Abstract
A 38-year-old man visited our emergency department presenting with a 6-day persistent fever. The man had undergone an orthodontic procedure 7 days prior to the visit. He had a fever with a temperature of 38.2℃ and a diastolic murmur (grade III) was detected at the left sternal border. Reddish-brown lines beneath the nails were present, and raised lesions which were red and painful were detected on the soles of the patient's feet. Laboratory findings showed an elevated inflammatory marker. Transthoracic and transesophageal echocardiograms, showed a bicuspid aortic valve, and moderate aortic regurgitation and vegetation were noted. Treatment with antibiotics was given, but 4 days later, a 12 lead electrocardiogram revealed complete atrioventricular (AV) block. Immediately, a temporary pacemaker was inserted, and the following day an aortic valve replacement was performed. Intraoperative findings revealed a fistula around the AV node. He has suffered no subsequent cardiac events during the follow-up.
Keywords: Endocarditis, Atrioventricular block, Aortic valve
Introduction
Bicuspid aortic valve is the most common congenital heart disease, occurring in 0.9-2.0% of the general population.
In most cases, heart function is maintained normally, and as a result, there are many cases in which it is overlooked until the valve is functionally impaired. Common complications of bicuspid aortic valve are aortic stenosis or regurgitation, aortic dissection and infective endocarditis.1) In most cases, the symptoms appear during adulthood. Of the latter cases, infective endocarditis accounts for a high degree of the incidence of complications such as valve perforation, valve destruction, abscesses, and heart failure, and the resulting mortality is high. An early diagnosis and surgical treatment would therefore be mandatory for these cases.2)
We experienced a patient with bicuspid aortic valve who developed a complete atrioventricular (AV) block due to the formation of a fistula during the antibiotic treatment for infective endocarditis. The patient had improved through the early surgical treatments. Here, we report our case with a review of the literature.
Case
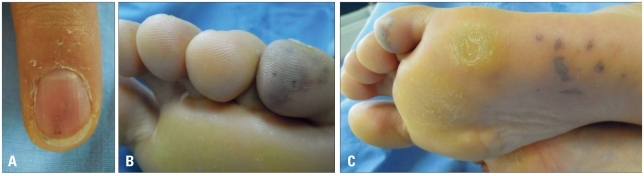
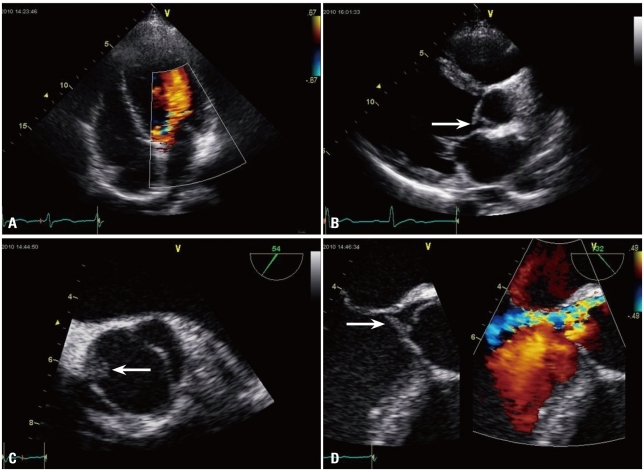
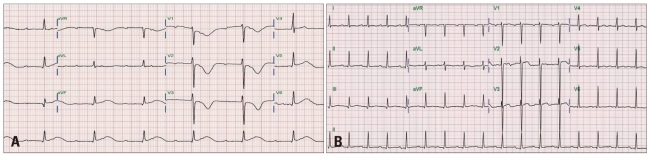
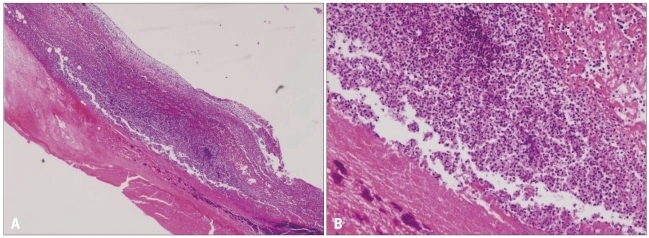
A 38-year-old man visited our emergency department presenting with a 6-day persistent fever. His medical history included hypertension. He reported having undergone an orthodontic procedure 7 days prior to his visit, and had subsequently suffered from a mild fever which was treated with amoxicillin and non steroid anti inflammatory drugs. On physical examination, he had a fever with a temperature of to 38.2℃ and his blood pressure was normal. A diastolic murmur (grade III) was detected at the third intercostals space along left sternal border for the first time. Reddish-brown lines beneath the nail were present, and raised lesions which were red and painful were detected on the soles of the patient's feet (Fig. 1). A chest X-ray did not show cardiomegaly or pulmonary edema, and a 12-lead electrocardiogram revealed a regular sinus rhythm with a mean rate of 81 beats/min. On admission, his hematological and biochemical values were within their normal ranges, with the exception of the erythrocyte sedimentation rate at 29 mm/h (normal, 0-10 mm/h) and C-reactive protein levels at 13.9 mg/dL (normal, 0-0.3 mg/dL). Three blood cultures were positive for gram positive Staphylococcus aureus, which was sensitive to oxacillin. Transthoracic echocardiography demonstrated normal left ventricular systolic function (ejection fraction 65%), but moderate aortic regurgitation and bicuspid aortic valve were noted. The echocardiogram also revealed vegetation on the bicuspid aortic valve. A transesophageal echocardiogram also revealed vegetation (0.8 × 0.8 cm) on the bicuspid aortic valve, but an abscess was not detected (Fig. 2). The patient was then treated intravenously with vancomycin (2 g/day), gentamicin (200 mg/day), and ceftriaxone (2 g/day), and with diuretics and angiotensin-converting enzyme inhibitors. 