Abstract
Anaphylactic reactions in the peri-operative period are often serious and potentially life-threatening conditions, involving multiple organ systems in which the clinical manifestations are the consequence of the release of preformed mediators from mast cells and basophils. Anaphylaxis is an immune mediated type I allergic reaction following the massive release of mediators from mast cells and basophils as a response to an allergen. Anaphylactoid reactions are defined as those reactions that produce the same clinical picture with anaphylaxis but are not IgE mediated, occur through a direct nonimmune-mediated release of mediators from mast cells and/or basophils or result from direct complement activation. The occurrence of these reactions during anesthesia, although quite rare, remains a major concern for the anesthesiologists. Thus, the need for systematic screening before surgery and the awareness and expert advice to anaesthesiologists seems to be very critical.
Keywords: anaphylaxis, anaphylactoid reactions, perioperative period, review
Anaphylaxis and anaphylactoid reactions in the peri-operative period are often serious and potentially life-threatening conditions that affect multiple organ systems1. These reactions although quite rare, with an incidence of less than 1 in 10000-200002 anaesthesias and 1 in 6500 administrations of neuromuscular blocking agents (NMBAs), remain a major area of concern and a source of continual debate among anesthesiologists3. Clinical practice guidelines published by Associations of Anaesthetists provide a data-supported approach to the management of anaphylaxis during anaesthesia4.
According to the nomenclature of the European Academy of Allergology and Clinical Immunology in 2001 and the updated form in 2003, allergic reactions in the peri-operative period are divided in type I allergic and non-allergic hypersensitivity reactions3,5.
The true incidence of these reactions is difficult to be established, as many of them are not diagnosed or not reported and the estimated frequency varies considerably between epidemiological studies from different countries6,7.8. However, epidemiological studies conducted during the last years provided some evidence of the their incidence. Moreover, they explored the underlying mechanisms of both allergic and non-allergic reactions and the possibility to identify the patients at risk as well as the drugs which are often associated with these reactions. In that respect, a 6-year follow-up study (1996-2001) conducted in Norway, evaluating the perianaesthetic anaphylaxis, showed that neuromuscular blocking agents (NMBAs) (mainly suxamethonium) were the main drugs causing immunoglobulin E-mediated anaphylaxis in a percentage of 93.2% compared to other drugs9. However, these results are not in accordance with other studies and this may be due to referral bias, differences in testing methods or geographical differences. Furthermore, due to the fact that during the years 1997-2000 rocuronium was found to be responsible for an increasing number of adverse reactions (55) and deaths (3), Norwegian Medicines Agency recommended that rocuronium should be used only in situations demanding urgent intubation and that rocuronium should not replace suxamethonium)10.
In another survey conducted in France during the years 1999-20008, it was shown that among 789 patients who experienced anaphylactic and anaphylactoid reactions during anaesthesia, anaphylactic reactions were diagnosed in 66% and anahylactoid in 34% of the study population. The most common causes of anaphylaxis were NMBAs accounting for 58%, latex for 16% and antibiotics for 15.1% of the cases. Among NMBAs, rocuronium and succinycholine were the main responsible drugs accounting for 43.1% and 22,6 respectively. There were no differences between anaphylactic and anaphylactoid reactions as far as the occurrence of atopy, asthma or drug intolerance is concerned and the writers concluded that these results corroborate with the need for allergoanaesthesia centers.
Concerning the deaths due to anaesthesia related anaphylaxis, it is reported that anaphylaxis is involved totally or partially in 3% of the deaths in France11 and in 10% of the deaths in UK1 ).
Drugs or substances responsible for anaphylactic reactions during the preoperative period
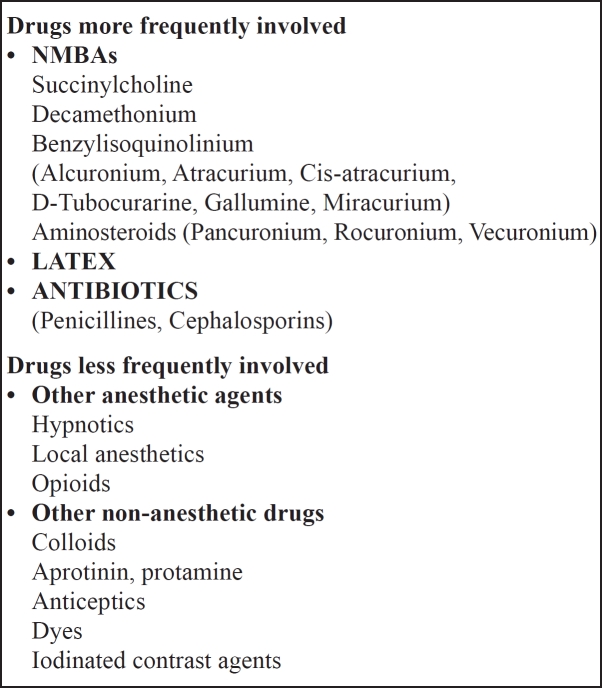
As shown in Table 1, NBMAs, latex and antibiotics are the most common agents responsible for anaphylactic reactions during anaesthesia.
