Abstract
Sudden infant death syndrome (SIDS) is defined as the sudden death of an infant under one year of age which remains unexplained after a thorough case investigation, including performance of a complete autopsy, examination of the death scene and review of the clinical history. SIDS is one of the leading causes of infant mortality and occurs from the first month, until the first year of life for newborns and infants.
The aim of this review was to identify and examine risk factors responsible for causing the sudden infant death and to propose certain measures in order to protect newborns and infants from sudden death. The potential factors that contribute to the occurrence of SIDS include inadequate prenatal care, low birth weight (<2499gr), premature infants, intrauterine growth delay, short interval between pregnancies and maternal substance use (tobacco, alcohol, opiates). Moreover, factors related to infant’s sleep environment such as the prone or side sleeping position and thick coverlet increase the risk of sudden death in infants. Also, the combination of risk factors such as that of prone sleeping position and soft bed mattress are linked to a 20-fold increased risk of death. Finally, polymorphisms in the serotonin transporter gene (5-HTT), viral respiratory infections, long Q-T (responsible for the presence of fatal arrhythmia) are related to the SIDS.
Literature review indicates that each individual risk factor contributes to the appearance of SIDS and the establishment of certain protective measures for parents and health professionals has reduced its prevalence. But the precise identification of the SIDS causes and how these contribute to the occurrence of sudden death in neonates and infants, remains a challenge for health professionals.
Keywords: sudden death, newborn, infant, risk factors, prevention, review
Willinger et al., (1991) first described the sudden infant death syndrome (SIDS), as "the sudden death of an infant under one year of age which remains unexplained after a thorough case investigation, including performance of a complete autopsy, examination of the death scene and review of the clinical history"1. SIDS appears in newborns and infants, without any indication that their life is in danger2.
The annual incidence rate of SIDS in '80s was 1.53% per 1000 live births in the USA, while in 2004 it decreased to 0.51%3. Deaths due to SIDS, in the general population amounted to 2200 per year4. Moreover, SIDS is classified by the Center of Disease Control (CDC) as the third leading cause of overall infant mortality in the USA5.
SIDS occurs between the first month and before the first year of an infant's life. Infants aged 2-4 months endanger greater risk of SIDS, while most deaths occur in infants during the sixth month of their life6.
The differential diagnosis of SIDS in neonates and infants includes asphyxiation or drowning, heart disease (arrhythmia), electrolyte disturbances or dehydration, poisoning, trauma, infections (pneumonia, sepsis, meningitis) and congenital metabolic disorders7.
Few researchers proposed the specification of diagnostic criteria for sudden death in neonates. Beckwith B. (2003), proposed three categories related to SIDS, which classified the neonate or infant in the relevant category. The first category includes infants aged from three weeks to eight months, without the previous appearance of SIDS in the family environment, infants without evidence of abuse, trauma or accident and neonates with a significant degree of anxiety in the thymus, adrenal glands or other organs. The second category consists of infants who exhibit the criteria of the above category, except those that are >1 year old, who have history of sudden death in the family environment and inflammatory disorders. Finally, the last category concerns cases of deaths of infants, which made an autopsy after their death1.
According to the literature review, the possible risk factors that contribute to the incidence of SIDS are demographic, relevant to the pregnancy and the birth, the sleep environment, genetic, infective and cardiovascular.
Demographic factors
Low socioeconomic status, maternal young age, low maternal education and single marital status, are associated with the occurrence of SIDS1. Infants who did not live with their father were 50% higher sensitive in sudden death, unlike those who grew up with their father8. Also, several studies have reported that male infants present 30-50% more chances to die from sudden death9,10.
Factors related with pregnancy and birth
Pregnancy related factors (mothers with inadequate prenatal care11, intrauterine growth retardation, short intervals during pregnancies, second pregnancy or after) are connected with increased incidence of SIDS. The sudden death of a second child in a family comes 80-90% natural. Also, birth related factors such as premature 10 and low birth weight infants (infants that were borned at 1000-1499 gr are threatened 4 times higher to die from SIDS and those borned at 1500-2499 gr are threatened 3 times more respectively)12,13.
Substances abuse like tobacco, drugs and alcohol, in pregnancy period, are correlated with SIDS. Tobacco use in pregnancy affects the intrauterine fetal development. During an antismoking campaign, infants borned by mothers who smoke during pregnancy, have 3 times more risk to appear SIDS before the campaign14. The avoidance of smoking during pregnancy estimated that could have reduce SIDS cases by almost 21%.15 The effect of passive smoking was higher in infants <10 weeks and seems to doubles the possibility of SIDS16. Whereas, a home environment free of tobacco use, reduces the chances of SIDS6.