4 days later, the patient showed a resolution of fever, but he had dizziness and a 12-lead electrocardiogram (ECG) revealed complete AV block (Fig. 3A). Transthoracic echocardiography showed enlarged vegetation of the aortic valve with moderate aortic regurgitation and newly developed mild mitral regurgitation. Immediately, a temporary pacemaker was inserted, and the following day an aortic valve replacement was performed. Intraoperative findings revealed a fistula beneath the right cusp. Surgical pathology examination of the excised valve showed two semilunar leaflets, one of which demonstrated vegetation (1.5 × 1.3 cm) (Fig. 4). Examination also detected acute inflammation (Fig. 5). The postoperative course was uneventful. On the 6th post operative day, an ECG showed 1st degree AV block and repeated blood cultures yielded negative results. After 1 month, an ECG showed a normal sinus rhythm (Fig. 3B). The patient has suffered no cardiac events during follow-up.
Fig. 1.
A: Reddish-brown lines beneath the nails. B and C: Painful red raised lesion on the soles of the feet.
Fig. 2.
Transthoracic and transesophageal echocardiography. A: Moderate aortic regurgitation on apical view. B: The presence of vegetation (arrow) in the aortic valve tip on parasternal long axis view. C: Two leaflets seen in the aortic valve on a transesophageal echocardiogram. The vegetation (arrow) is seen in the left leaflet. D: The presence of vegetation (arrow) in the aortic valve tip on a transesophageal echocardiogram. The presence of aortic regurgitation seen on Doppler echocardiogram.
Fig. 3.
Electrocardiogram. A: Electrocardiogram on hospital day 4: complete atrioventricular block. B: Electrocardiogram on post-op day 30: normal sinus rhythm.
Fig. 4.
Intraoperative and surgical pathology finding. A: Intraoperative finding: the presence of a fistula (arrow) around the atrioventricular node below the left cusp. B: Surgical pathology finding: two leaflets seen in the aortic valve. A 1.5 × 1.3 cm sized vegetation seen in a leaflet.
Fig. 5.
Microscopic finding. Histologic exam shows aortic valve leaflet vegetation with many inflammation cell and necrotic tissue (A, H&E stain 50×) (B, H&E stain 200×).
Discussion
Bicuspid aortic valve disease is the most common congenital heart defect, having an incidence in the general population of 0.9 to 2.0%, and a frequency of 54% of all patients aged > 15 years with valvular aortic stenosis. It shows a male predilection with a male-to-female ratio of approximately 3 : 1.1),3),4)
Although the clinical presentation of patients with bicuspid aortic valve can vary from severe valve disease in infancy to asymptomatic valve disease in old age, symptoms typically develop in adulthood.5) In association with the functions of aortic valve, the clinical symptoms may include stenosis or regurgitation or symptoms may also occur as a result of aortic dissection or endocarditis.1),5) In the study case, the patient maintained a normal daily life, and first received a diagnosis of infective endocarditis during adulthood.
According to earlier studies, infective endocarditis has been reported to occur in 7-25% of the total cases of bicuspid aortic valve. It is probable, however, that this number is an overestimate due to reporting bias. Recent studies have also shown that the annual incidence of infective endocarditis is estimated at approximately 2%.5),6) For these reasons, according to the practice guidelines of American College of Cardiology/American Heart Association, the prophylactic use of antibiotics for treatment of bacterial endocarditis is not any longer recommended in patients with bicuspid aortic valve.7) Infective endocarditis commonly occurs in younger patients (mean age, 38-53 years), and mortality resulting from it has been reported to be approximately 9%. In cases of infective endocarditis occurring in patients with bicuspid aortic valve, as opposed to infective endocarditis occurring in other native valves, valve perforation, valve destruction, heart failure and valvular, perivalvular or myocardial abscess are more commonly noted.1),6) Once a perivalvular abscess develops, the infection progresses into the his bundle or the AV node in 45% of total patients. As a result, bundle-branch or AV blocks may occur.8-10) In the study case, a perivalvular fistula developed and an infection occurred in the AV node. This was followed by the development of a complete AV block.