Table 1. Drugs involved in anaphylaxis during the perioperative period3.
NMBAs, including succinylcholine, are associated with the most frequent incidence of anaphylaxis (50- 70%) 6,10,12.
Latex - a component of most sterile and nonsterile gloves, face masks, tourniquets, catheters and airway devices, is the second most common cause of anaphylaxis. As reported in a French study, latex was the causative agent of anaphylaxis in 22.3% of cases13.
Antibiotics Anaphylactic reactions to antibiotics administered during the peri-operative period continue to increase with time and count for 15% of the cases13.
Hypnotics, local anesthetics, opioids and inhaled anesthetics as well as colloids, aprotinine14 (0,09%), protamine, antiseptics, dyes and iodinated contrast agents3 are less often or rarely associated with anaphylaxis.
Pathogenesis and Clinical Manifestations1,3
The clinical manifestations of anaphylaxis are derived from the acute release of mediators from mast cells and less often from basophils.
Anaphylaxis is a type I immune mediated allergic reaction involving mast cells and possibly basophils whereas anaphylactoid reactions occur through a direct non-immune mediated release of mediators from mast cells and/or basophils or result from direct complement activation, presenting clinically with symptoms similar to anaphylaxis. Anaphylaxis can occur peri-operatively, presenting with severe allergic reactions, during surgery where multiple drugs are administered and mainly during anesthesia15.
Anaphylaxis is a clinical syndrome that affects multiple organ systems due to a massive release of mediators from tissue mast cells or circulating basophils, as a response to an allergen. On initial exposure to an allergen in pre-senitized individuals, IgE is produced and binds to high-affinity IgE receptors on the membrane of mast cells and basophils. On re-exposure to the same antigen, the antigen cross-links two IgE receptors. This initiates a signal transduction cascade which results in the release of preformed mediators such as histamine, proteases, proteoglycans and platelet activating factor15,16,17. Phospholipid metabolism then generates potent inflammatory leukotrienes (LTC) and prostaglandins (PGD). As potent vasoactive mediators, histamine, LTC4 and PGD2 are implicated in:
Histamine: vasodilation, smooth muscle constriction, direct cardiac effect and nerve end stimulation which could present as erythema, edema, arterial hypotension, bronchial and gastrointestinal constriction, tachycardia, pruritus and angioedema,
LTC4 and PGD2 cause bronchoconstriction and increased vascular permeability
Anaphylactoid reactions are derived from the activation of the complement and/or bradykinin cascade and the direct activation of mast cells and/or basophils. The clinical symptoms of these reactions are similar and indistinguishable from anaphylaxis, and sometimes severe, leading to cardiovascular collapse and death18.
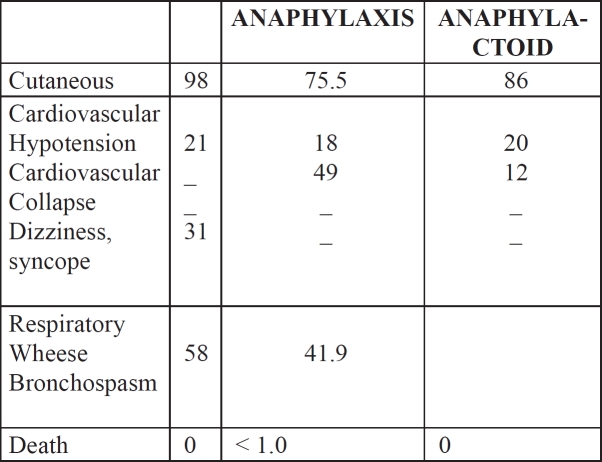
Severe allergic reactions during anesthesia or surgery are characterized by a different clinical profile from reactions in the non-operating setting19 (Table 2).
Table 2. Clinical manifestations of serious allergic reactions19.
Management of anaphylaxis
The management of anaphylaxis consists of:
Withdrawing the drug responsible for this reaction
Interrupting the effects of preformed mediators release as a response to the antigen(drug)
Preventing more mediator release
Immediate management
The cornerstones of treatment are19,20 :
Immediate discontinuation of the anesthetic and drug
Early administration of epinephrine at 5 to 10 µg IV bolus doses for hypotension and at 0.1 to 0.5 mg IV doses in the presence of cardiovascular collapse
Airway support with 100% oxygen
Intravenous administration of crystalloid (2-4 L) for the replacement of the peripheral vasodilation
Histamine 1 and 2 blockers
Bronchodilators and corticosteroids
Epinephrine infusion may be necessary to maintain blood pressure
Concluding remarks
The potencial severity of anaphylactic reactions during the peri-operative period or anesthesia should focus on developing a rational approach to reduce its incidence by identifying potential risk factors before surgery. History of atopy and presence of drug or food intolerance should be carefully assessed during anesthesia pre-operative evaluation and patient's medical history. Since anaphylaxis may occur at any time during anaesthesia, the most important point should be alertness and immediate management by anaesthesiologists and allergists.