The chances of sudden death increased by 2-5 times in neonates whose mother have used drugs (opiates)17,18, 6-8 times in cases of maternal alcohol use (particularly the first 3 months of pregnancy), 2-8 times when mothers had drunk alcohol in the last 24 hours before the neonate death19. Infant's siblings with fetal alcohol syndrome reported 10 times more chances of sudden death20.
Sleep environment
The environment of sleep concerns the infant's sleep position, the bed's quality, the sharing of the bed and the occurrence of smoking during infant's sleep.
Newborns vulnerable to sudden death are those who change position during sleep and remain in prone position21. The SIDS risk was 37 times higher at infants who changed position during sleep compare to those who remained in this position throughout the whole sleep duration22,23. Infants who sleep in lateral position provoke twice the risk of sudden death, in contrast to those sleeping in supine position24. Instantly, many parents and health professionals may notice that supine sleeping position impairs neonatal respiratory system and increases the risk of gastro-esophageal reflux25.
Soft, old pillows and sleeping mats from polystyrene have been shown to increase by 2-3 times the risk of sudden death9,17,25. Also, heavy comforters covering the baby's head, implicate to be associated with sudden death26,27. When the newborn's body temperature increases, due to increased room temperature, fever, sweating or excessive clothing the chances of SIDS is increased16. While combinations of risk factors such as the prone position and soft layer or increased body temperature and sleep in prone position, are associated with the risk of sudden death, 2 and 6 times, respectively28,29.
Also, infant's sharing bed with parents or siblings (twins) has been implicated with a high risk of SIDS30. Babies under <13 weeks who sleep with their parents are in greater risk13.
Genetic factors
Polymorphism serotonin transporter gene (5-HTT) was observed at infants who developed sudden death. This gene is affected by the functions of the autonomic nervous system31.
Infections
Viral respiratory infections are mainly responsible for the occurrence of sudden death. Mild degree of respiratory viral infection was observed by investigators in cases of sudden death infants up to 80%32.
Toxins produced from bacteria like s.aureus and e.coli, pose a particular risk to the life of infant. The toxins of such bacteria are absorbed by mucosal surfaces, or indicate an upcoming bacteremia, affecting principally the cardiovascular and respiratory systems, creating "channels" in cell membranes, which disrupts the smooth ions33.
Cardiovascular factors
Long Q-T syndrome is associated with changes in the Na+/K+ pump. Abnormalities shown in ion heart channels, are related to the sudden death and hence the baby is at risk of potentially fatal arrythmia34. According to American Academy of Pediatrics, rare genetic disorders are result to mutations of the cardiac tissue, like fatal loss of cardiac function35.
Protective measures against SIDS
Although the causes of SIDS are not precisely identified, it seems that the above factors have positive effects in sudden death. American Academy of Pediatrics has already established protective measures to decrease the incidence of SIDS. These measures are:
The position of the infant at bedtime is the most modifiable factor. It is suggested that the appropriate sleep position for infants is the supine one. The side sleeping position is a risk factor for sudden death for this reason it is not recommended35.
It is preferred to avoid the high temperature of the infant, keeping tolerable room temperature, avoiding excessive clothing35.
It is recommended that the sleep surface should be firm and hard30.
Research studies confirm that the pacifiers help to reduce the risk of sudden death when they are administered at the beginning of sleep. The American Academy of Pediatrics recommends that parents should provide pacifiers to their infants from the first month of their life35. However, pacifier use is implicated in the creation of medium otitidas37 and airway obstruction37.
The baby crib is recommended to be located in the same room with the parent's bed and is advised not to make changes in the environment of sleeping infants, at least for the first year of the infant’s life38,39.
Immunization in time seems also to be protective from SIDS40.
The education of parents and health professionals are equally important, contributing decisively in reducing the risk of SIDS41.
Conclusions
Concluding, the SIDS seems to be a multifunctional syndrome, without a clear etiologic mechanism. For this reason, exploring the way each risk factor contributes to the occurrence of sudden death in newborns and the establishment of certain protective measures for parents and health professionals, still remain a challenge.
