utility of a walking programme for moderately depressed, obese, or overweight elderly women in primary care: a randomised controlled trial. BMC Public Health 2008;8:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morgan O. Approaches to increase physical activity: reviewing the evidence for exercise-referral schemes. Public Health 2005;119:361-70. [DOI] [PubMed] [Google Scholar]
- 10.Williams N, Hendry M, France B, Lewis R, Wilkinson C. Effectiveness of exercise-referral schemes to promote physical activity in adults: systematic review. Br J Gen Pract 2007;57:979-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Institute of Health and Clinical Excellence. A rapid review of the effectiveness of ERS to promote physical activity in adults. NICE, 2006.
- 12.Sorensen J, Skovgaard T, Puggaard L. Exercise on prescription in general practice: a systematic review. Scand J Prim Health Care 2006;24:69-74. [DOI] [PubMed] [Google Scholar]
- 13.Pavey T, Anokye N, Taylor A, Trueman P, Moxham T, Fox KR, et al. The effectiveness and cost-effectiveness of exercise referral schemes: a systematic review and economic evaluation. 2011. www.hta.ac.uk/1815. [DOI] [PMC free article] [PubMed]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG, the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006-12. [DOI] [PubMed] [Google Scholar]
- 15.Khan K, ter Riet G, Glanville J, Sowden A, Kleijen J, eds. Undertaking systematic reviews of research on effectiveness: CRD’s guidance for those carrying out or commissioning reviews. 2nd ed. NHS Centre for Reviews and Dissemination, University of York, 2001.
- 16.The Cochrane Collaboration. Cochrane handbook for systematic reviews of interventions. 2011. www.cochrane-handbook.org.
- 17.Taylor AH, Fox KR. Effectiveness of a primary care exercise referral intervention for changing physical self-perceptions over 9 months. Health Psychol 2005;24:11-21. [DOI] [PubMed] [Google Scholar]
- 18.Taylor A, Doust J, Webborn N. Randomised controlled trial to examine the effects of a GP exercise referral programme in Hailsham, East Sussex, on modifiable coronary heart disease risk factors. J Epidemiol Community Health 1998:52:595-601. [DOI] [PMC free article] [PubMed]
- 19.Taylor AH. Evaluating GP exercise referral schemes. Findings from a randomised control study. University of Brighton. 1996.
- 20.Stevens W, Hillsdon M, Thorogood M, McArdle D. Cost-effectiveness of a primary care based physical activity intervention in 45-74 year old men and women: a randomised controlled trial. Br J Sports Med 1998;32:236-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harrison R, Roberts C, Elton P. Does primary care referral to an exercise programme increase physical activity one year later? A randomized controlled trial. J Public Health 2005;27:25-32. [DOI] [PubMed] [Google Scholar]
- 22.Isaacs A, Critchley J, Tai S, Buckingham K, Westley D, Harridge S, et al. Exercise evaluation randomised trial (EXERT): a randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only. Health Technol Assess 2007;11:1-185. [DOI] [PubMed] [Google Scholar]
- 23.Sorensen JB, Kragstrup J, Skovgaard T, Puggaard L. Exercise on prescription: a randomized study on the effect of counseling vs counseling and supervised exercise. Scand J Med Sci Sports 2008;18:288-97. [DOI] [PubMed] [Google Scholar]
- 24.Jolly K, Duda J, Daley A, Eves F, Mutrie N, Ntoumanis N, et al. Evaluation of a standard provision versus an autonomy promotive exercise referral programme: rationale and study design. BMC Public Health 2009;9:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murphy S, Raisanen L, Moore G, Edwards R, Linck P, Williams N, et al. A pragmatic randomised controlled trial of the Welsh National Exercise Referral Scheme: protocol for trial and integrated economic and process evaluation. BMC Public Health 2010;10:352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jolly K, Duda JL, Daley A, Ntoumanis N, Eves F, Rouse P, et al. An evaluation of the Birmingham exercise on prescription service: standard provision and a self-determination focused arm. Final Report, 2009.
- 27.Murphy S, Raisanen L, Moore G, Edwards R, Linck P, Hounsome N, et al. The evaluation of the National Exercise Referral in Wales. 2010. http://wales.gov.uk/docs/caecd/research/101104nationalexerciseschemeen.pdf.
- 28.O’Donovan G, Blazevich AJ, Boreham C, Cooper AR, Crank H, Ekelund U, et al. The ABC of physical activity for health: a consensus statement from the British Association of Sport and Exercise Sciences. J Sports Sci 2010;28:573-91. [DOI] [PubMed] [Google Scholar]
- 29.Taylor AH. The role of primary care in promoting physical activity. In: Riddoch C, McKenna J, eds. Perspectives on health and exercise. MacMillian Press, 2003.
- 30.Elley CR, Kerse N, Arroll B, Robinson E. Effectiveness of counselling patients on physical activity in general practice: cluster randomised controlled trial. BMJ 2003;326:793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lamb S, Bartlett H, Ashely A, Bird W. Can lay-led walking programmes increase physical activity in middle aged adults? A randomised controlled trial. J Epidemiol Community Health 2002;56:246-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harland J, White M, Drinkwater C, Chinn D, Farr L, Howel D. The Newcastle exercise project: a randomised controlled trial of methods to promote physical activity in primary care. BMJ 1999;319:828-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Munro J, Nicholl J, Brazier J, Davey R, Cochrane T. Cost effectiveness of a community based exercise programme in over 65 year olds: cluster randomised trial. J Epidemiol Community Health 2004;58:1004-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Department of Health. Exercise referral systems: a national quality assurance framework. DH, 2001.
- 35.Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol 2009;28:690-701. [DOI] [PubMed] [Google Scholar]
- 36.Sowden S, Raine R. Running along parallel lines: how political reality impedes the evaluation of public health interventions. A case study of exercise referral schemes in England. J Epidemiol Community Health 2008;62:835-41. [DOI] [PubMed] [Google Scholar]
- 37.Limb M. Government’s plans on public health are too vague, experts say. BMJ 2011;342: published online 18 February.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix 1: Literature search strategies
Web appendix 2: Summary of excluded studies from systematic review
Web figure 1: Meta-analysis of patients’ minutes spent in physical activity of at least moderate intensity per week, at 6-12 month follow-up
Web figure 2: Meta-analysis of patients’ estimated energy expenditure (kcal/kg per day; from self reports) during exercise referral schemes versus usual care, at 6-12 month follow-up
Web figure 3: Meta-analysis of patients’ total physical activity per week, at 6-12 month follow-up
Web figure 4: Meta-analysis of patients’ estimated energy expenditure (kcal/kg per day; from self reports during exercise referral schemes versus alternative physical activity interventions, at 6-12 month follow-up
Web table 1: Summary of physical fitness outcomes at follow-up
Web table 2: Summary of reported data for blood pressure and serum lipids at follow-up
Web table 3: Summary of weight and obesity measures at follow-up
Web table 4: Summary of reported data for respiratory function at follow-up
Web table 5: Summary of psychological outcomes at follow-up
Web table 6: Summary of reported data for health related quality of life at follow-up