References
- 1.Sidiropoulos I. In: Drug Allergy. Chavales A, Chatzisymeon K, editors. Thessaloniki, Greece: Rotonta; 2010. [Google Scholar]
- 2.Mertes PM, Laxenaire MC. Anaphylaxis during general anaesthesia. Prevention and management. CNS Drugs. 2000;14:115–133. [Google Scholar]
- 3.Dewachter P. Peri-operative anaphylaxis. In: Pichler WJ, editor. Drug hypersensitivity. Basel: Karger; 2007. [Google Scholar]
- 4.Association of Anaesthetists of Great Britain an Ireland Suspected anaphylactic reactions associated with anaesthesia. Anaesthesia. 2009;64:199–211. doi: 10.1111/j.1365-2044.2008.05733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnansson SGO, Bieder T, Dahl R, Friedman PS, Lanier BQ, Lockey RF, et al. Revised nomenclature for allergy for global use: report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol. 2004;113:832–836. doi: 10.1016/j.jaci.2003.12.591. [DOI] [PubMed] [Google Scholar]
- 6.Fisher M, Baldo BA. Anaphylaxis during anaesthesia: Current aspects of diagnosis and prevention. Eur J Anaesthesiol. 1994;11:263–284. [PubMed] [Google Scholar]
- 7.Levy JH, Gottge M, Zaffer R, McCall C. Weal and flare responses to intradermal rocuronium and cistracurium in humans. Br J Anaesth. 2000;85:844–849. doi: 10.1093/bja/85.6.844. [DOI] [PubMed] [Google Scholar]
- 8.Mertes PM, Laxenaire MC, Alla F. Anaphylactic and anaphylactoid reactions occurring during anesthesia in France in 1999-2000. Anesthesiology. 2003;99:536–545. doi: 10.1097/00000542-200309000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Harboe T, Guttormsen AB, Irgens A, Dybendal T, Florvaag E. Anaphylaxis during anesthesia in Norway. A 6 year single-center follow-up study. Anesthesiology. 2005;102:897–903. doi: 10.1097/00000542-200505000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Guttormsen AB. Allergic reactions during anaesthesia - increased attention to the problem in Denmark and Norway. Acta Anaesthesiol Scand. 2001;45:1189–1190. doi: 10.1034/j.1399-6576.2001.451001.x. [DOI] [PubMed] [Google Scholar]
- 11.Lienhart A, Auroy Y, Péquignot F, Benhamou D. Survey of anesthesia-related mortality in France. Anesthesiology. 2006;105:1087–1097. doi: 10.1097/00000542-200612000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Laxenaire M. Substances responsible for peranesthetic anaphylactic shock: a third French multicenter study(1992-1994) Ann Fr Anesth Reanim. 1996;15:1211–1218. doi: 10.1016/s0750-7658(97)85882-0. [DOI] [PubMed] [Google Scholar]
- 13.Mertes PM, Laxenaire MC, Membres du GERAP Epidemiologie des reactions anaphylactiques et anaphylactoides peranesthésiques en France. Septième enquète multicentrique. Ann Fr Anesth Reanim. 2004;23:1133–1143. doi: 10.1016/j.annfar.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 14.Dietrich W, Ebell A, Busley R, Boulesteix AL. Aprotinin and anaphylaxis: analysis of 12403 exposures to aprotinin in cardiac surgery. Ann Thorac Surg. 2007;84:1144–1150. doi: 10.1016/j.athoracsur.2007.05.015. [DOI] [PubMed] [Google Scholar]
- 15.Hepner DL, Castells MC. Anaphylaxis during the perioperative period. Anesthesia Analgesia. 2003;97:1381–1395. doi: 10.1213/01.ANE.0000082993.84883.7D. [DOI] [PubMed] [Google Scholar]
- 16.Adkinson F, Pongrack J. Drug allergy. In: Holgate ST, Church MK, Lichtenstein LM, editors. Allergy. 2nd ed. London: Mosby; 2001. [Google Scholar]
- 17.Koppert W, Blunk JA, Petersen LJ, Lars J, Skov P, Rentsch K. Different patterns of mast cell activation by muscle relaxants in human skin. Anesthesiology. 2001;75:659–667. doi: 10.1097/00000542-200109000-00019. [DOI] [PubMed] [Google Scholar]
- 18.Castells MC, Horan RH, Ewan PW. Anaphylaxis. In: Holgate ST, Church MK, Lichtenstein LM, editors. Allergy. 2nd ed. London: Mosby; 2001. [Google Scholar]
- 19.Menon DK. Allergic reactions in the preoperative period. Immunology and Transplantation. The Medicine Publishing Company Ltd. 2003. pp. 190–193.
- 20.Lee JM, Greenes DS. Biphasic anaphylactic reactions in pediatrics. Pediatrics. 2000;106:762–776. doi: 10.1542/peds.106.4.762. [DOI] [PubMed] [Google Scholar]
- 21.Nicklas RA, Bernstein IL, Li JT. Algorithm for the treatment of acute anaphylaxis. J Allergy Clin Immunol. 1998;101:S469–4. [Google Scholar]