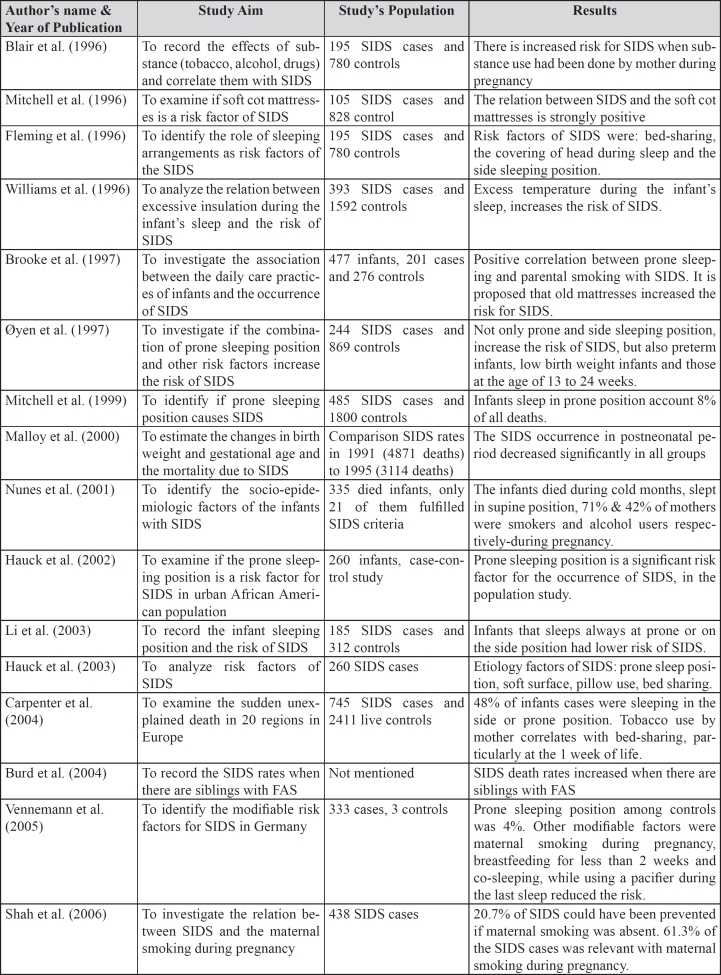
Table 1. Characteristics of the research studies (during the period 1996-2010), that introduced in this review.
SIDS: Sudden Infant Death Syndrome, FAS: Fetal Alcohol Syndrome
References
- 1.Beckwith JB. Defining the Sudden Infant Death Syndrome. Arch Pediatr Adolesc Med. 2003;157:286–290. doi: 10.1001/archpedi.157.3.286. [DOI] [PubMed] [Google Scholar]
- 2.Nunes ML, Pinho AP, Aerts D, Santacute AA, Martins MP, Costa JC. Sudden infant death syndrome: clinical aspects of an underdiagnosed disease. J Pediatr (Rio J) 2001;77:29–34. [PubMed] [Google Scholar]
- 3.Sids.org [homepage on the Internet]. U.S. Annual SIDS Rate per 1000 Live Births. American Sids Institute; [cited 2010 August 18]. Available from: http://www.sids.org/nannualrates.htm. [Google Scholar]
- 4.Adams SM, Good MW, Defranco GM. Sudden infant death syndrome. Am Fam Physician. 2009;79:870–874. [PubMed] [Google Scholar]
- 5.Cdc.gov [homepage on the Internet]. Center of Disease Control (CDC). Sudden Infant Death Syndrome. Center of Disease Control (CDC); [updated 2009 May 17; cited 2010 August 14]. Available from: http://www.cdc.gov/SIDS/ [Google Scholar]
- 6.Hunt CE, Hauck FR. Sudden infant death syndrome. CMAJ. 2006;174:1861–1869. doi: 10.1503/cmaj.051671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Academy of Pediatrics Distinguishing sudden infant death syndrome from child abuse fatalities. Pediatrics. 2006;118:421–427. doi: 10.1542/peds.2006-1245. [DOI] [PubMed] [Google Scholar]
- 8.Mathews TJ, Menacker F, MacDorman MF, US Centers for Disease Control and Prevention National Center for Health Statistics Infant mortality statistics from the 2002 period: linked birth/infant death data set. Natl Vital Stat Rep. 2004;53:1–29. [PubMed] [Google Scholar]
- 9.Brooke H, Gibson A, Tappin D, Brown H. Caseâcontrol study of sudden infant death syndrome in Scotland, 1992â5. BMJ. 1997;314:1516–1520. doi: 10.1136/bmj.314.7093.1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vennemann MM, Findeisen M, Butterfass-Bahloul T, Jorch G, Brinkmann B, Köpcke W, et al. Modifiable risk factors for SIDS in Germany: results of GeSID. Acta Paediatr. 2005;94:655–660. doi: 10.1111/j.1651-2227.2005.tb01960.x. [DOI] [PubMed] [Google Scholar]
- 11.Hauck FR, Moore CM, Herman SM, Donovan M, Kalelkar M, Christoffel KK, et al. The contribution of prone sleeping position to the racial disparity in sudden infant death syndrome: the Chicago Infant Mortality Study. Pediatrics. 2002;110:772–780. doi: 10.1542/peds.110.4.772. [DOI] [PubMed] [Google Scholar]
- 12.Malloy MH, Freeman DH. Birth weight- and gestational agespecific sudden infant death syndrome mortality: United States, 1991 versus 1995. Pediatrics. 2000;105:1227–1231. doi: 10.1542/peds.105.6.1227. [DOI] [PubMed] [Google Scholar]
- 13.Carpenter RG, Irgens LM, Blair PS, England PD, Fleming P, Huber J, et al. Sudden unexplained infant death in 20 regions in Europe: case control study. Lancet. 2004;363:185–191. doi: 10.1016/s0140-6736(03)15323-8. [DOI] [PubMed] [Google Scholar]
- 14.Mitchell EA, Milerad J. International consultation on environmental tobacco smoke (ETS) and child health. Geneva: World Health Organization; 1999. Smoking and sudden infant death syndrome; pp. 105–129. [Google Scholar]