In cases of aortic valve endocarditis associated with a perivalvular abscess, the mortality rate and incidence of recurrent infection are markedly increased. Most of these cases therefore need surgical treatment. Early diagnosis and surgical treatment of a perivalvular abscess are essential in preventing severe valvular destruction and improving the survival rate.2)
In conclusion, it is highly probable that severe complication will occur in patients with bicuspid aortic valve who develop infective endocarditis. Owing to this, there are many cases in which surgical treatment is necessary. Special attention should therefore be paid to these cases.
In the study case, the patient had not been diagnosed with bicuspid aortic valve, and had maintained a normal daily life without notable symptoms. Following the onset of infective endocarditis, a complete AV block occurred due to a perivalvular fistula. The symptoms were improved with early surgical management and there have been no subsequent cardiac events. We successfully treated a rare case of severe infective endocarditis of bicuspid aortic valve complicated with complete AV block by urgent operation. Here, we report our case with a review of the literature.
References
- 1.Yener N, Oktar GL, Erer D, Yardimci MM, Yener A. Bicuspid aortic valve. Ann Thorac Cardiovasc Surg. 2002;8:264–267. [PubMed] [Google Scholar]
- 2.Knosalla C, Weng Y, Yankah AC, Siniawski H, Hofmeister J, Hammerschmidt R, Loebe M, Hetzer R. Surgical treatment of active infective aortic valve endocarditis with associated periannular abscess--11 year results. Eur Heart J. 2000;21:490–497. doi: 10.1053/euhj.1999.1877. [DOI] [PubMed] [Google Scholar]
- 3.Ward C. Clinical significance of the bicuspid aortic valve. Heart. 2000;83:81–85. doi: 10.1136/heart.83.1.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kahveci G, Bayrak F, Pala S, Mutlu B. Impact of bicuspid aortic valve on complications and death in infective endocarditis of native aortic valves. Tex Heart Inst J. 2009;36:111–116. [PMC free article] [PubMed] [Google Scholar]
- 5.Siu SC, Silversides CK. Bicuspid aortic valve disease. J Am Coll Cardiol. 2010;55:2789–2800. doi: 10.1016/j.jacc.2009.12.068. [DOI] [PubMed] [Google Scholar]
- 6.Lamas CC, Eykyn SJ. Bicuspid aortic valve--A silent danger: analysis of 50 cases of infective endocarditis. Clin Infect Dis. 2000;30:336–341. doi: 10.1086/313646. [DOI] [PubMed] [Google Scholar]
- 7.Wilson W, Taubert KA, Gewitz M, Lockhart PB, Baddour LM, Levison M, Bolger A, Cabell CH, Takahashi M, Baltimore RS, Newburger JW, Strom BL, Tani LY, Gerber M, Bonow RO, Pallasch T, Shulman ST, Rowley AH, Burns JC, Ferrieri P, Gardner T, Goff D, Durack DT American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee; American Heart Association Council on Cardiovascular Disease in the Young; American Heart Association Council on Clinical Cardiology; American Heart Association Council on Cardiovascular Surgery and Anesthesia; Quality of Care and Outcomes Research Interdisciplinary Working Group. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 2007;116:1736–1754. doi: 10.1161/CIRCULATIONAHA.106.183095. [DOI] [PubMed] [Google Scholar]
- 8.Graupner C, Vilacosta I, SanRomán J, Ronderos R, Sarriá C, Fernández C, Mújica R, Sanz O, Sanmartín JV, Pinto AG. Periannular extension of infective endocarditis. J Am Coll Cardiol. 2002;39:1204–1211. doi: 10.1016/s0735-1097(02)01747-3. [DOI] [PubMed] [Google Scholar]
- 9.Arnett EN, Roberts WC. Valve ring abscess in active infective endocarditis. Frequency, location, and clues to clinical diagnosis from the study of 95 necropsy patients. Circulation. 1976;54:140–145. doi: 10.1161/01.cir.54.1.140. [DOI] [PubMed] [Google Scholar]
- 10.Bacchion F, Cukon S, Rizzoli G, Gerosa G, Daliento L, Thiene G, Basso C. Infective endocarditis in bicuspid aortic valve: atrioventricular block as sign of perivalvular abscess. Cardiovasc Pathol. 2007;16:252–255. doi: 10.1016/j.carpath.2006.11.001. [DOI] [PubMed] [Google Scholar]