- 15.Shah T, Sullivan K, Carter J. Sudden infant death syndrome and reported maternal smoking during pregnancy. Am J Public Health. 2006;96:1757–1759. doi: 10.2105/AJPH.2005.073213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Britton J. Passive smoking damages children's health. Practitioner. 2010;254:27–30. [PubMed] [Google Scholar]
- 17.Hauck FR. Changing epidemiology. In: Byard RW, Krous FR, editors. Sudden infant death syndrome. Problems, progress and possibilities, pages 31â57. London: Arnold; 2004. [Google Scholar]
- 18.Blair PS, Fleming PJ, Bensley D, Smith I, Bacon C, Taylor E, et al. Smoking and the sudden infant death syndrome: results from the 1993â5 caseâcontrol inquiry into stillbirths and deaths in infancy. BMJ. 1996;313:195–198. doi: 10.1136/bmj.313.7051.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Golding J. Sudden infant death syndrome and parental smoking- a literature review. Paediatr Perinat Epidemiol. 1997;11:67–77. doi: 10.1046/j.1365-3016.1997.d01-12.x. [DOI] [PubMed] [Google Scholar]
- 20.Burd L, Klug MG, Martsolf JT. Increased sibling mortality in children with fetal alcohol syndrome. Addict Biol. 2004;9:179–186. doi: 10.1080/13556210410001717088. [DOI] [PubMed] [Google Scholar]
- 21.Task Force on Sudden Infant Death Syndrome The changing concept of sudden infant death syndrome: diagnostic coding shifts, controversies regarding the sleeping environment, and new variables to consider in reducing risk. Pediatrics. 2005;116:1245–1255. doi: 10.1542/peds.2005-1499. [DOI] [PubMed] [Google Scholar]
- 22.Øyen N, Markestad T, Skjærven R, Irgens LM, Helweg-Larsen K, Alm B, et al. Combined effects of sleeping position and prenatal risk factors in sudden infant death syndrome: the Nordic Epidemiological SIDS Study. Pediatrics. 1997;100:613–621. doi: 10.1542/peds.100.4.613. [DOI] [PubMed] [Google Scholar]
- 23.Mitchell EA, Thach BT, Thompson JM, Williams S. Changing infant's sleep position increases risk of sudden infant death syndrome. New Zealand Cot Death Study. Arch Pediatr Adolesc Med. 1999;153:1136–1141. doi: 10.1001/archpedi.153.11.1136. [DOI] [PubMed] [Google Scholar]
- 24.Li DK, Petitti DB, Willinger M, McMahon R, Odouli R, Vu H, et al. Infant sleeping position and the risk of sudden infant death syndrome in California, 1997â2000. Am J Epidemiol. 2003;157:446–445. doi: 10.1093/aje/kwf226. [DOI] [PubMed] [Google Scholar]
- 25.Mitchell EA, Scragg l, Clements M. Soft cot mattresses and the sudden infant death syndrome. N Z Med J. 1996;109:206–207. [PubMed] [Google Scholar]
- 26.Markestad T, Skadberg B, Hordvik E, Morild I, Irgens LM. Sleeping position and sudden infant death syndrome (SIDS): effect of an intervention programme to avoid prone sleeping. Acta Paediatr. 1995;84:375–358. doi: 10.1111/j.1651-2227.1995.tb13653.x. [DOI] [PubMed] [Google Scholar]
- 27.Fleming PJ, Blair PS, Bacon C, Bensley D, Smith I, Taylor E, et al. Environment of infants during sleep and the risk of sudden infant death syndrome: results of 1993â95 study for confidential inquiry into stillbirths and deaths in infancy. BMJ. 1996;313:191–195. doi: 10.1136/bmj.313.7051.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hauck FR, Herman SM, Donovan M, Iyasu S, Merrick Moore C, Donoghue E, et al. Sleep environment and the risk of sudden infant death syndrome in an urban population: the Chicago Infant Mortality Study. Pediatrics. 2003;111:1207–1214. [PubMed] [Google Scholar]
- 29.Williams SM, Taylor BJ, Mitchell EA. Sudden infant death syndrome:insulation from bedding and clothing and its effect modifiers. Int J Epidemiol. 1996;25:366–375. doi: 10.1093/ije/25.2.366. [DOI] [PubMed] [Google Scholar]
- 30.Mitchell EA. Risk factors for SIDS. BMJ. 2009;339:b3466. doi: 10.1136/bmj.b3466. [DOI] [PubMed] [Google Scholar]
- 31.Hunt CE. Gene-environment interactions: implications for sudden unexpected deaths in infancy. Arch Dis Child. 2005;90:48–53. doi: 10.1136/adc.2004.051458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cutz E, Jackson A. Airway inflammation and peripheral chemoreceptors. In: Byard RW, Krous HF, editors. Sudden infant death syndrome. Problems, progress and possibilities. London: Arnold; 2001. pp. 156–181. [Google Scholar]
- 33.Morris JA, Harrison L, Brodison A, Lauder R. Sudden infant death syndrome and cardiac arrhythmias. Future Cardiol. 2009;5:201–207. doi: 10.2217/14796678.5.2.201. [DOI] [PubMed] [Google Scholar]
- 34.Franco P, Szliwowski H, Dramaix M, Kahn A. Decreased autonomic responses to obstructive sleep events in future victims of sudden infant death syndrome. Pediatr Res. 1999;46:33–39. doi: 10.1203/00006450-199907000-00006. [DOI] [PubMed] [Google Scholar]
- 35.American Academy of Pediatrics The changing concept of sudden infant death syndrome: diagnostic coding shifts, controversies regarding the sleeping environment, and new variables to consider in reducing risk. Pediatrics. 2005;116:1245–1255. doi: 10.1542/peds.2005-1499. [DOI] [PubMed] [Google Scholar]
- 36.Marter A, Agruss JC. Pacifiers: an update on use and misuse. J Spec Pediatr Nurs. 2007;12:278–285. doi: 10.1111/j.1744-6155.2007.00126.x. [DOI] [PubMed] [Google Scholar]
- 37.Simkiss DE, Sheppard I, Pal BR. Airway obstruction by a child's pacifier-could flange design be safer? Eur J Pediatr. 1998;157:252–254. doi: 10.1007/s004310050806. [DOI] [PubMed] [Google Scholar]
- 38.American Academy of Pediatrics. Task Force on Infant Sleep Position and Sudden Infant Death Syndrome Changing concepts of sudden infant death syndrome: implications for infant sleeping environment and sleep position. Pediatrics. 2000;105:650–656. doi: 10.1542/peds.105.3.650. [DOI] [PubMed] [Google Scholar]
- 39.Jorch G. Prevention of SIDS. Monatsschr Kinderheilkd. 2003;151:514–519. [Google Scholar]
- 40.Vennemann MM, Hoffgen M, Bajanowski T, Hense HW, Mitchell EA. Do immunisations reduce the risk for SIDS? A metaanalysis. Vaccine. 2007;25:4875–4879. doi: 10.1016/j.vaccine.2007.02.077. [DOI] [PubMed] [Google Scholar]
- 41.Yikilkan H, Unalan PC, Cakir E, Ersu RH, Cifcili S, Akman M, et al. Sudden Infant Death Syndrome: How Much Mothers and Health Professionals Know. Pediatr In. 2010 Jul 5; doi: 10.1111/j.1442-200X.2010.03202.x. Accepted Article; doi: 10.1111/j.1442-200X.2010.03202.x. [DOI] [PubMed] [Google Scholar]